Services on Demand
article
Indicators
Share
Journal of Human Growth and Development
Print version ISSN 0104-1282
Rev. bras. crescimento desenvolv. hum. vol.22 no.3 São Paulo 2012
ORIGINAL RESEARCH
Profile of technology-dependent children in Ribeirão Preto-SP
Aline Cristiane Cavicchioli OkidoI; Miyeko HayashidaII; Regina Aparecida Garcia LimaIII
IRN. Ph.D. candidate, Graduate Program in Public Health Nursing at the University of São Paulo at Ribeirão Preto College of Nursing
IIRN. Ph.D. in Nursing, University of São Paulo at Ribeirão Preto College of Nursing. E-mail: miyeko@eerp.usp.br
IIIRN. Advisor. Full Professor, Maternal-Infant Nursing and Public Health Department, University of São Paulo at Ribeirão Preto College of Nursing
ABSTRACT
The aim of this descriptive and exploratory research with a quantitative approach was to characterize technology-dependent children living in Ribeirão Preto - SP regarding gestation and birth conditions, origin of the special health needs and care demands. Participants were 102 mothers or responsible caregivers. Data were collected between January and April 2011 through the application of a form during home visits. The results revealed that 57% of the children are male; the predominant age range was between 1 and 4 years; 7.8% of the mothers had no prenatal follow-up; 96% were born in hospitals; 63.7% through c-section and, in 29.3% of cases, the children were premature. As for the origin of the special health needs, 65.7% had some congenital problem, 30.4% experienced problems during delivery and/or in the neonatal period and 30.4% experienced problems during the lifetime, defined as acquired causes. Regarding special care demands, all children display technological care demands, 92 need medication care, 74 developmental care and 102 modified habitual care. The study appoints relevant data to broaden these clients' visibility in official rates and public policies, so as to guarantee qualified and comprehensive care delivery.
Key words: pediatric nursing; child care; chronic illness.
INTRODUCTION
The epidemiological profile of children in Brazil has changed. At first, immunopreventable diseases considerably contributed to the morbidity-mortality situation. Today, perinatal problems outline a new trend in this context, with early neonatal deaths being responsible for more than half of Brazilian children's deaths in the first year of life. This indicates the need to adapt care processes, ranging from individual care to the organization process of the care network for pregnant women, delivered and infants1-3. In addition, other factors contributed to this change, such as the improvement in environmental and nutritional conditions of the Brazilian infant population, the implementation of health programs, strategies and actions focusing on the morbidity and mortality situation, like the National Immunization Program (PNI) for example and, finally, the incorporation of new technologies in the recovery of congenital and acquired childhood diseases1.
In this perspective, as a result of advances in public policies and medical practice in care delivery to preterm children, with congenital anomalies and chronic illnesses, a group of children emerged who need technological life-maintenance support4 and are part of the group known as children with special health needs (CRIANES)5 in Brazil and as children with special healthcare needs6 in international literature.
The CRIANES are children who need individual and personalized care, in weak health conditions, who need health and social service monitoring beyond what healthy children need4-6. Their problems can be physical, developmental and behavioral, sometimes needing the use of more sophisticated technologies to guarantee their survival; in this case, they are technology-dependent children. In a study involving children in the United Kingdom7, the following types of artifacts or devices were found: tracheotomy, nasal catheter, oxygen torpedo, oxygen concentrator, mechanical ventilation, intravenous drugs, parenteral nutrition, peritoneal dialysis and gastrostomy.
Another classification for children with special health needs is related to the required care demand: children with developmental care demands, i.e. children with neuromotor dysfunctions; children who demand medication care; children who demand modified habitual care, including special daily care that goes beyond the care offered to children who are considered healthy, like vital sign monitoring and oxygen saturation, and, finally, children who demand technological care, included in the group of dependents, which comprises children who depend on some life-maintaining device. It should be highlighted that this classification is merely didactical, as a child may require more than one care demand8.
Studies9-10 identify a lack of records on how many children with special health needs exist and indicate that they live in marginalized conditions and that health, education, transportation systems, among others, do not recognize them.
In the United States, although prevalence rates are not exact, in a study aimed at developing national estimates for the number of children with special health needs and their characteristics, it was observed that approximately 13% of children in the country fitted into this group11. The number of technology-dependent children is unknown in the United Kingdom as well, as there is no database showing this estimate; available information, however, suggests that technology-dependent children are under the age of two years, with possible regional variations in the prevalence of these cases12.
In Brazil, researchers from Rio de Janeiro developed a study aimed at characterizing discharged from pediatric intensive care and rank them according to the care types demanded after discharge. As a result, they identified that 6.3% of these children were considered as having special needs13.
The lack of epidemiological data represents a challenge for health professionals, as they are confronted with the invisibility of these clients in official rates and in public policies, hampering the planning and implementation of strategies aimed at these children.
Thus, the aim is to characterize technology-dependent children living in Ribeirão Preto - SP according to pregnancy and birth conditions, the origin of their special health needs and the care demands.
METHODS
A descriptive study with a cross-sectional design and a quantitative approach was developed14. The research took place in Ribeirão Preto, a city in the Northeast of São Paulo State.
As the study involved human beings, approval was obtained from the Research Ethics Committee, in compliance with National Research Ethics Committee - National Health Council Resolution 196/96, under protocol number 405/ CEP-CSE-FMInclusion criteria were set as follows: children up to 12 years of age, in line with the Child and Adolescent Statute15, living in Ribeirão Preto-SP and dependent on some technological device for life maintenance.
As information on this group of children was not systemized at health services, an active search was developed in the city between October and December 2010. First, nurses in the city's primary healthcare network were contacted, comprising 47 establishments, with 28 Primary Healthcare Units (UBS), 13 Family Health Units (USF), 5 Basic and District Health Units (UBDS) and one Basic and Specialized Unit; in addition to the Home Care Service - SAD and the Support Centre for the Physically Disabled - NADEF16. Explanations were provided about the project and the nurses' cooperation was asked to indicate technology-dependent children within their coverage area, including not only children the service monitored, but also children attended at other institutions.
The institutions that support children with special health needs, registered at the Municipal Council for Child and Adolescent Rights, as specified in articles 90 and 91 of the Child and Adolescent Statute15, were also visited. These included: Spina Bifida and Hydrocephalus Association; Cantinho do Céu - Home to the Exceptional; Ribeirão Preto Specialized Educational Activity Centre - CAEERP; Centro Ann Sullivan do Brasil; Child Center "Dr. Camilo de Matos"; Francisco de Assis Support Hospital; Home Medical Care Outpatient Clinic - University of Ribeirão Preto and the Dental Care Centre for Special Patients at the University of São Paulo at Ribeirão Preto School of Dentistry.
Although these institutions had a list with the names of all children registered, this did not always include information on the use of devices. Therefore, articulation with the professionals involved in care delivery to these children started with a view to getting further clarification on the use of technological devices. Two institutions that deliver care to these clients in Ribeirão Preto did not agree to participate in the research.
Also, strategies were elaborated to disseminate the research in written and spoken communication means. In addition, 150 posters were distributed across the health units and support services, inviting families of children using tube feeding, gastrostomy, tracheotomy, oxygen therapy, mechanical ventilation, peritoneal dialysis, among others, to invite in the study. It should be highlighted that, although these strategies were used successfully in international studies, did not cause any considerable impact in this study as, despite their use, only four people interested in participating in the research came forward.
In the belief that there were technology-dependent children who were not registered at any public health service, private home care services were contacted. In Ribeirão Preto, two large health insurances attend to the population, one of which informed mainly taking care of adults, and that children are rare. It was also informed that, besides medical monitoring and hospitalizations through the insurance, the Unified Health System contributed by providing inputs like drugs, daily material, oxygen torpedo and other equipment. Hence, the three children monitored at this service were also followed by the Municipal Health Secretary's Home Care Service and, therefore, were already included in the study. The second health insurance refused to participate in the study.
To identify technology-dependent children, the key-informant strategy was also used14. Thus, as one family was contacted, the researchers tried to find out whether they knew other children in the same condition. Through this strategy, a considerable number of children were surveyed who were not registered at the health services.
At the end of the active search, 124 children were identified who complied with the inclusion criteria. Home visits took place between January and April 2011 but, after the visit, it was identified that some children had stopped using the technological device, while others had died. In addition, some cases were excluded due to difficulties to get access to the families, as four failed attempts were identified as an exclusion criterion. Only one mother refused to participate in the research. Thus, in the end, 102 technology-dependent children participated in the study, five of whom were institutionalized in support institutions.
The data collection instrument applied during home visits include the child's identification data, with the name and address of the responsible person, and questions on pregnancy and birth conditions and the origin of the special needs. Another dimension that was addressed refers to four care demands: medication care, developmental care, technological care and modified habitual care demands7.
The instrument was completed, using mothers or responsible caregivers' reports as a source; hence, referred data were used. The patients' files were only used to complete the instrument of the five institutionalized children.
Data were coded and validated through double entry in an Excel worksheet, and then transferred to SPSS version 16.0 for descriptive analysis. Thus, results will be presented as frequencies and percentages for nominal variables and as means and standard deviations for numerical ones.
RESULTS
Identification of technology-dependent children
In the sample of 102 technology-dependent children, 58 (57%) are male and 44 (43%) female; ages between six months and 12 years, mainly between one and four years (40.2%), with a mean age of 5.5 years (standard deviation = 3.8). As for the color the mothers or responsible caregivers referred, 71 (69.6%) were considered white, 21 (20.6%) mulatto and 10 (9.8 %) black.
Pregnancy and birth conditions of technology dependent children
In Table 1, it is observed that, what prenatal care is considered, 71 (69.6%) mothers attended the recommended consultations, i.e. more than six; eight (7.8%), however, did not get any monitoring during this period. Regarding the reason for not participating in prenatal care, in two cases, scheduling difficulties were alleged and, in six, the biological mother's involvement with alcohol and drugs or psychiatric problems.
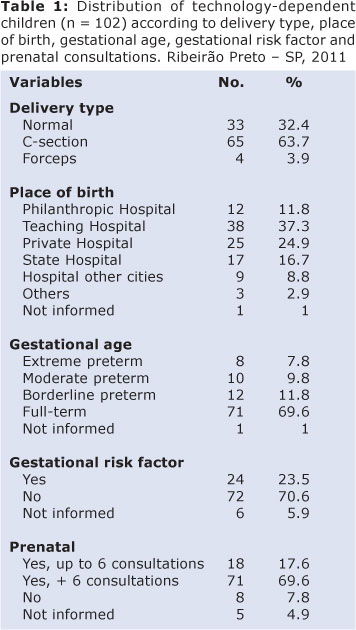
The children were mainly born through c-section (63.7%). Concerning gestational age, prematurity occurred in 30 (29.3%) cases. Eight (7.8%) of these children were born after less than 32 weeks of pregnancy, i.e. extreme prematurity.
As for the place of birth, 98 (96.1%) children were born at hospital institutions, 38 (37.3%) of whom at a tertiary teaching hospital. Only three children in the sample were born at home, at the primary healthcare unit and in the ambulance.
With regard to gestational risk factors, as mentioned, this information originated in the mothers or caregivers responsible for the technology-dependent children. Thus, out of 24 (23.5%) referred cases, twin pregnancy was the gestational risk factor in seven (29.2%); abuse of alcohol and illicit drugs in six (25%); four (16.7%) developed pregnancy induced hypertension; there were two (8.3%) cases of association between systemic arterial hypertension and type 2 diabetes; 1 (4.2%) case of toxoplasmosis; one (4.2%) case of gestational diabetes and one of (4.2%) type 1 diabetes; one (4.2%) case of antiphospholipid antibody syndrome (SAAF) and one (4.2%) case of uterine rupture.
The mean weight at birth was 2681 grams (standard deviation = 782.9) and the median 2780 grams, with 635 grams as the minimum and 4950 grams as the maximum weight. The mean height was 46.1cm (standard deviation = 5.1) and the median 47 cm, ranging from 28 cm to 56.5 cm.
For all 102 children who participated in the study, first and fifth-minute Apgar scores were available in 53 (52%) and 59 (57.8%) cases, respectively. The non-existence of this information is due to a lack of data records on the child's vaccination card. As for the first-minute Apgar, 36 (67.9%) children showed Apgar scores of 7 or higher, indicating no difficulty to adapt to extra-uterine life; 10 (18.9%) scored between 4 and 6, considered as moderate asphyxia, and seven (13.3%) scored 3 or less, classified as severe asphyxia at birth. Concerning the fifth-minute Apgar score, 47 (79.6%) children showed Apgar scores of 7 or higher, indicating no difficulty to adapt to extra-uterine life; 8 (13.6%) scored between 4 and 6, considered as moderate asphyxia, and 4 (6,8%) scored 3 or less, classified as severe asphyxia at birth.
Origins of special health needs
As for acquired causes during the pregnancy period, at birth and in the neonatal period, out of 102 children, 30 (29.4%) were born prematurely, 11 (36.7%) of whom needed hospitalization at neonatal intensive care units; 15 (14.7%) were diagnosed with neonatal hypoxia, following by hospitalization at a neonatal intensive care unit, and 5 (4.9%) needed intensive support soon after birth due to a congenital problem.
Congenital causes affected 67 (65.7%) technology-dependent children, including central nervous system malformations, followed by cardiac diseases, craniofacial malformations, digestive and urogenital malformations. Besides congenital causes, some syndromes were diagnosed, including Fetal Alcoholism Syndrome, Moebius Syndrome, Dandy-Walker Syndrome, Prunne Belly Syndrome, immunodeficiency and spinal amyotrophy.
Among acquired causes that are not related to the pregnancy, delivery and neonatal period, 31 (30.4%) children presented problems across the lifetime, such as tumors, drowning, falls, dog bites, medication administration errors, large surgeries and pediatric intensive care hospitalization due to worsening in clinical conditions.
Although the origins of the children's special health needs were analyzes separately in this study, they end up being related, as some children may suffer from different causes in life that provoke the worsening of their clinical condition.
Care demands of technology-dependent children
According to their special care demands, in line with the study objectives, the 102 (100%) children have technological care demands; 92 (90.2%) need medication care; 74 (72.5%) developmental care and all children need modified habitual care.
The technological devices were divided in three groups: related to feeding, such as nasogastric tube, gastrostomy and jejunostomy; related to urinary or intestinal elimination, including colostomy, ileostomy, urinary catheter and intestinal wash; and oxygenation-related devices, like the oxygen torpedo, oxygen concentrator, nasal catheter, tracheotomy and mechanical ventilation.
Out of 102 children, 71 (69.6%) used technological devices for feeding, 61 (85.9%) through gastrostomy and 10 (14.1%) use nasogastric or nasoenteral tubes. Twenty-nine (28.4%) children use elimination devices, 17 (58.6%) of whom use a urinary catheter for relief, 6 (20.7%) have a colostomy or ileostomy, 2 (6.9%) need intestinal washes, one (3.4%) has an esophagostomy, 2 (6.9%) use both urinary catheters for relief and intestinal washes and 1 (3.4%) maintains an urethrostomy. As for the use of respiratory devices, out of 31 (30.4%) children, 15 (48.4%) have an open-air tracheotomy, 9 (29%) receive oxygen therapy through a nasal catheter, 3 (9.7%) continue with the tracheotomy and use oxygen, and 4 (12.9%) need continuous or partial mechanical ventilation.
The mean usage time of technological devices was 38.2 months (standard deviation = 32.5), median 24 months, with a minimum of one month and a maximum of 144 months.
Among the participants, 92 (90.2%) had medication care demands. The daily medication these technology-dependent children most use includes anticonvulsants, with 57 (62%) children; 29 (31.5%) antibiotics therapy; 28 (30.4%) anti-reflux medication; 26 (28.3%) food supplements and vitamins; 21 (22.8%) corticosteroids and 19 (20.7%) muscle relaxants. Also, less frequently, some children use diuretics, anti-hypertensive drugs, hormones and anti-allergic medication.
As for developmental care demands, physiotherapy stands out, as 67 (65.7%) children are monitored; followed by speech, language and hearing therapy with 50 (49%) and occupational therapy with 21 (20.6%) children. Therapeutic riding and swimming are less frequent, involving only three (2.9%) and four (3.9%) children, respectively.
Modified habitual care demands include daily care that goes beyond what is offered to children who are considered healthy; thus, 62 (60.8%) interviewees affirmed specific care to prevent infections, including the sterilization of material and food and avoiding agglomerations like parties and malls. As a considerable part of the children have movement difficulties, 47 (46.1%) mothers or responsible caregivers inform care to prevent ulcers and malformations. Out of 102 participants, 45 (44.1%) demanded bronchoaspiration prevention-related care. Continuous monitoring of convulsive crises and vital signs and oxygen saturation are other modified habitual care acts the children require and correspond to 39 (38.2%) and 16 (15.7%) cases, respectively.
DISCUSSION
The present study results are similar to findings from other studies involving this clientele, among which the predominance of the male gender stands out, representing 57% of the children in this study11,17. The increased survival of CRIANES is another point to be highlighted, as 54.9% of the children are older than five years, affirming that technological and pharmacological advances and modernization guarantee many children's survival11,18.
The association between the origin of the special health need and the perinatal causes confirms epidemiological statistics that indicate morbidity and mortality due to perinatal problems as an ascending curve, responsible for more than 50% of deaths among children under the age of five in 20042. This association indicates the needs for actions that qualify perinatal care services, including measures to prevent complications during delivery and birth2-3.
Prematurity, a situation that involved 30% of the technology-dependent children, demands clinical, pharmacological and nutritional interventions until the child reaches maturity to adapt to extra-uterine life, in most cases demanding hospitalization at neonatal intensive care units. Thus, as they are discharged from intensive care, these infants become different from others, with countless care challenges18.
As another factor originating special health needs, congenital malformations represent the second cause of death in this age range, corresponding to 30% of deaths in children under one year of age in some Brazilian states19. In that sense, governmental strategies exist for their prevention, based on measures like folic acid use before conception and neonatal disease screening20. In addition, advances in diagnostic medicine have contributed to the detection of most malformations still during the pregnancy period, permitting anticipated planning for the infant's birth at an institution that offers adequate support and an experienced multiprofessional team19.
Causes acquired in the child's life are other determinants of special health needs, as exemplified in this study, through drowning, dog bites and falls. Accidents and violence are called external causes and represent important child morbidity and mortality and permanent disability factors, causing social, economic and emotional impacts21. Hence, it is important to plan preventive actions and establish family education strategies with a view to effective surveillance and a reduction in traumatic situations.
The findings reaffirm that transferring a technology-dependent child from the hospital to the home environment represents a big challenge, to the extent that these children and their relatives experience complex medical, social and affective problems, which cannot be managed at a sole care unit(23). A technology-dependent child at home requires responsibility for performing highly technical procedures from caregivers, which only qualified professionals should perform formally4; these procedures include tracheotomy cannula change, airway aspiration, medication preparation and administration, enteral feeding and washing children with stomas.
These children's care demands are specialized and are not part of the families' daily reality. Therefore, nursing can turn into an ally, through the sharing between professionals' technical-scientific knowledge and caregivers' popular knowledge, contributing to the child's wellbeing, avoiding complications and frequent rehospitalizations8.
Discharge planned together with the family and home visits for monitoring become an important source of support, through information, individualized care and continuous follow-up, minimizing feelings of anxiety and fear24. In this perspective, these clients' visibility in official statistics and public policies needs to be enhanced through further studies on the theme, which can provide support to devise the care process for children with special health needs and their families.
REFERENCES
1. Macinko J, Guanais FC, Souza MFM. Evaluation of the impact of the family health program on infant mortality in Brazil, 1990-2002. J Epidemiol Community Health. 2006; 60(1): 13-19. [ Links ]
2. Ministério da Saúde. Saúde Brasil 2004: uma análise da situação de saúde. Brasília: Ministério da Saúde; 2004. 364p. [ Links ]
3. Drumond EF, Machado CJ, França E. Óbitos neonatais precoces: análise de causas múltiplas de morte pelo método Grade of Membership. Cad Saúde Pública. 2007; 23(1): 157-166. [ Links ]
4. Kirk S, Glendinning C, Callery P. Parent or nurse? The experience of being the parent of a technology - dependent child. J Adv Nurs. 2005; 51(5): 456-64. [ Links ]
5. Brown-Hellsten M. Doença Crônica, Incapacidade ou Tratamento Terminal para a Criança e Família. In: Hockenberry MJ, Wlison D, Winkelstein ML. Wong Fundamentos de Enfermagem Pediátrica. 7ª ed. Rio de Janeiro (RJ): Guanabara- Koogan, 1999. p. 549-88. [ Links ]
6. McPherson MG, Arango P, Fox H, Lauver C, McManus M, Newachek PW, et al. A new definition of children with special health care needs. Pediatrics. 1998; 102(1): 137-41. [ Links ]
7. Kirk S, Glendinning C. Supporting "expert" parents- professional support and families caring for a child with complex health care needs in the community. Int J Nurs Stud. 2002; 39: 625-35. [ Links ]
8. Neves-Vernier ET. O empoderamento de cuidadoras de crianças com necessidades especiais de saúde: interfaces com o cuidado de enfermagem. [tese]. Rio de Janeiro: Escola de Enfermagem Anna Nery, Universidade Federal do Rio de Janeiro; 2007. p. 172. [ Links ]
9. Leal RJ. Os (des) caminhos dos cuidados às crianças com necessidades especiais de saúde no discurso das famílias: subsídios para uma política de seguimento. [tese]. Rio de Janeiro: Escola de Enfermagem Anna Nery, Universidade Federal do Rio de Janeiro; 2007. p. 141. [ Links ]
10. Vernier ETN, Cabral IE. Caracterização das crianças com necessidades especiais de saúde e seus familiares cuidadores, Santa Maria (RS), 2004-2005: subsídios para intervenções de enfermagem. Rev Soc Bras Enferm Ped. 2006; 6 (1): 37-45. [ Links ]
11. Dyck PC, et al. Prevalence and characteristics of children with special health care needs. Arch Pediatr Adolesc Med. 2004; 158: 885-90. [ Links ]
12. Glendinning C, Kirk S., Guiffrida AE, Lawton D. Techonology- dependent children in community: definitions, numbers and costs. Child Care Health Dev. 2001; 27(4): 321-334. [ Links ]
13. Cabral IE, Silva JJ, Zillmann DO, Moraes JRMM, Rodrigues EC. A criança egressa da terapia intensiva pediátrica na luta pela sobrevida. Rev Bras Enferm. 2004; 57(1): 35-9. [ Links ]
14. Polit D, Beck CT, Hungler B. Delineamentos para a pesquisa em Enfermagem. In: Polit D, Beck CT, Hungler B. Fundamentos de pesquisa em enfermagem: métodos, avaliação e utilização. 5ª ed. Porto Alegre (RS): Artmed; 2004. p. 161-244. [ Links ]
15. Brasil. Ministério da Saúde. Estatuto da Criança e do Adolescente. Lei nº 8.069 de 13 de julho de 1990. Dispõem sobre a proteção integral da criança e do adolescente. Diário Oficial [da] Republica Federativa do Brasil, Brasília, 16 jul.1990. [ Links ]
16. Ribeirão Preto, 2009. Relatório de Gestão da Secretária Municipal de Saúde do Município de Ribeirão Preto - 2010 (endereço http://www.ribeiraopreto.sp.gov.br/ssaude). [ Links ]
17. Kirk S. How children and young people construct and negotiate living with medical technology. Social Science & Medicine. 2010; 71: 1796-1803. [ Links ]
18. Cabral IE, Moraes JRMM, Santos FF. O egresso da terapia intensiva neonatal de três instituições públicas e a demanda de cuidados especiais. Esc Anna Nery Rev Enferm. 2003; 7 (2): 210-217. [ Links ]
19. Reis AT. O significado da cirurgia neonatal na presença de malformações congênitas: a visão materna para o cuidar de enfermagem. [tese]. Rio de Janeiro: Escola de Enfermagem Anna Nery, Universidade Federal do Rio de Janeiro; 2010. [ Links ]
20. Gaíva MAM, Corrêa ER, Santo EARE. Perfil clínico- epidemiológico de crianças e adolescentes que vivem e convivem com espinha bífida. Rev Bras Crescimento Desenvolvimento Hum. 2011; 21(1): 99-110. [ Links ]
21. Silva MAI, Pan R, Melo L, Bortoli OS, Nascimento LC. Perfil dos atendimentos a crianças e adolescentes vítimas de causas externas de morbimortalidade, 2000-2006. Rev Gaúcha Enferm. 2010; 31(2): 351-8. [ Links ]
22. Fracolli RA, Angelo MA Experiência da família que possui uma criança dependente de tecnologia. Rev Min Enferm. 2006; 10(2): 125-131. [ Links ]
23. Wang KW, Barnard A. Technology-dependent children and their families: a review. J Adv Nurs. 2004; 45(1): 36-46. [ Links ]
24. Pinto JP, Ribeiro CA, Pettengill MAM. O processo de recuperação da criança após a alta hospitalar: revisão integrativa. Acta Paul Enferm. 2010; 23(6): 837-42. [ Links ]
 Corresponding author:
Corresponding author:
acc@eerp.usp.br
Manuscript submitted Sep 18 2011
Accepted for publication Mar 30 2012