Servicios Personalizados
Revista
Articulo
Indicadores
Compartir
Journal of Human Growth and Development
versión impresa ISSN 0104-1282versión On-line ISSN 2175-3598
J. Hum. Growth Dev. vol.29 no.2 São Paulo mayo/ago. 2019
https://doi.org/10.7322/jhgd.v29.9433
PROTOCOLS
Fractality and chaotic behavior of heart rate variability as hypotension predictors after spinal anesthesia: Study protocol for a randomized controlled trial
Hermes Melo Teixeira BatistaI, II, III; Gylmara Bezerra de Menezes SilveiraIV; Marcelo Ferraz CamposI; Juliana Spat CarlessoI; Vítor Engracia ValentiV; Rodrigo Daminello RaimundoI; Andrés Ricardo Pérez RieraI
ILaboratório de Delineamento e Escrita Científica, Centro Universitário Saúde ABC - Santo André (SP), Brasil
IIDepartmento de Anestesiologia, Hospital Universitário Júlio Bandeira (HUJB) - Cajazeiras (PB), Brasil
IIIFaculdade de Medicina Estácio de Juazeiro do Norte (Estácio FMJ) - Juazeiro do Norte (CE), Brasil
IVHospital Regional do Cariri (ISGH) - Juazeiro do Norte (CE), Brasil
VDepartmento de Terapia da Fala e Audiologia, Faculdade de Filosofia e Ciências (UNESP) - Marília (SP), Brasil
ABSTRACT
INTRODUCTION: All drugs and techniques that induce the anesthetic state act in some way in the Autonomic Nervous System (ANS). The administration of local anesthetics in the subarachnoid space produces motor, sensitive and sympathetic block, with latencies and variable and independent block levels. The motor block is the first to install, followed by the sympathetic and the sensitive. Sympathetic blockage affects 2 to 6 dermatomes above the sensory block. The recovery of spinal anesthesia is assessed through a scale defined in 1979 by Bromage and is based exclusively on the return of motor function and does not take into account the recovery of ANS activity. The persistence of sympathetic block may imply a higher incidence of urinary retention, bradycardia and hypotension
OBJECTIVE: To assess cardiac autonomic modulation during perioperative hypotension caused by subarachnoid anesthesia.
METHODS: A randomised, double-blind clinical trial will be performed in a large hospital located in the southern region of Ceará, Brazil and at the HUJB in Cajazeiras, Paraíba. Sixty patients from the anaesthesia outpatient clinic were enrolled. Patients were divided into two groups: one group received Bupivacaine with clonidine, and the other group received only bupivacaine at a dose of 15 mg. The sample consisted of 60 ASA patients I to III, submitted to orthopedic surgery of lower limbs and lower abdomen under spinal anesthesia. The Heart Rate Variability will be evaluated in three moments: rest, before anesthesia; 20 min after the blockade was installed, and at the time of motor function recovery according to the Bromage criteria and prognostic indices will be evaluated in the development of perioperative hypotension in two groups. Linear methods will be used in the frequency domain and non-linear in chaos domain, Poincaré plot, approximate entropy, Detrended Fluctuation Analysis (DFA) and Correlation Dimension. The data will be collected through a Polar V800® heart rate meter and properly submitted for analysis and filtering by Kubios 3.0® software.
DISCUSSION: In the literature we find data evaluating the installation of sympathetic block through HRV using linear methods however, there is a lack of studies using methods based on the domain of chaos. Some studies address the value of HRV as a predictor of hypotension following subarachnoid anesthesia, mainly using linear methods in the frequency domain. It is understood to be important to analyze these factors using methods already validated in the domain of chaos, complexity and fractality, more compatible with the complexity of the behavior of biological systems, in the characterization of the autonomic function during the subarachnoid anesthesia. : The clinical trial was registered in the Brazilian Registry of Clinical Trials (ReBEC) under the number RBR-4Q53D6.
Keywords: spinal anesthesia, autonomic nervous system, heart rate, recovery room post anesthetic, sympathic block, hypotension.
Authors summary
Why was this study done?
Administration of local anesthetics into the intrathecal space blocks sensory, motor and sympathetic nerve conduction. Throughout the duration of the block, patients should receive constant monitoring. Post-anesthetic recovery room discharge criteria assess only motor function recovery.
What did the researchers do and find?
The researchers conducted a randomized clinical trial protocol to assess autonomic function at motor recovery in patients receiving spinal anesthesia with isobaric bupivacaine alone or clonidine-associated isobaric bupivacaine. Results await publication.
What do these findings mean?
If the initial hypothesis is confirmed, the findings should suggest a review of discharge from the anesthetic recovery room discharge criteria in patients receiving spinal anesthesia and include assessment of the autonomic nervous system, as well as assessment of motor function recovery.
INTRODUCTION
Subarachnoid anesthesia consists of the administration of local anesthetics in the intrathecal space, suppressing nerve conduction through the spinal cord. It is relatively easy and inexpensive technique and widely used worldwide1.
Local anesthetics have selective affinity for various types of nerve fibers, which is called differential block. The fibers of the sympathetic nervous system are more sensitive, being blocked by lower anesthetic concentrations, followed by the sensory fibers responsible for pain, touch and, finally, motor fibers1,2.
Blocking of the sympathetic efferent fibers is responsible for the main complications resulting from spinal anesthesia, and the intensity of bradycardia and hypotension related to the height reached by the blockade. Levels above T4 are strongly associated with these complications. Blocking height is different for each type of nerve fiber, with sensitive blocking reaching two dermatomes above the motor block, and sympathetic block may reach up to six dermatomes above the sensitive. It is assumed that the duration of sympathetic block, which starts first, also ceases its effects before sensory and motor block, accepting a similar duration of action of the local anesthetic in all nerve fibers2.
Several complications may be associated with subarachnoid anesthesia, the most common being bradycardia, nausea, vomiting, hypotension and anxiety. There are reports in the literature of cardiorespiratory arrest right after spinal anesthesia. The rate of complications is inherent to the clinical condition of the patient, the surgical pathology, or reached height of the anesthetic block, however there are reports of cardiorespiratory arrest after spinal anesthesia in healthy patients without previous comorbidities3,4. Early identification of greater propensity for complications is essential to reduce the time between diagnosis and conduct, implying a reduction in morbidity and mortality1,3,4.
The discharge from the post anesthetic recovery from in patients receiving spinal anesthesia obeys the Bromage Scale, which qualitatively evaluates the return of motor function, without, however, taking into account the autonomic component5. Since the installation of the blockade is differential, it is believed that its duration is also different, and that patients reaching grade II of the Bromage Scale, with motor function in recovery, may still present sympathetic block, being subject to the complications resulting from this block5.
The functioning of the heart does not occur in an exactly regular way. The sinoatrial node controls the heart rate by sending the beat information between 60 and 90 bpm. However, the sympathetic and parasympathetic nervous systems are in constant conflict modulating this information. The sympathetic tends to increase the heart rate and the parasympathetic decreases it. The result is a difference of a few milliseconds between each heartbeat, even at a regular pace. This variation is considered physiological and healthy, since it reflects the body's ability to respond to diverse external and internal demands. That is, high heart rate variability means health. While low variability indicates the inability of the organism to adapt to meet variation; whether physiological or not of the individual's metabolic demands, meaning pathology or aging6.
The evaluation of Heart Rate Variability through ECG or heart rate meter is a validated technique used worldwide to evaluate the overall functioning of the autonomic nervous system or its sympathetic and parasympathetic components. Some studies demonstrate the changes in HRV during the installation of subarachnoid anesthesia7; however, no studies were found describing changes in HRV during recovery from anesthesia, or the duration of sympathetic blockade. Figure 1 shows the evolution of the spectrogram during the perioperative period of a patient submitted to an orthopedic surgical procedure under spinal anesthesia.
Subarachnoid anesthesia consists of the administration of local anesthetics in the intrathecal space, suppressing nerve conduction through the spinal cord. It is relatively easy and inexpensive technique and widely used worldwide1.
Local anesthetics have selective affinity for various types of nerve fibers, which is called differential block. The fibers of the sympathetic nervous system are more sensitive, being blocked by lower anesthetic concentrations, followed by the sensory fibers responsible for pain, touch and, finally, motor fibers1,2.
Blocking of the sympathetic efferent fibers is responsible for the main complications resulting from spinal anesthesia, and the intensity of bradycardia and hypotension related to the height reached by the blockade. Levels above T4 are strongly associated with these complications. Blocking height is different for each type of nerve fiber, with sensitive blocking reaching two dermatomes above the motor block, and sympathetic block may reach up to six dermatomes above the sensitive. It is assumed that the duration of sympathetic block, which starts first, also ceases its effects before sensory and motor block, accepting a similar duration of action of the local anesthetic in all nerve fibers2.
Several complications may be associated with subarachnoid anesthesia, the most common being bradycardia, nausea, vomiting, hypotension and anxiety. There are reports in the literature of cardiorespiratory arrest right after spinal anesthesia. The rate of complications is inherent to the clinical condition of the patient, the surgical pathology, or reached height of the anesthetic block, however there are reports of cardiorespiratory arrest after spinal anesthesia in healthy patients without previous comorbidities3,4. Early identification of greater propensity for complications is essential to reduce the time between diagnosis and conduct, implying a reduction in morbidity and mortality1,3,4.
The discharge from the post anesthetic recovery from in patients receiving spinal anesthesia obeys the Bromage Scale, which qualitatively evaluates the return of motor function, without, however, taking into account the autonomic component5. Since the installation of the blockade is differential, it is believed that its duration is also different, and that patients reaching grade II of the Bromage Scale, with motor function in recovery, may still present sympathetic block, being subject to the complications resulting from this block5.
The functioning of the heart does not occur in an exactly regular way. The sinoatrial node controls the heart rate by sending the beat information between 60 and 90 bpm. However, the sympathetic and parasympathetic nervous systems are in constant conflict modulating this information. The sympathetic tends to increase the heart rate and the parasympathetic decreases it. The result is a difference of a few milliseconds between each heartbeat, even at a regular pace. This variation is considered physiological and healthy, since it reflects the body's ability to respond to diverse external and internal demands. That is, high heart rate variability means health. While low variability indicates the inability of the organism to adapt to meet variation; whether physiological or not of the individual's metabolic demands, meaning pathology or aging6.
The evaluation of Heart Rate Variability through ECG or heart rate meter is a validated technique used worldwide to evaluate the overall functioning of the autonomic nervous system or its sympathetic and parasympathetic components. Some studies demonstrate the changes in HRV during the installation of subarachnoid anesthesia7; however, no studies were found describing changes in HRV during recovery from anesthesia, or the duration of sympathetic blockade. Figure 1 shows the evolution of the spectrogram during the perioperative period of a patient submitted to an orthopedic surgical procedure under spinal anesthesia.
Hypotheses
1. Patients who received spinal anesthesia present a reduction in heart rate variability and, upon reaching the criteria of discharge from the PACU by the Bromage scale, still present residual sympathetic block, being subject to a greater risk of postural hypotension, urinary retention and hypothermia.
2. Patients with low resting heart rate variability have a higher risk of hypotension and mortality after subarachnoid blockade.
3. Clonidine administered in the subarachnoid space increases the risk of perioperative hypotension.
To evaluate cardiac autonomic modulation during perioperative hypotension caused by subarachnoid anesthesia.
METHODS
Study Design
This is a randomised, double-blind clinical trial will be performed in a large hospital located in the southern region of Ceará, Brazil. Sixty patients from the anaesthesia outpatient clinic were enrolled. Patients were divided into two groups: one group received Bupivacaine with clonidine, and the other group received only bupivacaine at a dose of 15 mg. The study, to be carried out in the county of Juazeiro do Norte, Ceará, Brazil and at the HUJB in Cajazeiras, Paraíba. The sample consisted of 60 ASA patients I to III, submitted to orthopedic surgery of lower limbs and lower abdomen under spinal anesthesia. The Heart Rate Variability will be evaluated in three moments: rest, before anesthesia; 20 min after the blockade was installed, and at the time of motor function recovery according to the Bromage criteria and prognostic indices will be evaluated in the development of perioperative hypotension in two groups (Table 1). Linear methods will be used in the frequency domain and non-linear in chaos domain, Poincaré plot, approximate entropy, Detrended Fluctuation Analysis (DFA) and Correlation Dimension. The data will be collected through a Polar V800® heart rate meter and properly submitted for analysis and filtering by Kubios 3.0® software. The collection will be performed in the period between october 1, 2018 and March 1, 2019.
The structure of the study will be based on the protocol will use The SPIRIT-PRO Extension found on the Equator Network.
Sample size
Using a sample error of 5% and a confidence level of 95% for type I error, we reached a number of 30 individuals.
HRV will be evaluated in three initial moments: during rest before the administration of spinal anesthesia; 20 minutes after anesthetic block and when the patient reached the criteria for discharge from the PACU by the Bromage Score. The control will be HRV measured at rest before anesthesia.
The following methods of evaluation of HRV based on chaos theory will be used: the discontinuous fluctuation analysis, the approximate entropy, the Poincaré plot and the correlation dimension.
The data will be collected with the V800 polar heart ratemeter and analyzed and filtered manually at first, being refilled using the Kubios HRV 3.0 software.
The height of the blockade reached will be measured and recorded in all patients using the thermal sensitivity test, in addition to all hemodynamic parameters routinely followed during a standard anesthesia (pressure levels, ECG, temperature, pulse oximetry).
Recruitment
The recruitment of patients will be performed in the preparation of the surgical center, before the pre-anesthetic evaluation in both hospitals. They will receive guidance on the study and procedures to be performed. The collection period will be from October 1, 2018 to March 1, 2019.
Eligibility criteria for participants
Voluntary patients admitted to orthopedic surgery and general surgery under spinal anesthesia at the Cariri Regional Hospital in the city of Juazeiro do Norte and patients submitted to gynecological procedures at the HUJB in Cajazeiras, Paraíba. There will be no gender distinction between patients.
Inclusion criteria
Included in the study will be ASA I to III patients admitted to the CRH for orthopedic and trauma surgeries of the lower limbs or low abdominal surgeries and patients submitted for gynecological surgery in the HUJB. The anesthesia given will be spinal anesthesia with hyperbaric bupivacaine with or without adjuvants in the neuroaxis, without the use of sedation. Patients who accept and sign the Term of Free and Informed Consent form will participate in the study (Figure 2).
Exclusion Criteria
Patients will be excluded if they use antihypertensive drugs that act in the nervous conduction of the myocardial fibers, drug addicts, smokers, subjected to other types of surgical procedures or anesthetic technique. Patients with decompensated clinical conditions or in recent use of anticoagulants that contraindicate spinal anesthesia will be excluded. The use of other anesthetic techniques in association with subarachnoid blockade will also not be included in the sample, as well as important blood loss in the preoperative period (above 500 ml) with a need for aggressive volume replacement.
Information and locations from which data will be collected
The collections will be started at the Cariri Regional Hospital, a highly complex hospital located in Juazeiro do Norte, Ceará and at the HUJB in Cajazeiras, Paraíba. The V800 polar® cardiofrequency meter will be used to record the RR intervals of the patients in the surgical block in the preparation spaces of the patient, operating room and post anesthetic recovery room. A second group of patients will have their collection performed at HUJB, a medium complexity hospital located in Cajazeiras, Paraíba; all in the Brazilian Northeast following the same temporal and spatial sequence.
Interventions
HRV will be evaluated in three initial moments: 1. Rest, prior to administration of spinal anesthesia; 2. 20 minutes after the anesthetic block is installed and 3. at the moment the patient reaches the discharge criteria for the PACU by the Bromage Score (Figure 1). The HRV collected during anesthesia and PACU will be compared to the control that will be the HRV of the patient measured at rest before the anesthesia.
Experimental Protocol
Initially the volunteers will be submitted to the pre-anesthetic evaluation with complete anamneses and physical examination. All will be monitored with pulse oximetry, cardioscopy, noninvasive pressure and temperature. The HRV measurement will be performed using a V800 polar® heart rate meter with the patient in the supine position, in a quiet environment, at a temperature of 24°C and humidity <50%. Patients were divided into two groups: one group received Bupivacaine with clonidine, and the other group received only bupivacaine. Neither patients nor anesthesiologists will know what group they belong to. The randomization will be done by lottery by a professional who will not administer the anesthesia. After checklist of safe surgery and release for surgery, patients will be referred to the operating room. Subarachnoid anesthesia will be performed in the indicated cases and after 20 minutes a new HRV collection will be performed. After the surgical procedure, the patient will be referred to the post-anesthetic recovery room and will be evaluated using the criteria of Aldrete and Kroulick and the Bromage Scale. Upon reaching Bromage 2, a new HRV measurement will be performed. The collections will be filtered using manual method in Excel for windows and then receive standard filtering using Kubios 3.0 software.
Monitoring
Patients will receive multi-parameter monitoring with Dixtal DX 2020 Monitor to measure blood pressure, temperature, oximetry, and cardioscopy throughout the time from preparation to discharge of PACU. After the monitoring will be used the V800 polar® heart rate meter and the analysis of the series of RR intervals will be performed with a computer equipped with the windows 10 operating system, using the software excel for windows 2013 and Kubios 3.0 for the final analysis of the time series.
The variables in the frequency domain, LF, HF and LF/HF will be evaluated; in the domain of DFA chaos, Poincaré plot, approximate entropy, sample entropy and correlation dimension.
RESULTS
Current criteria for PACU discharge in patients undergoing spinal anesthesia do not include recovery from autonomic function, which may be associated with an early discharge to the ward and a greater chance of postoperative complications such as bradycardia, hypotension and urinary retention. The aim of this study was to identify the relationship between duration of sympathetic blockade and motor block obtained with spinal anesthesia and the relation of HRV indices based on the theory of chaos with perioperative hypotension.
Statistical methods
The statistical program PRISMA 7 will be used to compare HRV parameters at different times. The indices to be analyzed are: Poincaré plot, DFA, DC and approximate entropy. It will be considered as significant p <0.05. The data will be analyzed using the ANOVA statistical tests to compare the 3 means, Wilcoxon et de paired Student (paired because it is the same sample at different times), to compare the data at different moments, besides the positive predictive value, sensitivity and specificity to determine the risk of hypotension associated with HRV resting measures.
Ethical aspects
The study was submitted to the Ethics Committee on Research in humans of the Institute of Health and Hospital Management (ISGH), being approved and under the seem No. 2,447,717. All study participants will be informed about the procedures, equipment, objectives and methods to be used. The confidentiality of all information related to the identity of the participant and the impersonality of the data collected was guaranteed. It was also informed the possibility of contacting the researchers or the CEP if there is a need to clarify any relevant aspect or complaint related to the research. After the free acceptance of the terms, the volunteers read and signed the Term of Free and Informed Consent, according to the norms of the National Health Council.
The clinical trial was registered in the Brazilian Registry of Clinical Trials (ReBec) under number RBR-4Q53D6. With the title: Fractal and chaotic behavior of heart rate variability in subarachnoid anesthesia. The complete protocol can be accessed at ReBec8.
DISCUSSION
The surgical procedure is a time of great stress for the body. The aggression provided in the perioperative period begins before the act with the anxiety and the fears experienced by the patient, reaching its apex in the surgical trauma itself. It triggers an exacerbated metabolic endocrine response with release of catecholamines, cortisol, glucagon, interleukins, and tumor necrosis factor. Anesthesia modulates this response, preserving the autonomic balance, mainly decreasing the sympathetic response inducing analgesia and hypnosis9.
Various drugs and techniques are used to provide anesthesia and to attenuate the body's response to surgical aggression. There is no consensus on what the ideal anesthetic would be for each procedure, mainly because of the difficulty in measuring its effectiveness in the short and long term. Today it is accepted that the type of anesthesia has influence on the prognosis in some contexts. Cakmakkaya, in a recent meta-analysis, makes a survey between the associations of epidural anesthesia with general anesthesia as a prognostic factor of tumor recurrence in cancer patients, finding data still inconsistent9.
The modulation of the metabolic endocrine response provided by the anesthesia is individualized, and may itself trigger catecholamines, such as at the moment of intubation. Opioids, the basis of analgesia in general anesthesia, trigger immunosuppression and may be responsible, when in inadequate doses, for higher rates of infection. Regional neuroaxis anesthesias inhibit nerve afferentation, however, they do not completely block the endocrine metabolic response, since it inhibits the passage of surgical stimulation conducted by the nerve pathway, but has no effect on the conduct of the information of aggression by the endocrine and immune pathways. Anesthesia should be conducted in an individualized way, however, a reliable measure of the endocrine metabolic response and the effect of anesthetics on the modulation of surgical stress is necessary, since both excess and insufficiency are detrimental10,11.
Several devices have been proposed to evaluate the autonomic function and the analysis of the heart rate variability has been highlighted by its non-invasiveness and ease of handling of the signals, and several studies have been published using this method in the most varied scenarios and clinical conditions12.
The analysis of heart rate variability can be done using linear, time or frequency, and nonlinear methods in the chaos domain. Most published studies use linear methods, and it is currently believed that they do not adequately represent the complexity of interactions between the various systems of the organism and environmental influences9-12.
In view of the large number of studies using heart rate variability and the various possibilities of interpretation of the data obtained, some with dubious conclusions, The European Society of Cardiology together with The North American Society of Pacing and Electrophysiology developed a task force and published in 1996 a document standardizing the values of linear HRV analysis methods in time and frequency domain, physiological interpretation and clinical applications13. After this publication, other methods of analysis of heart rate variability have emerged, based on chaos theory, fractalness and complexity, and the current evidence suggests that these methods more appropriately represent the complexity of the functioning of biological systems, bringing to light information which were not identified by traditional methods. Thus, the ESC Working Group, the European Heart Rhythm Association and the Asia Pacific Heart Rhythm Society organized a new task force to search the literature for non-linear methods of heart rate variability, to describe technical aspects of these methods and suggest clinical applications. Only 21 articles met the eligibility criteria14.
Linear methods are analyzed in the domain of time and frequency. The vast majority of existing studies evaluating HRV in the surgical setting use linear methods in the frequency domain. Frequency domain methods consider the spectrum of the heart rate-generating signal and are classified as LF, HF, LF/HF. Variations of LF and HF are recognized as markers of sympathetic and parasympathetic activity. Total spectral density, identified as the area under spectral components between 0.03 and 0.5 Hz, reflects the autonomic tone. Spectral analysis of HRV reveals 2 main components; LF with a central frequency between 0.03 and 0.15 Hz and HF between 0.15 and 0.5 Hz. The HF component correlates well with the respiratory signal and is considered a marker of parasympathetic activity, while the LF component is associated with a mixture of sympathetic and parasympathetic activities, predominantly sympathetic. VLF (very low frequency), very low frequency components and apparently represents the renin-angiotensin-aldosterone system and the LF / HF ratio, which characterizes the autonomic balance15,16.
Fujiwara et al.17 demonstrated during the installation of subarachnoid anesthesia initial elevation of LF, followed by significant reduction of LF/HF. These parameters were extrapolated to non-linear methods, which better reflect the behavior of the physiological systems, especially the Poincaré Plot, with SD1 showing close correlation with HF, representing the parasympathetic component of the autonomic nervous system17.
The LF/HF ratio acts as an indicator of the sympatovagal balance. After dispersion of the blockade at T3-T4 levels, the LF/HF ratio practically doubled and returned to baseline when the blockade reached T1-T2. In this case, the sympatovagal balance does not seem to have changed, however, the spectral density examination reveals a significant reduction in total power that is not obvious in the isolated examination from nude or LF/HF ratio alone17.
The resulting temporal series (extracted) of biological signals in their great majority present complex and chaotic behavior, and it is not possible to characterize its nature with a single method of analysis. In the analysis of heart rate variability in the chaos domain, the association of 2 or 3 methods reveals more complex and more representative information of natural events (approximate entropy, Poincaré plot, DFA, correlation dimension, etc.). The joint analysis of the results allows estimating the complex, regular or random behavior of the time series, bringing to light a greater amount of information and possible variables18.
Some studies use linear HRV methods as predictors of hypotension after spinal anesthesia. However, the hypotension associated with spinal anesthesia is the result of several and complex interactions, mainly related to the adaptability of the organism after local anesthetic administration and the achieved blocking time, among others (previous hydration, interaction with antihypertensives, magnesium sulfate, anxiety). There have been reports of PCR after installation of spinal anesthesia in young patients, without significant comorbidities. We believe that measures of preoperative HRV along with measures post-installation of spinal anesthesia are more reliable to predict hypotension. Linear methods do not reflect the complexity of the adaptive interactions of the organism after sympathetic blockade of spinal anesthesia. Nonlinear methods in the domain of chaos seem to be more suitable19,20.
There are studies describing parameters of heart rate variability using linear methods21 during the period of subarachnoid anesthesia. However, it is not found in the literature, descriptions of the recovery parameters of the same, which justifies this work. When the duration of spinal anesthesia is mentioned, Introna considers that the sensory, motor and autonomic blocks regress at equivalent moments22. There is also a lack of studies describing the chaotic, fractal and complex behavior of HRV during spinal anesthesia. We also question the discharge criteria of PACU, which evaluates only the return of motor function, neglecting the restoration of sympathetic function to the state prior to anesthesia and the complications associated with it, such as bradycardia affecting up to 13% of patients and hypotension23 occurring in 5% to 56%.
The HRV analysis of time series from the measurement of ECG RR intervals based on conventional methods does not accurately reflect the complexity of the cardiac autonomic control. The biological signal results from the cardiac response to the various internal and environmental stimuli and presents stochastic behavior, best represented by non-linear methods, based on chaos theory and represent the complexity and fractality of the signal24,25.
Thus, the work in question has relevance, in the sense in which it will bring to light, objective data of the autonomic function during the installation of the subarachnoid anesthesia and the post anesthetic recovery period, relating temporally the return of the motor function and the restoration of the sympathovagal balance through analysis of heart rate variability24.
Chaos and complexity indices
There are several techniques of analysis of time series described and that are based on statistical, geometric and informational artifice. In this study, the DFA, Poincaré Plot, approximate entropy and correlation dimension will be used. Here is a brief description of each method.
DFA
The trendless fluctuation analysis was developed by Peng in 1995 and provides a quantitative parameter of the autocorrelation properties of a time series. It measures the complexity of the biological signal using its fractal property, estimating the occurrence of self-similarity in the RR intervals at different scales. It uses short-range segments represented by index α1, which involves correlations from 4 to 16 beats and long range by α2, involving series of 16 to 64 beats. In mathematical terms, DFA implies that a given interval of a time series is partially dependent on the preceding interval. It was developed with the purpose of filtering the signal, removing from it the fluctuations due to the influence of the external environment26.
Long-range correlations represent the sympathetic component of the ANS, while the short-range correlation corresponds to both components; sympathetic and parasympathetic. Quantitative representation simplifies the interpretation of the signal. DFA values close to 0.5 represent the absence of correlation within the temporal or spatial series, with presence of randomness, implying worse prognosis27 and in the case of this study, a higher propensity to hypotension after spinal anesthesia. Values close to 1 indicate fractal dynamics in the RR interval analyzed, that is, it represents the healthy individual, with a good capacity to respond to the demands of the surgical stress. Values close to 1.5 tend to present strongly correlated behavior tending to regularity, that is, low heart rate variability.
Krstacic, studying patients with cardiomyopathy, identified that deviation of the DFA values from the normality agreed to as 1.0, be it higher or lower, present a loss of fractality and are associated with higher morbidity and worse prognosis, tending to the randomness or regularity of the signal28.
The Poincaré Plot
The Poincaré plot is the two-dimensional graphical representation of a series of data using ordered pairs, where xn is plotted on the x-axis and xn + 1 plotted on the y-axis. Thus, each point on the Poincaré graph is given by the ordered pair (xn, Xn + 1).
Poincaré plot analysis can be done qualitatively or quantitatively. In the qualitative analysis, one observes the shape of the graph. More concentrated points correspond to patients with low heart rate variability, indicative of weakened organisms. More scattered points are observed in healthy individuals.
For the quantitative analysis of the Poincaré plot, an ellipse is plotted to the plot points with the center being the mean of the RR intervals. From this the index SD1 and SD2 are calculated. The SD1 measures the standard deviation of the distances of the points to the diagonal y = x; determines the width of the ellipse and represents the parasympathetic nervous system. The SD2 measures the standard deviation of the distances from points to the line y = -x + RRm, where RRm is the mean of the RR intervals of the series; is measured from the ellipse length and reflects the variability of the global heart rate29.
Approximate Entropy
The approximate entropy reflects the complexity of the signal. It was developed by Pincus in 1991 to quantify the regularity of biological signals in relatively small and noisy series23. It can be used to predict future patterns from previous values within a time series. The presence of similar repetitive patterns in a series of RR intervals implies an approximate low value entropy, whereas an irregular sequence implies high values of entropy.
Series with approximate low entropy present low complexity and tend to signal regularity. This is observed in aging and in pathological states, being associated with greater morbidity and mortality. High values of entropy are observed in complex systems and are related to high variability and good prognosis23,29.
Correlation Dimension
The correlation dimension is a probabilistic representation of the trajectory in the phase space of a given time or space series, taking into account the possible degrees of freedom, which describes how much two points within this trajectory are correlated. It reflects the dimension or density of the strange attractor of a data set, which configures the point of convergence of the series30.
The correlation dimension translates the complexity of a given series of data, thus, the larger the dimension, the greater the complexity, that is, a greater number of state variables is needed to describe its dynamics. However, not all variables can be identified and it is not possible to know exactly the total number of degrees of freedom. Thus, for application in the clinical interpretation of the cardiovascular system, the correlation dimension is constructed from observable variables, using algorithms that can be applied to relatively short series.
Limitations
The perioperative period has many factors that may interfere with the study result. The emotional state of the patient, the noise present in the operating room, the level of surgical aggression, which varies between the various procedures, in addition to the surgeon's skill. Further studies need to be performed to confirm the hypotheses listed.
Future Perspectives
There are in clinical use, monitors partially using indices of heart rate variability, combined with other physiological measures, and that it is proposed to measure perioperative nociception. The nociception index (NoL) is based on the combination of heart rate signals, heart rate variability, photoplethysmographic wave amplitude, skin conductance, and skin conductance fluctuations and was validated in 201631. In addition to this, ANSindex is in the early stages of clinical studies that use HRV as a predictor of hypotension after spinal anesthesia. It uses for its algorithm linear method in the domain of the frequency LF and HF and converts the indexes in a value that goes from 00 to 100 and provides an objective value to differentiate predominance of the sympathetic or parasympathetic nervous system. High values of ANSindex indicate sympathetic predominance, while low values indicate parasympathetic predominance. Prashanth, in a study of 108 patients, found that ANSindex values above 24% or more had a high predisposition to develop hypotension after spinal anesthesia32.
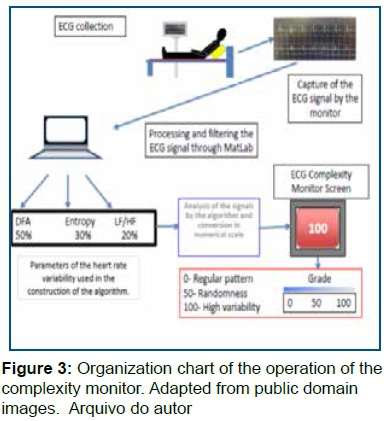
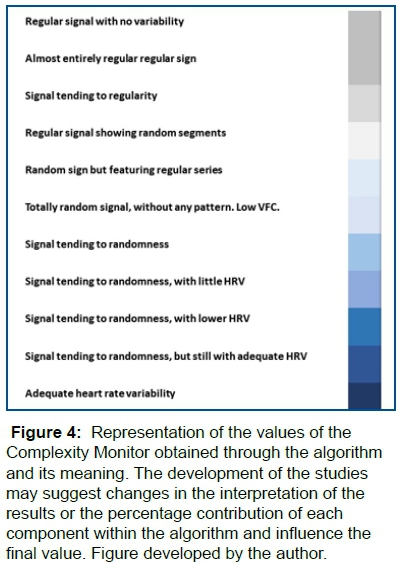
The aim of this work is to use methods of the HRV chaos domain as a predictor of perioperative hypotension and to use as a basis for the development of a device that has the ability to present in a simple, objective and real time the complex behavior of the ECG signal in the scenario surgical (Figure 3). The equipment will be based on an algorithm based on the DFA methods, approximate entropy and Correlation Dimension, all based on chaos theory, condensing the data of these variables into a simple stepped numerical value. The scale will include values between 00 and 100, which will be plotted on the monitor screen (Figure 4). The value 00 will correspond to the regularity of the signal, 50 will be equivalent to a complex signal with good variability and 100 a random signal (Figure 1). It will be established for the construction of the algorithm a proportionality of 50% of the DFA, 30% of the correlation dimension and 20% of the approximate entropy. The percentage of contribution of each method was defined after an initial pilot study of 15 patients belonging to the study group and that will be included in the original study, where the relevance of each method during spinal anesthesia was observed. These percentages may change during project development.
This algorithm will initially be developed to be used in patients under spinal anesthesia. Further studies should be performed to identify the possibility of use as prognosis in other scenarios and groups of patients.
The budget project for the construction of the device will be submitted to the Ministry of Education of Brazil through the EBSERH network and resources will be sought from the ReHUF funds.
The ECG signal will initially be collected from the patient and scanned into a standard monitor, then filtered and processed into hardware using the MatLab program. The values of DFA α1, approximate entropy and LF̸HF will be extracted. The values obtained will be submitted to the algorithm under development and converted into a simple numerical scale ranging from 0 to 100 and will be plotted in the Complexity Monitor. The software will display on the screen the value corresponding to the last 2 minutes of the ECG and will be updated every 5 seconds with the previous 2 minutes. The final value will have a delay of at least 5 s and will correspond to the previous 2 minutes (Figure 1 and Figure 2).
The complexity level (ComplexLev) index will be developed for specific use in the surgical center and its algorithms are initially based on data obtained from patients submitted to spinal anesthesia. Its function is to identify early deterioration of the control of the autonomic nervous system, by reducing the complexity of the ECG signal, in real time during the surgical procedure, using objective interpretation, allowing quick decision making. The early identification of deterioration is a preponderant factor in reducing morbidity and mortality in the surgical patient.
The applications in other scenarios as a predictor of morbidity and mortality, simplified assessment of the general clinical condition of diabetic patients, hypertensive patients, nephropathies, etc., will be possible with the use of the same algorithm or after modifications of the methods to be used. The possibilities are many and will arise as new research is done.
REFERENCES
1.Mordecai MM, Brull SJ. Spinal anesthesia. Curr Opin Anaesthesiol. 2005;18(5):527-33. DOI: http://doi.org/10.1097/01.aco.0000182556.09809.17 [ Links ]
2.Cwik J. Postoperative considerations of neuraxial anesthesia. Anesthesiol Clin. 2012; 30(3):433-43. DOI: http://doi.org/10.1016/j.anclin.2012.07.005 [ Links ]
3.Kumari A, Gupta R, Bajwa SJS, Singh A. Unanticipated cardiac arrest under spinal anesthesia: An unavoidable mystery with review of current literature. Anesth Essays Res. 2014;8(1):99-102. DOI: http://doi.org/10.4103/0259-1162.128923 [ Links ]
4.Kopp SL, Horlocker TT, Warner ME, Hebl JR, Vachon CA, Schroeder DR, et al. Cardiac arrest during neuraxial anesthesia: frequency and predisposing factors associated with survival. Anesth Analg. 2005;100(3):855-65. DOI: http://doi.org/10.1213/01.ANE.0000144066.72932.B1 [ Links ]
5.Wahi A, Singh AK, Syal K, Sood A, Pathania J. Comparative efficacy of intrathecal bupivacaine alone and combination of bupivacaine with clonidine in spinal anaesthesia. J Clin Diagn Res. 2016;10(4):UC06-8. DOI: http://doi.org/10.7860/JCDR/2016/16343.7565 [ Links ]
6.Cornforth DJ, Tarvainen MP, Jelinek HF. How to calculate renyi entropy from heart rate variability, and why it matters for detecting cardiac autonomic neuropathy. Front Bioeng Biotechnol. 2014;2:34. DOI: http://doi.org/10.3389/fbioe.2014.00034 [ Links ]
7.Lee SH, Lee DH, Ha DH, Oh YJ. Dynamics of heart rate variability in patients with type 2 diabetes mellitus during spinal anaesthesia: prospective observational study. BMC Anesthesiol. 2015;15:141. DOI: http://doi.org/10.1186/s12871-015-0125-6 [ Links ]
8.Registro Brasileiro de Ensaios Clínicos (ReBec). Fractalidade e comportamento caótico da variabilidade da frequência cardíaca na anestesia subaracnóide. [cited 2019 Fev 28] Available from: http://ensaiosclinicos.gov.br/rg/RBR-4q53d6/. [ Links ]
9.Cakmakkaya OS, Kolodzie K, Apfel CC, Pace NL. Anaesthetic techniques for risk of malignant tumour recurrence. Cochrane Database Syst Rev. 2014;(11):CD008877. DOI: http://doi.org/10.1002/14651858.CD008877.pub2 [ Links ]
10.Vanderlei FM, Vanderlei LCM, Garner DM. Heart rate dynamics by novel chaotic globals to hrv in obese youths. J Hum Growth Dev. 2015;25(1):82-8. DOI: https://doi.org/10.7322/jhgd.96772 [ Links ]
11.Valenti VE. The recent use of heart rate variability for research. J Hum Growth Dev. 2015;25(2):137-40. DOI: https://doi.org/10.7322/jhgd.102991 [ Links ]
12.Tulppo MP, Kiviniemi AM, Hautala AJ, Kallio M, Seppänen T, Mäkikallio TH, et al. Physiological background of the loss of fractal heart rate dynamics. Circulation. 2005; 112(3):314-9. DOI: https://doi.org/10.1161/CIRCULATIONAHA.104.523712 [ Links ]
13.Malik M, Camm AJ, Bigger JT, Breithardt G, Cerutti S, Cohen R, et al. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Eur Heart J. 1996;17(3):354-81. [ Links ]
14.Sassi R, Cerutti S, Lombardi F, Malik M, Huikuri HV, Peng CK, et al. Advances in heart rate variability signal analysis: joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Europace. 2015;17(9):1341-53. DOI: https://doi.org/10.1093/europace/euv015 [ Links ]
15.Vanderlei LCM, Pastre CM, Hoshi RA, Carvalho TD, Godoy MF. Noções básicas de variabilidade da frequência cardíaca e sua aplicabilidade clínica. Rev Bras Cir Cardiovasc. 2009;24(2):205-17. DOI: http://dx.doi.org/10.1590/S0102-76382009000200018 [ Links ]
16.Abreu LC. Variabilidade da frequência cardíaca como marcador funcional do desenvolvimento. J Hum Growth Dev. 2012;22(3):279-82. DOI: https://doi.org/10.7322/jhgd.46712 [ Links ]
17.Fujiwara Y, Sato Y, Shibata Y, Asakura Y, Nishiwaki K, Komatsu T. A greater decrease in blood pressure after spinal anaesthesia in patients with low entropy of the RR interval. Acta Anaesthesiol Scand. 2007;51(9):1161-5. DOI: https://doi.org/10.1111/j.1399-6576.2007.01435.x [ Links ]
18.Tapanainen JM, Thomsen PEB, Køber L, Torp-Pedersen C, Makikallio TH, Still AM, et al. Fractal analysis of heart rate variability and mortality after an acute myocardial infarction. Am J Cardiol 2002;90(4):347-52. [ Links ]
19.Sassi R, Signorini MG, Cerutti S. Multifractality and heart rate variability. Chaos. 2009;19(2):028507. DOI: https://doi.org/10.1063/1.3152223 [ Links ]
20.Silva MAC, Nicácio MB, Pimentel IDO, Lopes PFF, Rebouças GM, Medeiros HJ. Métodos não lineares para a mensuração da modulação autonômica. Neurociências. 2014; 10(2):94-103. [ Links ]
21.Roy B, Ghatak S. Métodos não-lineares para avaliar mudanças na variabilidade da frequência cardíaca em pacientes com diabetes tipo 2. Arq Bras Cardiol. 2013;101(4):317-27. DOI: http://dx.doi.org/10.5935/abc.20130181 [ Links ]
22.Introna R, Yodlowski E, Pruett J, Montano N, Porta A, Crumrine R. Sympathovagal effects of spinal anesthesia assessed by heart rate variability analysis. Anesth Analg. 1995; 80(2):315-21. [ Links ]
23.Pincus SM. Approximate entropy as a measure of system complexity. Proc Natl Acad Sci USA. 1991;88(6):2297-301. [ Links ]
24.Wagner CD, Persson PB. Chaos in the cardiovascular system: na update. Cardiovasc Res. 1998;40(2):257-64. [ Links ]
25.Lima DGS, Saraiva AO, Santos CY, Oliveira SMR, Pereira RP, Sombra WG, et al. Characterization of heart rate variability during total venous anesthesia: a case report. Amadeus Int Multidisc J. 2018;2(4):57-70 . DOI: https://doi.org/10.14295/aimj.v2i4.31 [ Links ]
26.Peng CK, Havlin S, Stanley HE, Goldberger AL. Quantification of scaling exponents and crossover phenomena in nonstationary heartbeat time series. Chaos. 1995;5(1):82-7. DOI: https://doi.org/10.1063/1.166141 [ Links ]
27.Tapanainen JM, Thomsen PEB, Køber L, Torp-Pedersen C, Ma¨kikallio TH, Still AM, et al. Fractal analysis of heart rate variability and mortality after an acute myocardial infarction. Am J Cardiol. 2002;90(4):347-52. [ Links ]
28.Krstacic G, Krstacic A, Smalcelj A, Milicic D, Jembrek-Gostovic M. The "Chaos Theory" and nonlinear dynamics in heart rate variability analysis: does it work in short-time series in patients with coronary heart disease? Ann Noninvasive Electrocardiol. 2007;12(2):130-6. DOI: https://doi.org/10.1111/j.1542-474X.2007.00151.x [ Links ]
29.Ferreira MT, Messias M, Vanderlei LCM, Pastre CM. Caracterização do comportamento caótico da variabilidade da frequência cardíaca (VFC) em jovens saudáveis. Tend Mat Apl Comput. 2010; 11(2): 141-150. [ Links ]
30.Claus D Wagner, Pontus B Persson; Chaos in the cardiovascular system: an update, Cardiovascular Research, Volume 40, Issue 2, 1 November 1998, Pages 257-264, https://doi.org/10.1016/S0008-6363(98)00251-X [ Links ]
31.Edry R, Recea V, Dikust Y, Sessler DI. Preliminary intraopera-tive validation of the nociception level index: A noninvasivenociception monitor. Anesthesiology. 2016;125(1):193-203. DOI: https://doi.org/10.1097/ALN.0000000000001130 [ Links ]
32.Prashanth A, Chakravarthy M, George A, Mayur R, Hosur R, Pargaonkar S. Sympatho-vagal balance, as quantified by ANSindex, predicts post spinal hypotension and vasopressor requirement in parturientsundergoing lower segmental cesarean section: a single blinded prospective observational study. J Clin Monit Comput. 2017;31(4):805-11. DOI: https://doi.org/10.1007/s10877-016-9906-9 [ Links ]
 Correspondence:
Correspondence:
riera@uol.com.br
Manuscript received: December 2018
Manuscript accepted: May 2019
Version of record online: October 2019














