Servicios Personalizados
Revista
Articulo
Indicadores
Compartir
Estudos de Psicologia (Natal)
versión impresa ISSN 1413-294Xversión On-line ISSN 1678-4669
Estud. psicol. (Natal) vol.23 no.3 Natal jul./set. 2018
https://doi.org/10.22491/1678-4669.20180020
DOI: 10.22491/1678-4669.20180020
PSYCHOBIOLOGY AND COGNITIVE PSYCHOLOGY
Impact of Alzheimer's disease related anosognosia in caregivers' quality of life
Impacto da Anosognosia Associada à Demência de Alzheimer na Qualidade de Vida de Cuidadores
Impacto de Anosognosia asociada a la demencia de Alzheimer en la calidad de vida de cuidadores
Ricardo Mendes Gomes PereiraI; Wânia Cristina de SouzaII; Marta Kerr PontesIII; Ana Idalina de Paiva SilvaIV
ICorpo de Bombeiros Militar do Distrito Federal
IIUniversidade de Brasília
IIIRede SARAH de Hospitais de Reabilitação
IVUniversidade Federal de Goiás
ABSTRACT
Alzheimer's disease (AD) has anosognosia as one of its symptoms, defined as a change in the individual's ability to judge their difficulties, and is observed as having a significant impact on quality of life of caregivers. This study evaluated the impact of anosognosia related to AD in quality of life (QoL) of caregivers. Fifty AD patients were evaluated through the Addenbrooke's Cognitive Examination, Dementia Questionnaire – expanded, while caregivers were evaluated using the Scale of QoL in AD and Dementia Questionnaire (caregiver versions). We observed that caregivers of patients with signs of anosognosia had lower scores on QoL and these patients had worse cognitive scores. Anosognosia and QoL were negatively correlated, as QoL and cognitive functioning. Controlling for cognitive functioning, we observed that anosognosia has a greater impact on QoL in individuals with more severe cognitive impairments.
Keywords: alzheimer disease, quality of life, caregivers, anosognosia.
RESUMO
A Demência de Alzheimer (DA) apresenta como um dos sintomas a anosognosia, um prejuízo na capacidade de o indivíduo julgar alterações decorrentes da doença. Relaciona-se a diversos comprometimentos cognitivo/comportamentais e é apontada como tendo significativo impacto sobre a qualidade de vida (QV) dos cuidadores. Avaliamos o impacto da anosognosia relacionada à DA sobre QV de cuidadores. Foram avaliados 50 pares paciente-cuidador com Exame Cognitivo de Addenbrooke, Questionário de Demência Ampliado e Escala de QV na DA. Observamos que cuidadores de pacientes com sinais de anosognosia apresentavam menores escores de QV, sendo que pacientes com sinais de anosognosia apresentam pior desempenho cognitivo. Escores de anosognosia e QV apresentaram correlação negativa, enquanto QV e quadro cognitivo apresentou correlação positiva. Controlando o funcionamento cognitivo, observamos que a anosognosia apresenta maior impacto na QV em indivíduos com quadro cognitivo mais grave.
Palavras-chave: demência de alzheimer, qualidade de vida, cuidadores, anosognosia.
RESUMEN
Anosognosia es uno de los síntomas de la demencia de Alzheimer (AD), y se considera que tiene un impacto significativo en la calidad de vida (QOL) de los cuidadores. Evaluamos el impacto de la anosognosia relacionada con AD en los cuidadores de calidad de vida. Hubo 50 pares paciente y su cuidador con el examen cognitivo de Addenbrooke, Cuestionario Ampliado de y Escala de calidad de vida. Hemos observado que los cuidadores de pacientes con signos anosognosia tenían menores puntuaciones de calidad de vida con los pacientes con peor rendimiento cognitivo. Anosognosia y la calidad de vida mostraron una correlación de negativa, mientras que la calidad de vida y el marco cognitivo presentaron correlación positiva. Controlando el funcionamiento cognitivo, observamos que la anosognosia tiene mayor impacto en la calidad de vida en pacientes con marco cognitivo más severo.
Palabras clave: enfermedad de alzheimer, calidad de vida, cuidadores, anosognosia.
The first description of what we now call Alzheimer's disease (AD) was made in 1906, by the neuropathologist Alois Alzheimer. He described a fifty-one year old woman, that presented what at the time was called 'presenile dementia'. The patient, Auguste Deter, suffered from hallucinations, memory deficits and changes of her sleep pattern, with nocturnal agitation. Initially described as a pathology that only occurred in individuals under sixty five year old, today AD is considered to be the most frequent cause of dementia in individuals over 65, being directly responsible for 50% to 75% of cognitive decline in this age group (Rowland, Pedley, & Merritt, 2009), and with the incidence of 13.8 of 1000 habitants each year in Brazil (Charchat-Fichman, Caramelli, Sameshima, & Nitrini, 2005). The disease is defined by neurodegenerative symptoms, characterized by progressive dementia caused by loss of neurons and synapses in the cerebral cortex and certain subcortical regions, with both amyloid plaques and neurofibrillary tangles being identified in specific brain regions in greater number than in normal ageing (Honig, Small, & Mayeux, 2015).
One of the first signs of AD are difficulties to store new information, with the memory preserved for past events. As the disease progress, language impairments, apraxia, and executive functioning deficits may appear, causing significant difficulties with daily living activities and social functioning (Rowland et al., 2009). Neuropsychiatric changes, as sleep pattern changes, psychomotor agitation and apathy may be part of the symptoms.
DA prevalence in Brazil is estimated to be 1.1 million individuals (Costa et al., 2013). There is no statistics of the percentage of individuals that are institutionalized or living with their families, but a large percentage of the patients are taken care by family members in the course of the disease. There are previous studies that shows that caregivers of dementia patients shows increased prevalence of anxiety and depressions symptoms, more frequent doctor visits, weight loss, lower quality of life (QoL) (Ho, Chan, Woo, Chang, & Sham, 2009), increased risk of developing intense depression symptoms (Schoenmakers, Buntinx, & Delepeleire, 2010), with worst results being from caretakers of patients with lowest functional independence scores (Pinto, Barbosa, & Ferreti, 2009).
Etters, Goodall, and Harrison (2008), reviewing influencing factors of caregivers' burden, showed that the necessity of offering specialized care is related to adverse effects in the caregiver's health, and the earlier necessity for institutionalization. In AD, decreased caregiver's QoL is related to the financial burden and the behavioral costs of family routine changes (Theofilou, 2012). It is also found that specific AD characteristics impact caregivers QoL, with aggressiveness, apathy, patient irritability and caregiver's age are factors that influence care perceived burden (Conde-Sala et al., 2016; Turró-Garriga et al., 2008).
Besides cognitive and behavioral symptoms observed in AD, the patient's lack of ability to perceive his own limitations can usually be observed. This auto perception deficit is related to several cognitive and behavioral deficits and is followed by difficulties on treatment-related decision taking (Gambina et al., 2013), adherence to medicine intake (Rosen, 2011), can limit the patients engagement to rehabilitation activities that could potentially help him (Prigatano, 2009), and increases the risk of accidents (Pachana & Petriwskyj, 2006). This symptom is called anosognosia.
Anosognosia (from the greek nosos - disease and gnosis - knowledge), is usually used to refer to an individual's inability to perceive its own difficulties and was initially described by Babinski (1914) as the inability of the subject to perceive changes of sensitivity and motor function after brain injury. Different neurological conditions show similar symptoms as those observed by Babinski, for which the term anosognosia started to be used. Nowadays, the term is used in all situations in which individuals are unaware of theirdisabilityor cannot perceive the extent of their difficulties (Marková & Berrios, 2014; Prigatano, 2010).
In the context of Alzheimer's disease (AD) anosognosia is considered as one of its symptoms, and its prevalence rate is believed to be between 20% and 81% of diagnosed patients (Migliorelli et al., 1995; Sanz et al., 2015; Starkstein, 2014). It is observed as being correlated with the severity of the condition (Perrotin et al., 2015; Starkstein, Jorge, Mizrahi, & Robinson, 2006), and it's shown to have a positive correlation with the severity of dementia, age of the patient at symptoms onset and the presence of behavioral disinhibition (Lautenschlager, 2015; Mak, Chin, Ng, Yeo, & Hameed, 2015; Marková, Clare, Wang, Romero, & Kenny, 2005; Mograbi & Morris, 2014).
As for the impact of anosognosia on the QoL of caregivers, Seltzer, Vasterling, Yoder and Thompson (1997) point out that the lack of perception of memory deficits leads to increased caregiver burden. The presence of anosognosia is observed as a factor that increases the physical stress, social isolation, dependence and stress related to patient care (Turró-Garriga, & López-Pousa, 2012).
However, there is no consensus in the study of anosognosia in AD if the insight impairment is domain specific or a general impairment in judgment (Avondino & Antoine, 2015; Kashiwa, Kitabayashi, & Narumoto, 2005). In an attempt to verify this issue, assessing the individual's ability in judging their performance in different areas, Leicht, Berwig and Gertz (2010) proposed an instrument whose objective was to compare the anosognosia related to the ability to perform activities of daily living, memory, apathy and attention. The results showed that patients with AD had difficulty judging performance in all areas, overestimating their performance when compared to the evaluation of caregivers. However, the comparison between domains showed differences in the intensity of anosognosia, with anosognosia related to cognitive functioning shown to have a positive correlation with deficits in recent memory.
Although there is no methodological consensus on the best way to evaluate anosognosia in AD, the evaluation by comparing the assessment of the potential perceived by the patient and the one given by their caregivers is the most common method (Sousa, Santos, Brasil, & Dourado, 2011). In a review of the methodological difficulties on the research of anosognosia, Cocchini, Beschin, Sala, & Della (2012) suggested that studies on anosognosia should explore different aspects of the symptom and its intensity on different domains, as these data could be used to better characterize the possible reasons for the lack of insight. The discrepancy analysis could follow these guidelines, using protocols to evaluate the functionality potential on activities of daily living. However, the presence of neuropsychiatric symptoms, mood disorders, and the caregiver perceived burden could influence the evaluation of the patient's performance by his caregiver (Conde-Sala et al., 2013).
We were not able to find attempts to verify the relationship between anosognosia regarding the perception of cognitive difficulties and behavioral alterations of the individual with AD and the caregiver's QoL. We believe that even though the most striking feature of AD is memory loss, aspects related to the patient's difficulty in perceiving their own deficits could impact negatively caregiver's QoL, regardless of cognitive deficits of the patient.
Our main objective was to verify the correlation between the QoL of caregivers of individuals with AD and the presence of anosognosia in e individuals, to analyze this correlation, and if we could observe differences on how anosognosia's two domains (cognitive functioning and behavioral changes) are correlated with caregivers QoL. Our hypothesis was that the discrepancy between the perception of the difficulties between patients and their caregivers would be correlated with caregivers QoL, regardless of the cognitive status of the patient.
Method
Participants
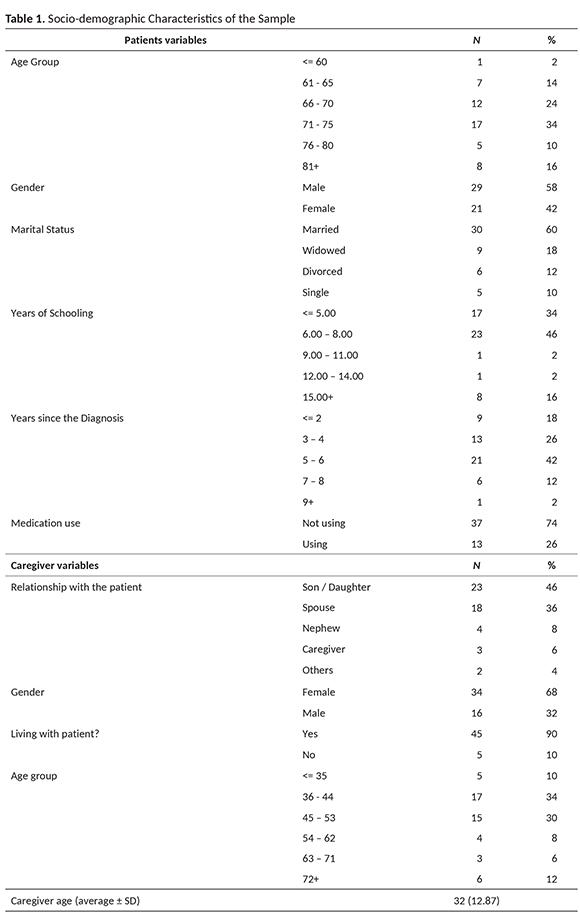
A hundred participants were part of the study. Fifty of those were patients admitted to the Cognitive Decline Program of the International Center for Neuroscience and Rehabilitation, one of the units of the SARAH Network Rehabilitation Hospitals in Brasília, Brazil between September to December 2013. All patients met diagnostic criteria for AD, according to the Diagnostic and Statistical Manual of Mental Disorders – DSM-V (American Psychiatric Association, 2013), without associated vascular comorbidities. The other 50 participants were their caregivers.
Materials and instruments
The following instruments were used:
Addenbrooke Cognitive Examination-Revised (ACE-R) – This examination seeks to accomplish both the detection of early stages of dementia, as well as differentiate its subtypes. It evaluates six cognitive domains: orientation, attention, memory, verbal fluency, language, and visuospatial skills in a score from zero to one hundred. It is validated for the Brazilian population, with normative data for healthy elderly and a proposed cut-off of 79 points, with good sensitivity (100%) and specificity for AD (79%), according to Carvalho (2009).
Dementia Questionnaire - Extended (QD) – This questionnaire is the translation of the instrument proposed by Migliorelli et al. (1995), to evaluate the presence of anosognosia by evaluating the discrepancy of the patient and family assessments between forty-two behaviors divided into two sections. The 'A' section is specific to intellectual functioning, while the 'B' section evaluates behavioral changes. The evaluation takes place on a four-point Likert scale by setting the frequency of occurrence of each behavior as never, sometimes, often, and always. The questionnaire is presented in a version for the patient and one for the caregiver. The translation presented by Almeida and Crocco (2000) proposed twelve additional items to evaluate basic functions of daily living and allow more extensive evaluation of behavior changes. To evaluate differences between groups with and without significant signs of anosognosia associated with ADwe also used the cut-off proposed by Migliorelli et al. (1995).
Quality of Life Scale in AD - The Quality of Life Scale in AD is composed of 13 items evaluated in a Likert scale of four points, where the highest rates indicate better QoL. It is validated for use in Brazil (Novelli, 2006), and has good reproducibility and internal consistency (α = 0.82) (Novelli, 2003). In this study, we used the caregiver/family member version (Quality of Life Scale in Alzheimer's Dementia, caregiver Version/family - CQdV).
Neuropsychiatric Inventory (NPI) – The NPI (Cummings et al., 1994) is an instrument that measures 12 symptoms usually observed in dementia: delusions, hallucinations, agitation, depression / dysphoria, anxiety, euphoria, apathy, disinhibition, irritability / lability, abnormal motor behavior without purpose, sleep disorders and nocturnal behavior, eating disorders and eating habits. They are assessed for their frequency and intensity, ranging 0-144 points.
Procedure
Individuals admitted to the Cognitive Decline Program of the International Center for Neuroscience and Rehabilitation are initially referred for admission by a multidisciplinary team. At the admission, organic causes for the reported behavioral and cognitive changes are investigated. Supplementary examinations are then requested, aiming to exclude treatable causes of cognitive decline. After this admission, patients are referred for neuropsychological evaluation in a separate, soundproof room and controlled distractor stimuli. It is requested that the primary caregiver join the evaluation, since external confirmation of data can be necessary due to the cognitive impairment.
The patients and caregivers were invited to the study prior to the neuropsychological evaluation. Those who accepted the invitation were asked to fill the Informed Consent. Afterward, the QD was administered to the patient. Then the caregiver was directed to a nearby room to answer the CQdV and the caregiver's version of QD. After application of QD and CQdV, the neuropsychological evaluation was conducted with ACE-Rand NPI. The total time of the described procedures was about two hours.
The research project was approved by the Ethics Committee on Research with Human Beings - CEP-FS / UnB, of the Faculty of Health Sciences of the University of Brasilia (UnB) and was also approved by the Research Ethics Committee of the SARAH Network Rehabilitation Hospitals.
Data analysis
Data wereanalyzed using SPSS - Statistical Package for the Social Sciences version 20, and Pearson correlation analysis was performed between the obtained measurements.
Results
Comparing Scores of the Scales Used Between Groups
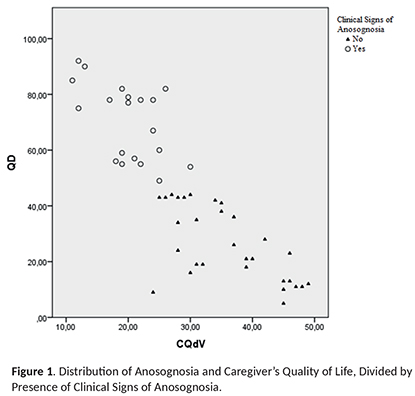
When comparing the results of measurements of CQdV and ACE-R, taking into account the cut proposed by Migliorelli et al. (1995) among patients with signs or absence of anosognosia, it is observed that caregivers of individuals with Anosognosia symptoms had significantly lower scores in CQdV (With clinical signs of anosognosia = 20.0 ± 5.1; Without clinical signs of anosognosia = 35.9 ± 7.8; p < 0.01). Patients with signs of anosognosia also showed lower scores in the cognitive assessment (With clinical signs of anosognosia = 49,6 ± 14,0; Without clinical signs of anosognosia = 58.2 ± 12.3; p < 0.05), suggesting that the presence of anosognosia is correlated with lower caregiver's quality of life scores and patients' worse cognitive functioning. The correlation between QD and CQdV can be seen in Figure 1, which shows the distribution of QD and CQdV scores, according to the cut for signs of Anosognosia of clinical importance (Migliorelli et al., 1995).
Comparing demographic variables and QD scores, patients who showed anosognosia signs had significantly more years since the diagnosis (With clinical signs of anosognosia = 5,5 ± 2,0; Without clinical signs of anosognosia = 3.9 ± 1.8; p < 0.01).
Correlations Between Measures
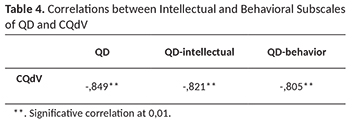
The data in Table 2 show the correlations between measurements taken from QD, ACE-R, and CQdV. Significant negative correlation (-.849, p = 0.05) between the scores of anosognosia and the assessment of QoL was observed, showing that higher scores anosognosia are correlated with the lower QoL perceived by caregivers. Taking into account the subscales of QD, we observed that both intellectual (-.821) and behavioral domains (-.805) are related to lower QoL.
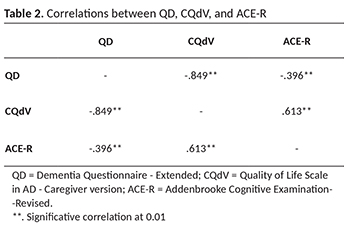
We also found significant correlations between the cognitive functioning, assessed by the ACE-R and QOL (.613, p < 0.01) with better cognitive performance related to better QoL.
Correlations between Anosognosia Domains and Other Measures
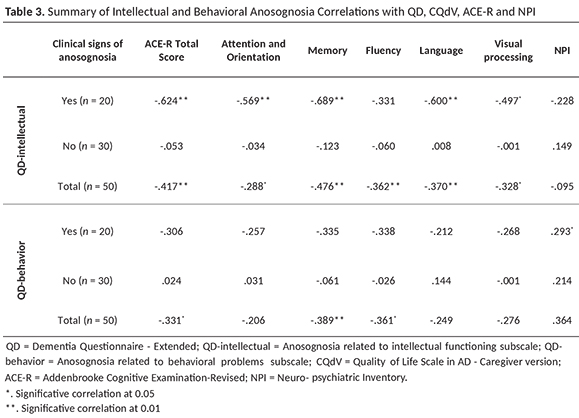
As expected, given the correlation between the total score of anosognosia and the total score of ACE-R seen in Table 2, correlations were found between the intellectual and behavioral domains of anosognosia (n = 20) with the total score of ACE-R, with a higher correlation between the intellectual domain.
When we consider the cut proposed by Migliorelli et al. (1995) for QD, it is possible to observe in Table 3 that the correlation between the domains of cognitive and behavioral anosognosia differs in the group that showed significant signs of anosognosia. The intellectual domain of anosognosia had a significant negative correlation with the total cognitive score and four of ACE-R subscales (fluency showed no significant correlation), but not with the NPI score. In contrast, anosognosia related to behavior changes was not correlated with the total score of ACE-R or any of its subscalesbut was correlated with NPI scores.
Correlations between Anosognosia Domains and Caregivers Qol
The data in Table 4 show that the two domains of anosognosia valued at QD, as the presence of cognitive and behavioral changes, had a significant negative correlation with QOL scores assessed by the caregiver.
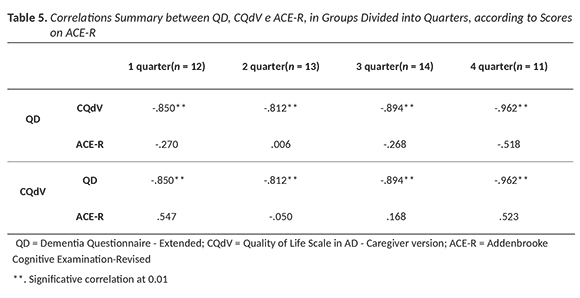
Correlations Between QD, CQdV,and ACE-R Divided into Groups According to Cognitive Scores
Patients were divided into four groups according to their scores on the ACE-R so that it could assess the correlations between the QD and CQdV in different cognitive performances. The data of Table 5 show that, regardless of the cognitive status of the patient, a significant negative correlation between anosognosia assessment scores (QD) and evaluation of caregivers QoL (CQdV) could be observed, with higher correlation in the group with worse scores on cognitive assessment (ACE-R). In this analysis, no correlation was found between the scores of ACE-R and CQdV.
Discussion
The aim of this study was to increase understanding of the relationship between anosognosia and caregiver QoL, focusing in two domains of anosognosia.
Despite knowing that the prevalence of anosognosia varies according to the severity and cognitive impairment of individuals, our results showed that even though correlation between caregiver QoL and the cognitive functioning of patients was found (consistent with previous researches - Ho et al., 2009; Schoenmakers et al., 2010), we also found a significant negative correlation between the symptoms of anosognosia and QOL of caregivers, with stronger correlation on patients with worst cognitive scores. This analysis aimed to answer one of the questions in our study, if anosognosia was correlated with caregivers QoL regardless of patients' cognitive status. There have been no previous studies that performed this analysis, with studies correlating the presence of anosognosia with caregiver burden, but without evaluating the relationship of anosognosia with cognitive functioning (Turró-Garriga & López-Pousa, 2012).
Understanding that anosognosia is correlated with caregivers QoL even when patients have only mild cognitive deficits suggests that the guidelines offered to family members, in a rehabilitation program, should think about including anosognosia in their orientations. Rehabilitation in AD is generally understood as based on the educational process of caregivers and family members, trying to improve their quality of life and decrease care related burden (Prigatano & Morrone-Strupinsky, 2010). Understanding anosognosia as a clinically relevant symptom makes it necessary to understand the nature of anosognosia in AD, so that the professionals can develop a program focused on the individual demands (Clare, 2004).
In AD, where we do not expect cognitive recovery, and whose rehabilitation strategies aimed at anosognosia are related to environmental changes and family orientation, to understand how anosognosia works can actually help the planning stages of rehabilitation interventions to lower the possibility of patient engagement in risk behaviors. These situations, related to daily living activities, is identified as a source of burden and loss of quality of life of caregivers and family members (Etters et al., 2008; Seltzer et al., 1997; Turró-Garriga & López-Pousa, 2012; Vellone, Piras, Talucci, & Cohen, 2008).
Our results showed that even in patients with mild cognitive impairment, those who have some degree of awareness about their difficulties (impaired perception, but not having yet fully anosognosia) should be targeted for interventions to decrease problems due to the presence of anosognosia, aiming at QoL gain for caregivers. Reviews have shown effectiveness of rehabilitation programs aimed at providing psychosocial interventions (Brodaty, Green, & Koschera, 2003; Kelleher, Tolea, & Galvin, 2015; Spijker et al., 2008), with results indicating that this type of intervention entails gain in QoL, decreased caregiver burden and reduces the chance of institutionalization of the patient.
At the group analysis, it was observed that patients with anosognosia scores above the clinical cut proposed by Migliorelli et al. (1995) had worse cognitive performance, with a higher degree of correlation observed in the cognitive domain of anosognosia. This result is consistent with other studies, where anosognosia scores are negatively correlated with cognitive status (Charchat-Fichman et al., 2005; Kashiwa et al., 2005; Reed, Jagust, & Coulter, 1993; Satler & Tomaz, 2013; Turró-Garriga & López-Pousa, 2012; Zanetti et al., 1999).
The relationship of anosognosia and cognitive functioning can be understood knowing that patients with longer diagnosis had more prominent signs of anosognosia: as the disease progress, cognitive condition worsens, causing damage in several functions, including the evaluation of the patient own difficulties.
One of the objectives of this study was to verify the possibility of identifying different domains of anosognosia, related to cognitive functioning and the presence of behavioral changes. In our study, we observed that in the group with higher scores of anosognosia, the different domains could be observed. The cognitive domain of anosognosia was negatively correlated with the cognitive status of the patient, while the behavioral domain showed no such correlation. Conversely, the behavioral domain was positively correlated with the presence of neuropsychiatric symptoms, while the cognitive domain did not show this correlation.
Our results suggest that in individuals who have higher anosognosia scores, the two anosognosia domains assessed by our chosen scale could be observed. However, the results also showed a significant negative correlation between anosognosia and QoL of caregivers, observed both in the cognitive and behavioral domains, suggesting that no matter in what domain anosognosia is shown to be more evident, there is a negative correlation with QoL of the caregiver.
Understanding that the two evaluated domains are also correlated with lower QoL makes the distinction between these domains important for planning interventions focused on the individual demands, creating strategies to reduce the impact of anosognosia in specific situations where the presence of this could put the patient at risk.
Although research is still needed to fully understand anosognosia in AD, the evidence that anosognosia is correlated with caregivers even when patients have only mild cognitive deficits, the presence of symptoms of anosognosia correlates negatively with caregivers QoL shows that interventions focused on solving problems situations associated with anosognosia could positively impact caregivers QoL. Considered that in our study 90% of caregivers were living with the patients, interventions with this focus could possibly reduce the burden of AD care, delaying the need for institutionalization (Alvarez & Vigil, 2006).
The main limitation of this study was not doing a careful investigating of executive functions. We chose to use the domains of general cognitive status and behavioral changes evaluated by QD, but evidence can be found linking anosognosia with executive functioning. Future studies could evaluate the relationship between executive functioning and anosognosia in AD, and its impact on caregivers QoL.
References
Almeida, O., & Crocco, E. (2000). Percepção dos déficits cognitivos e alterações do comportamento em pacientes com doença de Alzheimer. Arquivos de Neuropsiquiatria, 58(2-A), 292-299. Retreived from http://www.scielo.br/pdf/%0D/anp/v58n2A/58n2aa15.pdf [ Links ]
Alvarez, M., & Vigil, P. (2006). Factores asociados a la institucionalización de pacientes con demencia y sobrecarga del cuidador. Revista Del Ministério do Trabajo y Assuntos Sociales, (60), 129-147. Retrieved from http://www.empleo.gob.es/es/publica/pub_electronicas/destacadas/revista/numeros/60/Est11.pdf [ Links ]
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [ Links ]
Avondino, E., & Antoine, P. (2015). Heterogeneity of cognitive anosognosia and its variation with the severity of dementia in patients with Alzheimer's disease. Journal of Alzheimer's Disease, 50(1), 89-99. doi: 10.3233/JAD-150496 [ Links ]
Babinski, J. (1914). Contribution à l'étude des troubles mentaux dans l'hémiplégie organique cérébrale (anosognosie). Revue Neurologique, (27), 845-848. [ Links ]
Brodaty, H., Green, A., & Koschera, A. (2003). Meta-analysis of psychosocial interventions for caregivers of people with dementia. Journal of the American Geriatrics Society, 51(5), 657-664. doi: 10.1034/j.1600-0579.2003.00210.x/full [ Links ]
Carvalho, V. M. (2009). Addenbrooke's Cognitive Examination - Revised (ACE-R): adaptação transcultural, dados normativos de idosos cognitivamente saudáveis e de aplicabilidade como instrumento de avaliação cognitiva breve para pacientes com doença de Alzheimer provável leve (Dissertação de Mestrado). Faculdade de Medicina da Universidade de São Paulo, São Paulo. [ Links ]
Charchat-Fichman, H., Caramelli, P., Sameshima, K., & Nitrini, R. (2005). Declínio da capacidade cognitiva durante o envelhecimento. Revista Brasileira de Psiquiatria, 27(1), 79-82. doi: 10.1590/S1516-44462005000100017 [ Links ]
Clare, L. (2004). The construction of awareness in early-stage Aílzheimer's disease: A review of concepts and models. The British Journal of Clinical Psychology / The British Psychological Society, 43(Pt 2), 155-75. doi: 10.1348/014466504323088033 [ Links ]
Cocchini, G., Beschin, N., & Sala, S. D. (2012). Assessing anosognosia: A critical review. Acta Neuropsychologica, 10(3), 419-443. Retrieved from http://eprints.gold.ac.uk/7614/1/Cocchini_et_al_2012_Acta NPSgica.pdf [ Links ]
Conde-Sala, J. L., Reñe-ramirez, R., Torró-Garriga, O., Gascón-Vayarri, J., Campdelacreu-Fumadó, J., Juncadella-Puig, M., & Garre-Olmo, J. (2013). Severity of dementia, anosognosia, and depression in relation to the quality of life of patients with Alzheimer disease: Discrepancies between patients and caregivers. The American Journal of Psychiatry, 22(2), 138-147. Retrieved from: http://www.sciencedirect.com/science/article/pii/S1064748112000036 [ Links ]
Conde-Sala, J. L., Turró-Garriga, O., Piñán-Hernández, S., Portellano-Ortiz, C., Viñas-Diez, V., Gascón-Bayarri, J., & Reñé-Ramírez, R. (2016). Effects of anosognosia and neuropsychiatric symptoms on the quality of life of patients with Alzheimer's disease: a 24-month follow-up study. International Journal of Geriatric Psychiatry, 31(2), 109-19. doi: 10.1002/gps.4298 [ Links ]
Costa, A. F.; Chaves, M. L. F.; Picon, P. D.; Krug, B. C.; Gonçalves, C. B. T.; Amaral, K.M., ... Ronsoni, R. M. (2013). Doença de Alzheimer. In Ministério da Saúde (Ed.), Protocolos clínicos e diretrizes terapêuticas. (Vol. 2, 2nd ed., pp. 147-167). Brasília: Editora MS. [ Links ]
Etters, L., Goodall, D., & Harrison, B. E. (2008). Caregiver burden among dementia patient caregivers: A review of the literature. Journal of the American Academy of Nurse Practitioners, 20(8), 423-8. doi: 10.1111/j.1745-7599.2008.00342.x [ Links ]
Gambina, G., Bonazzi, A., Valbusa, V., Condoleo, M. T., Bortolami, O., Broggio, ... Moro, V. (2013). Awareness of cognitive deficits and clinical competence in mild to moderate Alzheimer's disease: Their relevance in clinical practice. Neurological Sciences, 35(3), 385-390. doi: 10.1007/s10072-013-1523-5 [ Links ]
Ho, S. C., Chan, A., Woo, J., Chong, P., & Sham, A. (2009). Impact of caregiving on health and quality of life: A comparative population-based study of caregivers for elderly persons and noncaregivers. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 64(8), 873-9. doi: 10.1093/gerona/glp034 [ Links ]
Honig, L. S., Small, S. A., & Mayeux, R. (2015). Alzheimer disease. In Merritt's Neurology (pp. 713-735). New York: Wolters Kluwer Health. [ Links ]
Kashiwa, Y., Kitabayashi, Y., & Narumoto, J. (2005). Anosognosia in Alzheimer's disease: Association with patient characteristics, psychiatric symptoms and cognitive deficits. Psychiatry and Clinical Neurosciences, 59(6), 697-704. Retrieved from http://psychiatryonline.org/article.aspx?articleid=104273 [ Links ]
Kelleher, M., Tolea, M. I., & Galvin, J. E. (2015). Anosognosia increases caregiver burden in mild cognitive impairment. International Journal of Geriatric Psychiatry, 31(7), 799-808. doi: 10.1002/gps.4394 [ Links ]
Lautenschlager, N. T. (2015). Awareness of memory deficits in subjective cognitive decline, mild cognitive impairment, Alzheimer's disease and Parkinson's disease. International Psychogeriatrics, 27(3), 355-6. doi: 10.1017/S1041610214002786 [ Links ]
Leicht, H., Berwig, M., & Gertz, H.-J. (2010). Anosognosia in Alzheimer's disease: The role of impairment levels in assessment of insight across domains. Journal of the International Neuropsychological Society, 16(3), 463-73. doi: 10.1017/S1355617710000056 [ Links ]
Mak, E., Chin, R., Ng, L. T., Yeo, D., & Hameed, S. (2015). Clinical associations of anosognosia in mild cognitive impairment and Alzheimer's disease. International Journal of Geriatric Psychiatry, 30(12), 1207-14. doi: 10.1002/gps.4275 [ Links ]
Marková, I. S., & Berrios, G. E. (2014). The construction of anosognosia: History and implications. Cortex, 61, 9-17. doi: 10.1016/j.cortex.2014.09.011 [ Links ]
Marková, I. S., Clare, L., Wang, M., Romero, B., & Kenny, G. (2005). Awareness in dementia: Conceptual issues. Aging & Mental Health, 9(5), 386-393. doi: 10.1080/13607860500142945 [ Links ]
Migliorelli, R., Petracca, G., Teson, A., Sabe, L., Leiguarda, R., & Starkstein, S. E. (1995). Neuropsychiatric and neuropsychological correlates of delusions in Alzheimer's disease. Psychological Medicine, 25(3), 505-513. doi: 10.1017/S0033291700033420 [ Links ]
Migliorelli, R., Tesón, A., Sabe, L., Petracca, G., Petracchi, M., Leiguarda, R., & Starkstein, S. E. (1995). Anosognosia in Alzheimer's disease: A study of associated factors. Journal of Neuropsychiatry, 7(3), 338-244. Retrieved from http://psycnet.apa.org/psycinfo/1996-27461-001 [ Links ]
Mograbi, D. C., & Morris, R. G. (2014). On the relation among mood, apathy, and anosognosia in Alzheimer's disease. Journal of the International Neuropsychological Society, 20(1), 2-7. doi: 10.1017/S1355617713001276 [ Links ]
Novelli, M. M. P. C. (2006). Validação da escala de qualidade de vida (QdV-DA) para pacientes com doença de Alzheimer e seus respectivos cuidadores/familiares (Doctoral dissertation). Retrieved from: http://www.teses.usp.br/teses/disponiveis/5/5138/tde-17102014-120122/es.php [ Links ]
Pachana, N. A., & Petriwskyj, A. M. (2006). Assessment of insight and self-awareness in older drivers. Clinical Gerontologist, 30(1), 23-38. doi: 10.1300/J018v30n01_03 [ Links ]
Perrotin, A., Desgranges, B., Landeau, B., Mézenge, F., La Joie, R., Egret, S., ... Chételat, G. (2015). Anosognosia in Alzheimer disease: Disconnection between memory and self-related brain networks. Annals of Neurology, 78(3), 477-86. doi: 10.1002/ana.24462 [ Links ]
Pinto, M., Barbosa, D., & Ferreti, C. (2009). Qualidade de vida de cuidadores de idosos com doença de Alzheimer. Acta Paulista de Enfermagem, 22(5), 652-657. Retrieved from http://www.scielo.br/pdf/ape/v22n5/09.pdf [ Links ]
Prigatano, G. P. (2009). Anosognosia: Clinical and ethical considerations. Current Opinion in Neurology, 22(6), 606-11. doi: 10.1097/WCO.0b013e328332a1e7 [ Links ]
Prigatano, G. P. (2010). The study of Anosognosia (1st ed.). New York: Oxford University Press. [ Links ]
Prigatano, G. P., & Morrone-Strupinsky, J. (2010). Management and rehabilitation of persons with anosognosia and impaired self-awareness. In G. P. Prigatano (Ed.), The study of anosognosia. (1st ed., pp. 495-516). New York: Oxford University Press. [ Links ]
Reed, B. R., Jagust, W. J., & Coulter, L. (1993). Anosognosia in Alzheimer's disease: Relationships to depression, cognitive function, and cerebral perfusion. Journal of Clinical and Experimental Neuropsychology, 15(2), 231-44. doi: 10.1080/01688639308402560 [ Links ]
Rosen, H. J. (2011). Anosognosia in neurodegenerative disease. Neurocase, 17(3), 231-41. doi: 10.1080/13554794.2010.522588 [ Links ]
Rowland, L. P., Pedley, T. A., & Merritt, H. H. (2009). Merritt's Neurology. Philadelphia: Lippincott Williams & Wilkins. [ Links ]
Sanz, A. C., Calvo, M. A., Gento, I. R., Delgado, E. I., Ríos, R. G., Herrero, ... Tola-Arribas, M. A. (2015). Anosognosia in Alzheimer disease: Prevalence, associated factors, and influence on disease progression. Neurología, 31(5), 296-304. doi: 10.1016/j.nrl.2015.03.006 [ Links ]
Satler, C., & Tomaz, C. (2013). Cognitive anosognosia and behavioral changes in probable Alzheimer 's disease patients. Dementia & Neuropsychologia, 7(2), 197-205. doi: 10.1590/S1980-57642013DN70200010 [ Links ]
Schoenmakers, B., Buntinx, F., & Delepeleire, J. (2010). Factors determining the impact of care-giving on caregivers of elderly patients with dementia. A Systematic Literature Review. Maturitas, 66(2), 191-200. doi: 10.1016/j.maturitas.2010.02.009 [ Links ]
Seltzer, B., Vasterling, J. J., Yoder, J., & Thompson, K. A. (1997). Awareness of deficit in Alzheimer's disease: Relation to caregiver burden. The Gerontologist, 37(1), 20-24. doi: 10.1093/geront/37.1.20 [ Links ]
Sousa, B. D., Santos, R. L., Brasil, D., & Dourado, M. (2011). Consciência da doença na demência do tipo Alzheimer: uma revisão sistemática de estudos longitudinais. Jornal Brasileiro de Psiquiatria, 60(1), 50-56. doi: 10.1590/S0047-20852011000100010 [ Links ]
Spijker, A., Vernooij-Dassen, M., Vasse, E., Adang, E., Wollersheim, H., Grol, R., & Verhey, F. (2008). Effectiveness of nonpharmacological interventions in delaying the institutionalization of patients with dementia: a meta-analysis. Journal of the American Geriatrics Society, 56(6), 1116-28. doi: 10.1111/j.1532-5415.2008.01705.x [ Links ]
Starkstein, S. E. (2014). Anosognosia in Alzheimer's disease: Diagnosis, frequency, mechanism and clinical correlates. Cortex, 61, 64-73. doi: 10.1016/j.cortex.2014.07.019 [ Links ]
Starkstein, S. E., Jorge, R., Mizrahi, R., & Robinson, R. G. (2006). A diagnostic formulation for anosognosia in Alzheimer's disease. Journal of Neurology, Neurosurgery, and Psychiatry, 77(6), 719-25. doi: 10.1136/jnnp.2005.085373 [ Links ]
Theofilou, P. (2012). Evaluation of quality of life for caregivers of patients with Alzheimer's disease. Journal of Alzheimer's Disease & Parkinsonism, 2(1), 1-2. doi: 10.4172/2161-0460.1000e106 [ Links ]
Turró-Garriga, O., & López-Pousa, S. (2012). Evaluación de la anosognosia en la enfermedad de Alzheimer. Revista de Neurologia, 54(4), 193-198. Retrieved from https://www.neurologia.com/articulo/2011428 [ Links ]
Turró-Garriga, O., Soler-Cors, O., Garre-Olmo, J., López-Pousa, S., Vilalta-Franch, J., & Montserrat-Vila, S. (2008). Distribución factorial de la carga en cuidadores de pacientes con enfermedad de Alzheimer. Revista de Neurologia, 46(10), 582-588. Retrieved from http://www.sld.cu/galerias/pdf/sitios/rehabilitacion-adulto/distribucion_factorial_de_la_carga_en_cuidadores_de_pacientes_con_enfermedad_de_alzheimer.pdf [ Links ]
Vellone, E., Piras, G., Talucci, C., & Cohen, M. Z. (2008). Quality of life for caregivers of people with Alzheimer's disease. Journal of Advanced Nursing, 61(2), 222-231. doi: 10.1111/j.1365-2648.2007.04494.x [ Links ]
Zanetti, O., Vallotti, B., Frisoni, G. B., Geroldi, C., Bianchetti, A., Pasqualetti, P., & Trabucchi, M. (1999). Insight in dementia: When does it occur? Evidence for a nonlinear relationship between insight and cognitive status. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 54(2), 100-106. doi: 10.1093/geronb/54B.2.P100 [ Links ]
 Endereço para correspondência:
Endereço para correspondência:
Setor Policial - SAIS A.E. 3, Bloco B
CEP 70.602-600
E-mail: RicardoMGP@gmail.com
Recebido em 25.Out.16
Revisado em 18.Jul.18
Aceito em 17.Dez.18
Ricardo Mendes Gomes Pereira, Doutor em Ciências do Comportamento pela Universidade de Brasília (UnB), 2º Tenente do Quadro de Oficiais Bombeiro Militar / Complementar (QOBM/Compl.) do Corpo de Bombeiros Militar do Distrito Federal (CBMDF).
Wânia Cristina de Souza, Doutora em Medicina pela Toyama Medical and Pharmaceutical University, Japão, é Professora Associada da Universidade de Brasília (UnB). E-mail: wcspsi@gmail.com
Marta Kerr Pontes, Doutora em Ciências do Comportamento pela Universidade de Brasília (UnB), é Psicóloga na Rede SARAH de Hospitais de Reabilitação. E-mail: martakp@gmail.com
Ana Idalina de Paiva Silva, Doutora em Ciências do Comportamento pela Universidade de Brasília (UnB), é Professora Adjunta I da Universidade Federal de Goiás (UFG). E-mail: Psicologa.ana.idalina@gmail.com














