Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
SMAD. Revista eletrônica saúde mental álcool e drogas
versão On-line ISSN 1806-6976
SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. port.) vol.9 no.1 Ribeirão Preto abr. 2013
ORIGINAL ARTICLE
Long Term Psychiatric Institution: Profile of patients and human resource indicators
Institución Psiquiátrica de Larga Permanencia: Perfil de pacientes e indicadores de recursos humanos
Maria Odete PereiraI; Marli de Carvalho JericóII; Marcia Galan PerrocaIII; Helena Ayako MukaiIV
IPhD, Professor, Universidade Federal de São Paulo, São Paulo, SP, Brazil
IIPhD, Professor, Faculdade de Medicina de São José do Rio Preto, São José do Rio Preto, SP, Brazil
IIIPhD, Adjunct Professor, Faculdade de Medicina de São José do Rio Preto, São José do Rio Preto, SP, Brazil
IVMSc, Professor, Centro Estadual de Educação Tecnológica Paula Souza, Lins, SP, Brazil
ABSTRACT
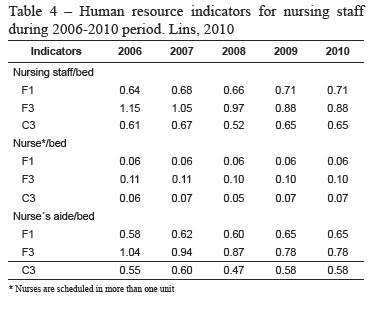
This descriptive study aimed to investigate the social-demographic and epidemiological profile of patients and human resource indicators in a neuropsychiatric hospital located in southeastern Brazil. The data related to the human resources (2006-2010) and the social-demographic and epidemiological characterization of the patients (2010) were extracted from the hospital management system database and staff scheduling worksheets. The study included 105 patients with a mental disorder diagnosis. Most were male 60 (57.1%), mean age 52.5 (11.4) years, duration of hospitalization up to 15 years 84 (80%), and primary diagnosis of schizophrenia 50 (47.7%), and mental retardation 41 (39%). The nursing staff/bed ratio ranged from 0.52 to 1.15 and the nurse/bed from 0.05 to 0.11. The aim of this research is to contribute to the development of mental health policies and equip the administrator for the strategic decision making processes.
Descriptors: Mentally Ill Persons; Psychiatric Nursing; Quality Indicators, Health Care.
RESUMEN
Este estudio descriptivo tuvo como objetivo investigar el perfil sociodemográfico y epidemiológico de pacientes e indicadores de recursos humanos en un hospital neuro psiquiátrico localizado en la región sudeste de Brasil. Los datos relativos a los indicadores de recursos humanos (2006-2010) y caracterización socio demográfica y epidemiológica de los pacientes (2010) fueron extraídos de la base de datos del sistema de gestión hospitalaria y planillas de escala de personal. Participaron del estudio 105 pacientes con diagnóstico de trastorno mental. La mayoría era del sexo masculino 60 (57,1%), edad media 52,5 (11,4) años, tiempo desde internación hasta 15 años 84 (80%) y diagnóstico principal de esquizofrenia 50(47,7%) y retardo mental 41(39%). La relación enfermería/camas varió de 0,52 a 1,15 y la enfermero/camas de 0,05 a 0,11. El objetivo es que los resultados de esa averiguación puedan aportar en la elaboración de políticas de salud mental e instrumentalizar el gestor en la tomada de decisión y establecimiento de estrategias de acción.
Descriptores: Enfermos Mentales; Enfermería Psiquiátrica; Indicadores de Calidad de la Atención de Salud.
Introduction
The psychiatric care until the second half of the twentieth century was based mainly on the hospitalization and institutionalization of the mentally ill. In Brazil, the psychiatric reform began in 1987, aimed at regulating the mental patients' rights and the phasing out of the asylums. The planned and programmed reduction of beds should be accompanied by the expansion of the Community-based network, with the deployment of alternative services and when necessary the accreditation of psychiatric beds in general hospitals(1).
Data from the Ministry of Health(2) shows that, in 1996, there were 72,514 psychiatric beds, which were reduced to 42,076 in 2005; however, they were concentrated in large cities, especially in the Southeast - 60%.
The psychiatric hospital care took new directions with the 251/GM Ordinance, 2002 (1), which established guidelines and standards to improve the quality of hospital services, respecting universality and equity principles. It was then created the National Hospital/Psychiatry Evaluation System (PNASH) that defined quality indicators for hospital ratings.
The indicator is a quantitative measurement used as a guide to monitor and evaluate the patient care(3). It enables the redesign and reorganization of the operations, by offering subsidies for the decision-making process(4). The systematic use of indicators guides the continuous improvement of the quality of care and the increase in productivity; thus, benefiting patients, professionals, and the administration(5).
The deinstitutionalization of mental patients and their subsequent social reintegration changed the profile of this population. Therefore, researchers addressing this issue contribute to the planning and organization of the services forming the psychiatric care network, and the improvement of welfare policies(6).
After the psychiatric reform, few studies have investigated the social-demographic and epidemiological characteristics of patients in different scenarios: long-term institutions(7), Center for Psychosocial Care (CAPS)(8), Day Hospital(9), short-term institution(6, 10) and short and long-term institutions (11-12).
Objectives
The objective of the study is to analyze the social demographic and epidemiological characteristics of the patients and the human resource indicators in a neuropsychiatric hospital.
Methodology
Design and Subjects
This is a descriptive cross-sectional study developed in a large neuropsychiatric public hospital located in the Southeastern region of Brazil. The institution serves primarily patients from the Unified Health System (SUS), with catchment areas from the VI Regional Health Department (VI-DRS) located in Bauru. Currently it holds 340 inpatient beds, with 160 beds designated for psychiatric and 180 beds for neurological patients.
The staff consists of 696 employees, with 199 in the administrative area, and 497 in the clinical area. The nursing staff is composed of 31 nurses and 298 nurse aides. Among the other professionals involved, there are thirty doctors (five psychiatrists and two neurologists), four physical therapists, two speech therapists, three dentists, ten psychologists, eleven social workers, three pharmacists, and eleven occupational therapists.
The research involved only patients with mental disorders admitted to the Management of Integral Health (GAIS) IV and the Center for Protected Housing (NMP), totaling 105 patients divided into three confinement units. The F1 and F3 units have 70 beds reserved for residents with severe and persistent mental disorders with a history of several years of confinement. The C3 unit (40 beds) is part of the NMP and has eight apartments reserved for patients with a lower degree of dependence.
The variables are as follows:
1-Social-demographic: gender, age, education, marital status, source of income, place of residence, and length of stay;
2-Epidemiological: principal diagnosis, comorbidities, therapy of continuous-use medications;
3-Human resource indicators: nursing staff/bed, nurse/bed, and nurse aide/bed ratios;
Procedures for Data Collection
Data collection was conducted only after the formal approval by the hospital Ethics Committee on Research at the São José do Rio Preto School of Medicine (Protocol no. 319/2010. The data related to the human resources (2006-2010) and the social demographic and epidemiological characterization of the patients (2010) were extracted from the hospital management system database and nursing staff scheduling worksheets provided by the nursing staff administration.
The diagnoses were expressed according to the International Statistical Classification of Diseases and Related Health Problems (ICD-10). The pharmacy provided the medication costs. The human resource indicators were calculated according to the recommendations of the Hospital Commitment to Quality (CQH)(13).
Submission and Data Processing
The statistical analysis of the data was performed with The R Foundation for Statistical Computing version 2.13.0 software. The descriptive analysis is presented as absolute frequency, mean, standard deviation, and percentage.
Results
There was a predominance of illiterate males 60 (57.1%), ages from 41 - 60 years 61 (58.1%), mean age 52.5 (11.4) years, range - 18-80 years; 94 singles (89.5%); with no income 71 (67.7%); from the Bauru region 72 (68.6%), and length of stay up to 15 years 84 (80%). In relation to the inpatient units, F3 held a mostly female population - 18 (69%), ages 61-80 years - 3 (11.5%). The longest confinement time (26-29 years) was more prominent in the C3 unit - 5 (13%) and the shorter (≤ 5 years) was in the F3 unit 9 (34.6%), (Table 1).
Schizophrenia 50 (47.7%) was the main diagnosis (Table 2) being predominant in units F1 - 20 (50%) and C3 - 21 (53.8%). Followed by mental retardation 41 (39%) in unit F3 - 9 (34.6%). With regard to comorbidities, smoking predominated with 65 (33.5%). Followed by obesity 45 (23.2%), hypertension 21 (10.8%), and diabetes mellitus 18 (9.3%).
There was a consumption of 381,564 of psychotropic drugs tablets, at a cost of R$ 135,713.01. The neuroleptics were the most used drugs - 205,344 (53.8%) tablets annually, totaling R$ 128,525.84. The continuous-use medications that were non-specific for mental disorders totaled 68,952 tablets at a cost of R$ 5,051.04 (Table 3). Antihistamines had the highest consumption - 21,240 tablets (30.8%) followed by anti-glycemic - 20,520 (29.7%), and anti-hypertensive 18,000 (26.1%).
Regarding the indicators for nurse staffing human resources, the nursing staff/bed ratio during the investigated period ranged from 0.52 to 1.15, the nurse/bed from 0.05 to 0.11 and the nurse aide/bed from 0.47 to 1 04 (Table 4).
Discussion
The findings show a predominance of males - 57.1% confirming results from other studies with 53.4%(12) and 65.5%(10). It is noteworthy that men generally present mental disorders that require early confinement.(11). The majority of patients - 58.1% belonged to the 41 to 60 age group, a contrast to the studies conducted in Rio de Janeiro where the ages of the patients were less than 40 (52.6%)(11), and between 30 and 49 (56%)(12). There were a considerable number of elderly patients, in the 60 to 80 age group - 28 (26.7%), similar to the 31.3 percentages found in the psychosocial census conducted by the Health Department with 58 long-stay institutions located in the state of São Paulo(2).
The institution, under study, showed a considerable number of illiterate patients – 57.1%, comparable to the results from other studies from 50%(12) and 70% (2). The incomplete schooling intensifies the conditions of social exclusion (14) since the inability to understand the instructions provided by the health professionals may negatively affect the adherence to the treatment(6). Therefore, the institution offers literacy classes through the Literacy Program for Youth and Adults (PROAJA), the Center for Youth and Adults Education (CEJA) or a Hospital Class. Currently, 21% of residents are enrolled in one of these programs.
The data demonstrated the majority as being single 89.5%, and with no sources of income 67.7%. The lack of social interaction may have contributed to this situation since added to the symptomatic isolation resulting from the disease, there is the discrimination and rejection of the mentally ill(9).
Schizophrenia was the most frequent diagnosis (47.7%), similar to the findings in other studies, 43.3%(10) and 53.6%(12). Among the commodities, the higher percentages of smokers (62%) are close to the results found in Porto Alegre from 38.9 to 54.3%(15) and in São Paulo - 50 to 84%(16). Obesity was the second most common comorbidity. The incidence of obesity among schizophrenic patients treated with psychotropic is from 40 to 75%(17).
The F3 unit patients consumed the largest number of anxiolytic and antipsychotic medications because of the high number of psychiatric complications; thus, evidencing that the mental illness treatments are still rooted in the pharmacological model(8). The use of antipsychotic drugs is associated with significant increases in weight and metabolic changes and, consequently, with an increased risk of cardiovascular death(18).
The high cost of maintaining a psychiatric patient is evident in the consumption of continuous-use medications, both psychotropic (R$ 135,713.01) and the ones used for clinical problems (R$ 5,051.04). However, it is necessary to emphasize that this study considered only the continuous-use medications; thus, this cost could be altered with the inclusion of all the medications consumed by the patient. The research demonstrates that the psychiatric confinement originates the highest cost among all specialties funded by the Unified Health System (SUS)(19).
The patient profile found in this study and the lengthy confinement justifies the existence of long-stay psychiatric institutions, despite the deinstitutionalization proposed by the Psychiatric Reform. In Brazil, in 2008, the SUS provided 32.735 psychiatric hospital beds, i.e., 0.172 beds per 1.000 populations(2). The state of São Paulo had 58 psychiatric hospitals totaling 13,190 beds, with 432 beds in general hospitals, with a ratio of 0.34 beds/1,000 (pop.); down from the 0.45beds/1,000 (pop.), recommended by the Ministry of Health, and lower than countries such as Italy (4.63), United Kingdom (5.8), and Norway (12) beds/10.000 (pop.).(20)
According to the World Health Organization (WHO)(20), one cannot transition from what is a hospital service to a community-based one, by essentially closing the psychiatric institutions without providing appropriate alternative structures. In the United States, the psychiatric reform resulted in increased numbers of homeless people, because the articulation between the psychiatric hospitals and the community-based services never occurred (21). Knowledge of the institutionalized population enables the planning and execution of their social reintegration; thus, avoiding the lack of assistance.
As for the human resource indicators in the units analyzed, the ratios between the number of nursing staff/bed varied from 0.52 to 1.15 and the nurse/bed showed the following variations 0.05-0.11. The data provided by the Hospital Quality Commitment (CQH)(13) for the fourth quarter of 2009, regarding the psychiatric hospitals in the program, explain the mean of 0.12 nurses/bed (0.08 to 0.37 ranges). These results demonstrate a difference in nursing staffing among the various psychiatric hospitals, and in the institution being analyzed, this value is lower than the referenced.
The nurse is responsible for establishing the quanti-qualificative framework of the professionals needed to meet the patient demands in relation to the health care (22). There are very few researches dealing with the number of patients that a nursing staff can efficiently care for (23). Although mental patients usually do not present clinical problems requiring constant nursing care, they necessitate continuous monitoring because of mood instability, with instances of self and peer aggression, escape and suicide attempts(23).
Therefore, it becomes necessary to perform additional studies to determine the suitable quanti-qualitative framework of the team, to be able to provide good nursing care and ensure patient safety. The results from this institution may differ from other studies; thus demonstrating the need for more research in order to provide the appropriate care required by the mentally ill.
Conclusion
The aim of this research is to contribute to the development of mental health policies and to equip the administrator for the strategic decision making processes.
References
1. Ministério da Saúde (BR). Reforma psiquiátrica e política de saúde mental no Brasil. Documento apresentado à Conferência Regional de Reforma dos Serviços de Saúde Mental: 15 anos depois de Caracas. OPAS. Brasília, novembro 2005. [ Links ]
2. Secretaria da Saúde de São Paulo. Desafios para a desinstitucionalização dos moradores em hospitais psiquiátricos do estado de São Paulo. São Paulo: FUNDAP: Secretaria da Saúde; 2008. 170 p. [ Links ]
3. Joint Commission on Accreditation of Healthcare Organizations (JCAHO). Accreditation manual for hospitals. Nurs Care. 1992 79-85. [ Links ]
4. Bittar OJNV. Indicadores de qualidade e quantidade em saúde. Rev Admin Saúde. 2004; 6(2):15-8. [ Links ]
5. Travassos C, Noronha JC, Martins M. Mortalidade hospitalar como indicador de qualidade: uma revisão. Ciênc Saúde Coletiva. 1999;4(2):367-81. [ Links ]
6. Castro AS de. Caracterização sócio demográfica e clínica das reinternações psiquiátricas no Hospital Santa Tereza de Ribeirão Preto, no período de 2006 a 2007. [dissertação de mestrado]. Ribeirão Preto: Escola de Enfermagem de Ribeirão Preto da Universidade de São Paulo; 2009. 90 p.
7. Fleck MPA, Wagner L, Wagner M, Dias M. Long-stay patients in a psychiatric hospital in Southern Brazil. Rev Saúde Pública. 2007;41(1):124-30. [ Links ]
8. Carvalho MDA, Silva HO, Rodrigues LV. Perfil epidemiológico dos usuários da rede de saúde mental do município de Iguatu, CE. SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. Port.) [Internet]. 2010 [acesso 5 ago 2011]; 6(2):337-49. Disponível em: www2.eerp.usp.br/resmad/artigos/SMAD v6 n2 a7. Pdf. [ Links ]
9. Alves AMO. Perfil sócio demográfico e clínico do portador de doença mental crônica egresso do Hospital-Dia de Psiquiatria da Santa Casa de Campo Grande-MS. [Dissertação] Campo Grande (MS): Universidade Católica Dom Bosco; 2003. [ Links ]
10. Barros NHS. Características biossociodemográficas e diagnósticos de pacientes internados em hospital psiquiátrico de Campo Grande-MS. [dissertação de mestrado]. Campo Grande (MS): Universidade Católica Dom Bosco. Programa de Mestrado em Psicologia; 2007. [ Links ]
11. Silva JPL, Coutinho ESF, Amarante PD. Perfil demográfico e socioeconômico da população de internos dos hospitais psiquiátricos da cidade do Rio de Janeiro. Cad Saúde Pública. 1999;15:505-11. [ Links ]
12. Gomes MPC, Couto MCV, Pepe VLE, Almeida LM, Delgado PGG, Coutinho ESF. Censo dos pacientes internados em uma instituição asilar no estado do Rio de janeiro: dados preliminares. Cad Saúde Pública. 2002;18(6):1803-7. [ Links ]
13. Programa de Qualidade Hospitalar (CQH).Compromisso com a qualidade hospitalar: apresentação dos indicadores dos hospitais participantes referente ao 4º trimestre de 2009 [Internet]. [acesso 15 out 2011]. Disponível em: http://www.cqh.org.br/?q=node/322site.pdf [ Links ]
14. Ministério da Educação (BR). Classe hospitalar e atendimento pedagógico domiciliar : estratégias e orientações. Brasília: Secretaria de Educação Especial – MEC, SEESP; 2002. 35 p. [ Links ]
15. De Boni R, Pechansky F. Prevalência de tabagismo em uma unidade de internação psiquiátrica de Porto Alegre. Rev Psiquiatria Rio Grande do Sul. 2004;3(25):475-8. [ Links ]
16. Malbergier A, Oliveira HP Júnior. Dependência de tabaco e comorbidade psiquiátrica. Rev Psiquiatr Clin. 2005;32:276-82. [ Links ]
17. Wirshing D. Schizophrenia and obesity: impact of antipsychotic medications. J Clin Psychiatry. 2004;65(Suppl 18):13-26. [ Links ]
18. Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost and causes of death among public mental health clients in eight states. Prev Chronic Dis. [Internet] 2006. Apr [acesso 12 ago 2011]. Disponível em: http://www.cdc.gov/pcd/issues
19. Mello R. A questão da interdisciplinaridade no dia a dia da enfermeira que atua em Centros de Atenção Diária de Saúde Mental. Rev Bras Enferm. 1998;51(1):19-34. [ Links ]
20. Organização Mundial de Saúde. The world health report 2001 mental health: new understanding, new hope. Lisboa (PT); abril 2002. [ Links ]
21. Lovisi VR. Internação psiquiátrica na região de Ribeirão Preto no período de 1989 a 1993. [dissertação de mestrado]. Ribeirão Preto: Escola de Enfermagem de Ribeirão Preto da Universidade de São Paulo; 1998. 96 p.
22. Conselho Federal de Enfermagem (BR). Resolução n.293/2004. Fixa e estabelece parâmetros para o dimensionamento do quadro de profissionais de Enfermagem nas unidades assistenciais das instituições de saúde e assemelhados. [acesso 18 ago 2009]. Disponível em: http://www.corensp.org.br/resolucoes/resolucao293.htm. [ Links ]
23. Martins PASF. Sistema de classificação de pacientes na especialidade enfermagem psiquiátrica [dissertação de mestrado]. São Paulo (SP): Escola de Enfermagem da Universidade de São Paulo; 2001.
 Correspondence
Correspondence
Marcia Galan Perroca
Faculdade de Medicina de São José do Rio Preto, Curso de Graduação em Enfermagem
Av. Faria Lima, 5416
Bairro: São Pedro
CEP: 15090-000, São José do Rio Preto, SP, Brasil
E-mail: marcia.perroca@famerp.br
Received: Oct. 17th 2011
Accepted: Nov. 13th 2012













