Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Journal of Human Growth and Development
versão impressa ISSN 0104-1282
Rev. bras. crescimento desenvolv. hum. vol.22 no.1 São Paulo 2012
ORIGINAL RESEARCH
The difficulties of social adaptation of patients with HIV/AIDS
Jaqueline KawagoeI; Loide Corina ChavesI; Fernando Luiz Affonso FonsecaII, III; Rosangela FilipiniI; Márcia de Toledo BlakeIV; Simone de Oliveira CamilloI
ICurso de Enfermagem da Faculdade de Medicina do ABC, Santo André; SP, Brasil
IICurso de Gestão em Saúde Ambiental da Faculdade de Medicina do ABC, Santo André, SP, Brasil
IIIDepartamento de Ciências Biológicas - Universidade Federal de São Paulo-Campus Diadema, Diadema, SP, Brasil
IVLaboratório de Escrita Científica, Faculdade de Medicina do ABC
ABSTRACT
Quantitative study of a descriptive nature undertaken at Unidade de Referência em Doenças Infecciosas Preveníveis da Faculdade de Medicina do ABC designed to evaluate the prejudices that still exist in relation to HIV or AIDS patients, as well as their reasons and to investigate the difficulties in social adaptation of those patients. The sample comprised 20 HIV/AIDS patients seen from the Reference Unit and for data collection used a questionnaire. Most (11, 55%) of respondents reported an impact on their lives after the discovery of HIV seropositivity, usually in social life (friends, family and health services). It was found that the lack of knowledge about the disease is a factor of prejudice. In this study we could confirm the existence of prejudice related to HIV-positive patients, even after three decades of the first occurrence of HIV/AIDS.
Key words: HIV; AIDS; social life; prejudice; adaptation difficulty.
INTRODUCTION
The human immunodeficiency virus HIV-1 and HIV-2 are members of the family Retrovidae, subfamily Lentiviruses. These two types of viruses came from different moments of contact between primates and humans. HIV-1 originated from the human-Chimp contact and the HIV-2 contact with the mangabeyfugilento¹.
In the early 80, the first appearance of the disease, which would be classified as acquired immunodeficiency syndrome (AIDS), was notified by the Centers for Disease Control (CDC, USA) and common features were observed among the affected: male, homosexuals and/or intravenous drug users ¹.
In Brazil, in 1982, the first two cases of AIDS were identified by dermatologist Valéria Petri, from Escola Paulista de Medicina2.
Since the first notification of AIDS in Brazil until the year 2008, there were 506,499 cases of the disease. Considering the distribution in Brazil, 18,155 occurrences were recorded in the Northern region (04%), 58,348 in the Northeast (12%), 305,725 in the Southeast (60%), 95,552 in the South region (19%) and 28,719 in Mid-western region (6%)3.
In the same period cited previously, 333,485 cases were reported in male and 172,995 in female. Note the proportion of male and female cases being diminished considerably which in 1986 the reason was 15.1: 1 and in 2006 moved to 1.5: 1 ³.
In research on the treatment for AIDS in the international arena, held by the International Association of Physicians in AIDS Care (IAPAC), in 18 countries, including Brazil, with 3,000 individuals with AIDS, it was found that these individuals still concealed the disease with fear of discrimination, of which more than half of them (54%) were "somewhat" or "very" concerned that others know their diagnosis and of these, 83% have revealed the reason of social discrimination. It was also cited the concern about the expulsion of family and friends, inability to establish new relationships, potential loss of employment and changes to the reputation4.
Another survey conducted by the Ministry of Health exemplifies the prejudices that still exist in Brazil. From 8,000 people interviewed, 22.5% said they would not buy vegetables or greens in places where HIV-seropositive individuals work and 13% said that a teacher with AIDS can't teach classes at any school3.
HIV transmission occurs through sexual intercourse and exposure to secretions containing infected cells. Other means of transmission are: parenteral exposure to blood and blood products, perinatal or vertical transmission5.
The contagion of HIV does not occur through sex, provided that they use condoms correctly; shared masturbation; kiss on the cheek or mouth; sweat and tear; insect bite; handshake or hug; common use of cutlery or glasses and using the same bus seat6.
The increased HIV patients´ survival is disclosed in campaigns as a way to demystify the disease. According to the Ministry of Health, between 1995 and 2007, the survival rates doubled from 58 months to 108 months in the regions southeast and south of the country, due to the early diagnosis, availability of antiretroviral drugs and the continuous clinical monitoring3.
The interest in developing this study originated by an experience within the community and extra-hospitalar contact with a patient. He was found before the provision of nursing assistance in the semio-technical stage, at a trade show he attended every weekend. After the intra-hospital meeting, in which his HIV diagnosis was found, the patient became apprehensive with regard to disclosure to others, including his family, who was not aware of his illness, as noted in his book, and he quit attendance to the fair.
Therefore, this experience raised a great motivation to carry out this survey, questioning still existing concepts and prejudices, as currently the general population appropriates instructive information about AIDS. However, why is there still an intolerance of social interaction among population and the HIV-seropositive individuals?
Is it pure prejudice or fear of living with others' problems?
Thus, the objectives are: check the prejudices that still exist in relation to patients with HIV / AIDS, as well as the reasons for which there are, and investigate the difficulties of social adaptation among patients with AIDS.
METHODS
This is a quantitative descriptive study, with the exploratory technique used to obtain data through field research and unstructured literature review.
The study was conducted in Unidade de Referência em Doenças Infecciosas Preveníveis da Faculdade de Medicina do ABC, after approval by the Ethics Committee on Human Research of the faculty (protocol No. 283/2009), according to Resolution 196/96 of Conselho Nacional de Saúde (CNS).
The sample consisted of 20 HIV or AIDS patients, attended at the clinic after consenting to participate in this study and signing the Term of Free and InformedConsent. Initially a letter was sent, along with the research project, to the nursing manager and to the clinical director of the clinic to be researched, requesting authorization to carry out this study and indications of patients who fit the desired population.
A structured and semi-structured questionnaire, composed of nine (09) open-ended questions, was used for data collection.
The open and semi-structured questions were designed to allow more spontaneity in the informant´s responses and meet the objectives proposed in this study. The open questions corresponded to numbers 04 and 08, the semi-structured corresponded to numbers 01, 03, 06 and 09 and the structured corresponded to numbers 02, 05 and 07. Question number 01 featured the informant´s identification. The questions numbers 02 to 06 were referring to the type of discrimination incurred by the customer due to his HIV/AIDS diagnosis. The questions numbers 07 and 08 were referring to the client´s possible isolation from social life, after being aware of his diagnosis. Question number 09 referred to the reasons that lead people to present any type of discrimination to those with HIV/AIDS, according to the opinion of the study subjects. The results were presented in tables, in absolute and relative frequencies, or in the form of text for the numerically small results .
RESULTS
The results regarding the issues of the questionnaire administered to the 20 HIV or AIDS patients, attended at the clinic of Unidade de Referência em Doenças Infecciosas Preveníveis da Faculdade de Medicina do ABC are presented in tables, in absolute and relative frequencies.
DISCUSSION
The age range of people who participated in this study varied from 20-60 years, eight females and twelve male. Most subjects (09; 45.0%) were aged 40-50 years, while 40% (08) were aged 30-40 years, 10% (02) 50-60 years and 5% (01) 20-30 years.
Note that the proportion man woman is consistent with data obtained by Ministry of Health, in which the ratio obtained was 1.5: 1, respectively. Twelve men and eight women participated in this study, resulting in the ratio of 1.5:1 ³.
The subjects´ marital status in this study varied, with the majority (08; 40%) being single, whereas 30% (06) with a partner, 20% (04) were married, 5% (01) was separated and 5% (01) divorced.
Table 1 shows that the majority (11; 55%) of the subjects responded that did not suffer discrimination because of their diagnosis. However, it is noteworthy that of those, many reported verbally that did not disclose their diagnosis to anyone.

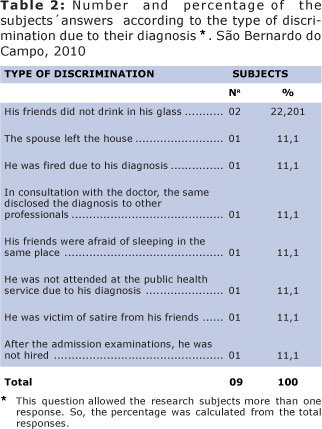
The highest occurrence (02; 22.2%) of discrimination reported by the research participants was related to non-use of the same household appliance by friends. This discrimination shows how the lack of knowledge about the forms of disease transmission can cause constraints to seropositive individuals.
It was also cited in the same proportion (01; 11.1%) the spouse´s moving out the home, dismissal, disclosure of diagnosis to others, fear of sleeping along with the person, care refusal at health services, friends´ satires and not being hired due to their diagnosis.
It can be observed that most (04; 44.4%) subjects reported having suffered prejudice among friends, as is shown in Table 3.
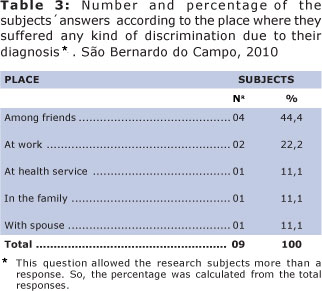
The second greatest occurrence (2; 22.2%) of prejudice was at work, which may be a consequence of the number of absences or delays arising from the use of antiretroviral medications that require medical supervision and, most commonly, early in treatment for causing side effects. These conditions lead to a forced diagnosis disclosure and, often, the person resigns or is fired from his job for not withstanding the "pressure".
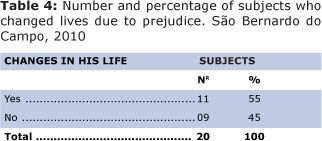
Most subjects (11; 55%), according to data presented in Table 4, showed changes in their lives by the prejudice suffered after discovering the diagnosis. These changes in the patient's life reflect negatively, as can be seen in Table 5.
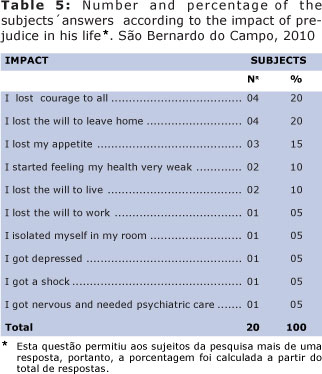
The answers that prevailed in Table 5 are related to loss of mood (04; 20%) and the desire to leave home (04; 20%), followed by loss of appetite (03; 15%), the feeling of having weak health (02; 10%) and loss of will to live (02; 10%). It was also mentioned the loss of will to work, isolation, depression, shock, nervousness and need for psychiatric treatment in equal proportions (01; 05%).
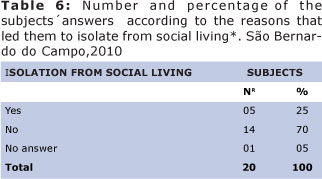
Table 6 shows that the majority of the subjects (14; 70%) did not isolate from social life after discovering the HIV/AIDS diagnosis. However, many reported verbally that they had not disclosed their health status to anyone.
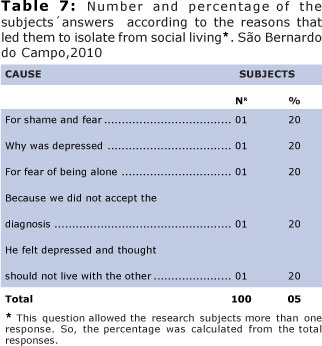
It can be seen in Table 7 that the responses became similar in proportion and they are all related to the stigma acquired after the disease, that is the same to say that HIV-infected patients feel inferior to other people due to the diagnosis and, thus, isolate themselves from social life.
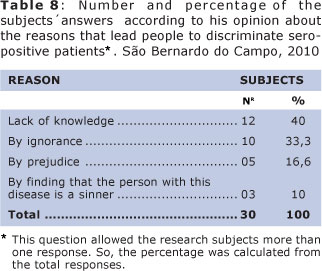
As the data presented in Table 8, the main causes of prejudice related to HIV-positive patients in their perception are the lack of knowledge about the disease and its modes of transmission. The factor most often reported was lack of knowledge (12; 40%), followed by ignorance (10; 33.3%), for pure prejudice (05; 16.6%) and factors relevant to the history of the disease, such as homosexuality and promiscuity (03; 10%). The population is generally well informed about the modes of HIV transmission but is unaware of the everyday situations that provide risk of infection8.
It is important that, in addition to treatment by health services, measures are implanted to answer the questions of the seropositive patients social network, so that bias does not exist in the community and, therefore, to improve the quality of life for those with the disease9.
The bias perceived by the respondents only makes the experience with seropositivity even worse, since the stigma imposed by society becomes a pre-determinant of prejudice. The fact that people close to the patient are prejudiced already affects social interactions.
It is noteworthy that, according to the Ministry of Health, the secrecy is guaranteed to people with HIV, but many companies disregard this law in admission examinations10.
The impact of prejudice on the participants' lives showed in this study the great stigma that HIV/AIDS holds today, using the fact that the transmission of information about HIV is abundant today.
According to WHO, discrimination and stigma related to HIV-positive patients significantly increase feelings of social isolation on them11.
The discovery of seropositivity may influence social interactions, as evidenced by the omission of diagnosis and subsequent isolation and depression in many cases10.
Considering the stated facts, it can be inferred that there are many losses and difficulties faced by HIV-positive patients, which may reflect on various aspects such as financial, social, and especially the personal.
The lie and omission of the diagnosis to others serve often as a strategy for the patient's coping with the disease, especially in the initial phase, when occurs the discovery and initiation of treatment10. As is the case of the patient who raised this study, who reported to relatives that his hospitalization was due to Psoriasis crisis, information given by him and confirmed in his files.
The fact of having a disease considered deadly for years and historically associated with homosexuality and promiscuity, leads the patient to a disparity of emotions and desires which are reproduced in the form of fear, shame, anxiety and depressão12.
According to literature, the data observed for several years, showed a reduction in the proportion of individuals in the population who certainly know the disease forms of transmission, 50% in 1998 to 40% in 2005, and the belief of virus transmission by social contact with infected people without fluid exchange remains high13.
These data draw attention because the HIV/AIDS information transmission suffer certain limitations to reach the population and this reality creates suffering and distress in living with HIV/AIDS, what is known and reported by this research participants.
Thus, it was found that after three decades of the HIV detection, responsible for AIDS development, there is still prejudice related to HIV-positive patients and that this discrimination perceived by them interfere negatively on their living with the disease.
We can infer that the population knowledge about the disease is still insufficient, leading to situations often embarrassing and inhumane to patients. Such circumstances lead the person to withhold the diagnosis for fear of prejudice, making treatment difficult and taking him to a life with difficulties in social interaction to be transposed.
Therefore, we emphasize the importance of awareness campaigns about the disease, mainly about the ways of transmission, associated to the actions of demystification, so that the HIV positive patient does not face prejudice, beyond the difficulties of the disease itself and all the history that accompanies it.
For this is essential an effort by the media together with the department of justice, department of work and entities that protect the rights of workers and/or people living with HIV/AIDS, to highlight the limitations arising from the stigma associated with the disease and not only the infection itself.
REFERENCES
1. Daspett C. Um estranho entre nós: a repercussão do diagnóstico de HIV/AIDS na trajetória de casais heterossexuais soroconcor-dantes. São Paulo, 2005. Dissertação (Mestrado em Psicologia Clínica). Pontificia Universidade Católica de São Paulo, 2005. [ Links ]
2. Moreira MS. Psiconeuroimunologia. Rio de Janeiro: Editora Medsi, 2003. 256 págs. [ Links ]
3. Ministério da Saúde. Boletim epidemiológico 2008. Disponível em: http://www.aids.gov.br/Acesso em: 19 de jun. 2009. [ Links ]
4. Scaldaferri A; Araújo FE.Pesquisa sobre o preconceito e o estigma de pacientes soropositivos. São Paulo, 2008. [ Links ]
5. Rachid M; Schechter M. Manual de HIV/AIDS. 5ª edição. Rio de Janeiro: Editora Revinter, 2000. 222 págs [ Links ]
6. Ministério da Saúde. Formas de contágio. Disponível em: <http://www.aids.gov.br/data/Pages/LUMIS81B68422PTBRIE.htm>. Acesso em: 19 de jun. 2009. [ Links ]
7. Lakatos EM; Marconi MA. Metodologia Científica. 2ª edição. São Paulo: Editora Atlas S.A., 1995. 140 págs. [ Links ]
8. Lima MM. et.al.Conhecimento da população de Viçosa, MG, sobre as formas de transmissão da AIDS. Departamento de Biologia Geral, Universidade Federal de Viçosa. Minas Gerais, 2007. [ Links ]
9. Tunala LG. Fontes cotidianas de estresse entre mulheres portadoras de HIV. RevSaude Publica. 2002; 36(4supl): 24-31. [ Links ]
10. Garrido PB; Paiva V. Aids, estigma e desemprego: implicações para os serviços de saúde.São Paulo, 2007. Rev Saúde Pública 2007;41(Supl. 2):72-9 [ Links ]
11. Organização das Nações Unidas. Programa Conjunto das Nações Unidas sobre HIV/Aids. El SIDA: cuidados paliativos.Ginebra; 2001. [ Links ]
12. Carvalho CML; Galvão MTG. Enfrentamento da AIDS entre mulheres infectadas em Fortaleza - CE.São Paulo, 2008. Revista da Escola de Enfermagem USP 2008; 42(1):90-7. [ Links ]
13. Ferreira MP; Grupo de Estudos em População, Sexualidade e Aids. Nível de conhecimento e percepção de risco da população brasileira sobre o HIV/Aids, 1998 e 2005.RevSaude Publica. 2008; 42(Supl1): 65-71. [ Links ]
 Corresponding author:
Corresponding author:
fon_fonseca@yahoo.com.br
Manuscript submitted Apr 06 2011
Accepted for publication Dec 20 2011.













