Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Revista da SBPH
versão impressa ISSN 1516-0858
Rev. SBPH vol.22 no.2 São Paulo jul./dez. 2019
ARTICLES
PROCOPE-H: An intervention proposal in coping with hospitalization in children and adolescents
PROCOPE-H: Uma proposta de intervenção no coping da hospitalização em crianças e adolescentes
Jodi Dee Hunt Ferreira do Amaral1, I; Sônia Regina Fiorim Enumo2, II
IUniversidade Federal de Uberlândia (UFU)
IIPontifícia Universidade Católica de Campinas (PUC-Campinas)
ABSTRACT
When children and adolescents are hospitalized, emotional, social and cognitive developmental difficulties may occur. Achieving an understanding on how the coping process occurs may provide for better management. This study presents the Promotion of Coping Hospitalization Program (PROCOPE-H), including eight different resources - three games, two activities and three books. The User Satisfaction Inventory, before and after Feelings Protocol, Adapted Hospital Play Evaluation Instrument (ABHa), Coping of Hospitalization, Ailment and Treatment Scale (COPHAT-CA), specially designed for this study, and Coping of Hospitalization Scale (COPE-H) were administered to select resources and evaluate PROCOPE-H. Parents/Caregivers responded a sociodemographic protocol, the COPHAT-P (parents/caregivers version) and the COPE-H-Caregivers. Seven children/adolescents hospitalized (4 girls; 6 to 14 years old) took part in PROCOPE-H to verify its feasibility. Participants presented high averages in Confidence in going back to school (M = 4.5), Knowing how to express and control feelings (M = 4.25), Confidence to coping with procedures (M = 4.25), Confidence in coping with hospitalization (M = 4.0) and Learning (M = 4.0); all reported Confidence in coping with the effects of treatment. PROCOPE-H was well evaluated and therefore may be considered a promising psychological intervention for hospitalization.
Keywords: coping; hospitalization; intervention; children; adolescents.
RESUMO
Quando crianças e adolescentes são hospitalizados, podem ocorrer prejuízos no desenvolvimento emocional, social e cognitivo. Compreender como o processo de enfrentamento/coping ocorre pode ajudar as intervenções. Este estudo apresenta o Programa de Promoção do Coping da Hospitalização (PROCOPE-H), com cinco sessões, contendo oito recursos - três jogos, duas atividades e três livros, Protocolo de Sentimentos antes e após sessão e Inventário de Satisfação do Usuário. Foram aplicados o Instrumento de Avaliação do Brincar no Hospital adaptado (ABHa), Escala de Coping da Hospitalização, Adoecimento e Tratamento (COPHAT-CA) especialmente elaborada, e Escala de Coping da Hospitalização (COPE-H), para subsidiar a seleção dos recursos da intervenção e avaliar o PROCOPE-H. Os responsáveis responderam um protocolo sociodemográfico, o COPHAT-P (versão pais) e o COPE-H-Pais. Para verificar sua adequação, o PROCOPE-H foi aplicado em sete crianças/adolescentes hospitalizados (4 meninas; 6-14 anos). Estes apresentaram maiores médias em Confiança em voltar para a escola (M = 4,5), Saber expressar e controlar sentimentos (M = 4,25), Confiança para enfrentar os procedimentos (M = 4,25), Aprendizagem (M = 4,0), Confiança para enfrentar a internação (M = 4,0); todos relataram Confiança para enfrentar os efeitos do tratamento. O PROCOPE-H foi bem avaliado pelos participantes, sendo considerado como uma intervenção promissora.
Palavras-chave: coping; hospitalização; intervenção; crianças; adolescentes.
When children and adolescents are hospitalized, emotional, social and biological developmental difficulties may occur. Understanding how the child/adolescent copes is essential for designing interventions and thus preventing possible traumas and/or future behavioral/emotional consequences. Knowledge on how to use resources already available to the child/adolescent and how to aquire other methods for coping with hospitalization, diagnosis and treatment, potentially provides for better managment of the whole process. Parents/guardians perception, on the ways in which their children deal with their hospitalization, diagnosis and treatment, is equally necessary to offer adequate psychosocial care.
Many different types of resources have been used to ease the difficulties of hospitalization or provide therapeutic benefits for those who have chronic diseases. Bibliotherapy has been used by researchers to intervene in pediatric patients with cancer (Bernardino, Elliott, & Rolim, 2012; Fontenele, Pinto, Andrade, Dias, & Moura, 2006). Other authors have written specialized books or manuals for patients and families to deal with cancer (Nucci, 1997; Pedrosa, 2000a, 2000b, 2000c, 2003, 2004; Pedrosa, Marques, & Campos, 2011; Pedrosa, Monteiro, & Campos, 2012) and hospitalization in general (Franklin, 2010; McGrath, 2004; Moura, Junior, Dantas, Araújo, & Collet, 2014).
Various authors have also highlighted play as a tool that provides a therapeutic effect for sick and or hospitalized children (Aley, 2002; Motta & Enumo, 2010; Quiles, Ortigosa, & Méndez, 2003). Therapeutic play differs from recreational play in that it is mediated by a trained therapist who deals with questions related to the fears and psychosocial well-being of the patient (Aley, 2002). It is also used to promote the following strategies: Information Seeking, Distraction, Emotional Expression or Regulation (Broening, 2014; Wiener, Battles, Mamalian, & Zadeh, 2011). Oliveira, Dias and Roazzi, (2003) aimed to verify the power of puppets and stories in ceasing anger and sadness. They used two control groups (non-hospitalized and hospitalized) and an experimental group (hospitalized). Results showed that emotional regulation modified according to the play activity function regardless of age and gender.
Other authors have designed programs, for specific diseases such as sickle cell disease, which includes identification and expression of feelings and the Coping Pain Game (Oliveira, Enumo, & Paula, 2017). Authors found a significant increase in the proportional adaptive coping strategies and a decrease in maladaptive coping strategies. Emotional regulation was also perceived to be greater after the intervention. This is significant because Emotional Regulation is one of the 12 coping categories in the Motivational Theory of Coping (MTC) (Skinner & Wellborn, 1994; Skinner & Zimmer-Gembeck, 2007, 2016). Vicente (2017) developed the "Coping Clock" program for hospitalized children and demonstrated that, in a control group, the mean adaptive macro categories were significantly higher at post-test. As for the intervention group, there was an increase in the average of adaptive coping behaviors and a decrease of the maladaptive coping. Oliveira (2014) conducted a cross-over study with patients in pain due to vein or arterial puncture divided into two groups. Group 1 saw audiovisual distractions before and during procedure while group two only received after. No differences were found between control and intervention groups in relation to stress symptoms and catastrophizing pain, however on administered scales, significant differences were found during periods with and without intervention as scores were lower during the period of distraction. Carry over effect analysis showed that approximately 30% of the estimated effect in pain relief were exclusively due to the distraction intervention.
Garioli (2016), to evaluate coping, adapted the Computer Assessment Instrument of Coping to Hospitalization (AEHcomp) (Motta & Enumo, 2010) to the MTC and verified its validity evidences. The new scale, named Coping with Hospitalization Scale (COPE-H), in two versions (COPE-H-Child and COPE-H-Caregiver) is composed of an administration booklet (both male and female versions) that contains 17 colored scenes depicting coping responses and 66 items inserted into thought balloon cards, a response form and a correction and interpretation form. The sample was composed of 133 children aged 6 to 12 years old and their caregivers. Exploratory factor analysis suggested three factors: 1) Maladaptive Coping with Hospitalization, 2) Adaptive Coping with Hospitalization, and 3) Involuntary and Voluntary Disengagement Coping with Hospitalization, with satisfactory Cronbach's alpha (.69 to .98).
Subsequently, other authors used the COPE-H to evaluate coping before and after intervention (Vicente, 2017) and coping in hospitalized children (Silveira, Lima, & Paula, 2018). However, this scale presents some limitations as it prioritizes the coping of hospitalization, and it does not evaluate issues related to disease and treatment comprehension, treatment procedures, side effects and outcomes and expectations for returning to school after hospitalization.
Therefore, the Coping Scale for Hospitalization, Ailment and Treatment (COPHAT) (Amaral, 2019) was designed, in two versions, to tap key coping elements in hospitalized children/adolescents (COPHAT-CA), and their respective parents/guardians perceptions (COPHAT-P). For each version of the scale, parents (COPHAT-P) and children/adolescents (COPHAT-CA), 35 items were created through interviews and literature review. The main authors studied for the generation of each item were studies from the field (Chiatonne, 1988; Compas, Jaser, Dunn, & Rodriguez, 2012; Nucci, 2002; Moraes & Enumo, 2008; Motta & Enumo, 2002, 2004a, 2004b, 2010). Items were pooled into five categories: 1) Aspects associated to disease and treatment comprehension; 2) Aspects related to hospitalization; 3) Aspects corresponding to treatment procedures and outcomes; 4) Aspects associated to treatment side effects and 5) Aspects related to expectations for returning to school.
This study aimed to present a personalized play intervention - the Promotion of Coping Hospitalization Program (PROCOPE-H) and evaluate its effectiveness. It was hypothesized that children and adolescents would report decrease in negative feelings (sadness, fear and anger) and increase in positive feelings (joy) after each session and that both children/adolescents and their parents/caregivers would perceive beneficial changes in behavior and positively evaluate the program as a whole.
Method
Participants
Seven children/adolescents (4 girls and 3 boys), aged 6 years to 14 years, and their parents/guardians participated. At least one child/adolescent from each of the following age groups participated: early childhood (6-7 years), middle childhood (8-10 years), late childhood/preadolescence (10-12 years), and adolescence (13-14 years). Four girls from each age group participated and three boys from each age group (except adolescence) took part.
Procedures
All parents/caregivers signed written consent forms. Children/adolescents over 12 years also signed written consent forms. Ethical approval was obtained through Ethical Committees of two universities (CAAE, n. 69087817.2.0000.5481, Comitê de Ética em Pesquisa da PUC-Campinas; n. 9087817.2.3001.5152, Comitê de Ética em Pesquisa Universidade Federal de Uberlândia).
The Program of Promotion of Coping with Hospitalization (PROCOPE-H) is based on four stages, as follows:
Stage 1: Obtain parental and child consent. Administer instruments COPHAT-CA (Amaral, 2019), COPE-H-Child (Garoli, 2016) and Adapted Hospital Play Evaluation Instrument (ABHa) (Motta & Enumo, 2002);
Stage 2: Score instruments and plan intervention on items scoring a 3 or 4. Resources are chosen based on ABHa responses and scored items content. For example, if child reported liking to read on ABHa and scored 3 or 4 on item on Disease Comprehension, a book on this topic is chosen. Intervention may be from 1 to 5 sessions, on average;
Stage 3: Conduct sessions. Before and after each session, evaluate how much the child is feeling anger, sadness, fear and joy. After the session, also question how the session went and if any other feelings were brought up. Ask how much the session helped with feeling and how the session went in general;
Stage 4: After finishing administering program instruments COPHAT-CA, COPE-H-Child, and Evaluation and Satisfaction Inventory (Amaral, 2019) calculate results.
Before intervention, children/adolescents were administered the child/adolescent version of the COPHAT-CA (Amaral, 2019), the ABHa and the COPE-H-Child in order to design sessions of the personalized play intervention the PROCOPE-H. Parents/caregivers responded to a sociodemographic protocol, the parent/guardian version of the COPHAT-P, and the parent version of the COPE-H-Caregivers.
A personalized play intervention the PROCOPE-H was individually planned for each participant, based on responses to the COPHAT-CA, ABHa and COPE-H-Child. Item responses scored 3 (almost always) or 4 (always) were considered questions needing to be addressed. ABHa responses were used to tap participants play preferences and therefore choose adequate resources. The PROCOPE-H was then carried out individually for each child/adolescent.
At the beginning and the end of each session, each participant was asked to rate each of the following feelings: fear, sadness, anger and joy on a scale from 0 (never) to 4 (always). After completion of PROCOPE-H, participants as well as their caregivers were given an Evaluation and Satisfaction Inventory containing seven questions addressing the following: learning about their disease and treatment, level of confidence felt in relation to facing the difficulties of hospitalization, level of confidence for facing procedures, facing treatment side effects, level of confidence in going back to school, knowing how to express and control feelings after working with the psychologist, level of satisfaction for participating in the activities proposed by the psychologist and overall evaluation of the PROCOPE-H.
Results/Discussion
Participants ranged in age from 6 to 14 years (M = 10 years, 3 months; SD = 32.97 months). The children/adolescents had varied needs for hospitalization: Leukemia (n = 2), Pancreatitis (n = 1), Diabetes (n = 1), abdominal mass (n = 1), attempting suicide (n = 1), under investigation for fainting (n = 1). They participated of 2 sessions in average (M = 2.00; DP = 1.15; min. = 1; max. = 4). Addressing guilt was a key intervention goal as the majority, 4 out of 7 participants reported this feeling (Table 1).
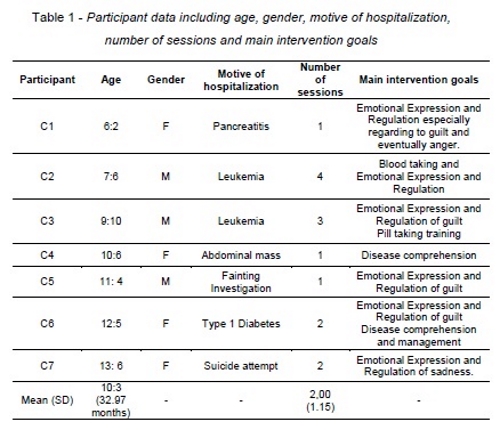
To reach the goals of each session different resources were chosen based on session goal, the age of patient and time. Three games, two activities and three books were used (Table 2). The names of the commercial games will remain in the Portuguese for readers to find material in the Portuguese language. Following is a description of how each one of the resources was used with patients and the results from session.
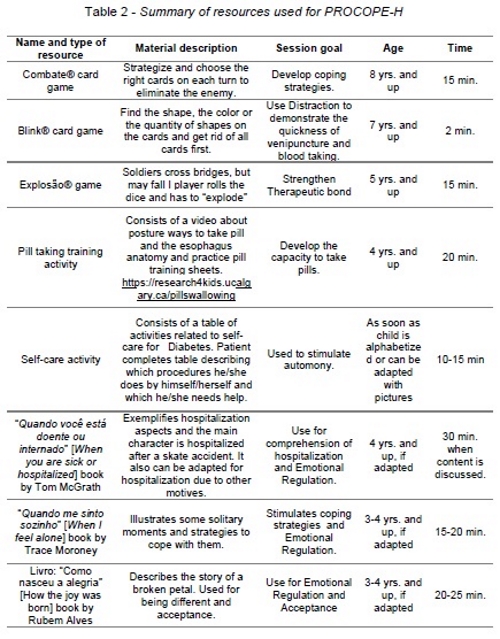
The Combate® (Combat) card game and the activity Pill taking training were used with C3, called Super M (boy, 9 yrs.), after verifying that he had issues related to Categories 2 and 3 from the COPHAT-CA. He reported a score of three (almost always) for items from both categories related to difficulty in pill taking and experiencing emotions such as fear, anger and sadness for being hospitalized. Therefore, after reading the book "Quando você está doente ou internado" (When you are sick or in the hospital), which approaches feelings related to hospitalization, patient and psychologist played the Combate® card game. This card game aims strategy. The goal is to eliminate the opponent's cards first. It was used as a warmup to develop coping strategies in Session 2 (S2). During S2, Super M created coping strategy cards. For each feeling/sensation he designed shields on one side of the card and wrote a phrase on the other. For fear he wrote "I am Super M and I can face fear"; for pain: "I am Super M and I can deactivate the pain"; for guilt, "I am Super M and I can win guilt over" and for anger "I am Super M and I can control my anger". At the end of S2, C3 reported that his anger decreased from 4 (always) to 0 (never) and added that the S2 helped him with anger because he did the 'combating the feelings deal". Interestingly enough, after the cards were laminated and given to the patient, he himself decided to make necklaces out of them with the help of his sister.
During the third and last session, the pill taking training activity was used. This activity consists of a video about posture for pill taking, the esophagus anatomy and practice pill training sheets. More information can be found on the following site: https://www.youtube.com/watch?v=Zxqs7flHJQc. C3 (Super M) had reported to sometimes feeling fear of being hospitalized on Category 2 and almost always felt fear when taking medicine on Category 3. During intervention, patient was engaged and even downloaded the video on his notebook. The video is in English, so the psychologist translated as it was being viewed. The flexibility of the esophagus anatomy is shown to guarantee the child that he/she will not choke while taking pills, nor while training. Training was performed with Tic Tacs® and SweeTarts®. C3 swallowed both. Training sheets were left with patient for him to train and test out different head positions.
The Self-Care activity was used with C6, called Doll (girl, 12 yrs.), as she reported issues related to Category 1: Disease Comprehension. The Self-Care Activity aims to pin down what a patient can already do alone and what activities require help. This patient reported being able to do the following activities alone: stick finger, put tape on monitor to measure blood glucose, see the results on the monitor, record the results, adjust insulin according to results, choose best place to inject insulin, prepare to inject, determine dose and inject insulin. She reported needing help from her mother to adjust diet. She did not know what measuring ketones meant and the psychologist explained it to her after talking to the medical team. Patient was encouraged to begin doing what her mother helped her with. Patient stated that the session helped her very much because she was distracted from being hospitalized. She was also stimulated to ask for things she wanted from the playroom such as coloring pencils. Patient role played requesting the psychologist for the pencils and then actually asked for them to the playroom keeper in front of the psychologist.
Before and after S1, C2, called Joaquim of Fear and Courage (boy, 7 yrs.), said he only had happy feelings, despite of being sad the day before for not being able to get out of bed. C2 reported high scores on Category 2 items for COPHAT-CA, and on items related to crying, anger and sadness on COPE-H. The Blink® card game was used with C2 aiming to demonstrate Distraction as a coping strategy and specifically the quickness of a blood withdrawal when one does not keep looking at blood being taken and distracts oneself with other thoughts. After this session, the mother affirmed that she was aware of her child´s fear and that the session was very helpful because her son was calmer at the next blood withdrawal. She also reported that the child stated: "I did it just the way the girl who played with me told me to do" and that is the reason why playing helped him. When asked at the end of the session, how it went, C2 said it was "cool."
At the initial feelings record of S2, C2 reported zero (0) point for joy and anger, and 4 points for fear and sadness because he was going to have to "get sticked". The game Explosion® (Explosion) was played to strengthen patient bond with psychologist as C2 had referred on the ABHa that he liked playing the game. This is a game in which soldiers cross bridges, but when the bomb explodes, they may fall down. Children coping with vein puncture is not always a positive linear event, in fact it may present some ups and downs, but persistence, as presented to C2 may diminish fear over time as C2 has showed courage. Data by Oliveira (2014) also indicates that resources for Distraction of vein puncture provided by intervention was effective in pain relief. However, more studies should be conducted. At end of session, C2 reported that sadness had went down to one point, while fear continued 4 points, and joy increased to 4 points because he played.
During the initial feelings report of S4, C2 was feeling zero point for anger, sadness and fear, and 4 points for joy because he was not going to "get sticked" that day". The book "Quando me sinto sozinho" (When I'm feeling lonely) was chosen to reinforce Self-Reliance and Support-Seeking, as the main character shares what makes him feel lonely and what strategies he uses to cope. Scores were maintained at the end of session, however C2 did affirm that he was happy because he had read the book.
The book "Quando você está doente ou internado" (When you are sick or in the hospital), by McGrath (2004) was used with C1, called Mary Guilt and Anger (girl, 6 yrs.), C4, called Pain and Lightness (girl, 10 yrs.) and C5, called Joy (boy, 11yrs.). The main character in the book is hospitalized after skate accident. The book presents feeling such as sadness, anger and fear as well as procedures performed in the hospital. C1 reported zero (0) point for joy, sadness, anger and one (1) point for fear. According to the patient, her fear was that her pancreas was going to grow. Her diagnosis was pancreatitis due to trauma from falling from her bicycle. Feeling guilt was a highlighted score on the COPE-H. During book reading, the patient stated that the skate was to blame and that is why the main character broke his leg and in the patient's case, her bicycle was to blame. Psychologist pointed out that accidents happen. C1 also talked about the friends she made at the hospital. At the end of the Session 4, fear maintained a score of one, however joy increased to 4 points. Nonetheless, a discussion occurred between the neighbor patient caretaker and some health care team members on the patients discharge and the C1 announced she was angry. Briefly it was pointed out that sometimes unpleasant things happen, and each patient may have different experiences at discharge.
C4, Pain and Lightness (girl, 10 yrs.), reported that the session helped her because reading the book made her feel more comfortable talking about her feelings with the psychologist. She also reported that she felt lighter. Therefore, this suggests that C4 used Support Seeking and the session contributed to Self-Reliance of patient.
After reading the book, C5, Joys (boy, 11yrs.), reported the same score of joy presented in the feeling's report of S4 because "Joy never leaves". When asked if other feelings emerged during session, he promptly answered happiness and curiosity in relation to the book and courage for not fearing needles. This event shows the potential of interventions on emotions not reported or not felt at the begin, but brought up during book reading, as a patient can recognize situations and feeing and thus obtain better coping strategies related to Problem-Solving, Support-Seeking, Accommodation and Self-Confidence. C5 participated in only one session and was then discharged. According to the study by Oliveira et al. (2017), participants perceived greater effectiveness of Emotional Regulation after intervention.
The book "Como nasceu a alegria", by Alves (2011) was used with C7, called Coping with Sadness (girl, 13yrs.). During the feeling's report of S1, C7 reported zero (0) point for all feelings and at post session reported zero (0) for all again, except for joy which was reported as one (1) point. This book was chosen because it is about a sad flower that discovers how joy is born from sadness and encounters self-acceptance. At end of S1, C7 affirmed that it helped her with the feeling of joy because she could talk about what happened for her to be hospitalized. The use of this book and others in this study is supported by findings in other studies (Bernardino et al., 2012; Fontenele et al., 2006).
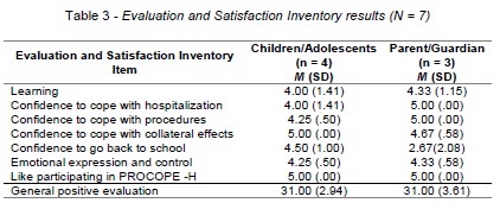
Four of the seven children/adolescents who participated in two or more sessions responded to the Child/Adolescent Evaluation and Satisfaction Inventory (C2, C3, C6 and C7). Participants answered seven questions on a Likert scale from 0 to 5 points. A final sum of these seven items were then pooled into a general score adding up to a minimum of 0 points to a maximum of 35. Questions were as follows:
1) When I participated in the activities with the psychologist, I think I learned about my illness and the treatment (0 = nothing to 5 = a lot);
2) To cope with the difficulties of hospitalization, I feel that I am now (0 = very insecure to 5 = a lot more confident);
3) To cope with the procedures, I feel I am now (0 = very insecure to 5 = a lot more confident);
4) To cope with the treatment effects, I feel I am now (0 = very insecure to 5 = a lot more confident);
5) I feel like I'm now (0 = very insecure to 5 = a lot more confident) about going back to school;
6) In relation to my feelings, I feel that after working with the psychologist, I know how to express and control them (0 = less to 5 = more);
7) In relation to participating in the activities with the psychologist (0 = I detested it a lot to 5 = I liked it a lot).
Three of the seven parent/caregivers whose child/adolescent in two or more sessions responded the Parent/Caregivers Evaluation and Satisfaction Inventory (P2, P3, and P7) regarding their perceptions of their child/adolescent. Item content was the same as the Child/Adolescent Evaluation and Satisfaction Inventory. P6 was not present at hospital discharge.
Child/Adolescent rated the Confidence to cope with collateral effects (M = 4.0, SD = 0.0) and Like participating in the PROCOPE-H (M = 4.0, SD = 0.0) items as highest on the Child/Adolescent Evaluation and Satisfaction Inventory, suggesting that PROCOPE-H impacted especially their confidence to cope with side effects and showing that chosen resources were well accepted by participants. Feeling more confident to go back to school was also reported (M = 4.50, SD = 1.00) indicating that participants felt comfortable with resuming routine with peers and teachers. The participants evaluated more confidence to cope with medical procedures (M = 4.25, SD = 0.50) and more emotional expression and control (M = 4.25, SD = 0.50). These two items could be related as medical procedures trigger emotional responses and regulation. PROCOPE-H aimed to target coping with procedures as well as evaluating with the participant his/her emotions before and after each session. The lowest evaluated items were Learning about their disease and treatment (M = 4.0, SD = 1.41) and the level of confidence felt in relation to coping with the difficulties of hospitalization (M = 4.0, SD = 1.41). Although these items were evaluated with the lowest score on the questionnaire, they are not low if fact. However, in futures studies, duration of hospitalization and number of hospitalizations should be accounted for as they were varied in this study and participants may already have learned about disease/treatment or had already established adapted coping strategies to hospitalization. Overall PROCOPE-H was well evaluated by participants (M = 31.00, SD = 2.94) (Table 3). As stated beforehand, a maximum of 35 points could be scored for general positive evaluation.
Parents or caregivers evaluated the PROCOPE-H well also (Table 3) and reported higher or equal scores on all items except Confidence in going back to school and Confidence to cope with collateral effects. Items rated as highest after the program by parents/caretakers were more confidence in coping with hospitalization (M = 5.00, SD = 0.00) and the medical procedures (M = 5.00, SD = 0.00). Next was Confidence to cope with collateral effects (M = 4.67, SD = 0.58) and following was Learning about their disease and treatment (M = 4.33, SD = 1.15) as well as having more emotional expressing and control (M = 4.33, SD = 0.58) were rated. Different than their children, they reported that participants were little confident to go back to school (M = 2.67, SD = 2.08). Differences may be due to the fact that interventions were focused on the children and not their parents; which could in turn warrant intervention for parents in future studies.
Conclusion
PROCOPE-H participants reported decreases in anger, sadness, and fear and increase in joy after sessions with psychologist as hypothesized. Emotional regulation is a topic which deserves more attention in future studies of child and adolescent hospitalization, as well as evaluating it systematically before and after interventions. Number of hospitalizations, duration of hospitalization and patient age should also be assessed or intervention effectiveness. PROCOPE-H was well rated by participants and their guardians indicating that the pilot was feasible, as study rationale proposed, and be continued to be used in future larger samples.
References
Aley, K. E. (2002). Developmental approach to pediatric transplantation. Progress in Transplantation, 12(2), 86-91. [ Links ]
Alves, R. (2011). Como nasceu a alegria. São Paulo: Paulus. [ Links ]
Amaral, J. D. H. F. A. (2019). Risco psicossocial familiar e coping da hospitalização em crianças e adolescentes: Avaliação e intervenção. Tese de Doutorado. Programa de Pós-Graduação em Psicologia, Pontifícia Universidade Católica de Campinas, Campinas, SP. [ Links ]
Bernardino, M., Elliott, A., & Rolim N. M. (2012). Biblioterapia com crianças com câncer. Informação & Informação, 17(3), 198-210. http://dx.doi.org/10.5433/1981-8920.2012v17n3p198 [ Links ]
Broening, C. V. (2014). Efeitos da preparação psicológica pré-cirúrgica em crianças submetidas a cirurgias eletivas e suas memórias. Tese de Doutorado. Programa de Pós-Graduação em Psicologia, Universidade Federal de Santa Catarina, SC. [ Links ]
Chiatonne, H. B. C. (1988). A criança e a hospitalização. In V. A. Angerarmi-Camon (Org.), A Psicologia no Hospital (pp. 42-132). São Paulo: Traço. [ Links ]
Compas, B. E., Jaser, S. S., Dunn, M. J., & Rodriguez, E. M. (2012). Coping with chronic illness in childhood and adolescence. Annual Review of Clinical Psychology, 8, 455-480. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3319320/ [ Links ]
Fontenele, M. D. F. S., Pinto, V. B., Andrade, F. J. M. D., Dias, A. P., & Moura, R. M. (2006). A biblioterapia no tratamento do câncer infantil. Diálogo Científico, 1(165), 1-24. [ Links ]
Franklin, G. C. (2010). Cadê o medo. São Paulo. Ciranda Cultural. [ Links ] Garioli, D. S. (2016). Escala de Coping da Hospitalização (COPE-H): Processo de adaptação. Tese de Doutorado. Programa de Pós-Graduação em Psicologia, Universidade Federal do Espírito Santo, Vitória, ES. [ Links ]
McGrath, T. (2004). Quando você está doente ou internado. Ajudar para curar crianças. São Paulo. Paulus. [ Links ]
Moraes, E. O., & Enumo, S. R. F. (2008). Estratégias de enfrentamento da hospitalização em crianças avaliadas por instrumento informatizado. PsicoUSF, 13(2), 221-231. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1413-82712008000200009&lng=pt&tlng=pt [ Links ]
Motta, A. B., & Enumo, S. R. F. (2002). Brincar no hospital: Avaliação do enfrentamento da hospitalização. Psicologia: Saúde & Doença¸ 3(1), 23-41. http://www.scielo.mec.pt/scielo.php?script=sci_arttext&pid=S1645-00862002000100003&lng=pt&tlng=pt [ Links ]
Motta, A. B., & Enumo, S. R. F. (2004a). Brincar no hospital: Estratégia de enfrentamento da hospitalização infantil. Psicologia em Estudo, 9(1), 19-28. https://dx.doi.org/10.1590/S1413-73722004000100004 [ Links ]
Motta, A. B., & Enumo, S. R. F. (2004b). Câncer infantil: Uma proposta de avaliação das estratégias de enfrentamento da hospitalização. Estudos de Psicologia (Campinas), 21(3),193-202. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-166X2004000300004&lng=pt&tlng=pt [ Links ]
Motta, A. B., & Enumo, S. R. F. (2010). Intervenção psicológica lúdica para o enfrentamento da hospitalização em crianças com câncer. Psicologia: Teoria e Pesquisa, 26(3), 445-454. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-37722010000300007&lng=pt&tlng=pt [ Links ]
Moura, F. M., Costa Junior, Á. L., Dantas, M. S. A., Araújo, G. C. B., & Collet, N. (2014). Intervenção lúdica a crianças com doença crônica: Promovendo o enfrentamento. Revista Gaúcha de Enfermagem, 35(2), 86–92. https://doi.org/10.1590/1983-1447.2014.02.41822
Nucci, N. A. G. (1997). O leão sem juba. São Paulo.
APACC. Oliveira, N. C. A. C. (2014). A técnica da distração no alívio da dor em crianças hospitalizadas: Um ensaio clínico randomizado. Dissertação de Mestrado. Universidade de São Paulo, Ribeirão Preto, SP. [ Links ]
Oliveira, C. G. T., Enumo, S. R. F., & Paula, K. M. P. (2017). A psychological intervention proposal on coping with pain for children with Sickle Cell Disease. Estudos de Psicologia (Campinas), 34(3), 355-366.http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-166X2017000300355&lng=en&tlng=en [ Links ]
Oliveira, S. G., Dias, M. G. B. B., & Roazzi, A. (2003). O lúdico e suas implicações, estratégias de regulação das emoções em crianças hospitalizadas. Psicologia: Reflexão & Crítica, 16(1), 1-13. https://dx.doi.org/10.1590/S0102-79722003000100003 [ Links ]
Pedrosa, A. M. (2000a). Entendendo e participando do tratamento do câncer infantil: Um livro de orientação para pais e pacientes – Quimioterapia (1) Recife: NACC.
Pedrosa, A. M. (2000b). Entendendo e participando do tratamento do câncer infantil: Um livro de orientação para pais e pacientes – Saúde bucal e Saúde oral (2). Recife: NACC.
Pedrosa, A. M. (2000c). Entendendo e participando do tratamento do câncer infantil: Um livro de orientação para pais e pacientes – Cateter (3). Recife: NACC.
Pedrosa, A. M. (2003). Entendendo e participando do tratamento do câncer infantil: Um livro de orientação para pais e pacientes – Dor (4). Recife: NACC.
Pedrosa, A. M. (2004). Quando seu colega de escola tem câncer. Recife: NACC. [ Links ]
Pedrosa, A. M., Marques, R., & Campos, S. (2011). Entendendo e participando do tratamento do câncer infantil: Um livro de orientação para pais e pacientes – Manual prático de terapia Intensiva (6). Recife: NACC.
Pedrosa, A. M., Monteiro, H., & Campos, S. (2012). Livrinho sabe tudo. Informações de saúde para crianças e adolescentes. Recife: NACC. [ Links ]
Quiles, M. J., Ortigosa, J. M., & Méndez, F. X. (2003). Preparación a la hospitalización y a la cirurgía. In J. M. Ortigosa, M. J. Quiles, & F. X. Méndez (Orgs.), Manual de Psicología de la Salud con niños, adolescentes y famílias (pp. 305-324). Madrid: Pirâmide. [ Links ]
Silveira, K. A. L, Lima, V. L., & Paula, K. M. P. (2018). Estresse, dor e enfrentamento em crianças hospitalizadas: Análise de relações com o estresse do familiar. Revista da SBPH, 21(2), 5-21. http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1516-08582018000200002&lng=pt&tlng=pt [ Links ]
Skinner, E. A., & Wellborn, J. G. (1994). Coping during childhood and adolescence: A motivational perspective. In D. L. Featherman, R. Lerner, & M. Perlmutter (Eds.), Life- span development and behavior (v. 12, pp. 91-133). Hillsdale, NJ: Erlbaum. [ Links ]
Skinner, E. A., & Zimmer-Gembeck, M. J. (2007). The development of coping. Annual Review of Psychology, 58, 119–144.
Skinner, E. A., & Zimmer-Gembeck, M. J. (2016). The development of coping: Stress, neurophysiology, social relationships, and resilience during childhood and adolescence. New York: Springer. [ Links ]
Vicente, S. R. C. R. M. Proposta de intervenção psicológica para melhorar as estratégias de enfrentamento da criança hospitalizada. Tese de Doutorado. Programa de Pós-Graduação em Psicologia, Universidade Federal do Espírito Santo, Vitória, ES. [ Links ]
Wiener, L., Battles, H., Mamalian, C., & Zadeh, S. (2011). ShopTalk: A pilot study of the feasibility and utility of a therapeutic board game for youth living with cancer. Support Care Cancer, 19, 1049-1054. http://dx.doi.org/10.1007/s00520-011-1130-z. [ Links ]
1 Psicóloga pela Universidade Federal de Uberlândia (UFU), com especialização em Psicossomática pelo Instituto Sedes Sapientae, em Análise Transacional pela União Nacional de Análise Transacional-UNAT e em Psicologia Clínica na Abordagem Comportamental-Cognitiva em Terapia pela UFU. Mestre em Imunologia e Parasitologia Aplicadas pela UFU. Doutora em Psicologia pela Pontifícia Universidade Católica de Campinas. Atualmente, é Psicóloga da Gerência de Psicologia e Psicopedagogia da Saúde do Hospital das Clínicas da UFU. Preceptora e Tutora do Programa de Residência Multiprofissional em Saúde da Faculdade de Medicina da UFU, na área de Saúde da Criança. Atua no Setor de Oncologia, com crianças e seus familiares no ambulatório, e no Setor de Hemodíálise. Bolsa de doutorado da Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES/MEC). Contato: jdhfdapsi@yahoo.com.br.
2 Psicóloga pela Pontifícia Universidade Católica de Campinas (PUC-Campinas). Mestre em Educação Especial pela Universidade Federal de São Carlos. Doutora em Psicologia Experimental pela Universidade de São Paulo. Professora Emérita da Universidade Federal do Espírito Santo. Atualmente, é Professora Doutora do Programa de Pós-Graduação em Psicologia e do Programa de Pós-Graduação em Ciências da Saúde da PUC-Campinas. Líder do Grupo de Pesquisa em Psicologia da Saúde e Desenvolvimento da Criança e do Adolescente (PUC-Campinas). Foi bolsista de produtividade em pesquisa do CNPq entre 2001-2018. É Editora Associada da Revista Estudos de Psicologia (Campinas). Bolsista de produtividade em pesquisa em nível 1B do Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). Contato: sonia.enumo@puc-campinas.edu.br.














