Servicios Personalizados
Revista
Articulo
Indicadores
Compartir
Journal of Human Growth and Development
versión impresa ISSN 0104-1282versión On-line ISSN 2175-3598
J. Hum. Growth Dev. vol.32 no.2 Santo André mayo/ago. 2022
https://doi.org/10.36311/jhgd.v32.13369
CASE REPORT
Post COVID-19 Disseminated Mucormycosis in a 55-year-old patient in Western Amazon: Case report
Sebastião Afonso Viana Macedo NevesI, II; Lidyane Liadja Souza SilvaI; Rosely Antunes PatzinaIV, V; Cesar Cilento PonceIV, V; Jordy Souza CordeiroIII; Aline Oliveira de AraújoIII; Evelyn Lepka de LimaIV; Irenilce Souza de MatosII, III; Juvencio José Duailibe FurtadoVIII, IX; Letícia Varize PussiIII; Erine Aragão CavalcanteII; Marcos Vinícius da SilvaVI, VII
IUniversidade Federal do Acre, Programa de Graduação em Medicina, Rio Branco, Acre, Brasil
IIHospital das Clínicas de Rio Branco, Rio Branco, Acre, Brasil
IIICentro Universitário Uninorte, Rio Branco, Acre, Brasil
IVInstituto de Infectologia Emilio Ribas, São Paulo, São Paulo, Brasil
VHospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, Departamento de Anatomia Patológica, São Paulo, São Paulo, Brasil
VIInstituto Adolfo Lutz de São Paulo, São Paulo, São Paulo, Brasil
VIIFaculdade de Ciências Médicas e da Saúde da Pontifícia Universidade Católica, Sorocaba, São Paulo, Brasil
VIIIFaculdade de Medicina do ABC, Santo André, São Paulo, Brasil
IXHospital Heliópolis, Chefe do Departamento de Infectologia, São Paulo, São Paulo, Brasil
ABSTRACT
A feared fungal disease surprised and became a warning to severe cases of COVID-19, especially to health professionals involved with the pandemic. Designated as black fungus for public health services in India, where reported data reflects an increase of more than eighty times the expected increase for Rhizopus among the communities. The disease has become even more worrisome due to the high mortality already established as an opportunistic infection, coupled with the reserved prognosis for all those infected and hospitalised by the SARS-CoV-2 severity criteria. This patient, who was submitted to corticosteroid therapy, in an excessive dose, therefore immunosuppressive, developed a severe, disseminated clinical form. It was verified the progression of the lesions and thus the high risk of trans- surgical lethality, or, also, by the insufficiency of conduct in removing the lesions to their satisfaction. Thus, the therapeutic option is the associated use of micafungin, liposomal amphotericin B and isavuconazole for the regressive phase. The patient remains hospitalised with progressive and discrete improvement. Until the opportunity of reevaluation of the surgery by the interspecialty collaboration.
Keywords: Mucormycosis, Zygomycosis, Mucormycosis Post COVID-19, Case report.
RESUMO
Uma temida doença fúngica surpreendeu e se tornou um alerta para casos graves de COVID-19, principalmente aos profissionais de saúde envolvidos com a pandemia. Designado como fungo preto para serviços de saúde pública na Índia, onde os dados relatados refletem um aumento de mais de oitenta vezes o aumento esperado para Rhizopus entre as comunidades. A doença tornou-se ainda mais preocupante devido à alta mortalidade já estabelecida como infecção oportunista, aliada ao prognóstico reservado para todos os infectados e internados pelos critérios de gravidade do SARS-CoV-2. Esse paciente, que foi submetido à corticoterapia, em dose excessiva, portanto imunossupressora, desenvolveu uma forma clínica grave e disseminada. Verificou-se a progressão das lesões e, portanto, o alto risco de letalidade transcirúrgica, ou, ainda, pela insuficiência de conduta na remoção das lesões a contento. Assim, a opção terapêutica é o uso associado de micafungina, anfotericina B lipossomal e isavuconazol para a fase regressiva. O paciente permanece internado com melhora progressiva e discreta. Até a oportunidade de reavaliação da cirurgia pela colaboração interespecialista.
Palavras-chave: Mucormycosis, Zygomycosis, Mucormycosis pós COVID-19, estudo de caso
Authors summary
Why was this study done?
This study was done due to the rarity of the case and its epidemiological importance in Western Amazon, being the first in the state of Acre.
What did the researchers do and find?
After clinical evaluation, imaging exams and biopsies, the patient was diagnosed with disseminated Mucormycosis and evaluated by the medical specialties of ophthalmology, head and neck surgery and otorhinolaryngology. Due to the divergence of surgical conduct and the high lethality of the approach due to the extension of the lesions, drug therapy with amphotericin B and itraconazole was chosen. Therefore, after regression of the lesions, surgical re-evaluation was performed.
What do these findings mean?
These findings show that although Mucormycosis is mainly associated with immunocompromised patients, those previously immunocompetent can develop the disseminated forms, requiring inter-specialty follow-up for an effective therapeutic manage.
INTRODUCTION
The Mucormycosis is caused by filaments of fungi of the Mucoraceae family that is observed in diabetic and immunocompromised patients, in any organ or in the disseminated form, rhino-cerebral, the latter being the most common form. Transplanted, decompensated diabetic patients, patients with metabolic acidosis, burns, persistent neutropenia for more than four weeks or prolonged corticosteroid, immunosuppressants, immunobiologicals for autoimmune diseases, use are also factors risk.
The infection can also occur in an atypical way in immunocompetent patients who have undergone surgery, trauma, or even catheter infections. The gold standard diagnosis is biopsy with histopathological analysis of the fungus, observing various characteristics of the hyphae. Cultures and swabs can be performed, but they have low sensitivity due to inadequate growth of the fungus and probable contamination2.
Symptoms depend on the site of infection, and may include orbital pain and swelling, proptosis, ophthalmoplegia due to injury of the third, fourth and sixth cranial pairs or even seventh pair involvement, causing paresis or paralysis or, less frequently, loss of vision due to optic nerve damage. In addition, sinusitis-like symptoms, otologic and nasopharyngeal cavity lesions are predominant in Mucormycosis1.
The treatment of choice is liposomal amphotericin B at an initial dose of 5mg/kg/day and, after a few months of treatment, broad spectrum azole drugs are used, the most effective being posaconazole 300mg or isavuconazole 200mg, in addition to specific antibiotics if there is a dermatological lesion that requires antibiotic therapy1,3.
The aim of this clinical report is to describe a rare case of epidemiological and clinical importance of chronic Mucormycosis in a male patient from the Western Amazonia. For, there are few cases described in the medical literature from the North Region, this is the first from the state of Acre. Moreover, they are frequently associated with previously immunosuppressed patients, being rare in immunocompetent patients.
Patient information
J.N.C.M. male, married, electrician, natural of Sena Madureira - Acre, from the urban area of Rio Branco - Acre, previously healthy, without comorbidities and family history of 1st degree of systemic arterial hypertension. Was admitted in May 2021 in Intensive Care Unit (ICU) due to Severe Acute Respiratory Syndrome (SARS) by COVID-19, however, did not require orotracheal intubation (OTI).
Diagnostic assessment
The patient was with normal mucous membrane, hydrated, lucid and oriented in time and space, with reduced muscular strength in the upper and lower left limbs and presenting left ocular proptosis (Figure 1).

Cardiac auscultation with normal sounds and regular heart rhythm with two clicks and no murmurs. Respiratory apparatus presented reduced vesicular murmur at bilateral bases, besides computerised tomography (CT) evidencing bilateral pleural effusion (Figure 2), oxygen saturation in room air of 89%. Flat abdomen, flaccid, fluid-air sounds, tympanic to percussion, painless on superficial and deep palpation, Traube's space free. Lower limbs with slight to moderate edema to the left and capillary refill time of less than 3 seconds.

Diagnostic hypothesis
During the ICU stay he was prescribed corticosteroids in immunosuppressive dose, and throughout hospitalisation he evolved with left amaurosis, facial hemiparesis and pulsatile headache, and was initially diagnosed with ischemic stroke, with observation of cavernous sinus thrombosis. After resolution of the respiratory syndrome he was discharged with progressive deescalation of prednisone.
Nevertheless, 20 days after medical discharge, he presented worsening of the headache and sought outpatient care with an infectious disease specialist who ordered tests, including Magnetic Nuclear Resonance (MNR) and opted to hospitalise the patient in the infectious disease sector of the Hospital das Clínicas do Acre for a better diagnostic elucidation.
During hospitalization at the infectious disease ward of the Hospital das Clínicas do Acre, the diagnostic hypothesis of fungal infection - mucormycosis was raised, and an MRI of the skull was requested, which showed extensive involvement of the left maxillary sinus, orbit and facial bones, as well as vascular involvement (Figure 3-4).


Necrotic material was then collected from the facial sinuses, but the analysis initially identified only colonization by Aspergillus sp (Figures 5-6). It was decided to send the anatomopathological material to another pathology service.
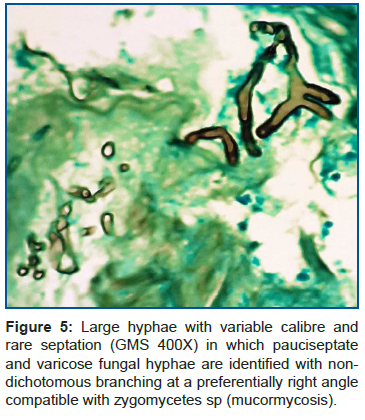

After evaluation of the ophthalmology, head and neck surgery and otorhinolaryngology specialties, there was disagreement as to surgical indication by the department of infectology. The material was then sent to the Emílio Ribas Institute of Infectology (IIIER), where the pathology service of the IIIER/Adolpho Lutz confirmed the pathological diagnosis of Mucormycosis in a re-analysis of the slide (Figure 5-6).
Therefore, the patient was requested to be transferred to the IIER and started on treatment with amphotericin B deoxycholate 50mg for 22 days. Afterwards, he was discharged from the ward on itraconazole and followed up as an outpatient while awaiting transfer, however, the disease continued to progress with worsening of the general clinical picture.
Evolution
On March 11, 2022 the patient was admitted to the Instituto de Infectologia Emilio Ribas (IIIER), in São Paulo, to allow more detailed exams and broad surgical management. Treatment was restarted with Amphotericin B deoxycholate 50mg, but presented intolerance to the side effects, and was replaced by amphotericin B lipid complex at a dose of 5mg/kg/day (350mg/day). A Fibro Naso- Laryngoscopy was carried out by the otorhinolaryngology team of the Clinics Hospital of Sao Paulo without further success in collecting material.
Referred to Hospital Heliópolis on 16/03/2022 for possible collection and gathering of material, as well as evaluation of a possible surgical approach. The slide of the material collected from the biopsy in Acre was transferred to the IIER, where it was reviewed, with the results described below.
Prognostic evaluation
In view of the anatomopathological evidence, the severity of the general clinical picture and the extent of the disease, a joint meeting was held on 24/03/22 with the Head and Neck Surgery, Radiology and Imaging Diagnosis, Otorhinolaryngology, Neurosurgery and Infectology teams of the Hospital Heliópolis, in which it was agreed that a surgical approach was impossible due to the already very advanced and widespread stage of the lesions, notably in the region of the cavernous sinus, with involvement of the carotid artery and point invasion.
It was decided that the risk of the surgical approach would far outweigh the benefits, besides not being technically possible to remove the lesion entirely, a condition that would be fundamental for a curative treatment. Therefore, clinical treatment was chosen, prioritising the return to the state of Acre, the patient was referred for outpatient follow-up with Infectology at the Serviço de Assistência Especializada (SAE) at the Hospital das Clínicas, and given the reserved prognosis, the patient and his wife were informed of the severity of the case. The patient was readmitted to the infectology ward, and the adoption of a new therapeutic protocol, based on the latest international clinical evidence available, was decided together with the patient.
The adopted scheme has an initial phase with the association of Micafugin and liposomal Amphotericin B, aiming at the regression phase of the infectious picture in which the maintenance of the treatment with isolated Isavuconazole will be done. Therefore, we seek a therapeutic proposal with clinical treatment, and possible reevaluation of a new surgical approach later. In May 2022 the patient underwent a cranial CT angiography, showing the persistence of the extensive lesions (Figure 7).

Written informed consent was obtained from the patient for publication of the results and details of this case.
DISCUSSION
An increase in the number of cases of mucormycosis was observed worldwide during the COVID-19 pandemic, with India standing out in the number of cases, as eighty times more cases of post-COVID-19 Mucormycosis are attributed there than in the rest of the world, largely due to the mucorales being opportunistic fungi4. In Brazil, according to data from the Ministry of Health, in 2021, until October 4, 90 cases of mucormycosis were recorded, of which 47 of these patients were diagnosed with COVID- 195.
Like other endemic mycoses, mucormycosis is not treated as a compulsorily notifiable disease by the Ministry of Health, so epidemiological data do not reflect the total number of patients with the infection. Moreover, the main factor for the development of the disease is the presence of comorbidities such as diabetes mellitus or immunosuppression states5. From the clinical point of view, the most common presentation of the disease is the rhino- orbital-cerebral form, affecting the nasal mucosa, paranasal sinuses, palate and brain. Other less affected systems are skin, lung and gastrointestinal tract. In addition, it presents trophism by the vascular system, which ends up facilitating its ascension to tissues and organs, producing inflammation and necrosis6. Commonly, when invasion of the Central Nervous System occurs, it can course with hemiparesis/hemiplegia or paresis, besides ophthalmoplegia and periorbital edema, symptoms presented by the patient of the case, and which led to the diagnosis, initially, of CVA.
The patient reported here presented with ARDS due to infection by the SARS-CoV-2 virus, having received immunosuppressive doses of corticosteroids, outside the inflammatory phase of the viral disease. Therefore, it is possible to attribute the correlation between immunosuppressive therapy and susceptibility to mucorales infection, since the patient in this case was previously healthy.
Due to the impossibility of surgical management in the state, it was necessary to transfer the patient to São Paulo. Out-of-Domicile Treatment (OHT) was requested by the Unified Health System, regulated by SAS Administrative Rule N° 055, of February 24, 1999. The request was refused by the state and the patient had to take legal action against the request, which was later granted. However, this was detrimental to proper clinical management.
The drug of choice for the treatment of Mucormycosis is liposomal Amphotericin B, at an initial dose of 5mg/kg/day, and the intravenous route is the best for infection control. After this period, the use of azolic is suggested. Among the most effective are posaconazole, at an initial dose of 300mg 12/12h on the first day, and then once a day. Isavuconazole 200mg of 8/8 hours as an attack dose for 6 days can also be administered. These azoles can also be used intravenously reserved for patients who do not respond well to amphotericin B7, 8.
Recent clinical data reveal that among the antifungal drugs used, such as fluconazole, voriconazole, flucytosine, itraconazole, terbinafine, the drugs that have proven most reliable and effective in reducing and extinguishing the fungal infection are isavuconazole and posaconazole. Recent publications also highlight as solid and with distinct prognostic perspective, the association with micafungin, liposomal amphotericin B, and later, oral isavuconazole for the regressive phase.
However, despite studies showing that, when combined therapy was used, there was no difference in prognosis, the combination is still preferred because of the good results in practice8.
The debates among the medical multi- specialties allowed an adequate therapeutic choice aiming to decrease the surgical mortality inherent to the proposed procedure.
CONCLUSION
This case report promotes a discussion about the therapeutic approach to a rare disease in an immunocompetent patient with no previous comorbidities, but who, after interprofessional evaluation, presented an unfavorable prognosis due to the extension of the lesions. An innovative pharmacological treatment was initiated with good therapeutic response and progressive regression of the lesions, and the patient was referred again for surgical reevaluation. Therefore, with favorable prospects of surgical intervention with exeresis of the lesions and improved prognosis.
REFERENCES
1.UGURLU, S K. SELIM, S. KOPAR, A. SONGU, M. (2015). Rhino-orbital mucormycosis: Clinical findings and treatment outcomes of four cases. 45. Turkish Journal of Ophthalmology: Galenos Publishing, 2015. Disponível em: https://doi.org/10.4274/tjo.82474. Acesso em: 13 de maio de 2022. [ Links ]
2.LEWIS, R. Agents of Mucormycosis (Microbiology). Pulmonology Advisor, 2013. Disponível em: https://www.pulmonologyadvisor.com/home/decision-support-in-medicine/infectious-diseases/agents-of-mucormycosis-microbiology/. Acesso em: 13 de maio de 2022. [ Links ]
3. ABIDI, M Z. SOHAIL, M R. et al. Stability in the cumulative incidence, severity and mortality of 101 cases of invasive mucormycosis in high-risk patients from 1995 to 2011: A comparison of eras immediately before and after the availability of voriconazole and echinocandin-amphotericin combination therapies. 57. Mycoses: Wiley, 2014. Disponível em: https://doi.org/10.1111/myc.12222. Acesso em: 13 de maio de 2022. [ Links ]
4.NISHIOKA, S A. Mucormicose e COVID-19 na Índia. UNASUS, 2021. Disponível em: https://www.unasus.gov.br/especial/covid19/markdown/411#:~:text=J%C3%A1%20antes%20da%20pandemia%20a,0%2C06%20casos%20por%20 [ Links ]
5.100.000. Acesso em: 13 de maio de 2022. Mucormicose (Fungo Negro). Ministério da Saúde, 2021. Disponível em: https://www.gov.br/saude/pt-br/assuntos/saude-de-a-a-z/m/mucormicose-fungo-negro-1. Acesso em:13 de maio de 2022. [ Links ]
6.FUCHS, A. PORTUGAL, J. GONÇALVES, P. Fiocruz é referência nacional para o diagnóstico da mucormicose. Fiocruz, 2021. Disponível em: https://portal.fiocruz.br/noticia/fiocruz-e-referencia-nacional-para-o-diagnostico-da-mucormicose. Acesso em: 13 de maio de 2022. [ Links ]
7.Doenças infecciosas Agentes de Mucormicose (Microbiologia), 2022. https://www.google.com/url?sa=t&source=web&rc t=j&url=https://www.saude.go.gov.br/files//conecta-sus/produtos-tecnicos/I%2520I-%25202021/COVID-19%2520-%2520Fungo%2520negro%2520(mucormicose).pdf&ved=2ahUKEwji3NKyupH4AhUiRLgEHXvyCmsQFnoECBIQAQ&usg=AOvVaw3LWAh8Cgy20Rviur8Ao93y. Acesso em: 13 de maio de 2022. [ Links ]
8.GARY, M C. Mucormicose (zigomicose). UpToDate, 2022. Acesso em: 13 de maio de 2022. [ Links ]
 Correspondence:
Correspondence:
Sebastião Afonso Viana Macedo Neves
sebastiao.viana@ufac.br
Manuscript received: may 2021
Manuscript accepted: december 2021
Version of record online: june 2022














