Services on Demand
article
Indicators
Share
Journal of Human Growth and Development
Print version ISSN 0104-1282On-line version ISSN 2175-3598
J. Hum. Growth Dev. vol.32 no.2 Santo André May/Aug. 2022
https://doi.org/10.36311/jhgd.v32.11909
ORIGINAL ARTICLE
Self-compassion and positive and negative affects on medical students during the COVID-19 pandemic
Camila de Franco TobarI; Maikon MichelsII; Selma Cristina FrancoIII
IEstudante do quinto ano do Curso de Psicologia da Universidade da Região de Joinville -UNIVILLE - Joinville - SC - Brasil
IIDocente do curso de Psicologia da Universidade da Região de Joinville - UNIVILLE - Joinville - SC - Brasil
IIIDocente do curso de Medicina da Universidade da Região de Joinville - UNIVILLE - Joinville - SC - Brasil
ABSTRACT
INTRODUCTION: studies demonstrate a higher rate of anxiety, depression and stress symptoms among Medical students when compared to the general population. The context of the coronavirus pandemic (SARS-CoV-2) generated additional stress to these students
OBJECTIVE: the present study aimed to evaluate the emotional health of medical students at a Community University
METHODS: there were 437 participants, that answered a sociodemographic questionaire, the Positive and Negative Affect Schedule (PANAS) and the Scale of Self-compassion - Brazil
RESULTS: most (69%) are female, 63% live with their family, 35% have student loans, 59% practice some religion, 45% reported a diagnosis of psychological disorder, 27% use psychiatric medication and 9% use of psychoactive substances. More than 72% of women and 58% of men, presented scores of positive affects (PA), negative affects (NA), and self-compassion (SC) that were below the population mean. The report of psychological disorders and use of psychiatric drugs were also found to be significantly associated to lower rates of PA (respectively, p<0,0001 and p=0,030) and SC (p<0,001 in both) and higher rates of NA (p<0,001 in both
CONCLUSION: the results point to greater vulnerability of the psychological health of medical students during the pandemic and indicate the importance of adopting measures aimed at emotional well-being at the institutional level
Keywords: COVID-19, medical students, mental health, compassion.
Authors summary
Why was this study done?
Characteristics of medical training generate a strong stress load that can contribute to student's physical and psychological illness, which is aggravated by the context of the Covid- 19 pandemic. Considering that future professionals will soon be caring for the population, knowledge about the emotional health of medical students can support training institutions in implementing projects to mitigate such problems.
What did the researchers do and find?
A descriptive and exploratory study was carried out among 437 medical students from a community institution with the application of a sociodemographic questionnaire, Positive and Negative Affect Schedule (PANAS) and Self-Compassion Scale - Brazil. Students showed scores of positive affect (PA), negative affect (NA), and self-compassion (SC) lower than the population average, indicating difficulties to face situations that generate stress and less resilience. An association was also observed between the analyzed indexes and the report of psychological disorders and the use of psychiatric medications by the students.
What do these findings mean?
PA, NA, and SC scores lower than the population mean to point to greater vulnerability of medical students' psychological health during the pandemic and indicate the importance of adopting measures aimed at emotional well-being at the institutional level.
INTRODUCTION
The Medicine course is one of the hardest to get in, and also one of the most demanding. Besides the high academic workload, the training requires full-time dedication considering the study days, internships, and extracurricular activities. These factors, added to the growing awareness of the problems existing in the medical profession, a competitive environment among colleagues, financial concerns, and all the routines involved, generate a strong stress load that can contribute to the physical and psychological illness of students1,2.
Studies indicate a higher rate of anxiety and depression symptoms among medical students when compared to the general population2-5. Furthermore, research in Brazil and the USA indicate that the peculiarities of medical courses favor the development of burnout syndrome6,7. An aggravating factor for this situation is the use of psychoactive substances, which is higher among medical students when compared to students in other health courses and the general population8-10.
These aspects added to the current context of the new Coronavirus pandemic (SARS- CoV-2) generate an additional burden of anxiety and stress. The still incipient scientific knowledge about the virus and the ways to fight it is one of the greatest challenges worldwide today.
The need for isolation or social distancing and adherence to quarantine practices has generated economic, social, and psychological impacts. The numerous risk factors related to infection by the virus range from morbidities to social and family issues11. The uncertainty about the future and the mourning for the losses involved, either by facing the death of loved ones or even the loss of freedom, are generating emotional impacts on a large scale. Studies already point to increased reports of feelings like anger, fear, frustration, boredom, and confusion12.
In this context, medical students in the early stages of the course must deal with long hours in virtual classes, little contact, and interaction with classmates and professors. Students in the pre-clinical phase were early involved in attending the population in telephone triage/ triage centers, and those in the internship phase went on to see patients, following an entire biosafety protocol.
The concern for students' emotional well-being becomes more relevant in this scenario. One way to measure the emotional dimension of subjective well-being is through positive affect and negative affect. Positive affects (PA) consist of states of pleasant involvement and reflect how excited, active, and alert a person feels. Their low level would indicate states of sadness and lethargy13. Negative affects (NA), reflect a state of distress and unpleasant involvement, including a variety of aversive mood states such as anger, fear, and nervousness. A low level of AN would be indicative of tranquility and serenity13.
These constructs of subjective well-being are also related to self-compassion (SC)14. Studies point out that SC is positively related to positive affect and negatively related to negative affect14-17 and is associated with psychological health and emotional well-being18.
Self-compassion can be defined in various ways. Neff19 defines self-compassion based on three elements: 1) self-kindness, which involves experiencing feelings of caring and kindness for oneself in a compassionate way and with an impartial attitude toward one's inadequacies and shortcomings; 2) shared humanity, in which we recognize that individual experiences are part of experiences common to all human beings; and 3) mindfulness, which involves being open and engaging with one's suffering in a clear and balanced way.
Compassion at its core involves a motivation to care, the ability to tolerate unpleasant emotions, and the capacity for empathic understanding without judging or condemning20.
Self-compassion is especially important in challenging and unpleasant situations, as it is associated with resilience and stress regulation21. More self-compassionate individuals respond better to unpleasant emotions by adopting a kind and open attitude, as well as understanding that imperfections and difficult experiences are part of life14.
Considering the context of the pandemic by COVID-19 and the characteristics of the medical course, it was verified, the importance of evaluating the emotional reaction of medical students to this scenario, as well as how they deal with their emotional needs in stressful situations.
METHODS
This is a descriptive and exploratory study, carried out at a community college in Santa Catarina.
The participants in the study comprised medical students from the 1st to the 12th semester, who regularly enrolled in the course, totaling 580 students, 63.6% of whom were female. The exclusion criteria included students under 18 years of age, those who did not wish to participate, or those who were absent in class on the day of data collection.
The research was conducted through a structured self-completion questionnaire applied collectively in a virtual classroom environment via GoogleForms. The collection instrument was composed of two parts: a sociodemographic questionnaire (semester of the course, gender, age, residence with family members, student financing, practice of religion, diagnosis of psychological disorder, use of psychiatric medications, and use of psychoactive substances), followed by the psychological scales, the Positive and Negative Affect Schedule and the Self-Compassion Scale.
The Positive and Negative Affect Schedule (PANAS) in its version adapted for Brazil22 is a self-report scale that evaluates the frequency and intensity with which people experience these affects. It is composed of 10 items that assess PA and 10 items that assess NA. The items are made up of adjectives that represent the evaluated affects along with a five-point Likert scale, ranging from "not at all" to "extremely". Respondents are asked to mark the number that indicates how strongly they feel the affects described by the adjectives22. PANAS has demonstrated stable results, reliability, and validity considering an 8-week interval13.
The Self-Compassion Scale (SCS), developed by Neff23, is a self-report scale composed of 26 items that represent the construct Self-Compassion. For each of its 26 phrases or items, the respondent should mark how he/she feels about what he/she reads, indicating his/her preference based on a five-point Likert scale, ranging from "rarely" to "almost always". The scale aims to assess six elements: self-worth, mindfulness, shared humanity, self-criticism, isolation, and over-identification24.
To preserve anonymity, the questionnaires were identified only with the students' enrollment numbers, without their names. Such identification was necessary to allow later feedback to the students and to make possible an eventual intervention at the individual level in special situations identified by the research psychologists. All students present in class on the day the questionnaire was applied were invited to answer it. The applications took place from May 11 to 19, 2020, per class, and lasted approximately 20 minutes each. After the agreement of the teachers, a schedule of times was made for each class during the classes. At this time, classes had only been taking place virtually for two months due to the COVID-19 pandemic. By clicking on the survey link, the participant was taken to the ICF page. The inclusion criterion for the study was that the individual was regularly enrolled in the course and wished to participate in the survey, in which case he/she should click on "Yes, I am over 18 and agree to participate in the survey. If the respondent selected the option "I am under 18" or "I do not wish to participate in the survey", he was automatically taken to the acknowledgment message, ending the form.
Regarding ethical aspects, the study was approved by the university's Research Ethics Committee (CAAE 24711019.2.0000.5366), the course coordinator signed the Consent Form, and the study participants accepted the Informed Consent Form (ICF) on the homepage of the GoogleForms online form.
Data analysis was performed with the aid of the Microsoft Excel 2013 program. First, simple descriptive statistics were generated. The chi-square test was used to compare participants concerning gender. Next, Pearson correlations were obtained between PA, NA, and SC measures. The third step of the analysis involved f-test calculations to verify the similarity of variances, followed by t-tests for comparisons of groups according to sociodemographic and psychological characteristics (gender, living with family, student financing, religious practice, diagnosis of psychological disorder, use of psychiatric medication, and use of psychoactive substances). Three phases in medical school were considered, basic, pre-clinical, and internship, each comprising 4 semesters sequentially. The levels of PA, NA, and SC were classified as below average (0-39 percentile), average (40-60 percentile), and above-average (61-100 percentile). The significance level adopted was 0.05. Effect size via Cohen's d was calculated for group comparisons. Values greater than or equal to 0.8 represent a large effect size; between 0.8 and 0.2 are considered medium and less than 0.2 small. According to the Publication Manual of the American Psychological Association25, it is recommended to measure effect size next to p-value results, since these do not indicate the significance of a difference between groups, but only test data against the null hypothesis. Effect size gives significance to statistical tests and measures the strength of the evidence against the null hypothesis, thus reducing the risk of misinterpretation. Finally, a single-factor analysis of variance (ANOVA) was performed for positive affect (PA), negative affect (NA), and self-compassion (SC) to compare course phases.
RESULTS
Of the 580 students in the course, 135 were absent in class on the day of data collection or did not access the form. Among those present, 4 were excluded from the survey because they were minors, and 4 did not want to participate in the survey, which totaled 437 respondents (75% of the course students). The age range varied from 18 to 42 years, with a mean of 22.92 (SD = 3.78). Of the respondents 69% (n=300) were female and 31% (n=137) were male. The proportion of participants in the survey was higher among females (81%) than males (65%) with a significant difference (p<0.0001).
Considering the socio-demographic data, it was found that: 275 (63%) live with their families; 151 (35%) have student loans; 256 (59%) practice some religion; 196 (45%) reported having a diagnosis of a psychological disorder, 80 (18%) with more than one disorder; 117 (27%) use psychiatric medication, and 40 (9%) use psychoactive substances, and 19 (4%) chose not to answer the question.
The distribution of students by percentile of PA can be seen in figure 1. The results show that 75% of the students are in percentiles considered medium-low or very low for PA by the normative table of the Brazilian population22, with these high percentages already present since the first semesters of the course.
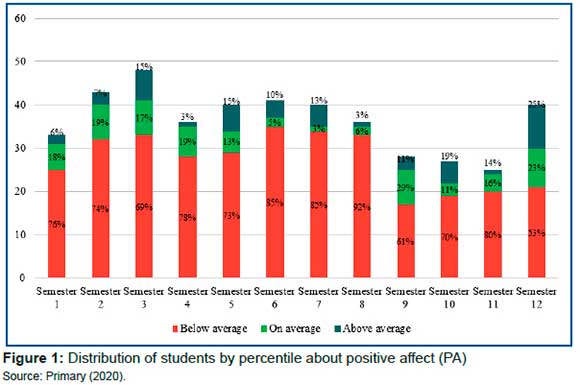
ANOVA group comparisons concerning course phases show oscillations in mean PAs for the three phases, basic education (2.70), preclinical (2.66), and internship (2.98), indicating that after entering the course there is a drop in PAs followed by an increase in them during clinical practice. In women, mean PA scores were higher in the preclinical phase (p=0.006). Among men, there was no such difference (p=0.070). Comparisons for negative affect and self-compassion in the three phases of the course showed no statistically significant differences in both genders.
Considering the average of students classified in the percentiles considered medium-high or high for NA when compared to the general population, it was observed that 53% presented NA above the population normative22, with some oscillations, not significant, in each semester for females (p=0.089) and male (p=0.745) sexes (figure 2).

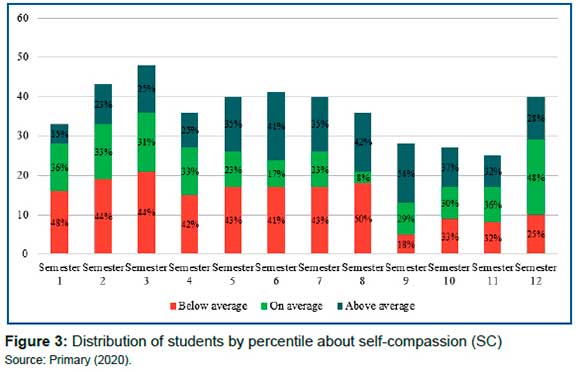
For self-compassion, 39% of the students are in the very low or medium-low percentiles, 29% in the medium, and 32% in the medium-high and high percentiles, according to the population normative24 (figure 3). The fluctuations seen across semesters is not significant for female (p=0.293) and male (p=0.082).
The correlations found between the scales applied for the female population were: PA with NA at r = -0.45 with self-compassion at r = 0.47; and negative affects with self-compassion at r = -0.60. For the male population, the correlations found were: positive affects with negative affects at r = -0.46 and with self-compassion at r = 0.49; and negative affects with self-compassion at r = -0.63. According to Cohen26, these are moderate (0.30 ≥ r ≤ 0.49) and strong (r ≥ 0.50) correlations.
Group comparisons were conducted regarding the means of PA, NA, and SC. The comparison regarding gender showed significant differences in the means of PA (p=0.022) and SC (p=0.007) which were higher among men and those of NA (p<0.001) among women (table 1).
Mean comparisons for PA, NA, and SC for males about social characteristics show an association between the report of psychological disorder and use of psychiatric medication with NA (respectively p<0.001 and p=0.006). No association between these factors was identified between PA and SC. In this group, we also observed a significant association between the practice of religion and PA (p=0.002) (table 2).
For females, we observed a significant association between the no report of psychological disorder and no use of psychiatric drugs with the PA (respectively, p<0.001 and p=0.030) and the SC (p<0.001 in both). An association was also identified between the report of psychological disorder and the use of psychiatric medications with the NAs (p<0.001 in both), according to table 3.
DISCUSSION
The comparison between enrolled academics and survey participants showed a higher proportion of females and a lower proportion of males. Studies using virtual interviews among university students show higher female participation27, with one of the explanations for this being that women are socialized more about connecting with others, which would lead them to be more emotionally connected, while men are socialized in terms of separation and have a more individualistic profile28.
The fact that most students reside with their families and practice some religion is positive since these are factors considered protective for good mental health. Having a religious belief can lead to a more adaptive posture when dealing with stressful events, reducing their negative impact. Additionally, religion can provide a sense of control, comfort, connection to other people, and closeness to a higher power29.
The high percentage of students with a reported diagnosis of psychological disorder (45%) indicates that the emotional health of these students is impaired when compared to the general population. In Brazil, anxiety disorder is present in 9.3% of the general population30 and the lifetime prevalence of depression is around 15.5% in the country31.
Many studies conducted on medical students in Brazil and other countries have reported high rates of psychological disorders2-7, use of medications8,10,32 and of psychoactive substances8-10,33, which added to the characteristics of the course that requires great dedication and commitment from the students produces a stressful environment capable of aggravating their mental health1,2.
This situation is not alleviated after graduation, since the exercise of the medical profession is stressful due to long working hours, sleep deprivation, unhealthy environments, and dealing with disease, suffering, and death, besides involving great visibility and social responsibility34. As a result, rates of psychiatric disorders and suicide are higher than those of the general population35.
The finding that 75% of the students are in percentiles considered medium-low or very low for PA when compared to the general population by the normative table of the PANAS scale22 is indicative of an impairment in the capacity for pleasant involvement. When we separate them by semesters, we observe that students start the course with low PA scores, worsening in the intermediate semesters and improving in the final semesters (figure 1). These findings are in agreement with other studies4,5 that demonstrate higher levels of depression in students in the intermediate years of the medical course.
Some authors29 also point out that during the medical course, there is an increase in the use of tranquilizers, tobacco, and others36, with the same trend for the consumption of alcoholic beverages. The authors suggest that these findings may be related to the fact that the practical activities that start in the fifth year of the course are anxiety-producing33. This final period is considered the most difficult, since it forces the student to fully dedicate himself to training, besides generating expectations about the duties and responsibilities that accompany the medical degree33. The worse PA results in the pre-clinical phase are worrisome since these students have not yet started their internship and are already more vulnerable from a psychological health point of view.
When analyzing the NAs, it is observed that 53% of students demonstrated a state of distress and unpleasant involvement above the population normative22. These PA and NA results are of concern, as they show a greater fragility of the emotional health of future health professionals, and may even cause psychological imbalance, which would be detrimental to the performance of their work37.
The levels of self-compassion follow the same trend as the PA, with better results in the last semesters. This finding indicates that these students are more engaged in self-care and the ability to tolerate unpleasant emotions20, aspects that would facilitate the transition to professional practice from the standpoint of emotional health.
The correlations found between the three scales applied to the female and male populations indicate that improving pleasant states of involvement, by increasing PA, would reflect on aversive mood states, reduce NA, and impact self-compassion to the extent that it is associated with psychological health and emotional well-being18.
The differences between genders found in our research regarding the means of PA, NA, and SC, showing higher levels of PA and SC among men and higher levels of NA among women, reflect gender issues already pointed out in other studies38,39.
In this sense, the social roles of the genders and the social norms of masculinity and femininity act by defining pre-established behaviors, in which the man seeks to fulfill a social expectation about the role he plays, demonstrating strength and security. Women, on the other hand, may express their suffering and vulnerability. Thus, characteristics commonly linked to women include sensitivity, emotionalism, and self-sacrifice, while those linked to men include strength, pragmatism, and independence40. A study by Nevid and Rathus indicates that women who adopt a more feminine role tend to experience stressful situations in a more aversive way and show reduced capacity for overcoming, which would lead them to states of greater distress and unpleasant engagements40.
Crawford and Henry39 indicate that low levels of PA are linked to depressive states and high levels of NA are related both to depressive states and anxiety. The findings of our study found among medical students of both genders mean scores of PA were below the general population mean and NA above the population mean, showing a situation of greater psychological vulnerability for the development of psychological disorders1,2.
The gender issue also permeated the results regarding psychological disorders and the use of psychiatric drugs. In our research, we found an association between these 2 factors NA in male students and PA and SC in female students.
This relationship between PA and NA with psychological disorders was identified in the study by Hofmann, Sawyer, Fang, & Asnaani41. According to the authors, a high level of NA and a low level of PA were associated with mood disorders such as depression and anxiety disorders. Additionally, Barnard and Curry42 indicate that the literature is consistent in stating that SC is inversely related to psychopathologies, with the development of SC reducing depression and anxiety disorders43. SC promotes PA, improving mental health and reducing depression, anxiety, and stress44.
Considering that depressive and anxious conditions and chronic stress lead to alterations in the hypothalamic-pituitary-adrenal axis45, the physiological consequences may cause damage to cognition. Authors46,47 point out that fatigue, difficulty in attention, concentration, and memory lead to a drop in productivity, irritability, aggressiveness, apathy, isolation, and a drop in self-esteem, among others, in such a way that these students may present a functional impairment, which, in turn, may result in learning difficulties.
When we add this drop in performance to factors that are parts of medical training, such as competitiveness, constant pressure, and high study/workloads, this feeds back into a vicious cycle increasing vulnerability to mood disorders2,48 and leads them to use inappropriate compensation mechanisms, such as avoidance or seeking relief through a substance or medication use8-10.
The semesters in which a worsening of emotional health is observed deserve special attention from the pedagogical point of view. One must evaluate what may be triggering this type of situation, if it is the lack of time or leisure time if it is the relationship with the teachers if it is the actual load of activities and tasks, among others.
Among men, we also observed a significant association between the practice of religion and PA (table 2), which supports the idea that religion can generate and/or sustain positive emotional states and maybe a protective factor for mental health. Although no significant differences were detected between men practicing or not practicing religion for the NA and SC, nor for women practicing or not practicing religion for the three constructs, the effect size between the groups was weak, which may indicate that the results are inconclusive.
A study by Lavrič and Flere49 points out cultural differences in the association between religiosity and PA and NA and concludes that there is no pattern of relationship between them. Thus, it is recommended that further studies be conducted to evaluate the relationship between religiosity, PA, NA, and SC in the Brazilian population.
The comparisons between PA, NA, and SC for variables considered protective of psychological health, such as living with the family, having student loans, and using psychoactive substances, did not identify any association in our research, which deserves further investigation to elucidate whether the socio-economic profile of students may have interfered with the results.
This study is unprecedented for investigating the emotional health of medical students during the pandemic of COVID-19 and encompassing both individuals in isolation with distance learning classes and those who were working on the front lines in hospitals and health care facilities. Even with a high adherence of medical students (75%), a limitation of the study is the low percentage of male participants. Another limitation refers to the use of self-report scales that consider the individual perception of each respondent and, therefore, are not as accurate as a clinical evaluation.
CONCLUSION
This study evaluated the levels of positive affect (PA) and negative affect (NA), as well as the level of self-compassion (SC) of medical students at a community college. It can be concluded that regardless of the stage of the course, students had lower emotional health indices and a higher prevalence of mood disorders when compared to the general population.
It can also be observed that students with higher self-compassion scores also had healthier PA and NA scores, which would be indicative of having a greater ability to tolerate unpleasant emotions, tend to be more resilient, and having better emotional balance.
It was observed that students arrive in the first semester with high levels of NA and low levels of PA and that throughout the 12 semesters of the course there is no worsening of these levels, but rather oscillations between semesters. This finding, without a clear pattern, allows us to conclude that the course does not seem to be contributing to the deterioration of the students' mental health. However, it is worth noting the need to repeat the evaluations on the students over the years to have a longitudinal follow-up that would allow more robust statements to be made. The fact that it was conducted in the early phase of the pandemic by COVID-19 may have been an external factor that may have affected the results found.
Professors and course coordinators are advised to be cautious when addressing this topic with students, especially given the stigma surrounding psychological illnesses. Self-perception of feelings of depression or anxiety is associated with weakness and shame, which in turn exacerbate the experience of NA.
The educational institution and the coordination of the medical course should be aware and prepared to offer support and help with stress management, reduction of anxiety and depression symptoms, and development of skills and competencies necessary for the development of greater resilience. It is suggested to focus on actions that seek humanization in the institutional environment and in the health services where students work, with an acceptance of the needs and a more attentive look at the students.
Open communication about mental health, as well as practices aimed at self-care, prevention of mental disorders, and listening to students, are important for early identification of symptoms of chronic stress, anxiety, or depression.
REFERENCES
1.Millan LR, Arruda PCVD. Assistência psicológica ao estudante de medicina: 21 anos de experiência. Revista da Associação Médica Brasileira. 2008; 54: 90-94. DOI: https://doi.org/10.1590/S0104-42302008000100027 [ Links ]
2.Bassols AM, Okabayashi LS, Silva ABD, Carneiro BB, Feijó F, Guimaraes GC, et al. First-and last-year medical students: is there a difference in the prevalence and intensity of anxiety and depressive symptoms?. Brazilian Journal of Psychiatry. 2014; 36: 233-240. DOI: https://doi.org/10.1590/1516-4446-2013-1183 [ Links ]
3.Moro A, Valle JBD, Lima LPD. Sintomas depressivos nos estudantes de medicina da Universidade da Região de Joinville (SC). Revista Brasileira de Educação Médica. 2020; 29: 097-102. DOI: https://doi.org/10.1590/1981-5271v29.2-015 [ Links ]
4.Amaral GFD, Gomide LMDP, Batista MDP, Píccolo PDP, Teles TBG, Oliveira PMD, et al. Sintomas depressivos em acadêmicos de medicina da Universidade Federal de Goiás: um estudo de prevalência. Revista de psiquiatria do Rio Grande do Sul. 2008; 30: 124-130. DOI: https://doi.org/10.1590/S0101-81082008000300008 [ Links ]
5.Mayer FB. Prevalência de sintomas de depressão e ansiedade entre os estudantes de medicina: um estudo multicêntrico no Brasil [Doctoral dissertation]. São Paulo: Universidade de São Paulo; 2017. DOI: https://doi.org/10.11606/T.5.2017.tde-13112017-154429 [ Links ]
6.Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among US medical students, residents, and early career physicians relative to the general US population. Academic medicine. 2014; 89(3): 443-451. DOI: https://doi.org/10.1097/acm.0000000000000134 [ Links ]
7.de Souza ACCR, Almeida AA, Cotta BSS, Ferreira AA. Prevalência da síndrome de burnout e a importância do autocuidado nos estudantes de medicina da faculdade ciências médicas de minas gerais. Revista interdisciplinar ciências médicas. 2019; 3(1): 29-36. [ Links ]
8.Oliveira LGD, Barroso LP, Wagner GA, Ponce JDC, Malbergier A, Stempliuk VDA, et al. Drug consumption among medical students in São Paulo, Brazil: influences of gender and academic year. Brazilian Journal of Psychiatry. 2009; 31: 227-239. DOI: https://doi.org/10.1590/S1516-44462009000300008 [ Links ]
9.Santos MCP. Uso de drogas entre estudantes de cursos da área de saúde [Master's thesis]. Joinville: Universidade da Região de Joinville; 2014. [ Links ]
10.Machado CDS, Moura TMD, Almeida RJD. Estudantes de medicina e as drogas: evidências de um grave problema. Revista brasileira de educação médica. 2015; 39: 159-167. DOI: https://doi.org/10.1590/1981-52712015v39n1e01322014 [ Links ]
11.Leitão FNC, Ferreira CRT, de Abreu KL, de Deus MBB, Junior HM, Morais MJD. Efeitos do isolamento social gerado pelo Covid-19 na qualidade de Vida da população em duas cidades brasileiras. Journal of Human Growth and Development. 2021; 31(3): 405-413. DOI: https://doi.org/10.36311/jhgd.v31.12609 [ Links ]
12.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The lancet. 2020; 395 (10227): 912-920. DOI: https://doi.org/10.1016/S0140-6736(20)30460-8 [ Links ]
13.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of personality and social psychology. 1988; 54(6): 1063. DOI: https://doi.org/10.1037//0022-3514.54.6.1063 [ Links ]
14.Krieger T, Hermann H, Zimmermann J, grosse Holtforth M. Associations of self-compassion and global self-esteem with positive and negative affect and stress reactivity in daily life: Findings from a smart phone study. Personality and individual differences. 2015; 87: 288-292. DOI: https://doi.org/10.1016/j.paid.2015.08.009 [ Links ]
15.Leary MR, Tate EB, Adams CE, Batts Allen A, Hancock J. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. Journal of personality and social psychology. 2007; 92(5): 887. DOI: https://psycnet.apa.org/doi/10.1037/0022-3514.92.5.887 [ Links ]
16.Neff K D, Rude SS, Kirkpatrick KL. An examination of self-compassion in relation to positive psychological functioning and personality traits. Journal of research in personality. 2007; 41(4): 908-916. DOI: https://doi.org/10.1016/j.jrp.2006.08.002 [ Links ]
17.Neff KD, Vonk R. Selfcompassion versus global selfesteem: Two different ways of relating to oneself. Journal of personality. 2009; 77(1): 23-50. DOI: https://doi.org/10.1111/j.1467-6494.2008.00537.x [ Links ]
18.Barnard LK, Curry JF. Self-compassion: Conceptualizations, correlates, & interventions. Review of general psychology. 2011; 15(4): 289-303. DOI: https://doi.org/10.1037%2Fa0025754 [ Links ]
19.Neff KD. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and identity. 2003; 2(2): 85-101. DOI: https://doi.org/10.1080/15298860309032 [ Links ]
20.Gilbert P, McEwan K, Matos M, Rivis A. Fears of compassion: Development of three selfreport measures. Psychology and Psychotherapy: Theory, research and practice. 2011; 84(3): 239-255. DOI: https://doi.org/10.1348/147608310x526511 [ Links ]
21.Allen AB, Leary MR. SelfCompassion, stress, and coping. Social and personality psychology compass. 2010; 4(2): 107-118. DOI: https://dx.doi.org/10.1111%2Fj.1751-9004.2009.00246.x [ Links ]
22.Zanon C, Hutz CS. Escala de afetos positivos e negativos (PANAS). In: Hutz CS, org. Avaliação em psicologia positiva. Porto Alegre: Artmed; 2014. p. 63-67. [ Links ]
23.Neff KD. The development and validation of a scale to measure self-compassion. Self and identity. 2003; 2(3): 223-250. DOI: https://doi.org/10.1080/15298860309027 [ Links ]
24.Souza LK, Ávila-Souza J, Gauer G. Escala de autocompaixão. In: Hutz CS, org. Avaliação em Psicologia Positiva: técnicas e medidas. São Paulo: CETEPP; 2016. p. 169-177. [ Links ]
25.American Psychological Association. Publication manual of the American Psychological Association. 6th ed. Washington, DC: Author; 2010. [ Links ]
26.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York: Lawrence Erlbaum Associates; 1988. [ Links ]
27.Porter SR, Whitcomb ME. Non-response in student surveys: The role of demographics, engagement and personality. Research in higher education. 2005; 46(2): 127-152. [ Links ]
28.England P. Separative and Soluble Selves: Dichotomous Thinking in Economics. In: Fineman MA, Dougherty T, editors. Feminism Confronts Homo Economicus. Ithaca: Cornell University Press; 2005. p. 32-56 [ Links ]
29.Frederick T, Purrington S, Dunbar S. Differentiation of self, religious coping, and subjective well-being. Mental Health, Religion & Culture. 2016; 19(6): 553-564. DOI: https://doi.org/10.1080/13674676.2016.1216530 [ Links ]
30.World Health Organization. Depression and other common mental disorders: global health estimates. Geneva: World Health Organization; 2017. [ Links ]
31.Brasil. Depressão: causas, sintomas, tratamentos, diagnóstico e prevenção. Ministério da Saúde [online]. 2020 Nov. [cited 2020 Dez 16]. Available from: https://www.gov.br/saude/pt-br/assuntos/saude-de-a-a-z/d/depressao [ Links ]
32.Dumitrascu CI, Mannes PZ, Gamble LJ, Selzer JA. Substance use among physicians and medical students. Medical Student Research Journal. 2014; 3(Winter): 26-35. [ Links ]
33.Lemos KM, Neves NMBC, Kuwano AY, Tedesqui G, Bitencourt AGV, Neves FBCS, et al. Uso de substâncias psicoativas entre estudantes de Medicina de Salvador (BA). Archives of Clinical Psychiatry (São Paulo). 2007; 34: 118-124. DOI: https://doi.org/10.1590/S0101-60832007000300003 [ Links ]
34.Nogueira-Martins LA, Jorge MR. Natureza e magnitude do estresse na residência médica. Revista da Associação Médica Brasileira. 1998; 44: 28-34. DOI: https://doi.org/10.1590/S0104-42301998000100006 [ Links ]
35.Santa ND, Cantilino A. Suicídio entre médicos e estudantes de medicina: revisão de literatura. Revista Brasileira de Educação Médica. 2016; 40: 772-780. DOI: https://doi.org/10.1590/1981-52712015v40n4e00262015 [ Links ]
36.Paduani GF, Barbosa GDA, Morais JCRD, Pereira JCP, Almeida MF, Prado MM, et al. Consumo de álcool e fumo entre os estudantes da Faculdade de Medicina da Universidade Federal de Uberlândia. Revista brasileira de educação médica. 2008; 32: 66-74. DOI: https://doi.org/10.1590/S0100-55022008000100009 [ Links ]
37.Lourenção LG, Moscardini AC, Soler ZASG. Saúde e qualidade de vida de médicos residentes. Revista da Associação Médica Brasileira. 2010; 56: 81-91. DOI: https://doi.org/10.1590/S0104-42302010000100021 [ Links ]
38.Nunes LYO, Lemos DCL, Júnior RDCR, Behar CB, dos Santos PPP. Análise psicométrica da PANAS no Brasil. Ciencias Psicológicas. 2019; 13(1): 45-55. DOI: http://dx.doi.org/10.22235/cp.v13i1.1808 [ Links ]
39.Crawford JR, Henry JD. The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large nonclinical sample. British journal of clinical psychology. 2004; 43(3): 245-265. DOI: https://doi.org/10.1348/0144665031752934 [ Links ]
40.Yarnell LM, Neff KD, Davidson OA, Mullarkey M. Gender differences in self-compassion: Examining the role of gender role orientation. Mindfulness. 2019; 10(6): 1136-1152. DOI: https://doi.org/10.1007/S12671-018-1066-1 [ Links ]
41.Hofmann SG, Sawyer AT, Fang A, Asnaani A. Emotion dysregulation model of mood and anxiety disorders. Depression and anxiety. 2012; 29(5): 409-416. DOI: https://doi.org/10.1002/da.21888 [ Links ]
42.Barnard LK, Curry JF. The relationship of clergy burnout to self-compassion and other personality dimensions. Pastoral Psychology. 2012; 61(2): 149-163. DOI: http://dx.doi.org/10.1007%2Fs11089-011-0377-0 [ Links ]
43.Gilbert P, Procter S. Compassionate mind training for people with high shame and selfcriticism: Overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice. 2006; 13(6): 353-379. DOI: https://doi.org/10.1002/cpp.507 [ Links ]
44.Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful selfcompassion program. Journal of clinical psychology. 2013; 69(1): 28-44. DOI: https://doi.org/10.1002/jclp.21923 [ Links ]
45.Mello AF, Juruena MF, Pariante CM, Tyrka AR, Price LH, Carpenter LL, et al. Depressão e estresse: existe um endofenótipo?. Brazilian Journal of Psychiatry. 2007; 29: s13-s18. DOI: https://doi.org/10.1590/S1516-44462007000500004 [ Links ]
46.Charney DS. Psychobiological mechanisms of resilience and vulnerability: implications for successful adaptation to extreme stress. American journal of Psychiatry. 2004; 161(2): 195-216. DOI: https://doi.org/10.1176/appi.ajp.161.2.195 [ Links ]
47.Lipp MEN. O stress está dentro de você. 2nd ed. São Paulo: Contexto; 2011. [ Links ]
48.Saravanan C, Wilks R. Medical students' experience of and reaction to stress: the role of depression and anxiety. The Scientific World Journal. 2014; 2014: 737382. DOI: https://doi.org/10.1155/2014/737382 [ Links ]
49.Lavric M, Flere S. The role of culture in the relationship between religiosity and psychological well-being. Journal of Religion and Health. 2008; 47(2): 164-175. DOI: https://doi.org/10.1007/s10943-008-9168-z [ Links ]
 Correspondence:
Correspondence:
Camila de Franco Tobar
camilatobar@yahoo.com.br
Manuscript received: may 2021
Manuscript accepted: december 2021
Version of record online: June 2022












 Curriculum ScienTI
Curriculum ScienTI

