Services on Demand
article
Indicators
Share
Journal of Human Growth and Development
Print version ISSN 0104-1282
Rev. bras. crescimento desenvolv. hum. vol.23 no.1 São Paulo 2013
ORIGINAL RESEARCH
Stress in children and adolescents with asthma
Marco Aurélio MendesI; Clemax Couto Sant'AnnaII; Maria de Fátima Bazhuni Pombo MarchIII
IGraduate program in Clinical Medicine of the Federal University of Rio de Janeiro (UFRJ) School of Medicine
IIAssociate Professor of Pediatrics of the Federal University of Rio de Janeiro
IIIAssociate Professor of Pediatrics of the Federal University of Rio de Janeiro
ABSTRACT
OBJECTIVE: to evaluate stress in children and adolescents with asthma and its association with clinical and psychosocial features.
METHODS: cross-sectional study conducted with asthmatic children and adolescents between 7 and 12 years old, seen at the pediatric pulmonary outpatient clinic. The Stress Childhood Scale, the Criterion of Economic Classification Brazil and a questionnaire were used to collect data. Statistical analysis was realized using the Chi-square Test, ROC curve, Fisher Test and Mann-Whitney. A logistic regression analysis model was used after univariety analysis.
RESULTS: stress was detected in 38 % (19/50) of the patients, with predominance of psychological reactions. Statistical significance associations were found between stress and scholar difficulties, socioeconomic class C2 and D (p = 0,013) and asthma symptoms in a period less than or equal to 7 years (p = 0,003). These associations remained after logistic regression model. There was no statistical significance association between asthma gravity and stress.
CONCLUSIONS: more than one-third of children and adolescents with asthma were stressed. This rate was higher in lower socioeconomic classes and in those patients with scholar difficulties and with symptoms of asthma in a period less than or equal to 7 years.
Key words: psychological stress; physiological stress; asthma; quality of life; affective symptoms.
INTRODUCTION
Asthma is a chronic inflammatory disease of the airways which is often reversible, either spontaneously or through treatment. It is characterized by bronchial hyperresponsiveness (BH) and variable air flow limitation1.
According to the World Health Organization (WHO), there are approximately 235 million people with asthma around the world, and asthma is considered the most common chronic disease in children2. In Brazil, 110,245 children younger than 14 years were hospitalized with asthma in public hospitals (Unified Healthcare System, SUS) in 20103.
Stress is a complex response of the body involving physical and psychological reactions, and occurs when individuals need to adapt to situations and events that threaten their physical and mental stability. When stress is intense or long-lasting, it may cause physiological changes that promote the manifestation of many symptoms and diseases. Stress is not only an immediate reaction but also a process that develops over time. It involves external factors, such as environmental events or changes, and internal factors, such as disposition, stance and beliefs. The dissemination of the term stress in the scientific community and general society is attributed to the endocrinologist Hans Selye4.
The association between asthma and emotional factors was observed a long time ago, passing by Hipocrates, William Osler and by the psychoanalytical references of the classic psychosomatic medicine. After the second half of the Twentieth Century, the concept of atopy, the important role of allergens and genetic susceptibility started to dominate the attention of the researchers of the field. However, what is known today about asthma does not explain the high global prevalence of the disease, increasing the attention given to emotional and psychosocial factors and encouraging a greater number of studies describing associations between stress and asthma5.
In children and adolescents, depressive characteristics such as irritability, tiredness and apathy, as well as anxiety, abdominal pain, nightmares, aggressiveness and learning difficulties are some of the most common stress symptoms. Moreover, complications inherent to the treatment of a chronic disease, such as asthma, may lead to parental overprotection, which then generates inappropriateness and vulnerability, and favors the stress response6. Stress in children with asthma may affect their quality of life, adherence to treatment and treatment success7.
The association between stress and high levels of cortisol was painstakingly studied by Hans Selye and high cortisol became practically synonymous of stress in the scientific literature. This association began to change after the studies that found hypocortisolism in patients with post-traumatic stress disorder (PTSD) and later, in patients with chronic stress, chronic stress syndrome, fibromyalgia, pelvic pain and asthma8,9.
In Brazil, there are few studies about childhood stress, which is commonly neglected by health professionals and families10.
The objectives of this study are to verify the presence of stress in children and adolescents with asthma and assess the association between stress and clinical and psychosocial variables.
METHODS
This is an observational, cross-sectional and descriptive study done with 50 children and adolescents with asthma followed at pneumology outpatient clinic of the Federal University of Rio de Janeiro (UFRJ), Institute of Puericulture and Pediatrics Martagão Gesteira (IPPMG) from May 2010 to August 2011.
The parents and patients were invited to participate in the study before any care was provided. The caregivers signed a free and informed consent form and the researcher clarified all their doubts. Patients aged more than 10 years signed an assent form.
The term caregiver in this study refers to the unremunerated person mainly responsible for the participant at home and who lives in the same home as the participant11.
As proposed by the WHO, participants aged < 10 years are defined as children and those aged between 10 and 19 years as adolescents12.
The inclusion criteria were: have a diagnosis of asthma confirmed by a physician of the pneumology outpatient clinic and age between 7 and 12 years. The exclusion criteria were: having other chronic diseases, having been hospitalized in the previous three weeks, cognitive impairment or inability to answer the study instruments.
The sample size was calculated by assuming the stress prevalence of 23.7% reported by a study on children with asthma10. The desired accuracy was 20% and the significance level 5%, resulting in a minimum sample size of 17 patients.
The study instruments are described below.
Childhood stress scale (CSS)
The CSS consists of a five-point Likert scale with 35 items which is filled out by the patient. It aims to assess the presence of stress in individuals aged 6 to 14 years. It was developed by Lipp and Lucarelli in 1997, revised in 2004 and approved by the Psychological Test Assessment System (SATEPSI) of the Brazilian Federal Council of Psychology (CFP)13. It is a simple instrument and takes about 15 minutes to complete, which can also be done by illiterate individuals.
The CSS is divided into four stress response-related factors: physical reactions (example, item 12 - "I have diarrhea."); psychological reactions (example, item 5 - "I worry about bad things that may happen."); psychological reactions with depressive component (example, item 13 - "I have little energy to do things."); psychophysiological reactions (example, item 1 - "I cannot sit still and am always doing different things.")13.
Economic classification criterion - Brazil (CCEB-2008)
The CCEB-2008 of the Brazilian Association of Research Companies (ABEP) was used for determining the socioeconomic classes of the sample. Socioeconomic class is determined by adding the points given to household items and characteristics, as well as the education level of the head of family. Eight classes are possible, listed in descending order: A1, A2, B1, B2, C1, C2, D and E14.
Standard questionnaire
A standardized questionnaire was used for interviewing the caregiver about the family and the child. The following variables were collected: child's age and gender, caregiver's age, number of people in the household ("How many people live at your home?"), home ownership status ("Is the home yours, rented or borrowed?", employment status of the caregiver ("Do you have a job?"), and school performance ("Has your child ever repeated a grade? Does s/he have any difficulty in school?"), school grade, asthma classification based on the Brazilian Guidelines for the Management of Asthma1 (intermittent, mild persistent, moderate persistent, severe persistent), presence of allergens in the household (affirmative answ er to any of the following questions: "Are there smokers in your home? Pets? Mold on walls, carpets, clothes or bed sheets?"), and time since diagnosis ("When did you notice your child had asthma?").
Statistical analysis
The statistical analyses were done by the software SPSS version 17.0. Numerical data were expressed as measures of central tendency (mean and median). Variability was verified by calculating the standard deviation (SD). The categorical data were expressed as frequency (n) and percentage (%). The significance level was set to 5%.
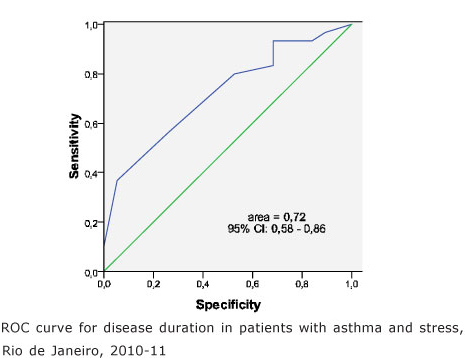
The chi-square, Fisher's exact and Mann-Whitney tests were used for verifying possible statistically significant associations. The variables chosen for the logistic regression model were those with statistical significance in the descriptive analysis and those considered by the literature as clinically relevant for childhood stress and asthma. The receiver operating characteristic (ROC) curve was constructed to find a cut-off point for the association between childhood stress and asthma symptom duration.
Ethical aspects
The study was approved by the IPPMG/UFRJ Research Ethics Committee under protocol number 02/09, on July 14, 2009.
The children and adolescents with stress according to the CSS were sent to the IPPMG Psychology Service. Their caregivers were given the phone numbers of the free applied psychology and psychotherapy services of Rio de Janeiro. The caregivers were informed about the importance of going to a psychologist for helping the child to manage stress.
RESULTS
Fifty patients with asthma aged 7 to 12 years and their caregivers were studied. Most (58%, 29/50) patients were females. The mean age of the sample was 9.26 (SD=1.63).
The mean age of the caregivers was 36.89 years (SD=8.41), and the median age was 36. Most caregivers (54%, 27/50) were formally or informally employed and 46% (23/50) were housewives. Most families (58%, 29/50) consisted of both parents living together; 78% (39/50) lived in their own homes and 80% (40/50) had five or less people living in the household. According to the CCEB18 criteria, 40% (20/50) belonged to the class C1; 24% (12/50) to the class C2; 22% (11/50) to the class D and 14 % (7/50) to the class B2.
The study sought to determine the cut-off point that best discriminated the association between disease duration and stress. According to the ROC curve, the best cut-off point was 7 years, with an area under the curve of 0.72 (95%CI: 0.58-0.86), as shown by Figure 1.
The variables were grouped for verifying associations with stress (Table 1). The variables school performance, socioeconomic class and symptom duration were associated with stress.
Logistic regression was used for selecting the best predictors of childhood stress (Table 2). The following variables were considered possible risk factors: being female, poor school performance, low socioeconomic class, moderate to severe persistent asthma, 7 years of less since diagnosis and presence of smokers in the household. The associated variables listed in Table 1 continued to be associated after logistic regression.
The scores of the CSS factors were, respectively: mean 21.68 (SD=5.01) - psychological reactions; mean 14.58 (SD=3.41) - psychophysiological reactions; mean 12.68 (SD=6.49) - psyTchological reactions with depressive component; mean 12 (SD= 4.93) - physical reactions.
DISCUSSION
Clinicians are aware of the relationship between negative life experiences and exacerbation of asthma. Severe negative events in the lives of children with asthma, especially when accompanied by chronic stressors such as poverty, and alcoholism and mental illness in the family, among others, increase the probability of new exacerbations of asthma15.
Chen and Miller9 developed a model based on the hypocortisolism hypothesis to explain the paradox between asthma and stress. The chronic stress process not only reduces the number of cortisol receptors but also reduces their sensitivity, and the result is greater resistance to the anti-inflammatory properties of glucocorticoids. The same down-regulation process occurs with prolonged exposure to high levels of epinephrine and norepinephrine, which leads to the down-regulation of the adrenergic receptors in the lungs and lymphoid tissues, increasing the expression of Th2 lymphocytes that produce cytokines related to the onset and continuation of the inflammatory process.
The results found by the present study show a high rate of stress in children and adolescents with asthma, higher than those found by studies with schoolchildren using the CSS in Brazil16,17, and higher than that of the only study found that administers the CSS to patients with asthma10.
Belonging to a low socioeconomic class (C2+D), poor school performance and disease symptoms for seven years or less were associated with childhood stress.
Given that children with intermittent and mild persistent asthma visit the emergency room less frequently than those with moderate and severe persistent asthma, intermittent asthma was grouped with mild persistent asthma and moderate persistent asthma was grouped with severe persistent asthma. No significant associations were found between asthma severity and stress. The association between childhood stress and asthma severity is controversial in the literature9. Calam, Gregg and Goodman18 showed that children with asthma in good health were not at risk of developing psychological disorders, contrary to those with poor health. Emotional hardships were related with poor health and not only with asthma. Bussing et al.19 found a greater prevalence of anxiety disorders in children with asthma. Stress was not found to be significantly associated with gender, despite the literature reports of a higher rate of stress in girls10.
Poor school performance was more common in the group with asthma and stress (p=0.026). This association is not consensual in the literature, probably because of the different ways of conceiving and measuring the problem20.
School absenteeism secondary to the disease and constant medical visits may prevent the child from keeping up at school, developing abstract thought, organizing notebooks and school material and learning13,10,20. The fear of infecting a child because of the disease floods the imagination of the child, facilitating the development of anxiety, which in turn may further hinder school performance21.
Patients with shorter time since diagnosis or since the onset of the first asthma symptoms were more stressed than those who had been dealing with the disease for a longer period, which is in agreement with Berenchtein10. The existence of this specific factor of adaptation to the disease found by the present study is reinforced by the absence of associations between age and stress (p=0.812). The child's and adolescent's knowledge about asthma acquired by experience with the disease over time may facilitate the management of the symptoms and lead to better predictability and control, resulting in a smaller impact on emotional and physical health. The more patients and families know about their condition, the less anxious they are and the more likely to adopt lifestyles compatible with the disease22.
The cognitive behavioral model is increasingly relevant for the treatment of chronic diseases, psychological wellbeing of patients, adherence to treatment and treatment success23. The emphasis of the model on being informed about the disease and the role of individual interpretations of reality may help children and adolescents with asthma to know more about the disease, promoting faster adaptation and developing autonomy.
Stress was not found to be associated with the variables age group and school grade, but 26.3% of the stressed patients were aged 7 to 8 years and most of them were in the early grades of elementary school. Starting school is a crucial moment for the child with asthma. The restrictions imposed by the disease, such as avoiding running, jumping, physical activity, or even the social exposure resultant from symptom manifestation, such as tiredness and coughing, may lead to socialization difficulties and isolation, making the asthmatic child feel excluded and often different from everyone else21. This opens the way for feelings such as shame, excessive shyness, and irritability, among others, which are common in children with stress.
Alati et al.12 studied data from 5135 children and adolescents from an Australian cohort and found that asthma in children aged 5 to 14 years was associated with internalizing behavior problems, such as anxiety, depression, isolation and somatic complaints. Asthma at age five years was also a significant risk factor for the presence of teenage behavior problems. Feitosa et al.24 studied 869 Brazilian children aged 6 to 12 years from the city of Salvador and found a greater prevalence of behavior problems in asthmatic children than in non-asthmatic children.
Smokers and allergens were present in the households of a significant number of study participants, indicating parental resistance or inability to adopt environmental control practices that improve the disease. The presence of smokers, mold and animals, associated or separately, were not related to stress. Although environmental control is still considered an important component for controlling asthma and, consequently, other disease-related variables, its importance is currently being questioned5.
Patients belonging to lower socioeconomic classes were more stressed than those of higher classes. This finding suggests the opportunity of creating programs specifically for these children and their families. Adherence to treatment, so very necessary in the case of chronic diseases like asthma, is often hindered because of financial difficulties that stem not only from the need of medication but also from the cost of reorganizing the household to reduce exposure to factors that possibly trigger attacks22,25.
Despite the relevance of the present results, it is possible that new studies with larger sample sizes that investigate caregiver stress will shed new light on the theme, since the literature shows a probable association between caregiver stress and children and adolescents with chronic diseases26.
The poor school performance of asthmatic children with stress indicates the need of a multidisciplinary intervention which includes professional education. The attention given to asthmatic patients in the early grades of elementary school and recent asthma diagnosis needs to be doubled.
The human development process results from the interaction of biological, social and cultural factors. Children, their families, their environments and their historical timing must be seen holistically, with psychism being the organizing core of these different aspects27,28. The high prevalence of stress found by the present study calls attention to the impact that emotional factors have on the daily lives of children and adolescents with asthma, and suggests interventions and public policy programs that take these factors into account and the inclusion of a psychologist in healthcare teams.
REFERENCES
1. IV Diretrizes Brasileiras para o Manejo da Asma, J Bras Pneumol. 2006; 32 Suppl : S447-74. [ Links ]
2. WHO World Health Organization. Asthma. [Internet]. [citado 2011 Set 5]. Disponível em: http://www.who.int/mediacentre/factsheets/fs307/en/index.html . Acesso: 05/09/2011. [ Links ]
3. Brasil Ministério da Saúde [Internet]. Indicadores de morbidade hospitalar do SUS. [citado 2013 Jan 1] Disponível em: http://www. datasus.gov.br. [ Links ]
4. Lipp, MEN. Manual do inventário de sintomas de stress para adultos de Lipp (ISSL). São Paulo: Casa do psicólogo; 2005: 10-4. [ Links ]
5. Douwes J, Brooks C, Pearce N. Asthma nervosa: old concept, new insights. Eur Respir J. 2011; v. 37: 986 - 90. [ Links ]
6. Lipp, MEN. Crianças estressadas: causas, sintomas e soluções. São Paulo: Papirus; 2000: 3- 63. [ Links ]
7. Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in children with asthma. Qual Life Res. 1996; 5:35-46. [ Links ]
8. Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneu-roendocrinology, 2000; v. 25: 1-35. [ Links ]
9. Chen E, Miller GE.Stress and inflammation in exacerbations of asthma. Brain , Behavior and Immunity, 2007;v. 21: 993-7. [ Links ]
10. Berenchtein B. A influência do stress na expressão clínica da asma infantil [dissertação]. São Bernardo do Campo: Universidade Metodista de São Paulo; 2004. [ Links ]
11. Fonseca NR, Penna AFG.Perfil do cuidador familiar do paciente com seqüela de acidente vascular encefálico.Ciência & Saúde Coletiva, 2008; 13 (4): 1175-1180. [ Links ]
12. Alati R, O'callaghan M, Najman JM, Williams GM, Bor W, Lawlor DA. Asthma and internalizing behavior problems in adolescence: alongitudinal study. Psychosomatic Medicine, 2005; v. 67: 462 - 70. [ Links ]
13. Lipp, MEN, Lucarelli MDV. Escala de stress infantil - ESI: manual. São Paulo: Casa do psicólogo; 2005: 8-45. [ Links ]
14. Critério Padrão de Classificação Econômica Brasil/2008. ABEP_Associação Brasileira de Empresas de Pesquisas. Disponível em http://www.abep.org. Acesso em: 25/10/2011. [ Links ]
15. Sandberg S, Paton JY, Ahola S, McCann DC, McGuinness D, Hillary CR et al.The role of acute and chronic stress in asthma attacks in children. Lancet 2000; 356 : 982 - 87. [ Links ]
16. Sbaraini CR, Schermann LB. Prevalência de estresse infantil e fatores associados: um estudo com escolares em uma cidade do Estado do Rio Grande do Sul, Brasil. Cad. Saúde Pública (Rio J). 2008; 24(5) : 1082-88. [ Links ]
17. Lipp MEN, Arantes JP, Buriti MS, Witzig T. O estresse em escolares. Psicologia Escolar e Educacional 2002; 6 (11): 51-6. [ Links ]
18. Calam R, Gregg L, Goodman R. Psychological adjustment and asthma in children and adolescents : the UK nationwide mental health survey. Psychosomatic Medicine 2005; 67 : 105 - 10. [ Links ]
19. Bussing R, Burket RC, Kelleher ET. Prevalence of anxiety disorders in a clinic-based sample of pediatric asthma patients. Psychossomatics 1996; 37 (2): 108-15. [ Links ]
20. Gustadt LB, Gillette JY, Mzarek DA, Fukuhara JT, LaBrecque JF, Strunk RC. Determinants of school performance in children with chronic asthma. Am. J. Dis. Child. 1989; 143(4) : 471-5. [ Links ]
21. Trinca MA, Bicudo IMB, Pelicioni MCF. A interferência da asma no cotidiano das crianças. Rev Bras Crescimento Desenvolvimento Hum. 2011; 21 (1): 70-84. [ Links ]
22. Vieira MA, Lima RAG. Crianças e adolescentes com doença crônica: convivendo com mudanças. Rev Latino-am Enfermagem 2002; 10(4): 552-60. [ Links ]
23. White, CA. Cogntive behavioral principles in managing chronic disease. WJM, 2001; 175: 338-42 [ Links ]
24. Feitosa CA, Santos DN, Carmo MBB, Santos LM, Telesc CAS,Rodrigues LC et al. Behavior problems and prevalence of asthma symptoms among Brazilian children. J Psychosom Res., 2011. 71(3): 160 - 5. [ Links ]
25. Mendonça MB, Ferreira EAP. Adesão ao tratamento da asma na infância : dificuldades enfrentadas por cuidadoras. Rev Bras Crescimento Desenvolvimento Hum. 2005; 15(1): 56-68. [ Links ]
26. Castro EK, Piccinini CA. Implicações da doença orgânica na infância para as relações familiares: algumas questões teóricas. Psicologia: Reflexão e Crítica, 2002; 15 (3) : 625-635. [ Links ]
27. Abreu LC. Heart rate variability as a functional marker of development. J. Hum. Growth Dev. 2013: 22(3): 279-282. [ Links ]
28. Brasil, Ministério da Saúde. Secretaria de Políticas de Saúde. Departamento de Atenção Básica. Saúde da criança: acompanhamento do crescimento e desenvolvimento infantil / Mi [ Links ]
 Correspondence to:
Correspondence to:
marcs@terra.com.br
Manuscript submitted Jun 06 2012,
Accepted for publication Nov 28 2012
Study done at the pneumology outpatient clinic of the Institute of Puericulture and Pediatrics Martagão Gesteira (IPPMG). Rua Bruno Lobo, 50, 20 andar. CEP 21941-590, Cidade Universitária, Campus do Fundão, Rio de Janeiro, RJ.












 Curriculum ScienTI
Curriculum ScienTI
