Services on Demand
article
Indicators
Share
Interamerican Journal of Psychology
Print version ISSN 0034-9690
Interam. j. psychol. vol.41 no.1 Porto Alegre Apr. 2007
ENFRENTANDO A LOS OTROS: ESTIGMA EN EL SECTOR SALUD
Stigma and discrimination for HIV/AIDS in the health sector: a polish perspective
Estigma y discriminación por VIH/SIDA en el sector salud: una perspectiva polaca
Maria Gañczak1
Pomeranian Medical University, Szczecin, Poland
ABSTRACT
The manifestations of the HIV/AIDS epidemic in Poland, as in other countries, have been received with stigma and discrimination towards those living with the disease. The social implications of stigma are worsened when they hinder the provision of effective treatment by members of the health sector. One such limitation is the perceived need for mandatory HIV testing among hospital patients. This practice can violate the rights of the patient and foster stigmatization. This quantitative study had as its main objectives to survey: 1) the degree of fear of acquiring HIV at work among surgeons and surgical nurses, and 2) the impact of HIV/AIDS training and practical experience with HIV patients on support for a testing policy of admitted patient and those who would undergo surgery among the same sample. Results evidence support for HIV testing of all inpatient admissions in hospitals and pre-operative testing among both nurses and surgeons. Training on HIV matters can be an important factor for lowering support for mandatory testing.
Keywords: HIV, Acquired Immune Deficiency Syndrome, Stigma, Health care service, Hospitalized patients, Poland.
RESUMEN
Las manifestaciones de la epidemia del VIH/SIDA en Polonia, al igual que en otros países, han sido recibidas con estigmatización y discrimen hacia las personas que viven con la enfermedad. Las implicaciones de este estigma empeoran cuando afectan negativamente el ofrecimiento de servicios por miembros del sector salud. Una de estas limitaciones es la necesidad percibida de llevar a cabo pruebas de VIH mandatorias entre pacientes hospitalizados. Esta práctica puede violar los derechos de los pacientes y fomentar estigmatización. Este estudio cuantitativo tuvo como objetivos principales explorar: 1) el nivel de miedo de adquirir VIH en escenarios de trabajo entre profesionales de la cirugía y enfermería, y 2) el impacto del adiestramiento sobre VIH/SIDA y experiencias prácticas con pacientes en el apoyo a políticas de pruebas de VIH compulsorias en pacientes en hospitales y de condición pre-operativa. Los resultados evidencian apoyo a pruebas de VIH en ambos tipos de pacientes entre profesionales de enfermería y cirugía. El adiestramiento sobre temas relacionados al VIH puede ser un factor importante al reducir el apoyo a estas purbas mandatorias.
Palabras clave: VIH, Síndrome de Inmunodeficiencia Adquirida, Estigma, Servicios de salud, Pacientes hospitalizados, Polonia.
HIV/AIDS became an urgent medical and social problem in the early 1980s. It has been spreading rapidly because of its characteristics and has become a health threat and the most devastating disease humankind has ever faced. HIV spreads making no distinctions by religion, language, ethnic origin, sex, or country base.
Research investigating the psychological experience of people living with HIV/AIDS (PLWHA) indicates that these patients do not suffer only from the physical disease process. They experience emotional agony not only because there is no cure for AIDS, but also because of a public frenzy that ends in blaming the victim. The social stigma attached to HIV and AIDS leads to social rejection of patients. Sontag (1988) pointed out that diseases of unknown cause and ineffective treatment evoke fear and revulsion, and that in North American culture cancer was once the disease of fear and shame. Nowadays, AIDS has replaced cancer, and the experiences of many PLWHA parallel those of cancer patients. Cherry and Smith (1993) have stated that the literature of social knowledge that explains cancer as a dreaded disease has been transferred to HIV. Such phenomena have been observed in many countries all over the world, among them Poland. HIV is currently a metaphor of "sinful" and "evil", discrediting an individual's claim to be a "moral character" and "one of us".
Stigma and discrimination fuel the HIV/AIDS epidemic by creating a culture of secrecy, silence, ignorance, blame, shame and victimization (Taylor, 2001). This has an effect on PLWHA as individuals, and on their illnesses, behavior and perception of the health care they receive. In Europe and North America HIV/AIDS is most prevalent in populations that have been disenfranchised by society, including homosexual men and intravenous drug users. Health care workers (HCWs), being human, bring to their medical work their foibles, anxieties, and deficiencies that characterize the human species. Unfortunately, there is no requirement in the medical school of any nation that the physician be sensitive to the problems of disenfranchised groups. When members of these groups acquire an illness related to their behavior, which is frowned upon by many HCWs, it becomes easier for such HCWs to behave in a discriminatory manner (Shapiro, Hayward, Guillemot, & Jayle, 1992).
An essential question to ask is the degree to which societal prejudices and stigmatization, linking the illness to one or another "specific lifestyle" and "sexual behavior", influence the health sector. The answer is crucial, because of the power of health professionals in their role of establishing the physical and emotional welfare of PLWHA.
HIV/AIDS in Poland
Epidemiological Situation
The first report of an AIDS case in Poland was made in 1986. The history of AIDS in Poland began with a homosexual. As a result, the disease was immediately stigmatized by its association with socially disapproved sexual behavior. Since that time, the number of newly registered HIV cases has stabilized at 500-600 persons per year. Data from the National Institute of Hygiene (2005) showed 9 new infections in 1986, 59 in 1988, 809 in 1990, 539 in 1995, 579 in 1997, 527 in 1999, 559 in 2001, and 574 in 2003. By the end of September 2005, there were reported to be 9659 HIV infected people in Poland. Many experts indicate that this figure is far from reality, due to the long asymptomatic period for HIV. Another factor affecting reporting is that individuals who may be infected with HIV avoid screening because they believe that self-disclosure will result in stigmatization. HIV infection is linked in many people's minds with homosexuality, injection drug use, sexual activity, and commercial sex - behaviors that not only make people feel uncomfortable, but also challenge attitudes and values. To disclose that they are sero-positive is difficult for people with HIV/AIDS, because they believe that society will isolate them and their social milieu will threaten them.
About three-thirds of those currently living with HIV/AIDS in Poland are males. The majority of newly detected HIV carriers are men aged 20-29. The main route of transmission is use of injectable drugs; 55% of PLWHA were infected in this way. Unfortunately, the main mechanism of transmission is unknown for about 25%.
A rapid increase in HIV-infected persons in neighboring countries, including Russia, Belarus, and the Ukraine, as well as the rise in importance of heterosexual intercourse as a means of spread, may become threats to the health of the Polish population (National Institute of Hygiene, 2005; Rosiñska & Werbiñska, 2004).
Myths and Facts
HIV/AIDS is a topic that has unleashed a flood of opinions. Unfortunately, these opinions are often based upon an insufficient knowledge about such a sensitive topic. As a result, people tend to develop unscientific explanations or myths. A major function of a myth is to reduce peoples' fears of personal vulnerability by implying that such events happen only to "other" kinds of people. Myths also provide convenient and over-simplified explanations of complex social issues. When repeated often enough, myths become "conventional wisdom" and may pass for well-established facts. Myths about HIV/AIDS have been particularly hard to dispel (Juszczyk & G³adysz, 1999; Sobeyko, 2003).
The arrival of HIV/AIDS in Poland was sufficiently delayed to allow time to prepare society to face the threat. The earliest initiative in prevention came from the Ministry of Health just after the first AIDS case was diagnosed. According to one or their circulars, HIV/AIDS is accepted as a contagious disease and should be so declared. The National AIDS Center as well as programs such as The National Program for HIV - Infection Prevention, and Care of People Living with HIV and AIDS was created to coordinate efforts to combat the infection. Interventions included widespread distribution of condoms, free needle-exchange programs, an anonymous HIV-testing system, and public information about the infection. In recent years, a number of governmental and non-governmental organizations (NGOs) have done much to try to change social attitudes towards PLWHA (Sobeyko, 2003).
At the beginning of the epidemic, HIV/AIDS education was introduced at Polish schools. This education was provided by various organizations outside the Department of Education, including sanitary-epidemiological centers and NGOs, and was financed by the Ministry of Health. At the end of the 1990s, schools implemented HIV/AIDS topics into their own curriculum. Students 13-15 years of age are given one hour of teaching per academic year on "STD/AIDS", and there is a second hour for older youth on the topic of "Immune Deficiency". Such educational interventions were associated with some positive changes. Surveys in Poland during 1990 to 2002 showed a significant increase in tolerance towards PLWHA among 15 and 17-year-olds (Gañczak, Boroñ-Kaczmarska, Leszczyszyn-Pynka, & Szych, 2005; Woynarowska, Szymañska, & Mazur, 1999).
Nonetheless, AIDS is still a serious social and psychological problem in Poland. Numerous campaigns have concentrated mainly on improving the knowledge of particular social groups, such as youth, persons vulnerable to infection, and medical staff. Unfortunately, adults who have already completed or dropped out of school have not yet been selected as a target population for HIV/AIDS educational campaigns. Furthermore, media, an important potential source of HIV/AIDS information, are reluctant to lead educational actions, and prefer to seek more sensational topics (Izdebski, 2003).
The lack of information and education on HIV/AIDS influences people's attitudes towards the infected. Surveys were conducted in Poland during 1997-1998 on randomly selected, representative groups. It was found that although nearly 90% knew the main routes of HIV transmission, less than 5% knew the prevalence of PLWHA in the community. There was a significant age-difference in the proportion of individuals willing to take care of a relative with AIDS, with almost 66% of 15-17-year-olds willing to do so, compared with only 33% of adults.
Nearly 50% of youth, but only 27% of adults, agreed that there is nothing wrong with homosexuality (Izdebski, 2000). This difference could perhaps be interpreted as evidence that education early in the school curriculum may lead to change of some homophobic attitudes. On the other hand, there is a general taboo against discussing homosexuality in society, and conservative forces such as the Roman Catholic Church actively oppose more open debate. Although the gay movement has gained a higher profile in some parts of the country, an evident change of social and public attitudes towards sexual minorities has not yet appeared, especially among adults (Staugard, 2000). Homophobic attitudes remain widespread among Poland and are major factor in HIV/AIDS-related discrimination. In illustration, doctors and nurses from all over Poland were surveyed in 1997-1998, and were found to believe that homosexuality is a "social pathology", like drug addiction, alcoholism, and Satanism (Ciastoñ-Przeclawska, 2001). In another 1997 survey, 70% of Poles aged 17-59 treated homosexuality as a disease and wanted such persons to be cured. Homophobic attitudes among political leaders are also widely reported. In November 2005, the former head of state Lech Walesa said: "I believe homosexuals need medical treatment". When asked whether homosexuality should be condemned, Polish Prime Minister Kazimierz Marcinkiewicz stated: "It's unnatural. The family is natural and the state must stand guard over the family. If a person tries to `infect' others with their homosexuality, then the state must intervene in this violation of freedom" (LifeSite, 2005, line 7). Lack of tolerance for homosexuality is not only a Polish phenomenon. A decade earlier, 25% of young people in the United States agreed with the statement that gay men "deserve to get AIDS" (Imperato, 1996).
Health Sector and HIV/AIDS Stigma Legislation
In Poland the right to medical care is guaranteed by article 68 of the Polish Constitution (1997). This means equal access to all publicly financed health institutions. The Charter of Patients Rights cites this article of the constitution as the basis of the right to medical care (Minister of Health and Social Welfare, 1998). The charter has no legal powers and was created simply to inform patients about their rights.
According to Article 30 of the Polish Act on Physician's Profession (1996), the right to medical care means the right to competent care, and that every physician must help a patient whenever she/he requests. It also adds that this obligation is in force when delay could result in death, grievous body harm, health disorder, or in other cases of emergency. This clause could allow a health provider o refuse to treat a patient in the absence of such conditions. Nevertheless, another clause was included to help avoid leaving patients being left without care. If a physician wants to discontinue treatment for a patient, he/she must inform the patient in a timely manner how to obtain care from another physician or health facility.
The Code of Medical Ethics (1993) also imposes the duty of helping any person who asks for it; however, the code also states that where justifiable, the physician is not forced to provide care, except in emergencies. Nevertheless, the physician must inform his patient about other possibilities for obtaining treatment.
Some physicians refuse to help PLWHA, without consequence. A fragment of a letter by a 30-year-old HIV-infected drug user sent to the United Nations Development Program Office in Warsaw stated: "I had a serious sinusitis, doctors were considering purulent meningitis as a consequence of the basic disease. But they left me without any help, not willing to mess up their hands" (Malinowska-Sempruch, 1997).
Patient autonomy means that a patient has the right to decide about his/her treatment and can refuse consent for any medical intervention. This includes HIV screening. The physician's duty to obtain informed, freely given consent is an obligation established by national and international law.
According to international guidelines for HIV/AIDS and Human Rights, an individual's interest in protecting her/his privacy is "particularly compelling in the context of HIV/AIDS". This is for two reasons: first - mandatory HIV test is invasive, and, second, disclosure of HIV status leads to stigma and discrimination from loss of privacy and confidentiality.
Article 17 of the International Covenant on Civil and Human Rights protects privacy and forbids lawless interference in somebody's private or domestic life, home, or correspondence, as well as lawless attempts on somebody's honor and good name. The Covenant also says that everyone has the right to such protection. Article 8 of the European Convention for Protection of Human Rights and Fundamental Freedoms states that everyone has a right to respect of her/his private and family life, home, and correspondence. Granting these rights means that PLWHA do not have to reveal their infection. These rights also imply the patient's right to anonymous screening for HIV.
Article 47 of the Polish Constitution guarantees the protection of private and domestic life, honor, good name and the right of deciding about personal life. This right is of great importance to PLWHA as it implies many rights for patients and many obligations for medical staff. For the first time informed consent was created in the Polish legal system by the act on Medical Care Centers (1997), article 19.1.3, which states that a patient has the right to consent or to refuse, after obtaining proper information. The Ministry of Health, in Recommendations for Medical Staff (1997), creates more specific requirements for HIV infection, stating that the patient must be fully informed about any plans to screen for HIV and about the nature of HIV infection itself. The physician must obtain the patient's informed consent for such screening and prepare the patient psychologically in the event there might be a positive result. The patient has a right to anonymous screening.
As mentioned above the number of PLWHA is increasing in Poland and all over the world. Many need surgical treatment and the risk of complications after surgery in HIV infected patients is shown to be lower than initially feared (Gerberding, Lewis, & Schecter, 1995). As the consequences of acquiring HIV infection are so great, most surgeons and nurses working at the surgical suit, where blood exposures are so common, understandably fear acquiring infection. As a result many support controversial policies such as universal preoperative HIV testing, and indeed many support testing of all inpatients (Chapman, Meadows, Catalan, & Gazzard, 1995; Danziger, Abel, Goddard, McGrouter, & Pawson, 1996; Joint Working Party of the Hospital Infection Society and the Surgical Infection Study Group, 1992).
There has been vehement debate surrounding the question of preoperative HIV testing of patients. Opponents, represented by people who are professionally involved in HIV/AIDS problem, state that routine HIV antibody testing of patients is not recommended. The testing is opposed by many because of the civil rights implications of a positive test result and the fear that HIV-positive patients would receive sub-optimal treatment. Testing should be undertaken only on the basis of clinical assessment or where it is in the interest of both: patients and HCWs. The provision of patient's confidentiality and privacy, as well as informed consent for testing is essential. Any argument that more stringent precautions would be put in place for those who are tested as HIV positive would fly in the face of universal precautions, which are meant to prevent the transmission of known and not-known blood-borne pathogens in all instances (Dammani, 2003; World Health Organization [WHO], 2000). On the other hand, medical personnel believes that, dealing with the patient, they have the right to know whether they are at risk for acquiring a potentially fatal infection after exposure to patient's blood. The routine HIV antibody testing would help them to prevent such an infection. They suggest that the knowledge that one of their patients is sero-positive would cause them to use special procedures during operations which would decrease the risk of acquiring HIV infection. According to this view, it is difficult to practice these precautions at the 100% level, 100% of the time (Shanson, 1991; Tyndall & Schechter, 2000).
HIV-antibody testing was implemented in Poland in 1985, just few months after such tests had been required in the rest of Europe. However, regarding this issue, the practice presently existing in Polish hospitals only theoretically fulfils requirements set by legal provisions. Lot of hospitals have implemented HIV testing concerning patients admitted to the surgical wards or admitted for diagnostic procedures. Although there are no requirements or standard protocols for pre-operative and universal testing of all admissions, surgeons often implement their own screening programs, some other permanently review the possibility. Most often the patient is informed about the character of surgical intervention (and about the consent) directly before it starts, usually in very hermetic professional language not understandable for the average person. The consent is given during preparation to the intervention so the patient rarely carefully reads what is to be signed. Regarding how stressed he/she is, it is not fair to call such consent "informed". The patient is not able to estimate any information given rapidly by the medical staff, often even not by the physician (Sobeyko, 2003). It must be said that such testing is illegal, simply because is not used to make a diagnosis. It appears that the information about serological status of the patient is "indispensable to a hospital" (Juszczyk, 1995). It is important to point out that routine screening of all patients admitted to the hospital is an easy way to destroy the patient's life and that is not the purpose of HCW's.
In light of these challenges and difficulties, the main objective of this study was to survey: 1) the degree of fear of acquiring HIV at work among surgeons and surgical nurses from the same surgical wards, and 2) the impact of HIV/AIDS training and practical experience with HIV patients on support for a testing policy of admitted patient and those who would undergo surgery among the same sample.
Method
A descriptive and analytical survey was conducted among doctors (2001) and nurses (2003) from the same wards representing surgical specialities at 4 hospitals located in the city of Szczecin (2 academic, 2 municipal), as well as 4 situated in the County of Western Pomerania. This region of north-western Poland borders Germany and the Baltic Sea and is close to Berlin. Hospitals were selected from a Health Department list using a random-number table. At the selected hospitals, all surgical wards participated.
Data Collection
An anonymous questionnaire was developed for the survey, using guidelines from a study in New York (Lowenfels, Wormster, & Jain, 1989). The survey covered the following areas:
- Part 1: Age and sex of doctor/nurse, type of hospital.
- Part 2: Number of HIV patients treated, attendance to HIV/AIDS training, level of concern of acquiring HIV infection at work, and number of sharps injuries per year.
- Part 3. Opinions about HIV testing of patients, and whether it should be mandatory.
Questionnaires were mailed to hospital administrators between May 2001 and March 2003. The purpose of the survey was explained to respondents and they were assured of anonymity. All doctors and nurses present in the ward on the day when the questionnaire was administered completed it. Each subject was asked to respond independently. No doctor or nurse present at the time of survey refused to participate. The final sample included 132 doctors and 383 nurses. Questionnaires were stored in a locked cabinet and computer data password-protected.
Data Analysis
Data analysis was performed with the use of STATISTICA PL software. Categorical data were analyzed by chi square, chi square test with Yates correction, Fisher exact test (two-side test), chi-square Mc Nemar test, and chi square for trend for more than two categories, with significance at p<0.05. For the purposes of comparing doctors and nurses with and without training and experience, all doctors/nurses who had had one or more courses together were grouped as having experienced the intervention, and all doctors/nurses with occupational experience of one or more known HIV patients were grouped as positive for that "intervention".
Results
Composition of Sample
The sample included doctors with a median of age 39 years (range 26-73) and nurses 20 to 58 years old, with a median of 36 years. The vast majority of doctors were males (n=106; 80%) and 99% (n=379) of nurses were female. Eighty per cent of participants were recruited from urban teaching hospitals, 15% from urban non-teaching, and 5% from rural. Location of work included general surgical wards (51%), ob/gyn wards (29%), orthopaedic wards (12%), urology (4%) and otolaryngology (4%).
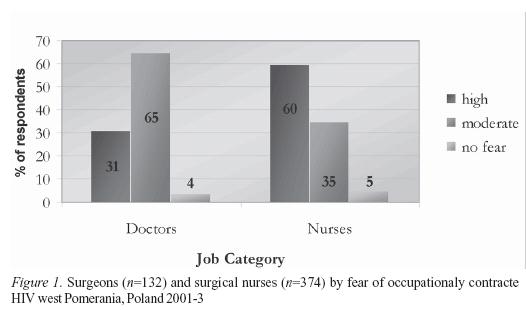
Training, Experience, History of Injury
One or more sessions of HIV/AIDS training was reported by 49% of doctors (n=65) and 77% (n=296) of nurses, one or more occupational experiences caring for a known HIV patients was reported by 55% (n=72) of doctors and 30% (n=116) of nurses. At least one percutaneous injury had been sustained in the preceding year by 98% (n=129) of doctors and 46% (n=177) of nurses. One per cent of doctors (n=1) and 17% (n=65) of active nursing staff did not regularly use gloves while in contact with potentially infected material. All doctors and 374 nurses answered the question regarding fear of contracting HIV infection at the workplace. HIV concern was admitted by 96% (n=127) of doctors and 95% of nurses (n=355) (Figure 1).
Attitudes towards HIV Testing
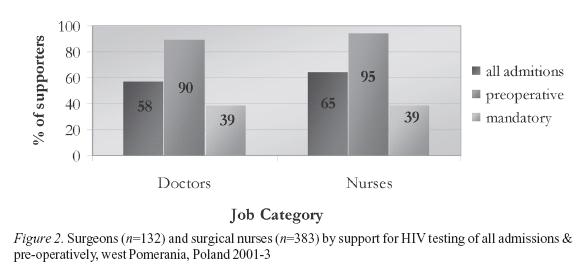
HIV testing of all inpatient admissions was supported by 58% (n=76; 95% CI 49-66%) of 132 doctors and 65% (n=247; 95%CI 59-69%) of 383 nurses (p>0.15) and pre-operative testing of all surgical admissions by 90% of doctors (n=119; 95%CI 84- 94%) and 95% (n=365; 95% CI 92-96%) of nurses - p<0.04 (Figure 2). There were statistically significant differences between numbers of doctors/nurses supporting HIV testing of all admissions and pre-operative testing (p<0.001) (Figure 2).
Regarding both job-categories (doctors and nurses), there were no differences in support of testing of all admissions by age (doctors: p>0.07, nurses: p>0.26), number of injuries in the past year (doctors: p>0.27; nurses: p>0.85). Among doctors there were no differences in support of testing of all admissions by type of hospital (p>0.99). Nurses from municipal hospitals were opting less for such testing than nurses from university and rural hospitals (p<0.002).
There were no differences in support of pre-operative testing by age (doctors: p>0.48; nurses: p>0.33), or by number of injuries in the past year (doctors: p>0.85; nurses: p>0.52), and type of hospital (doctors: p>0.79; nurses: p>0.58).
Mandatory Imposition of HIV testing
Of all respondents 39% doctors (n=51; 95%CI 31-48%) and 39% nurses (n=150; 95%CI 35-44%) thought HIV tests for all admissions should be mandatory. There was no differences in support of such testing by age (doctors: p>0.21, nurses: p>0.24), number of injuries (doctors: p>0.72), and type of hospital (doctors: p>0.75, nurses: p>0.05). Nurses who did not sustain percutaneous injury in the past year were less supportive for mandatory testing than nurses who reported such injury (p<0.02).
HIV Training, HIV Experience, & Attitudes to HIV Testing
Doctors - There was less support of mandatory testing of all admissions by doctors with HIV/AIDS training (p<0.04). Less doctors (34%) with experience with at least one patient supported mandatory HIV testing than doctors without such an experience (41%), but the difference was not statistically significant (p>0.38). The support for mandatory testing was less among doctors with both training and experience, than among doctors with neither training nor experience (chi square for linear trend comparing doctors with neither intervention to either training or experience, or to both training and experience: 4.040, p<0.04) (Figure 3). Confidence intervals included: No intervention - 46% (95%CI 30-62%), experience only - 34% (95%CI 24-46%), training only - 29% (95%CI 19-41%; both training and experience - 24% (95%CI 16-43%) (note: CI were wide for this group, since the sample sizes were relatively small). There was no difference in support of testing of all admissions and pre-operative HIV testing between doctors with and without either or both HIV training or experience (Table 1).

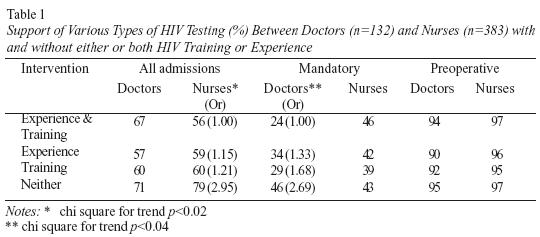
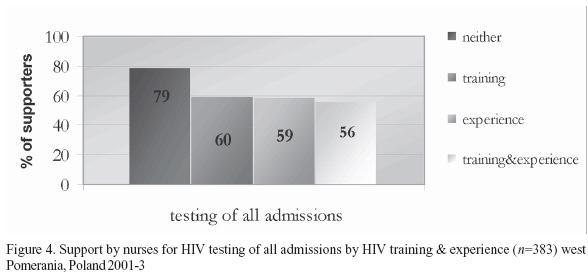
Nurses - Although support for HIV testing of all admissions was relatively high in both groups, there was significantly less support by nurses with HIV/AIDS training (p<0.01). Less nurses (59%) with experience with at least one patient supported such HIV testing than without such an experience (66%), but the difference was not statistically significant (p>0.16). The support for such testing was less among nurses with both: training and experience, than among nurses with neither training, nor experience (chi square for trend: 5.323, p<0.02) (Figure 4). Confidence intervals included: No intervention - 79% (95%CI 66-88%), training only - 60% (95%CI 55-66%), experience only - 59% (95%CI 50-68%), and both training and experience - 56% (95%CI 45-66%) (Figure 4). There was no difference in support of pre-operative HIV testing neither mandatory testing of all admissions between nurses with and without either or both HIV training or experience (Table 1).
Discussion
The most notable feature of this study lies in the divergence between official policy as stated by WHO and Polish regulations (Recommendation for Medical Staff, 1997; WHO, 2000,) and the views (although maybe not the practices) of surgeons and surgical nurses. In our survey, the vast majority of respondents favoured pre-operative HIV antibody testing and a large majority also supported universal HIV testing for all admissions. Concerning surgeons, HIV/AIDS training and practical experience with HIV patients decreased support only for mandatory imposition of HIV testing but not for the idea of testing of all admissions neither for pre-operative testing. The combined impact of training and experience was significantly greater in decreasing support for testing than a single intervention. Regarding nurses, HIV/ AIDS training and practical experience with HIV patients decreased support only for testing of all admissions but not for pre-operative testing. Again, the combined impact of training and experience was significantly greater in decreasing support for testing than a single intervention.
Occupational Risk & Fear of HIV transmission
In the current context in Poland, the results indicate that for most surgical doctors and nurses there is a substantial difference between real and perceived levels of risk for occupational HIV infection. Mathematical estimates of the chances of transmission of HIV to the surgeon vary from 0.1% to up to 10% over a 30-year period. The actual risk depends mainly on the prevalence of HIV infection amongst the surgical patients operated on (Shanson, 1991). The prevalence of HIV carrier state in Poland is relatively low (1.5 for 100,000) comparing to many other countries worldwide, so the risk of contacting infection while working at surgical suite is lower (Rosiñska & Werbiñska, 2004). Accordingly the less fear should be felt by Polish medical professionals, fewer should advocate for HIV screening of patients. Surveys of HCWs generally show that despite the seroprevalence in the population, a concern of contracting HIV at the surgical suit remains on the same level: 95-96% of Nigerian surgical specialists, 96% of practicing American general surgeons, and Polish orthopaedic surgeons and neurosurgeons reported such a concern (no data is available regarding surgical nurses) (Gañczak & Szych, 2004; Obi, Waboso, & Ozumba, 2005; Owotade, Ogunbodede, & Sowande, 2003; Patterson, Novak, & Mac-kinnon, 1998). What differs among surgical personnel worldwide are the numbers of preoperative HIV testing opponents and advocates. In contrast to Poland, in many countries opinions are usually balanced, or testing advocates are only in a small majority (Danziger, et al., 1996; Hoffman-Terry, Rhodes, & Reed, 1992; Wright, Young, & Stephens, 1995).
The degree of risk of occupational HIV infection among surgical nurses as compared with surgeons is greater among the first. Surgeons' injuries are likely to be caused by suture needles, which are believed to be less efficient in transmitting infection than hollow-bore needles. Surgeons also may be more likely to be wearing gloves when the exposure occurs. Wearing gloves may reduce the volume of blood introduced through the injury by more than half (Geberding, et al., 1995; Joint Working Party of the Hospital Infection Society and the Surgical Infection Study Group, 1992; Wright & Mc Geer; 1993). Although the risk of acquiring the occupational HIV infection is small, surgical nurses perceive it as greater comparing to the surgeons, and they fear more. Among the American surgeons, moderate concern was reported by 88%, extreme concern by 8% and no concern by 4% (Patterson, et al., 1998). Among Polish surgeons from this survey slight/moderate fear was expressed by 65%, high fear by 31%, and no fear by 4%. The majority of nurses (60%) reported a high degree of fear of occupational HIV, while moderate degree of fear was perceived only by 35%. The higher degree of fear is probably the main reason why nurses more often than surgeons opt for screening of patients.
Knowledge of Risk of Infection & Personal Experience
According to Brown, Macintyre and Trujillo (2003) there are two kinds of fear: the unfounded fear of casual contagion which can be dispelled through accurate information in appropriate training and the "healthy" fear of the real but low risk of infection from occupational exposures. The authors also agree that not training alone, but a combination of appropriate training and experience with HIV infected patients is necessary to reduce fear levels to a degree where the HCW would not feel the need to test all admissions or all pre-operative patients for HIV.
Currently at Polish hospitals it is not routine to offer regular education regarding blood-borne pathogens. It is usually a one-time or infrequent event, with voluntary attendance. And indeed, 50% of surgeons and 23% of nurses had never attended HIV/AIDS training. There is a lack of regulations regarding such education, as well as a shortage of licensed medical staff and facilities to provide it (Gañczak, Milona, & Szych, in press). The lack of knowledge among doctors and nurses about their actual risk of infection and about pre- and post-exposure prophylaxis could be the main reason for an "unhealthy" degree of fear resulting in the high number of preoperative HIV testing advocates (Gallop, Lancee, & Taerk, 1991; Highriter, Tessaro, & Randall-David, 1995; van Wiessen & Woodman, 1994).
There could be also another explanation of a large number of preoperative HIV testing advocates in surgical suites in Poland, where the HIV/AIDS is rare. Generally, HCWs there are unfamiliar with appropriate management techniques, which may influence discriminating attitudes (Foreman, Lyra, & Breinbauer, 2003).
According to our data 45% of surgeons and 70% of surgical nurses have never had professional contact with HIV infected patient. Contact with such a patient means that medical professionals are more able to develop personal relations (Foreman, et al., 2003). As has been pointed in some other studies conducted among medical personnel such personal experience could also reduce the high degree of fear we found among surgical doctors and nurses (Oerman & Gignac, 1991; Rea, Brown & Calder, 1992; van Wiessen & Woodman, 1994). Since even the best theoretical knowledge cannot replace insight gained by real occupational experiences with infected persons, training with HIV infected patients should be implemented in Polish hospitals, but in a structured educational setting, which would be expected to be more effective than any experience, as reported in this survey.
Disadvantages of Preoperative HIV Screening
The most frequently used HIV tests detect antibodies to HIV, not the virus itself. False negative antibody results that occur in the window period are also possible. In such situations personnel may feel an unjustified sense of security, and relinquish universal precautions. Another issue is that asking a patient about to undergo surgery to submit to an HIV test may generate unnecessary anxiety at an already stressful time, and that a positive result, if it appears, may come as a great shock for an unprepared patient. It is also said that any directive that increases the number of people tested who are at extremely low or now risk will lead to increased numbers of false-positive results. How to deal with false positives, however small they might be? The confirmation is possible only days or weeks later with the Western Blot test at designated reference laboratories. The anxiety to the patient and HCW in the intervening period cannot be doubted. The disadvantage is also the extraordinary expense and difficult logistics inherent in a program of universal testing. How often to retest patients and what is the cost of doing that? Another legitimate argument against universal preoperative HIV testing is in relation to emergency surgery. It should generally be accepted that for all forms of such type of surgery it is safest and most practicable to assume that the patient is HIV antibody positive without the need to perform screening antibody test. The last but not least argument of the pointlessness of preoperative HIV screening comes from the issue of proper counselling and informed consent. It is universally agreed that HIV testing must be accompanied by proper counselling before and after testing. The feasibility of providing proper pre-test counselling to the hundreds of patients before all invasive procedures is dubious in the extreme (Chapman, et al., 1995; Danziger, et al., 1996; Geberding, et al., 1995; Juszczyk, 1995; Shanson, 1991; Tyndall & Schechter, 2000).
Many surgeons and surgical nurses think they would take greater care in the operating room when operating on a high risk patient and believe this justifies screening. A study from San Francisco in a hospital experienced with AIDS patients and in which standard precautions were implemented showed that knowing the HIV status of the patient made no difference on the incidence of sharps injury (Gerberding, Littell, & Tarkington, 1990).
In considering possible implementation of obligatory HIV testing, we should not forget an obligation for doctors. According to the Polish Medical Code of Ethics of 1993 and Polish Doctors' Law of 1996, every doctor should keep secret information about his patient obtained during professional work, including prevention and control. This need is deeply justified by the fear of denying access not only to medical care, but also to employment, education, or religious affiliation. Unfortunately, at the average Polish hospital, keeping information from HIV test confidential is very difficult. Reassuring patients that confidentiality will not be breached does not result in implementing appropriate systems to keep the information secret. It has been found out that that the obligation of confidentiality is some sort of fiction that everybody declares but nobody respects (G³adysz, Juszczyk, & Dubik, 1999).
In this study, more doctors and nurses favoured preoperative HIV antibody testing than testing of all admissions. The difference suggests that for some of them it was unimportant to define the serological status of a non-surgical patient. It is unclear whether surgical personnel perceived other HCW's to be at lower risk, or whether they were simply more concerned about their personal risk than for other HCWs.
Limitations
An anonymous self-reported questionnaire based on recall of events has limitations. In particular, recall may be inaccurate. However, the questionnaires were completed anonymously, which is conducive to obtaining unconstrained opinions. Additionally, the large variety of hospitals was selected for random sampling and 100% response rate was achieved, so doctors and nurses in this report are likely to be representative of other surgical staff in the study area. Secondly, what people say and what they do may be different, so discriminating attitudes resulting in a large numbers of surgical staff supporting preoperative HIV testing of patients may not be translated into discriminatory behaviour. Thirdly, limitations include the small sample size of doctors which may influence the precision of the estimates.
Finally, these results may not be generalized to doctors and nurses from non-surgical wards. The extent to which the results of this study may apply to other parts of the country has to be considered. The West Pomeranian region is characterized by a higher incidence of HIV infection (2.2 per 100,000 population per year) than for Poland as a whole (Rosiñska & Werbiñska, 2004). This may influence Pomeranian doctors' and nurses' perception of their risk for acquiring HIV at work. Thus, desire for preoperative HIV testing may be stronger than in some other regions of Poland.
Recommendations
HIV/AIDS training programmes and practical experience working with known HIV patient positively influenced doctors' attitudes toward mandatory HIV testing and nurses' attitudes toward testing of all admissions, and the combined effect was greater than either alone. Therefore, it is recommended that both effective training in methods to minimise the risk of occupational HIV infection and practical experience working with known HIV patients should be designed and implemented for the surgical staff in the aim of eliminating inappropriate uses of HIV testing.
On the other hand, even many of the trained and experienced doctors and nurses in this survey had not changed their attitudes towards preoperative testing. So, probably, existing education for blood-borne infections should be improved as training and hospital policies may overestimate the real risk for contracting HIV infection in the surgical suite, and the differences between HIV/AIDS and other blood-borne infections may be over-emphasized. It appears that an important component of future educational efforts in this area should be also discussions of ignorance, professional ethics and responsibilities. Information sessions need to be coordinated by the different providers, who can share their personnel and resources to ensure that information is evidence-based. The level of support for pre-operative testing reported in this study was so high among nearly all surgeons and surgical nurses, that even a modest improvement is urgently needed.
For this to occur, hospitals must design properly documented training programmes with appropriate examinations. Such training should be initial and continued, since short-term education does not change values and behaviours (Green & Kreuter, 1991). Both lectures and workshops are needed to help surgical staff see the problem of infection from the perspective of PLWHA. Furthermore, the wider implementation of infection control procedures, as wearing gloves for every procedure involving contact with blood, should be more effective in reducing occupational risk of HIV than routine testing. In eight hospitals surveyed in this study, 17% of active nursing staff did not regularly use gloves.
HCWs have to understand that care of people infected with HIV and suffering from AIDS means not only the need for medical treatment, but must also include approaching patients with respect for their right to autonomy and to decide for themselves, their right to privacy, and their right to not be discriminated against. The stigmatizing character of this disease makes these requirements very important.
References
Brown, L., Macintyre, K., & Trujillo, L. (2003). Interventions to reduce HIV/AIDS stigma: What have we learned? AIDS Education and Prevention, 15, 49-69. [ Links ]
Chapman, K., Meadows, J., Catalan, J., & Gazzard, B. (1995). Testing patients for HIV before surgery: The views of doctors performing surgery. AIDS Care, 7(2), 125-128. [ Links ]
Cherry, K., & Smith, D. (1993). Sometimes I cry: The experience of loneliness for men with AIDS. Health Community, 5, 181-208. [ Links ]
Ciastoñ-Przec³awska, E. (2001). Doctors, nurses and social workers and some HIV/AIDS topics. Poznañ: Wydawnictwo Poznañskie. [ Links ]
Constitution of Poland from 2nd April 1997. (1997). Dziennik Ustaw, no 78, ref. 483. [ Links ]
Damani, N. N. (2003). Manual of infection control procedures (2nd edition). London, UK: Cambridge University Press. [ Links ]
Danziger, R., Abel, P., Goddard, N., McGrouther, D. A., & Pawson, M. E. (1996). Preoperative testing for HIV: A survey of surgeons` attitudes and practices.Lancet, 348, 1036-1037. [ Links ]
European Convention for Protection of Human Rights and Fundamental Freedoms. Retrieved December 15, 2005, from http://www.pfc.org./uk/legal /echrtext.htm [ Links ]
Foreman, M., Lyra, P., & Breinbauer, C. (2003). Understanding and responding to HIV/AIDS related stigma and discrimination in the health sector. Washington DC: Pan American Health Organization. [ Links ]
Gallop, R. M., Lancee, W. J., & Taerk, G. (1991). The knowledge, attitudes and concerns if hospital staff about AIDS. Canadian Journal of Public Health, 82, 409-412. [ Links ]
Gañczak, M., Boroñ-Kaczmarska, A., Leszczyszyn-Pynka, M., & Szych, Z. (2005). Polish adolescents and their beliefs and attitudes to HIV/AIDS and sexual relationships. Sex Education, 5, 1-14. [ Links ]
Gañczak, M., Milona, M., & Szych, Z. (in press). Nurses and occupational exposures to blood-borne viruses.Infection Control and Hospital Epidemiology. [ Links ]
Gañczak, M., & Szych, Z. (2004). Surgeons and their concerns of acquiring HIV infection. Ortopedia Traumatologia i Rehabilitacja, 6(Suppl. 1), 134. [ Links ]
Gerberding, J. L., Lewis, F. R., & Schecter, W. P. (1995). Are universal precautions realistic? The Surgical Clinics of North America, 75, 1091-1104. [ Links ]
Gerberding, J. L., Littell, C., & Tarkington, A. (1990). Risk of exposure of surgical personnel to patients` blood during surgery at San Francisco General Hospital. New England Journal of Medicine, 322, 1788-1793. [ Links ]
G³adysz, A., Juszczyk, J., & Dubik, A. (1999). Pre and post-testing counseling (2nd ed.). Wroc³aw: Volumed. [ Links ]
Green, L., & Kreuter, M. (1991). Health promotion planning: An educational approach. London, England: Mayfield. [ Links ]
Highriter, M. E., Tessaro, I., & Randall-David, E. (1995). HIV-related concerns and educational needs of public health nurses in a rural state. Public Health Nursing, 12, 324-334. [ Links ]
Hoffman-Terry, M., Rhodes, L. V., & Reed, J. F. (1992). Impact of HIV on Medical and Surgical Residents. Archives of Internal Medicine, 152, 1788-1796. [ Links ]
Imperato, A. M. (1996). AIDS and suburban adolescents: Knowledge, attitudes, behaviours & risks. Journal of Community Health, 2, 329-347. [ Links ]
Izdebski, Z. (2000). HIV/AIDS knowledge and social attitudes in Poland. Sexual behaviours. Warsaw, Poland: Wydawnictwo Naukowe PWN i UNAIDS. [ Links ]
Izdebski, Z. (2003). Society's knowledge about HIV/AIDS. Voluntary counselling and testing. HIV & AIDS Review, 2, 15-21. [ Links ]
Joint Working Party of the Hospital Infection Society and the Surgical Infection Study Group (1992). Risk to Surgeons from HIV and hepatitis: Guidelines on precautions and management of exposure to blood or body fluids. British Medical Journal, 305, 1305-1337. [ Links ]
Juszczyk, J. (1995). Should all patents admitted to the hospital be routinely screened for HIV? Seksuologia, 3-4, 42-51. [ Links ]
Juszczyk, J., & G³adysz, A. (1999). AIDS - epidemiology and prevention. Wroc³aw: Volumed. [ Links ]
LifeSite. (2005, October). Candidate for Prime Minister of Poland says homosexuality "Unnatural". Retrieved April 11, 2005 from http://www.lifesite.net/ldn/2005/oct/05100408.html [ Links ]
Lowenfels, A. B, Wormser, G. P., & Jain R. (1989). Frequency of puncture injuries in surgeons and estimated risk of HIV infection. Archives of Surgery, 124, 1284-1286. [ Links ]
Malinowska-Sempruch, K. (1997). Voices of people living with HIV. Warsaw, Poland: UNDP. [ Links ]
Medical Care Centers Act from 30th August 1997. (1997). Dziennik Ustaw, no 91, ref. 408. [ Links ]
Ministry of Health and Social Welfare (1998). Transformacja systemu ochrony zdrowia w Polsce. Warsaw, Poland: Author. [ Links ]
National Institute of Hygiene. (2005). HIV and AIDS in Poland. Retrieved September 30, 2005, from www.pzh.gov.pl [ Links ]
National Program for HIV Prevention & Care for People Living with HIV and Having AIDS: 2004-2006. (2004). Warsaw, Poland: Polish Ministry of Health & National AIDS Center. [ Links ]
Obi, S. N., Waboso, P., & Ozumba, B. C. (2005). HIV/AIDS: Occupational risk, attitude and behavior of surgeons in southeast Nigeria. International Journal of STD & AIDS, 16, 370-373. [ Links ]
Oerman, M. H., & Gignac, D. (1991). Knowledge and attitudes about AIDS among Canadian nursing students: Educational implications.Journal of Nursing Education, 30, 217-221. [ Links ]
Office of the High Commissioner for Human Rights, Geneva, Switzerland. (2005). International Covenant on Civil and Political Rights. Retrieved October 18, 2005, from http://www.unhchr.ch/ html/menu3/b/accpr.htm [ Links ]
Owotade, F. J., Ogunbodede, E. O., & Sowande, O. A. (2003). HIV/AIDS pandemic and surgical practice in a Nigerian teaching hospital. Tropical Doctor, 33, 194-196. [ Links ]
Patterson, J. M., Novak, C. B., & Mackinnon, S. E. (1998). Surgeons` Concern and Practices of Protection Against Blood-borne Pathogens. Annals of Surgery, 228, 266-272. [ Links ]
Polish Act on the Physician's Profession from 5th December 1996. (1997). Dziennik Ustaw, no 28, ref. 152. [ Links ]
Polish Medical Code of Ethics. (1993). Retrieved from http://www.portalmed.pl /xml/prawo/ medycyna/ komentarze/etyka/kodeks [ Links ]
Rea, D., Brown, Y., & Calder, B. (1992). Nurses' knowledge about and attitudes toward patients with AIDS. Journal of Continuing Education in Nursing, 23, 69-75. [ Links ]
Recommendations for Medical Staff. (1997). Warsaw, Poland: The National AIDS Affairs Coordinating Office. [ Links ]
Rosiñska, M., & Werbiñska, B. (2004). AIDS and HIV infection in Poland in 2002. Przegl¹d Epidemiologiczny, 58,171-179. [ Links ]
Shanson, D. C. (1991). Should patients be screened for HIV? Journal of Hospital Infection, 18(Suppl. A), 170-176. [ Links ]
Shapiro, M. F., Hayward, R. A., Guillemot, D., & Jayle, D. (1992). Residents' experiences in, attitudes toward, the care of persons with AIDS in Canada, France, and the United States. JAMA, 268, 510-515. [ Links ]
Sobeyko, J. (2003). Role of human rights in medical care of HIV infected patients. HIV & AIDS Review, 2, 5-8. [ Links ]
Sontag, S. (1988). AIDS and its metaphors. New York, USA: Farrar, Strauss & Girroux. [ Links ]
Staugard, F. (2000). Recommendations related to HIV prevention strategies among men who have sex with men (pp. 92-93). Report from Regional Conference "Together against AIDS", Malmo, Sweden. [ Links ]
Taylor, B. (2001). HIV, stigma and health: Integration of theoretical concepts and the lived experiences of individuals. Journal of Advanced Nursing, 35, 792-798. [ Links ]
Tyndall, M. V., & Schechter, M. T. (2000). HIV testing of patients: Let's waive the waiver. Canadian Medical Association Journal, 162, 210-211. [ Links ]
van Wiessen, K., & Woodman, K. (1994). Nurses' attitudes and concerns to HIV/AIDS: A focus group approach. Journal of Advanced Nursing, 20, 1141-1147. [ Links ]
World Health Organization. (2000). HIV and the Workplace and Universal Precautions. Fact Sheet 11.Retrieved February 17, 2004, from http://www3.who.int/whosis/factsheets -hiv-nurses/fact-sheet-11 [ Links ]
Woynarowska, B., Szymañska, M. M., & Mazur, J. (1999). Health of school-aged children in Poland. HIV/AIDS knowledge, beliefs and sexual behavior. Warsaw, Poland: Warsaw University Press. [ Links ]
Wright, J., & McGeer, A. (1993). HIV transmission between surgeons and patients in orthopaedic surgery. Clinical Orthopaedic Related Research, 297, 272-281. [ Links ]
Wright, J. G., Young, N. L., & Stephens, D. (1995). Reported use of strategies by surgeons to prevent transmission of blood-borne diseases. Canadian Medical Association Journal, 152, 1089-1095. [ Links ]
Maria Gañczak (Poland). M.D. and is a professor at the Pomeranian Medical University, Faculty of Health Sciences, Department of Hygiene, Epidemiology and Public Health, Szczecin, Poland. Her research interests include epidemiology and prevention of sharp injuries among health care workers, and prevention of HIV infection among adolescents. E-mail: mganczak@sci.pam.szczecin.pl
1 Dirección: mganczak@sci.pam.szczecin.pl













