Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Journal of Human Growth and Development
versão impressa ISSN 0104-1282
Rev. bras. crescimento desenvolv. hum. vol.24 no.1 São Paulo 2014
ORIGINAL RESEARCH
Nutritional status of neurological patients with reduced mobility
Rosana Farah SimonyI; Daniela Maria Alves ChaudI; Edeli Simioni de AbreuI; Silvana Maria Blascovi-AssisII
IProfessor of Nutrition at the Mackenzie Presbyterian University (Universidade Presbiteriana Mackenzie)
IIProfessor of Physiotherapy and of the Graduate Program in Developmental Disorder at the Mackenzie Presbyterian University
ABSTRACT
OBJECTIVE: to assess the nutritional status of neurological patients in physiotherapy treatment.
METHODS: this is a descriptive and transversal research in which all patients treated in an university physical therapy clinical at metropolitan region in Sao Paulo were invited to participate. After signing the informed consent by participants or their parents or guardians, nutritional consultation was scheduled to collect identification data and anthropometric data for the examination of bioelectrical impedance analysis and classification of nutritional status. We evaluated 24 patients of both sexes, aged between 3 and 62 years, divided into two groups (children and youth, and adults n = 10, n = 14) who underwent physical therapy in the clinic and who had limited mobility.
RESULTS: regarding socio-demographic variables, most of the patients had rated socioeconomic status between B1 and C1. The gastrointestinal symptoms most related were gastritis and gastro esophageal reflux. The most adult patients showed: normal weight (64.3%) followed by obesity (21.4%) and overweight (7.1%). They also submitted cardiovascular risk among moderate and high, according to waist circumference. The prevalence of malnutrition was 20% in children and adolescents. The percentage of body mass averaged 24.2%.
CONCLUSION: this is a sample that shows anthropometric commitments and important nutritional need for systematic monitoring of health education.
Key words: nutritional status, body composition, evaluation, neurology.
INTRODUCTION
The etiology of central nerve injury can vary from a congenital anomaly, vascular accidents, spinal cord injuries to degenerative illnesses. These clinical cases, apart from their seriousness and irreversibility in most cases, demand a long rehabilitation program, generating high cost for the government and resulting in major changes in the patient's lifestyle1.
Neurological disorders arising from injuries to the central nerve system may compromise the nutritional status depending on the affected area, having sometimes a detrimental effect on the physical and cognitive capacities required for a proper nutrition.
Brainstem injuries can, for example, infiltrate any of the cranial nerves that innervate facial and head structures, having an effect on nutrition, due to the fact that the patient is often unable to eat without running the risk of directing food or liquid into the lungs2.
Children with neurological damage are often affected by one or more factors that hamper proper food ingestion, such as alterations to chewing and gastric emptying, gastroesophageal reflux, motor incoordination, inability to feed oneself, which lead to nutritional and growth anomalies3.
Malnutrition is one of the factors that helps the most to delay growth, because of inadequate nutrient intakes, themselves affected by oral and motor dysfunctions4.
Patients with acute and chronic neurological illnesses can suffer dysphagia given the absence of swallowing reflexes, resulting in a high risk of malnutrition. Thus, so as to prevent aspiration, pneumonia or sepsis complications - which can all arise from the detrimental effects of the illness - nutritional support is highly advisable. Enteral tube feeding may be necessary when there is a high risk of food aspiration or when the patient does not ingest enough to meet nutritional needs2.
Kuperminc and Stevenson5, after reviewing the literature, claim that suction, chewing and swallowing disorders are common in patients with cerebral palsy and explain inadequate food intakes, exacerbating thereby the risk of malnutrition. In addition, many children with functional motor limitations are kept on inappropriate diets for their age for long periods, resulting in deficiency anaemia (mainly for lack of iron), malnutrition and repetitive infections, due to the unvaried offer of certain types of food (milk and dairy products, flour foods or juices after the age of six.) Malnourished children do not grow normally and their reply to the stimuli that promote development is hindered and increase nutritional risk.
Thus, a diet must be planned according with the clinical characteristics and the limitations of each patient, so as to, among others, help swallowing and reduce the reflux of gastric content into the esophagus. It is recommended that the child's head and body are kept in an uptilted position for a few minutes following a meal. In children with gastroesophageal reflux, meals must be of smaller amounts and served at shorter intervals so as to prevent loss of overall daily nutritional intakes. Children with difficulties to ingest liquid must be fed small amounts of mildly-consistent meals and given juice thickened with fruits and jelly, ensuring, thereby an adequate level of hydration6.
Another common complication in neurological patients is intestinal constipation. This is so because the longer the faeces remain in the colon, the harder they get, and more water absorption is needed; hence constipation. Chronic intestinal constipation is the result of, among others, a number of factors, such as, limited intake of fiber and liquids, few physical activities and use of antacids and anti-epileptic medicine7.
If the colon (large intestines) is not yet dilated (megacolon)8, families must be encouraged to offer a diet based on the adequate intake of liquids in general, foods rich in fiber, such as fruits (papaya, pineapple, orange with bagasse, black plum, mango, water melon) vegetables (mainly those of raw leaves) pulses (beans, peas, lentils) and wholemeal foods.
Some neurological patients often suffer digestive complications, pressure ulcers and weight gain. This weight gain usually occurs a few months after loss of body mass associated with the recovery from serious injuries, compromising sometimes basal metabolism by 10 to 30%, when compared to a person of the same age range, which reduces the energy needs in these patients. These two agents facilitate, thus, weight gain9.
The study of nutritional management of neurological patients has developed in the last years since the nutritional condition greatly affects the body's physiological responses and the state of injury in which they find themselves.
Growth disturbances are related to restricted mobility which results from neurological or biomechanical constraints. One hypothesis about disturbances to growth is related to nutritional factors, including inadequate diet, a result of swallowing and speech motor control difficulties. The application of physical force to the bones leads to a significant gain in bone mass10 irrespective of an individual's age and gender11. A decrease in strain, which is characterized by the mechanical pressure on the bones, resulting from extended periods of immobility is also related to a decrease in bone formation12. Lack of active mobility, therefore, affects different aspects of a neurological patient's life, justifying therefore research into nutritional aspects.
Anthropometry measures in a static way the different body parts. It includes weight, height, skin folds and limbs circumference. Among the advantages of anthropometric measurement, low cost, simple equipment and ease of result attainment stand out13. It is recommended to patients of different ages and levels of nutrition. These measures are extensively used in the assessment of nutritional status on an individual and broad population level, due especially to the ease with which measurements can be checked, the low-cost involved and to the vast availability of data on these. The most common measure-ments used in the nutritional diagnosis are weight and height. Generally, these measurements are used together, giving rise to indexes, such as the body mass index - BMI14.
BMI is recommended by the World Health Organization - WHO15 as a fast and cheap means to measure body fat. Despite all the advantages, recent studies have called into question the use of BMI on patients with spinal cord injuries because of changes in the body composition (loss of lean body mass and its replacement by fat mass). One of the examples was a review study carried out by Buchholz and Bugaresti16 on patients with spinal cord injuries, in which BMI average measurements between 20 and 27 kg/m2 were found, supposedly similar to those recommended by WHO17 to classify overweight and obesity. However, it is not known yet if these cut-off points could be used with patients with spinal cord injuries or other neurological impairment. This is because BMI may be underestimated due to difficulties in the collection of weight and height data, which are many times given by the patients themselves, putting under question the reliability of the results. Therefore, one alternative means of nutritional assessment is the electrical bioimpedance method through which the percentage of body fat can be obtained. Although the test does not reveal how fat is spread in the body, it allows us to find out if the values are within those recommended with regards to health standards and the prevention of chronic diseases in adult life18.
Obesity is directly related to body fat percentage (%F); however it is not possible to quantify it within the minimum error rates possible. In the last years, researchers in the area have developed and validated different techniques of evaluation of body composition. Yet, most of these meant high costs, rendering unfeasible their use19.
Because of all this, determining the nutritional condition and the body composition of neurological patients is of crucial importance, since they are vulnerable to weight gain and to an increase in the percentage of body fat, which can directly affect their mobility and degree of independence, hampering or limiting physiotherapeutic treatment and the continuity of assistance.
Thus, the aim of this study is to assess the nutritional status of individuals with neurological injuries, as well as describing their nutritional status from measurements of body mass index and body fat percentage.
Methods:
This was a cross-sectional study with primary data collection, in which patients treated at the physiotherapy clinic of a community university in São Paulo were assessed within the months of March 2011 and February 2012. The criteria for inclusion was the submission of a medical diagnosis of neurological damage and limited mobility, of gait abnormality and use of means of support such as crutches, walking sticks, walkers or wheelchairs.
At the beginning, a socio-demographic and lifestyle questionnaire was used containing, among others, questions on age, gender, educational background, marital status, smoking and drinking habits, gastrointestinal health and place and duration of injury. The socio-economic questionnaire recommended by the Brazilian Association for Demographic Studies - ABEP20 was used with the aim of describing more precisely the socioeconomic level.
Data on anthropometric variables, nutritional status classification and the bioimpedance analysis test were individually collected, at a time set with the patients and their legal guardians. The project was submitted to and approved by the Committee for Ethics in Research of the Mackenzie Presbyterian University under no. 1340/04/2011 and CAAE no. 0035.0.272.000-11.
Anthropometric Variables: The following criteria were adopted for the collection of anthropometric variables:
a) Weight:
• Children: those patients who could remain in an upright position were weighed on the scales, but when this was not possible, the accompanying adult was individually weighed prior to being weighed with the child on their lap. The child's weight was then obtained by deducting the amounts found. The weight was measured in Kilograms, using Filizola® platform scales for a maximum weight of 150 kilograms and a minimum of 100 grams. The patients wore light clothes and were barefoot when weighed.
• Adults: the patients were carried by physiotherapy team members and placed on a stretcher, so that the wheelchair could be weighed separately on the scales provided for this purpose. Then, the patients were put back in their respective wheelchairs and weighed. The patient's weight was obtained by deducting the value of the wheelchair. When weighing was not possible, the weight was provided verbally by the patients or their guardians.
b) Height
Height was calculated on the length of arm, which was arrived at by having one of the arms stretched out in a 90º angle with the body, measuring the distance between the wishbone and the tip of the middle finger. A flexible metric tape measure was used for this. Estimated height was obtained through the Kwok and Whitelaw21 equation, that is, the length between the wishbone and the arm (cm) multiplied by 2. In the cases this method could not be applied, height was given verbally from the patients or their guardians.
c) Waist Circumference
The abdominal circumference (AC) measu-rement was used around the umbilical button with the help of a 2mt-long inextensible tape measure and with a 1mm precision as measurement of waist circumference (WC) was impossible since most patients were on a wheelchair.
Classification of the nutritional status and the risk of metabolic diseases:
Classification of the nutritional status was realized following the body mass index (BMI) using the classification criteria recommended by the World Health Organization17 for adults and the growth curves of this index for children and adolescents15, using values of percentiles as reference. The patients' nutritional status was classified as malnutrition, eutrophy, overweight and obesity, based on the weight (kilograms) and height (meters) anthropometric variables.
As for the risk of cardiovascular diseases and the presence of abdominal obesity, the criteria used was the one proposed by Taylor et al22 for children and adolescents with AC above the 80th percentile, according to age and gender. For adults, references by the International Diabetes Federation (IDF)23 and the National Cholesterol Education Program (NCEP)24 were used and defined as:
• No risk: below 80 cm in adult women and below 94 cm in adult men
• Moderate risk: above 80 cm in adult women and above 94 cm in adult men
• High risk: above 120 cm in adult men; there are no reference values for children and adolescents.
Bimpedance Testing:
Following the collection of anthropometric data, all the patients underwent a bioelectrical impedance analysis (BIA), which is based on the conduction of low intensity electric current and estimates the percentage of lean body mass, fat mass, percentage of water and the basal metabolic rate. Prior to the execution of the test, all patients and their accompanying family members received the necessary instructions for the performance of the test so as to ensure the reliability of the data obtained.
The bioelectrical impedance analysis was carried out using a TANITA® model TBF-305 analyzer of corporal composition, with the patient lying on a non-conducting stretcher, with their arms and legs stretched at the surface's level. Then, the patient's skin was cleaned with alcohol-soaked cotton wool on the electrodes' contact areas, be they the left foot, ankle, hand and wrist so that the analyzer could be programmed to send low density electric current. The patient's data (age, gender, weight and height) was fed to the machine that provided the percentages of body fat (BF), lean body mass (LBM) in kilograms and the basal metabolic rate (BMR). All the patients were advised to observe the following recommendations: to refrain from consuming alcohol within 48 hours prior to the test, any food or liquid within 2 hours prior to the test and caffeine-based drinks; from hard physical exercise within 24 hours prior to the test; from taking diuretic medicine (if agreed with the doctor) within 7 days prior to the test; to remove all metal objects such as watches and jewelry during the test and, in the case of women, not to do the test during their menstrual period.
RESULTS AND DISCUSSION
The sample used in this study comprised 24 patients of both genders, with an age range of 3 and 62 years, all patients presenting a type of neurological disease and attending the physiotherapy clinic of a community university in São Paulo, between the months of February and December 2011. The diagnoses were varied, with brain injury, cerebral palsy, progressive diseases like multiple sclerosis or myopathies, spinal cord injury, congenital malformation and connective tissue diseases.
For the analysis of certain data, the 24 patients were divided into two groups: Group 1 (G1), of children and adolescents between the ages of 3 and 17 years (n = 10); and Group 2 (G2), of adults between the ages of 24 and 62 years. (n = 14).
It must be noted that in the study sample 45.8% (n = 11) of patients were female and 54.2% (n = 13) were male. The average age was 21.1 years (sd ± 17.4) and 25% (n = 6) of all patients were married.
Table 1 summarizes the socioeconomic profile of the sample studied, showing that 50% of the participants belonged to B2 class, followed by B1 together with C1 classes.
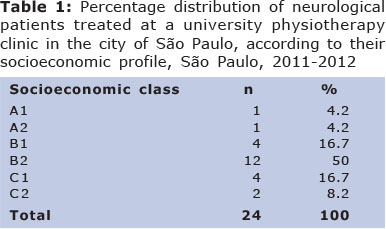
Table 2 shows the length of time for diagnosis and the characteristics of duration and frequency of physiotherapeutic treatment carried out at the clinic. It can be noted that the average time for diagnosis and physiotherapy treatment was 7.5 and 5.5 years, respectively. As a result of a neurological injury, 62.5% of patients had to undergo a type surgery after their diagnosis.
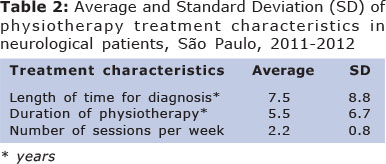
Figure 1 point to the prevalence of dis-comfort and/or gastrointestinal complications in the patients seen. It was found that 33.3% of all patients suffered gastritis and 20.8 gastro-esophageal reflux. These findings coincide with those in the medical literature, which claim that the presence of these gastrointestinal symptoms affect mainly patients with spinal cord injury, due to the need of surgeries, use of nasogastric tubes, as well as to the prevalence of parasympathetic tonus25,26, though the same symptoms may be present in patients with other neurological diagnoses.
It is important to mention that such complications cause discomfort in the patient and can affect directly their nutritional status, since frequent changes in diet are necessary to avoid or lessen the symptoms27.
Table 3 shows data of two cases of malnou-rishment in children and adolescents (G1) and a high percentage of overweight and obesity in adult patients (G2). As to cardiovascular risks, based on waist circumference in all age ranges, especially in adults, the presence of risk was observed. Nevertheless, this observation must be treated with caution, as circumference was measured while patients were lying, a position in which an error may have been incurred during execution.
Countless studies18,28,29 have noted the prevalence of overweight and obesity, based on BMI, in patients with neurological injury, although some writers point out that BMI is little sensible to evaluate obesity in this group of population. This is because, due to physical inactivity, these patients are prone to show high percentages of body fat with high risks of metabolic diseases and therefore health complications30.
Currently, there is no BMI optimal cut off points to diagnose the nutritional status of neurological patients, since BMI is a tool made to evaluate individuals in good health conditions15. That is why the use of bioelectrical impedance analysis can be considered a more precise method to aid in the analysis of body composition.
Table 4 shows data on body composition and basal metabolic rate (BMR) of neurological patients in this study, through bioelectrical impedance analysis according to their nutritional state. The result bear relationship with those expected in healthy individuals, since in states of malnourishment, BMR is low. The physiological explanation for this resides in the fact that the body starts to save energy in an effort to preserve the wellbeing of all vital organs and tissues. The reverse occurs in the case of obesity, characterized by the increase in body mass (both, fat mass and lean body mass) and, as a result, an increase in the daily basal caloric needs. It was interesting to find out that contrary to such claim, average BMR of overweight patients was higher than the average BMR in obese patients. This can be explained by the small sample size: 1 overweight patient and 3 obese patients, which prevents a more convincing explanation.
The data provided by the bioelectrical impedance test are only descriptive, due to the shortage of validated reference values in literature to classify the body composition of neurological patients. However, the data from the bioelectrical impedance test described in this study are pioneer and can corroborate the elaboration of future reference values for the adequate body composition of these patients.
CONCLUSION
We can conclude, based on the data collected, that there are several complications in these patients in relation to nutritional status, and the adult group had a higher prevalence of obesity and consequently a higher percentage of body fat. These results point to the peculiarities of this population, which needs constant review and guidance to increase their wellbeing and quality of life.
REFERENCES
1. Greve JMD. Reabilitação na lesão da medula espinhal. Rev Med. 1999;78(2):276-86. [ Links ]
2. Reming VM, Weeden A. Tratamento Clínico Nutricional para Distúrbios Neurológicos. In: Mahan LK, Escott-Stump S. Krause: Alimentos, Nutrição e Dietoterapia. 11ª ed. São Paulo: Roca; 2005. p.623-955. [ Links ]
3. Stevenson RD. Use of segmental measures to estimate stature in children with cerebral palsy. Arch Pediatr Adolesc Med. 1995;149:658-62. [ Links ]
4. Weisstaub G, Durán CC, Mujica JF, Briones C. Nutrición en el niño con daño neurológico. Rev Chil Pediatr. 1996;67(3):130-35. [ Links ]
5. Kuperminc MN, Stevenson RD. Growth and nutrition disorders in children with cerebral palsy. Dev Disabil Res Rev. 2008;14:137-46. [ Links ]
6. Rede Sarah De Hospitais De Reabilitação. Disponível em http://www.sarah.br/. Acesso em 23 de novembro de 2013. [ Links ].
7. Engler TMNM, Farage L, Mello PA. Constipação intestinal em pacientes admitidos em programa de reabilitação neurológica. Acta Paul Enferm. 2011;24(6):804-09. [ Links ]
8. Rodriguez TN, Rocha ECV, Zanandréa EF. Síndrome da obstipação intestinal. Rev Bras Med. 2004;61(4):174-80. [ Links ]
9. Cardozo-Gonzales RI, Villa TCS, Calin MHL. O processo da assistência ao paciente com lesão medular: gerenciamento de um caso como estratégia de organização da alta hospitalar. Medicina. 2001;34(1):325-33. [ Links ]
10. Brandão CMA, Vieira JGH. Fatores envolvidos no pico de massa óssea. Arq Bras Endocrinol Metab. 1999;43(6):401-08. [ Links ]
11. Ryan AS, Ivey FM, Hurlubut DE, Martel GF, Lemmer JT, Sorkin JD. et al. Regional bone mineral density after resistive training in young and older men and women. Scand J Med Sci Sports. 2004;14(1):16-23. [ Links ]
12. Bell KL, Boyd RN, Tweedy SM, Weir KA, Stevenson RD, Davies PS. A prospective, longitudinal study of growth, nutrition and sedentary behaviour in young children with cerebral palsy. BMC Public Health. 2010;10(1):179. [ Links ]
13. Waitzberg DL, Ferrini MT. Exame Físico e Antropometria. In: Waitzberg DL. Nutrição Oral, Enteral e Parenteral na Prática Clínica. 3ª ed. São Paulo: Atheneu; 2001. p.255-78. [ Links ]
14. Anjos LA, Warhlich V. Avaliação Antropométrica: In: Taddei JA, Lang RMF, Longo-Silva G, Toloni MHA. Nutrição em Saúde Pública. Rio de Janeiro: Rubio; 2011. p.55-72. [ Links ]
15. WHO (World Health Organization). Child Growth Standards (2007). Disponível em http://www.who.int/childgrowth/standards/en/. Acesso em 23 de novembro de 2013. [ Links ]
16. Buchholz AC, Bugaresti JM. A review of body mass index and waist circumference as markers of obesity and coronary heart disease risk in persons with chronic spinal cord injury. Spinal Cord. 2005;43(1):513-18. [ Links ]
17. WHO (World Health Organization). Obesity - Preventing and Managing the Global Epidemic. Report of a WHO Consultation. Geneva; 1998. [ Links ]
18. Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson RN, Waters, RL. et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol. 2003;95(6):2398-407. [ Links ]
19. Rezende F, Rosado L, Franceschinni S, Rosado G, Ribeiro R, Marins JCB. Revisão crítica dos métodos disponíveis para avaliar a composição corporal em grandes estudos populacionais e clínicos. Arch Latinoamer Nutr. 2007;57(4):327-34. [ Links ]
20. ABEP - Associação Brasileira de Empresas de Pesquisa, 2010. Disponível em http://www.abep.org/novo/FileGenerate.ashx?id=252. Acesso em 23 de novembro de 2013. [ Links ]
21. Kwok T, Whitelaw MN. The use of armspan in nutritional assessment of the elderly. J Am Geriatr Soc. 1991;39(1):492-96. [ Links ]
22. Taylor RW, Jones IE, Williams SM, Goulding A. Evaluation of waist circumference, waist-to-hip ratio, and conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3-19 y. Am J Clin Nutr. 2000;72(2):490-5. [ Links ]
23. IDF (International Diabetes Federation). Clinical Guidelines Task Force. Global Guidelines for Type 2 Diabetes. Diabet Med. 2005;23(5):469-80. [ Links ]
24. NCEP (National Cholesterol Education Program). Third Report of the Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). NHI Publication. 2001;01-3670. [ Links ]
25. Lim PA, Tow AM. Recovery and regeneration after spinal cord injury: a review and summary of recent literature. Ann Acad Med Singapore. 2007;36(1):49-57. [ Links ]
26. Ghafoor AU, Martin TW, Gopalakrishnan S, Viswamitra S. Caring for the patients with cervical spine injuries: what have we learned? J Clin Anesth. 2005;17(8):640-49. [ Links ]
27. Lobo SM, Miranda ALD. Disfunção do trato gastrointestinal prolongada em pacientes admitidos na terapia intensiva. Rev Bras Ter Intensiva. 2010;22(2):118-24. [ Links ]
28. Weaver FM, Collins EG, Kurichi J, Miskevics S, Smith B, Rajan S. et al. Prevalence of obesity and high blood pressure in veterans with spinalcord injuries and disorders: a retrospective review. Am J Phys Med Rehabil. 2007;86(1):22-9. [ Links ]
29. Gupta N, White KT, Sandford PR. Body mass index in spinalcord injury - a retrospective study. Spinal Cord. 2006;44:92-4. [ Links ]
30. Wilt TJ, Carlson FK, Goldish GD, MacDonald R, Niewoehner C, Rutks I, Shamliyan T. et al. Carbohydrate & Lipid Disorders & Relevant Considerations in Persons with Spinal Cord Injury. Evidence Report/Technology Assessment Nº 163. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [ Links ]
Manuscript submitted Aug 01 2013
Accepted for publication Dec 28 2013
Corresponding author:













