Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Contextos Clínicos
versão impressa ISSN 1983-3482
Contextos Clínic vol.8 no.1 São Leopoldo jun. 2015
https://doi.org/10.4013/ctc.2015.81.01
ARTIGOS
The indication and agreement to initiate treatment during the initial evaluation of psychodynamic psychotherapy
Indicação e concordância em iniciar tratamento durante avaliação inicial para psicoterapia psicodinâmica
Marina Bento GastaudI; Fernando BassoII; Lucas Seiki Mestre OkabayashiIII; Maria Lúcia Tiellet NunesIV; Cláudio Laks EizirikV
IUniversidade Federal do Rio Grande do Sul. Rua Ramiro Barcelos, 2400, 2º andar, 90035-003, Porto Alegre, RS, Brasil. marinagastaud@hotmail.com
IIPontifícia Universidade Católica do Rio Grande do Sul. Av. Ipiranga, 6681, Prédio 15, 90619-900, Porto Alegre, RS, Brasil. psicfernandobasso@gmail.com
IIIUniversidade Federal do Rio Grande do Sul. Rua Ramiro Barcelos, 2400, 2º andar, 90035-003, Porto Alegre, RS, Brasil. lucas.seiki@gmail.com
IVPontifícia Universidade Católica do Rio Grande do Sul. Av. Ipiranga, 6681, Prédio 15, 90619-900, Porto Alegre, RS, Brasil. marialuciatiellet@gmail.com
VUniversidade Federal do Rio Grande do Sul. Rua Ramiro Barcelos, 2400, 2º andar, 90035-003, Porto Alegre, RS, Brasil. ceizirik.ez@terra.com.br
ABSTRACT
This naturalistic and longitudinal study, following 557 outpatients who sought psychodynamic psychotherapy, aimed to verify factors associated with non-indication for psychodynamic psychotherapy and to establish predictors of non-agreement to initiate treatment for patients indicated for this treatment. It found that patients consulting for somatic or attention problems and/or with a low educational level were less likely to be indicated for psychodynamic psychotherapy; patients perceiving their symptoms as intense were more likely to be indicated for this treatment. The following were the predictors of non-agreement to initiate psychodynamic psychotherapy: low educational level, low family income, diagnosis of schizophrenia, schizotypal or delusional disorders, depressive problems and/or never experiencing psychotherapy. Psychodynamic psychotherapy, as every other treatment, appears to be suitable for a specific group of patients. Unless the technique performed by psychotherapists during psychodynamic psychotherapy's initial stages is improved, the relevance of referring a non-concordant profile to this psychotherapeutic modality is herein discussed.
Keywords: treatment indication, treatment compliance, suitability, premature discontinuation, psychodynamic psychotherapy.
RESUMO
Este estudo naturalístico e longitudinal, seguindo 557 pacientes ambulatoriais que buscaram psicoterapia psicodinâmica, teve por objetivo verificar fatores associados com não indicação para psicoterapia psicodinâmica, bem como estabelecer preditores de não concordância em iniciar tratamento entre pacientes que receberam indicação para esta modalidade terapêutica. A investigação encontrou que pacientes com queixas de problemas somáticos ou problemas de atenção e/ou com baixa escolaridade tiveram menor probabilidade de receberem indicação para psicoterapia psicodinâmica; pacientes que percebiam seus sintomas como intensos tiveram maior probabilidade de receberem indicação para este tratamento. Foram preditores de não concordância em iniciar psicoterapia psicodinâmica: baixa escolaridade, baixa renda familiar, diagnóstico de esquizofrenia, transtorno esquizotípico ou delirante, problemas depressivos e/ou estar buscando psicoterapia pela primeira vez. A psicoterapia psicodinâmica, como todas as formas de tratamento, parece ser adequada para um grupo específico de pacientes. A menos que as técnicas utilizadas pelos terapeutas durante as fases iniciais da psicoterapia psicodinâmica sejam aperfeiçoadas, a relevância de indicar o perfil de pacientes não concordantes para esta modalidade terapêutica é aqui discutida.
Palavras-chave: indicação para tratamento, aderência ao tratamento, contraindicação, abandono precoce, psicoterapia psicodinâmica.
Introduction
Before initiating treatment when receiving a potential patient for psychodynamic psychotherapy, the psychotherapist must perform an initial evaluation and decide the best specific course of action. This preliminary assessment aims to establish the best therapeutic approach for the case, based on indication or contraindication criteria (Rueve and Correll, 2006), and develops a therapeutic alliance. After the initial evaluation period, if the psychotherapist recommends psychodynamic psychotherapy for the patient, treatment goals are established and the contract is discussed between the psychotherapist and the patient. If both individuals agree to initiate treatment, psychodynamic psychotherapy commences. This assessment period typically requires several sessions/ interviews (Truant, 1998), generally, 2 to 4 (Etchegoyen, 2010).
Patient withdrawal during this initial period commonly occurs. The literature on this topic, although outdated, reveals this phenomenon: of 100 potential patients who contact a mental health service, only 50 will attend the initial interview (Garfield, 1994; Sparks et al., 2003). Thirty-three individuals will attend the first session of psychotherapy (Philips, 1985), 20 will remain in psychotherapy at the third session (Pekarik, 1983) and fewer than 17 will remain in treatment at the end of the tenth session (Garfield, 1994). Thus, the initial phase of psychotherapy is fundamental for treatment continuation (Barrett et al., 2008).
There is good evidence for analytically oriented psychotherapy for a range of disorders, in addition to studies indicating improvements in global functioning, interpersonal relationships, quality of life and patients' wellbeing (Leichsenring, 2005; Jung et al., 2007). Nevertheless, psychotherapy, like any other effective treatment in medicine or psychology, may lead to negative effects in either the patient or those around him (Crown, 1983; Linden, 2013). It is necessary to study the factors associated with an indication and decision to initiate treatment, specifically for insight-oriented psychotherapies because they require different prerequisites for the participation in psychotherapeutic work.
The systematic selection of patients results in a better longer-term outcome for psycho-dynamic psychotherapy when compared to a control procedure of random treatment selection (Watzke et al., 2010). Because systematic treatment selection appears to optimize the treatment outcome for psychodynamic psychotherapy, pursuing systematic treatment assignment strategies in mental healthcare settings is a worthwhile endeavor. However, clinical decision-making regarding the suitability of psychological therapies is hampered by limitations of psychotherapy research and our failure to understand therapeutic mechanisms (Fonagy, 2010). The conflicting evidence regarding a patient's characteristics associated with indication and agreement to initiate psychodynamic psychotherapy results from the absence of general consensus on indication/ contraindication criteria (Fonagy, 2010). Research is necessary to refine the criteria used to decide the allocation of individual and collective resources (Schestatsky, 1989).
Valbak (2004) reviewed the empirical studies published in the previous 20 years on outpatients' pre-therapy suitability for psychoanalytic psychotherapy and observed the following most promising variables with the highest correlations with a good outcome: a good quality of object relations, psychological mindedness and motivation for change. Nine years later, De Jonge et al. (2013) reviewed studies relating to patient characteristics, predictive factors and clinical judgments regarding the outcome of psychodynamic psychotherapy. Although observing similar results, the authors claim that object-related functioning, motivation and psychological mindedness appear to have low to moderate influence on the outcome of psychodynamic psychotherapy. However, in practice, the suitability of treatment was actually determined based on the clinical judgment of patient characteristics and an assessment of whether the psychotherapeutic process was likely to lead to a profitable patient-clinician relationship (De Jonge et al., 2013).
Psychodynamic clinicians agree that the motivation for treatment (a spontaneous search for treatment or availability of financial resources) is crucial to indicate psychodynamic psychotherapy but also postulate other possible factors associated with indication: the patient's current moment in life (considerable psychological distress, intact reality testing, an absence of acute symptoms that places patients' lives at risk), the patient's diagnosis and defensive style (Dewald, 1964; Kernberg, 2004; Keidann and Dal Zot, 2005; Gabbard, 2005). Therefore, it is imperative to empirically verify which characteristics of patients are related to clinical judgments when indicating psychodynamic psychotherapy. Because it is not necessarily inadvisable that some patients disagree with the initiation of psychodynamic psychotherapy, it appears important to evaluate patients' decisions to initiate treatment, particularly because this decision is an important component of psychotherapy indication. Knowing the variables associated with an agreement to initiate treatment would also enable the planning of more appropriate interventions for this clinical population. Thus, this study aimed to assess associations between patient characteristics (gender, age, education, income, diagnosis, source of referral, reason for consultation, medical history, symptoms, defensive style and quality of life) and the training level of the psychotherapist for the (a) psychotherapist's decision to indicate/contraindicate psychodynamic psychotherapy and (b) patient's decision to initiate treatment, once indicated.
Methods
This longitudinal and naturalistic study was performed in an outpatient clinic in the city of Porto Alegre, Southern Brazil. The clinic is part of a three-year post-graduation training course for psychodynamic psychotherapy. The treatments performed in this institution are open-ended and count on the weekly attendance established by the patient and psychotherapist at the initiation of psychotherapy. Psychotherapies performed in this clinic are very heterogeneous regarding the weekly frequency and treatment duration. Most patients consult once a week and the frequency often varies along the same case; among patients who started treatment between 2009 and 2014 and have already left the clinic (considering discharges and dropouts), the mean duration of psychotherapy was 7.3 months (standard deviation = 8.7). The therapists who work at this outpatient clinic operate with several theoretical frameworks within the psychodynamic approach, but favor authors of contemporary reference - such as object relations theory (especially Bion, Winnicott, Kaës and Aulagnier), and self psychology (Kohut).
The initial evaluation procedure occurs at two time frames: (i) an intake interview is conducted to initially screen patients who seek psychodynamic psychotherapy and (ii) if psychodynamic psychotherapy is indicated by the interviewer, the patient participates in a second evaluation with a psychotherapist. The 12 interviewers that performed the intake interviews were psychologists, specialists in psychodynamic psychotherapy, and had at least four years of clinical interview experience. The 58 psychotherapists were psychologists; 58.6% had previously completed the specialization course at the time of the study.
The study sample comprised all patients over 18 who sought treatment between May 2009 and December 2010 and agreed to participate in the study (signing an informed consent after the research goals and methods had been fully explained). The project was approved by the Research Ethics Committee of the Municipal Health Department of Porto Alegre.
Instruments
A clinical and socio-demographic questionnaire - Self-provided patient data were obtained from the initial registration form completed by patients during the intake interview and records of the psychologists who performed these interviews.
The World Health Organization Quality of Life - brief version (WHOQOL-Brief) - This instrument assesses patients' quality of life in four domains: Physical, Psychological, Social Relationships and Environment. The Brazilian version of the WHOQOL instruments was developed by the WHOQOL Centre for Brazil (Fleck et al., 2000).
The Symptom Check-List-90-Revised (SCL-90-R) - This instrument assesses nine dimensions of patients' symptomatology: Somatization, Obsessiveness/Compulsivity, Interpersonal sensitivity, Depression, Anxiety, Hostility, Phobic anxiety, Paranoid ideation and Psychoticism. This instrument also provides a measurement of the patient's global severity (GSI - Global Severity Index), the number of symptoms indicated by the patient within 90 possibilities (PST - Positive Symptom Total) and the intensity of the presented symptoms scored by the patient (PSDI - Positive Symptom Distress Index) (Derogatis and Savitz, 2000; Laloni, 2001).
The Defense Style Questionnaire (DSQ-40) - This instrument assesses patients' defensive style and enables the classification of the defenses used by a patient in three categories: mature, neurotic and immature factors. The instrument was originally developed by Bond et al. (1983), reorganized in the current format by Andrews et al. (1993) and translated and validated for the Brazilian population by Blaya et al. (2004, 2007).
Definitions of Terms
Previous psychiatric and psychotherapeutic treatment: treatment approaches conducted by a psychiatrist and only based on medication were considered psychiatric treatments; psychotherapeutic treatments included all psychotherapeutic approaches conducted by either psychiatrists or psychologists.
The reason for seeking treatment was defined according to the description given by the patient to the professional who conducted the initial interview. The interviewers rated the patients' complaints based on the definitions proposed in the internalizing, externalizing, neutral, and social behaviors scales of the ABCL - Adult Behavior Checklist (Achenbach and Rescorla, 2003). The categories included depressive problems, anxiety problems, somatic problems, avoidant personality problems, attention deficit/hyperactivity problems, antisocial personality problems.
Diagnosis: the patient's initial diagnosis provided by the interviewer through the International Classification of Diseases - 10th Edition (ICD-10) was considered. All interviewers were previously trained for this diagnostic classification system and received systematic supervision and guidance regarding the patients' diagnoses. For analytical purposes, the broad categories that comprise the chapter on mental and behavioral disorders were used (World Health Organization, 1992):
• F00-F09: Organic, including symptomatic, mental disorders
• F10-F19: Mental and behavioral disorders because of psychoactive substance use
• F20-F29: Schizophrenia, schizotypal and delusional disorders
• F30-F39: Mood [affective] disorders
• F40-F48: Neurotic, stress-related and somatoform disorders
• F50-F59: Behavioral syndromes associated with physiological disturbances and physical factors
• F60-F69: Disorders of adult personality and behavior
• F70-F79: Mental retardation
• F80-F89: Disorders of psychological development
• F90-F98: Behavioral and emotional disorders with an onset typically occurring in childhood and adolescence
• F99: Unspecified mental disorder.
Non-agreement to initiate treatment: it is important to distinguish a patient's withdrawal from psychotherapy dropout during this initial period. Garfield (1989) proposes that dropout is when the patient undergone psychotherapy and the evaluation period (initial interviews) precedes the psychotherapeutic process. The evaluation stage (the entire evaluation period preceding the contract) is a time when both patient and psychotherapist are evaluating whether this is a treatment to significantly invest in (Clarkin et al., 2006). Thus, the term "dropout" would be used to describe patients who agree to initiate psychotherapy but interrupt treatment before it is complete.
Data analysis
The variables were initially characterized in terms of frequencies and percentages. To detect associations between the outcomes and categorical variables (gender, education, income, diagnosis, source of referral, reason for consultation, medical history and training level of the psychotherapist), a Chi-Square test was performed. For less prevalent diagnoses, an association with the outcomes was determined using a Fisher's exact test. Because nearly all continuous variables had a normal distribution, a Student's t-test was performed to verify the association between outcomes and age, symptoms, severity of symptomatology, defensive style and quality of life. The variable without a normal distribution (Phobic Anxiety scores) was analyzed using a Mann-Whitney test. A Poisson regression was performed to verify the predictors of indication/non-indication and agreement/non-agreement to initiate psychotherapy (Barros and Hirakata, 2003; McNutt et al., 2003). All factors that were associated with the outcomes of a p value equal or less than 0.20 entered the stepwise regression. After including all these factors, those with a p value higher than 0.10 were excluded until the final model was achieved (a backward selection of variables) (Hosmer and Lemeshow, 2000). The results with a p value equal or inferior to 0.05 were considered significant.
Seventeen patients did not appropriately answer the WHOQOL-Brief, 41 did not appropriately answer the SCL-90-R and 51 did not appropriately answer the DSQ-40; the results of these cases were estimated by multiple imputation (Schafer, 1997), accounting for the answer standards from variables associated with the lost results.
Results
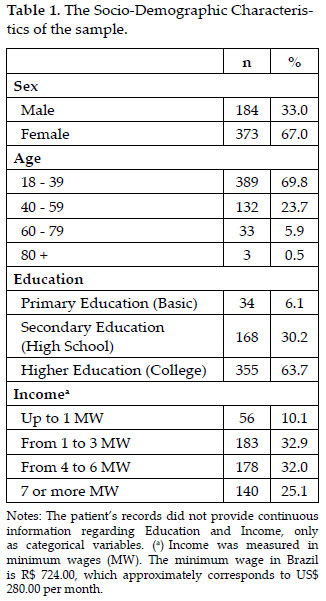
Between May 2009 and December 2010, 638 patients sought treatment in the clinic. Of these patients, 557 agreed to participate in this research, thus generating the final sample. Tables 1 and 2 describe the sample. The mean age of the patients was 35.2 years old (standard deviation = 13.1).
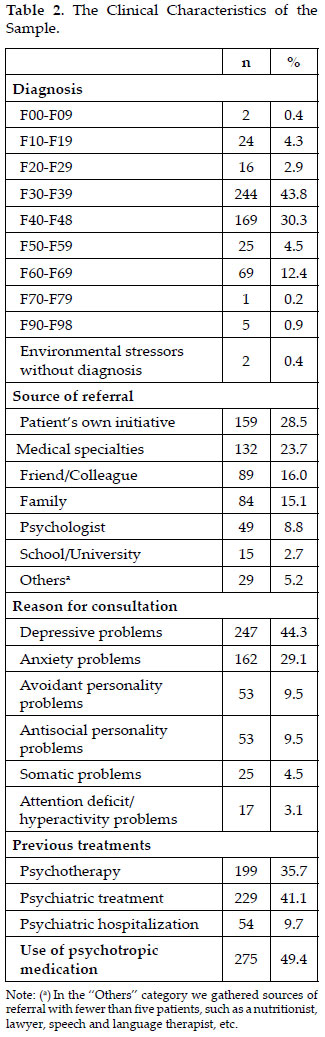
The highest percentage of patients was referred to specialist professionals after the intake interview (n = 161; 28.9% of the total sample). Thirty-six patients (6.5%) were referred to trainees (undergraduate students), 81 (14.5%) to psychotherapists in their first year of specialization training practice, 69 (12.4%) to psychotherapists in their second year and 82 (14.7%) to psychotherapists in their third year of training practice.
Indication for Psychotherapy
Psychodynamic psychotherapy was not indicated for 54 (9.7%) patients after the intake interview. A further 199 (35.7%) patients did not agree to initiate psychotherapy, and 304 (54.6%) agreed to initiate treatment. The interviewers contraindicated psychodynamic psychotherapy for 9.7% of the cases, but no psychotherapist contraindicated psychodynamic psychotherapy during the initial evaluation stages.
The final regression model was composed of the variables described in Table 3. Therefore, this study observed that patients consulting for somatic or attention problems and/or with a low educational level were less likely to be indicated for psychodynamic psychotherapy; patients perceiving their symptoms as intense were more likely to be indicated for this treatment.
Agreement to initiate Treatment
Among patients who had an indication for psychodynamic psychotherapy, 60.4% agreed to initiate treatment. Patients who did not agree to initiate treatment interrupted the evaluation process after the intake interview (n=74; 37.2%), 1 interview (33; 16.6%), 2 interviews (30; 15.1%), 3 interviews (23; 11.6%), 4 interviews (26; 13.1%), 5 interviews (4; 2.0%), 6 interviews (4; 2.0%), 7 interviews (3; 1.5%) or 8 interviews (2; 1.0%). Therefore, in 93.5% of cases in which the patient did not agree to initiate treatment, the initial evaluation phase involved the initial four interviews with a limit that could be extended to eight appointments (an average of 1.74 interviews, in addition to the intake interview - SD=1.87).
Table 4 shows the reasons provided by non-concordant patients for not initiating treatment. Altogether, 36.2% of cases did not justify the reason for discontinuing the appointments, simply not attending the following scheduled session. Financial problems were the most prevalent reason for non-concordance (17.1%). One patient claimed to be already satisfied with the results and only attended the screening interview. When informed how psychotherapy works, fifteen patients did not agree with the indication for psychodynamic psychotherapy and stated that this form of assistance would not be necessary.
The variables described in Table 5 comprised the final model. Therefore, the following were predictors of non-agreement to initiate psychodynamic psychotherapy during the initial evaluation stages: a low educational level, low family income, diagnosis of schizophrenia, schizotypal or delusional disorders, depressive problems and/or never participating in psychotherapy.
Discussion
In this study, the interviewers had a pattern of not indicating psychodynamic psychotherapy in the initial interview. The variables that were independently associated with treatment indication included education level, reason for consultation (somatic or attention problems) and symptom intensity.
Somatic and attention problems are complaints that are frequently associated with conditions that necessitate pharmacological treatment and are more frequently referred to physicians, psychiatrists or neurologists than psychotherapists. This referral process is a possible explanation for these problems being associated with a non-indication for psychotherapy. Furthermore, in order to treat patients with somatic complaints in psycho-dynamic psychotherapy it is necessary to consider the technical and theoretical precepts of Psychoanalytic Psychosomatics, taking into account that some somatic complaints may have psychological origins and repercussions.
The motivation to initiate psychotherapy depends on the patient's psychological distress level. It appears reasonable that interviewers indicate psychodynamic psychotherapy for patients who perceive their symptoms as intense and, therefore, show great motivation.
Patients provided various reasons for not initiating treatment, some of which (such as family problems, health problems or moving to another city) did not necessarily involve a non-agreement with the treatment modality. Nevertheless, most patients did not initiate treatment because of the characteristics of the interviewers, psychotherapists, clinic or treatment modality. As previously noted, psychodynamic psychotherapy is not suitable for every type of patient. Since the time when psychoanalysis was the predominant form of psychotherapy, modified psychoanalytic techniques and other methods and approaches have dominated the psychiatric treatment scene. Psychotherapists have selected patients for psychotherapy in a variety of manners, from quick clinical presumptions to extensive long-lasting examinations and testing, and based on all types of grounds, from idiosyncratic beliefs to formal theories or research data (Valbak, 2004). The selection of patients for different forms of psychotherapy remains a challenge, and the assessment of patient suitability is a difficult task in clinical practice.
Therefore, the decision to forego treatment is not necessarily harmful to the patient, considering that the initial assessment of his/her suitability for this specific treatment was not always well performed. Furthermore, because psychotherapies can produce side effects (Berk and Parker, 2009), it is not necessarily inadvisable that some patients disagree with the initiation of such treatment.
The following comments will focus on raising possible methods to improve the initial evaluation of patients considered for psycho-dynamic psychotherapy and launching possible technical changes to increase treatment compliance in cases of correct indication. Education level, income, diagnosis (schizophrenia, schizotypal or delusional disorders), depressive problems and the absence of previous psychotherapy were factors independently associated with patients' non-agreement to initiate psychotherapy.
The inverse relationship between education level and patient withdrawal during the early stages of psychotherapy, as shown in this study, corroborates the results obtained by Wierzbicki and Pekarik (1993) in their me-ta-analysis 20 years ago. Higher levels of education appear to be related to more benefits in psychotherapy (Olfson et al., 2010), most likely because patients with higher education levels identify themselves more with their psychotherapists, professionals with high education levels (Garfield, 1986; Weirzbicki and Pekarik, 1993). Furthermore, a low education level is related to expectations of fast and immediate psychotherapeutic effectiveness (Westmacott and Hunsley, 2010), thus leading to lower compliance. Specifically for psychodynamic psychotherapies, higher levels of education may also predict the suitability for treatment because they are related to a greater capacity for mentalization, introspection and a capacity to grasp metaphoric concepts.
Regarding the patient's income, reviews performed in the 1970s and 1980s (Baekeland and Lundwall, 1975; Garfield, 1986) noted that the economic position of the patient was inversely related to treatment compliance. In these cases, the absence of resources to invest in long-term psychotherapy may be responsible for the lower compliance (Hauck et al., 2007; Wang, 2007). Difficulties in accessing the clinic (dependency on unsatisfactory or insufficient transportation), incomplete information regarding their health conditions (dependency on public services with long waiting lines) and the limited knowledge regarding the functioning of psychotherapy are common problems faced by patients with financial difficulties.
In this study, patients who had previously participated in psychotherapy agreed more often to initiate treatment than patients initiating psychotherapy for the first time. This result is in accordance with previous studies (Werner-Wilson and Winter, 2010). Previous experiences with psychotherapy most likely led to more realistic expectations regarding its functioning, thus decreasing frustration concerning the frequency of sessions, duration of treatments and expectations regarding the psychotherapist.
There is a possibility that psychodynamic psychotherapy should not be the primary choice of treatment for patients presenting a diagnosis of schizophrenia, schizotypal or delusional disorders, even when combined with psychotropic medication. This study showed that patients with these diagnoses tended to disagree with the initiation of psychotherapy. According to Krarup (2008), there is evidence for the effect of cognitive behavioral psychotherapy on reducing persistent positive symptoms, improving social functioning, improving insight and reducing the time to remission. There is no evidence of any effect of psychodynamic psychotherapy on relapse rates, but the model is helpful for psychotherapists to obtain an empathic understanding of patients (Krarup, 2008). However, this perspective is not unanimous among clinicians (Valbak et al., 2003; Brenner and Volkan, 2004; Margison, 2005; Gibbs, 2007). The treatment for patients with psychotic spectrum disorders could combine individual psychodynamic psychotherapy, psychopharmacology, family approaches, intensive psychosocial engagement, and educational treatment (Rosenbaum et al., 2006; Tillman, 2008). Nevertheless, according to psychodynamic theory, psychotic patients resist initiating and sustaining any type of treatment because of their narcissistic relationships, primitive defense mechanisms, particularly splitting, and omnipotent denial (Murawiec and Zechowski, 2007).
In this study, depressive problems included constant crying, an absence of appetite, difficulty in decision-making, sleeping problems, low energy and sadness. These problems are difficult to tolerate, and some patients require immediate relief, whereas the nature of the psychodynamic approach tends to be exploratory, less directive and its visible results typically require many sessions. There is also the characteristic pessimism of patients presenting depressive problems in relation to initiating any task. Depressed patients may also only partially respond to treatment or prematurely withdraw (Taylor et al., 2012). Of those showing these sub-optimal therapeutic responses, Stimpson et al. (2002) estimated that a minimum of 30% of patients experience recurrent treatment failures. Some patients, perhaps following many failed attempts at treatment, may withdraw from all treatment endeavors. These patients feel they have exhausted all treatment possibilities and become seriously neglected and deprived (Taylor et al., 2012). Accumulating evidence suggests that to be effective, treatments for these depressions must be more complex and longer than required for simpler disorders (Hollon and Ponniah, 2010). Because patients' outcome expectations play an important role in initial appointment attendance (Swift et al., 2012), the desire for immediate relief should be explored in the early stages of psychodynamic psychotherapy.
One of the limitations of this study was that it focused nearly entirely on patient variables and failed to cover the characteristics of psychotherapists. The analytical field and therapeutic alliance established during the initial stages of psychotherapy play an important role in the concordance to remain in treatment (Piper et al., 1999; Barrett et al., 2008), but these roles were not focused on in the present research because they have been previously well-established in the literature.
Nevertheless, the only variable related to the psychotherapist tested in the present study, training level, did not show any association with the patients' decision to initiate treatment. The literature is contradictory on the relationship between the experience of the psychotherapist and patients' compliance with treatment (Krauskopf et al., 1981; Jenkins et al., 1986). In principle, it should be expected that the higher the training level, period of study and clinical experience of the psychotherapist, the higher the chance he/she will be qualified to perform a good evaluation and enable a good therapeutic alliance. However, other factors may compensate for the absence of experience, such as the possibility to supervise all cases and dedication to each specific case (because they have fewer patients). The enthusiasm of new psychotherapists, which Malan (1976) called "therapeutic eros", may play its role in this compensation.
We need to consider that, in psychodynamic psychotherapies, unconscious dimensions of the therapist and the patient (such as transference, countertransference, resistance to improvement, etc.) play an important role in adherence to treatment and its outcome. Quantitative research with large samples can hardly include the analysis of this unconscious dimension; this is a limitation of this research. We suggest the realization of single case studies, with process assessments - not only results - to try to understand the role that unconscious factors can play in understanding the indication and agreement to initiate treatment.
Despite this study being based on a large sample of patients, the data were collected in only one clinic with particular features that limited the generalization of the results. Moreover, we decided to perform a naturalistic study based on the natural environment of psychotherapies and not one deliberately established for research. This methodological approach has the advantage of providing a less artificial portrait of the reality of psycho-dynamic psychotherapies, but has the methodological disadvantage of a loose control of the studied variables.
Notwithstanding these limitations, this study emphasizes the possible characteristics of patients who do not adhere to psychodynamic psychotherapy. These results must be tested in further studies, in other clinics and cultural contexts, to draw definitive conclusions regarding the complex phenomenon of indication and decisions to initiate psychotherapy.
Conclusions
In this study, the following factors were associated with a non-indication for psychodynamic psychotherapy: consulting for somatic or attention problems, having an education level limited to primary education and the patient's perception that his/her symptoms have little intensity. The following factors were associated with not initiating psychodynamic psychotherapy: the absence of higher education, a family income lower than 4 Brazilian minimum wages, diagnosis of schizophrenia, schizotypal or delusional disorders, consulting for depressive problems and/or having no previous experience in psychotherapy.
Even if this study has analyzed patients during their evaluation period for psychotherapy, no patient referred for psychotherapy after the intake interview received a contra-indication for psychotherapy by his/her psychotherapist. Psychodynamic psychotherapists must consider the profile of patients who disagree with treatment initiation when indicating this psychotherapeutic modality and avoid treatment attempts that tend to fail. The psychodynamic technique adopted during the initial interviews must be improved to encompass the profile of probable non-concordant patients, or the criteria of indication and contraindication for psychodynamic psychotherapy must be reviewed and employed more rigorously by clinicians.
Some of the predictors of patients' early treatment interruptions observed in this study show inconsistency in the literature and must be better studied. However, other predictors have been associated with treatment dropout and non-adherence to psychotherapy in several studies, such as low income and low education (Baekeland and Lundwall, 1975; Wierzbicki and Pekarik, 1993; Garfield, 1994; Barrett et al., 2008; Swift and Greenberg, 2012). Psychotherapists that provide assistance to these cases must be aware that changes in standard psychodynamic techniques might be necessary for the success of these treatments, such as providing educational information about the patients' diagnosis, the employed technique of treatment and operationalization of psychotherapy (Walitzer et al., 1999; Wang et al., 2000; Edlund et al., 2002; Beutler et al., 2002; Reis and Brown, 2006; Barrett et al., 2008), and the use of aspects of the motivational interview to help patients explore and resolve their ambivalent feelings regarding treatment (Miller and Rollnick, 1991; Swart et al., 2007; Edlis-Matityahou, 2010).
To provide assistance to the low income and education population groups, it may not be sufficient to offer reduced fees; clinics must facilitate these patients' access to assistance by providing transportation and information regarding the disease and treatment. For those patients who do not fulfill the indication criteria for classic or standard psychodynamic psychotherapy, it may be useful to include a period of pre-therapy in the initial interviews that develops the capability to achieve insight. Despite the inconsistency of the techniques used in this pre-therapy period and classical psychodynamic principles, the literature has shown the potential benefit, for some patients, of using mixed techniques (Serralta et al., 2010).
Swift and Greenberg (2012) remind us that a number of strategies for reducing premature discontinuation in psychotherapy have been identified, including discussing expectations regarding psychotherapy roles and behaviors, providing education regarding adequate treatment duration, addressing motivation, repairing alliance ruptures, using psychotherapist feedback, addressing client preferences, providing time-limited interventions, and increasing perspective convergence in the psychotherapy dyad.
Despite the complexity and difficulty of empirically assessing this topic, more research must be performed to understand the indication and contraindication criteria for psycho-dynamic psychotherapy used by clinicians. Only in this manner will we be able to understand the high dropout rates and non-adherence described in the literature, to increase the effectiveness of the services provided, and to establish more efficient techniques to be used in the assessment period for psychodynamic psychotherapy.
References
ACHENBACH, T.M.; RESCORLA, L.A. 2003. Manual for the ASEBA Adult Forms and Profiles. Burlington, University of Vermont, Research Center for Children, Youth, and Families, 216 p. [ Links ]
ANDREWS, G.; SINGH, M.; BOND, M. 1993. The Defense Style Questionnaire. Journal of Nervous and Mental Disease, 181(4):246-56. http://dx.doi.org/10.1097/00005053-199304000-00006 [ Links ]
BAEKELAND, F.; LUNDWALL, L. 1975. Dropping out of treatment: a critical review. Psychological Bulletin, 82(5):738-783. http://dx.doi.org/10.1037/h0077132 [ Links ]
BARRETT, M.S.; CHUA, W.; CRITS-CHRISTOPH, P.; GIBBONS, D.T.; THOMPSON, D. 2008. Early withdrawal from mental health treatment: Implications for psychotherapy practice. Psychotherapy Theory, Research, Practice, Training, 45(2):247-267. http://dx.doi.org/10.1037/0033-3204.45.2.247 [ Links ]
BARROS, A.J.; HIRAKATA, V.N. 2003. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Medical Research Methodology, 3(21). Available at: http://www.biomedcentral.com/1471-2288/3/21. Accessed on: 09/06/2015. http://dx.doi.org/10.1186/1471-2288-3-21 [ Links ]
BERK, M.; PARKER, G. 2009. The elephant on the couch: Side-effects of psychotherapy. Australian and New Zealand Journal of Psychiatry, 43(9):787-794. http://dx.doi.org/10.1080/00048670903107559 [ Links ]
BEUTLER, L.E.; HARWOOD, T.M.; ALIMOHAMED, S.; MALIK, M. 2002. Functional impairment and coping style. In: J.C. NORCROSS (ed.), Psychotherapy relationships that work. New York, Oxford University Press, p. 145-170. [ Links ]
BLAYA, C.; KIPPER, L.; HELDT, E.; ISOLAN, L.; CEITLIN, L.H.; BOND, M.; MANFRO, G. 2004. Brazilian-Portuguese version of the Defense Style Questionnaire (DSQ-40) for defense mechanisms measure: A preliminary study. Revista Brasileira de Psiquiatria, 26(4):255-258. http://dx.doi.org/10.1590/S1516-44462004000400010 [ Links ]
BLAYA, C.; DORNELLES, M.; BLAYA, R.; KIPPER, L.; HELDT, E.; ISOLAN, L.; MANFRO, G.; BOND, M. 2007. Brazilian-Portuguese version of Defensive Style Questionnaire-40 for the assessment of defense mechanisms: Construct validity study. Psychotherapy Research, 17(3):261-270. http://dx.doi.org/10.1080/10503300500485581 [ Links ]
BOND, M.; GARDNER, S.T.; CHRISTIAN, J.; SIGAL, J.J. 1983. Empirical study of self-rated defense styles. Archives of General Psychiatry, 40(3):333-338. http://dx.doi.org/10.1001/archpsyc.1983.01790030103013 [ Links ]
BRENNER, I.; VOLKAN, V. 2004. Psychoanalytic treatments of schizophrenic patients (panel reports). International Journal of Psychoanalysis, 85(5):1231-1234. http://dx.doi.org/10.1516/G8TW-8B7E-MWC9-B20X [ Links ]
CLARKIN, J.F.; YEOMANS, F.E.; KERNBERG, O.F. 2006. Psychotherapy for borderline personality: Focusing on object relations. Washington, American Psychiatric Publishing, 390 p. [ Links ]
CROWN, S. 1983. Contraindications and dangers of psychotherapy. British Journal of Psychiatry, 143(5):436-441. http://dx.doi.org/10.1192/bjp.143.5.436 [ Links ]
DE JONGE, A.L.; VAN, H.L.; PEEN, J. 2013. The role of patient characteristics in the selection of patients for psychodynamic psychotherapy. Tijdschrift voor Psychiatrie, 55(1):35-44. [ Links ]
DEROGATIS, L.R.; SAVITZ, K.L. 2000. The SCL-90-R and the Brief Symptom Inventory (BSI) in primary care. In: M.E. MARUISH (ed.), Handbook of psychological assessment in primary care settings. Mahwah, Lawrence Erlbaum Associates, p. 297-334. [ Links ]
DEWALD, P. 1964. Psychotherapy: A dynamic approach. New York, Basic Books, 256 p. [ Links ]
EDLIS-MATITYAHOU, M. 2010. Predictions of premature termination within a University Counseling Center setting: An exploratory study using the Personality Assessment Inventory (PAI). Tennessee, USA. PhD dissertation. University of Tennessee. Available at: http://trace.tennessee.edu/utk_graddiss/794. Accessed on: 12/01/2014. [ Links ]
EDLUND, M.; WANG, P.; BERGLUND, P.; KATZ, S.; LIN, E.; KESSLER, R. 2002. Dropping out of mental health treatment: Patterns and predictors among epidemiological survey respondents in the United States and Ontario. American Journal of Psychiatry, 159(5):845-851. http://dx.doi.org/10.1176/appi.ajp.159.5.845 [ Links ]
ETCHEGOYEN, R.H. 2010. Los fundamentos de la técnica psicoanalítica. Buenos Aires, Amorrortu, 976 p. [ Links ]
FLECK, M.P.A.; LOUZADA, S.; XAVIER, M.; CHACHAMOVICH, E.; VIEIRA, G.; SANTOS, L.; PINZON, V. 2000. Application of the Portuguese version of the abbreviated instrument of quality life WHOQOL-bref. Revista de Saúde Pública, 34(2):178-183. http://dx.doi.org/10.1590/S0034-89102000000200012 [ Links ]
FONAGY, P. 2010. Psychotherapy research: Do we know what works for whom? British Journal of Psychiatry, 197(2):83-85. http://dx.doi.org/10.1192/bjp.bp.110.079657 [ Links ]
GABBARD, G. 2005. Psychodynamic psychiatry in clinical practice. 4th ed., Arlington, American Psychiatric Publishing, 652 p. [ Links ]
GARFIELD, S.L. 1986. Research on client variables in psychotherapy. In: A.E. BERGIN; S.L. GARFIELD (eds.), Handbook of psychotherapy and behavior change. 3rd ed., New York, Willey, p. 190-228. [ Links ]
GARFIELD, S. 1989. Giving up on child psychotherapy: Who drops out? Comment on Weisz, Weiss and Langmeyer. Journal of Consulting and Clinical Psychology, 57(1):168-169. http://dx.doi.org/10.1037/0022-006X.57.1.168 [ Links ]
GARFIELD, S.L. 1994. Research on client variables in psychotherapy. In: A.E. BERGIN; S.L. GARFIELD (eds.), Handbook of psychotherapy and behavior change. 4th ed., New York, Willey, p. 190-228. [ Links ]
GIBBS, P.L. 2007. The primacy of psychoanalytic intervention in recovery from the psychoses and schizophrenias. The Journal of the American Academy of Psychoanalysis and Dynamic Psychiatry, 35(2):287-312. http://dx.doi.org/10.1521/jaap.2007.35.2.287 [ Links ]
HAUCK, S.; KRUEL, L.; SORDI, A.; SBARDELLOTTO, G.; CERVIERI, A.; MOSCHETTI, L.; SCHESTATSKY, S.; CEITLIN, L.H. 2007. Factors related to early dropout in psychoanalytic psychotherapy. Revista de Psiquiatria do Rio Grande do Sul, 29(3):265-273. http://dx.doi.org/10.1590/S0101-81082007000300005 [ Links ]
HOLLON, S.D.; PONNIAH, K. 2010. A review of empirically supported psychological therapies for mood disorders in adults. Depression and Anxiety, 27(10):891-932. http://dx.doi.org/10.1002/da.20741 [ Links ]
HOSMER, D.W.; LEMESHOW, S. 2000. Applied Logistic Regression. 2nd ed., John Wiley and Sons, 392 p. http://dx.doi.org/10.1002/0471722146 [ Links ]
JENKINS, S.J.; FUQUA, D.R.; BLUM, C.R. 1986. Factors related to duration of counseling in a university counseling center. Psychological Reports, 58(2):467-472. http://dx.doi.org/10.2466/pr0.1986.58.2.467 [ Links ]
JUNG, S.I.; NUNES, M.L.; EIZIRIK, C. 2007. Assessment of psychoanalytic psychotherapy outcomes. Revista de Psiquiatria do Rio Grande do Sul, 29(2):184-196. http://dx.doi.org/10.1590/S0101-810820070 00200010 [ Links ]
KEIDANN, C.E.; DAL ZOT, J.S. 2005. Avaliação. In: C.L. EIZIRIK; S.S. SCHESTATSKI; R.W. AGUIAR (eds.), Psicoterapia de orientação analítica: fundamentos teóricos e clínicos. Porto Alegre, Artmed, p. 193-205. [ Links ]
KERNBERG, O. 2004. Aggressivity, narcissism, and self-destructiveness in the psychotherapeutic relationship: New developments in the psychopathology and psychotherapy of severe personality disorders. New Haven, Yale University Press, 342 p. http://dx.doi.org/10.12987/yale/9780300101805.001.0001 [ Links ]
KRARUP, G. 2008. Psychotherapy for schizophrenia. Ugeskrift for Laeger, 170(46):3755-3758. [ Links ]
KRAUSKOPF, C.I.; BAUMGARDNER, A.; MANDRACCHIA, S. 1981. Return rate following intake revisited. Journal of Counseling Psychology, 28(6):519-521. http://dx.doi.org/10.1037/0022-0167.28.6.519 [ Links ]
LALONI, D. 2001. Escala de Avaliação de Sintomas 90-R (SCL-90-R): adaptação, precisão e validade. Campinas, SP. PhD dissertation. Pontifícia Universidade Católica de Campinas. Available at: http://www.bibliotecadigital.puc-campinas.edu.br/tde_busca/arquivo.php?codArquivo=294. Accessed on: 12/01/2014.
LEICHSENRING, F. 2005. Are psychodynamic and psychoanalytic therapies effective? A review of empirical data. International Journal of Psychoanalysis, 86(3):841-868. http://dx.doi.org/10.1516/RFEE-LKPN-B7TF-KPDU [ Links ]
LINDEN, M. 2013. How to define, find and classify side effects in psychotherapy: From unwanted events to adverse treatment reactions. Clinical Psychology and Psychotherapy, 20(4):286-96. http://dx.doi.org/10.1002/cpp.1765 [ Links ]
MALAN, D. 1976. Toward the validation of dynamic psychotherapy. New York, Plenum Medical Book Company, 298 p. http://dx.doi.org/10.1007/978-1-4615-8753-8 [ Links ]
MARGISON, F. 2005. Integrating approaches to psychotherapy in psychosis. The Australian and New Zealand Journal of Psychiatry, 39(11-12):972-981. http://dx.doi.org/10.1080/j.1440-1614.2005.01715.x [ Links ]
McNUTT, L.A.; WU, C.; XUE, X.; HAFNER, J.P. 2003. Estimating the relative risk in cohort studies and clinical trials of common outcomes. American Journal of Epidemiology, 157(10):940-943. http://dx.doi.org/10.1093/aje/kwg074 [ Links ]
MILLER, W.; ROLLNICK, S. 1991. Motivational interviewing: Preparing people to change addictive behaviors. New York, Guilford Press, 349 p. [ Links ]
MURAWIEC, S.; ZECHOWSKI, C. 2007. Schizophrenic patient's constant refusal of psychotropic medication: Case report and psychodynamic remarks. Psychiatria Polska, 41(4):551-560. [ Links ]
OLFSON, M.; MARCUS, S.; DRUSS, B.; PINCUS, H.A. 2010. National trends in the use of outpatient psychotherapy. American Journal of Psychiatry, 167(12):1456-1463. http://dx.doi.org/10.1176/appi.ajp.2010.10040570 [ Links ]
PEKARIK, G. 1983. Follow-up adjustment of outpatient dropouts. American Journal of Orthopsychiatry, 53(3):501-511. http://dx.doi.org/10.1111/j.1939-0025.1983.tb03394.x [ Links ]
PHILIPS, E.L. 1985. Psychotherapy revised: New frontiers in research and practice. Hillsdale, Erlbaum, 252 p. [ Links ]
PIPER, W.E.; OGRODNICZUK, J.S.; JOYCE, A.S.; MCCALLU, M.; ROSIE, J.S.; O'KELLY, J.G. 1999. Prediction of dropping out in time-limited interpretative individual psychotherapy. Psychotherapy: Theory, Research, Practice, Training, 36(2):114-122. http://dx.doi.org/10.1037/h0087787 [ Links ]
REIS, B.F.; BROWN, L.G. 1999. Reducing psychotherapy dropouts: Maximizing perspective convergence in the psychotherapy dyad. Psychotherapy: Theory, Research, Practice, Training, 36(2):123-136. http://dx.doi.org/10.1037/h0087822 [ Links ]
REIS, B.F.; BROWN, L.G. 2006. Preventing therapy dropout in the real world: The clinical utility of videotape preparation and client estimate of treatment duration. Professional Psychology: Research and Practice, 37(3):311-316. http://dx.doi.org/10.1037/0735-7028.37.3.311 [ Links ]
ROSENBAUM, B.; VALBAK, K.; HARDER, S.; KNUDSEN, P.; KOSTER, A.; LAJER, M.; LINDHARDT, A.; WINTHER, G.; PETERSEN, L.; JORGENSEN, P.; NORDENTOFT, M.; ANDREASEN, A.H. 2006. Treatment of patients with first-episode psychosis: Two-year outcome data from the Danish National Schizophrenia Project. World Psychiatry, 5(2):100-103. [ Links ]
RUEVE, M.E.; CORRELL, T.L. 2006. The art of psychotherapy: Selecting patients for psycho-dynamic psychotherapy. Psychiatry (Edgmont), 3(11):44-50. [ Links ]
SCHAFER, J.L. 1997. Analysis of Incomplete Multivariate Data. London, Chapman and Hall, 437 p. http://dx.doi.org/10.1201/9781439821862 [ Links ]
SCHESTATSKY, S. 1989. Introdução ao planejamento em psicoterapia. In: C. EIZIRIK; R. AGUIAR; S. SCHESTATSKY (eds.), Psicoterapia de orientação analítica: teoria e prática. Porto Alegre, Artmed, p. 71-78. [ Links ]
SERRALTA, F.; POLE, N.; NUNES, M.L.; EIZIRIK, C.; OLSEN, C. 2010. The process of change in brief psychotherapy: Effects of psychodynamic and cognitive-behavioral prototypes. Psychotherapy Research, 20(5):654-575. http://dx.doi.org/10.1080/10503307.2010.493537 [ Links ]
SPARKS, W.A.; DANIELS, J.A.; JOHNSON, E. 2003. Relationship of referral source, race, and wait time on preintake attrition. Professional Psychology: Research and Practice, 34(3):514-518. http://dx.doi.org/10.1037/0735-7028.34.5.514 [ Links ]
STIMPSON, N.; AGRAWAL, N.; LEWIS, G. 2002. Randomised controlled trials: I investigating pharmacological and psychological interventions for treatment-refractory depression: Systematic review. British Journal of Psychiatry, 181(4):284-294. http://dx.doi.org/10.1192/bjp.181.4.284 [ Links ]
SWART, H.A.; ZUCKOFF, A.; GROTE, N.K.; SPIELVOGLE, H.N.; BLEDSOE, S.E.; SHEAR, M.K. 2007. Engaging depressed patients in psychotherapy: Integrating techniques of Motivational Interviewing and ethnographic interviewing to improve treatment participation. Professional Psychology: Research and Practice, 38(4):430-439. http://dx.doi.org/10.1037/0735-7028.38.4.430 [ Links ]
SWIFT, J.K.; GREENBERG, R.P. 2012. Premature discontinuation in adult psychotherapy: A meta-analysis. Journal of Consulting and Clinical Psychology, 80(4):547-559. http://dx.doi.org/10.1037/a0028226 [ Links ]
SWIFT, J.K.; WHIPPLE, J.; SANDBERG, P. 2012. A prediction of initial appointment attendance and initial outcome expectations. Psychotherapy, 49(4):549-556. http://dx.doi.org/10.1037/a0029441 [ Links ]
TAYLOR, D.; CARLYLE, J.A.; McPHERSON, S.; ROST, F.; THOMAS, R.; FONAGY, P. 2012. Tavistock Adult Depression Study (TADS): A randomized controlled trial of psychoanalytic psychotherapy for treatment-resistant/treatment-refractory forms of depression. BMC Psychiatry, 12(1):60. http://dx.doi.org/10.1186/1471-244X-12-60 [ Links ]
TILLMAN, J.G. 2008. A view from Riggs: Treatment resistance and patient authority-IX. Integrative psychodynamic treatment of psychotic disorders. The Journal of the American Academy of Psychoanalysis and Dynamic Psychiatry, 36(4):739-761. http://dx.doi.org/10.1521/jaap.2008.36.4.739 [ Links ]
TRUANT, G.S. 1998. Assessment of suitability for psychotherapy. I. Introduction and the assessment process. American Journal of Psychotherapy, 52(4):397-411. [ Links ]
VALBAK, K.; KOSTER, A.; LARSEN, K.A.; NIELSEN, J.R.; NORRIE, B. 2003. The Danish national multicenter schizophrenia project: Assessment of psychotic patients for dynamic psychotherapy (APPP). Nordic Journal of Psychiatry, 57(5):333-338. http://dx.doi.org/10.1080/08039480310002651 [ Links ]
VALBAK, K. 2004. Suitability for psychoanalytic psychotherapy: A review. Acta Psychiatrica Scandinavica, 109(3):164-178. http://dx.doi.org/10.1046/j.1600-0447.2003.00248.x [ Links ]
WALITZER, K.S.; DERMEN, K.H.; CONNORS, G.J. 1999. Strategies for preparing clients for treatment: A review. Behavior Modification, 23(1):129-151. http://dx.doi.org/10.1177/0145445599231006 [ Links ]
WANG, P.S.; GILMAN, S.E.; GUARDINO, M.; CHRISTIANA, J.M.; MORSELLI, P.L.; MICKELSON, K.; KESSLER, C. 2000. Initiation of and adherence to treatment for mental disorders: Examination of patient advocate group members in 11 countries. Medical Care, 38(9):926-936. [ Links ]
WANG, J. 2007. Mental health treatment dropout and its correlates in a general population sample. Medical Care, 45(3):224-229. http://dx.doi.org/10.1097/01.mlr.0000244506.86885.a5 [ Links ]
WATZKE, B.; RÜDDEL, H.; JÜRGENSEN, R.; KOCH, U.; KRISTON, L.; GROTHGAR, B.; SCHULZ, H. 2010. Effectiveness of systematic treatment selection for psychodynamic and cognitive-behavioural therapy: Randomised controlled trial in routine mental healthcare. The British Journal of Psychiatry, 197(2):96-105. http://dx.doi.org/10.1192/bjp.bp.109.072835 [ Links ]
WERNER-WILSON, R.; WINTER, A. 2010. What factors influence therapy drop out? Contemporary Family Therapy, 32(4):375-382. http://dx.doi.org/10.1007/s10591-010-9131-5 [ Links ]
WESTMACOTT, R.; HUNSLEY, J. 2010. Reasons for terminating psychotherapy: A general population study. Journal of Clinical Psychology, 66(9):1-13. http://dx.doi.org/10.1002/jclp.20702 [ Links ]
WIERZBICKI, M.; PEKARIK, G. 1993. A meta-analysis of psychotherapy dropout. Professional Psychology: Research and Practice, 24(2):190-195. http://dx.doi.org/10.1037/0735-7028.24.2.190 [ Links ]
WORLD HEALTH ORGANIZATION. 1992. International classification of diseases and related health problems, 10th revision. Geneva, World Health Organization, 195 p. [ Links ]
Submetido: 12/01/2015
Aceito: 30/03/2015














