Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Revista Brasileira de Terapias Cognitivas
versão impressa ISSN 1808-5687versão On-line ISSN 1982-3746
Rev. bras.ter. cogn. vol.11 no.1 Rio de Janeiro jun. 2015
https://doi.org/10.5935/1808-5687.20150003
RELATOS DE PESQUISAS RESEARCH REPORTS
Cognitive-behavioral therapy of a case of obsessive-compulsive disorder
Terapia cognitivo-comportamental de um caso de transtorno obsessivo-compulsivo
Ana Paula JustoI; Evandro Gomes de MatosII; Marilda E. N. LippIII
IDoutorado em Psicologia - (professora de pós graduação do Instituto de Psicologia de Controle do Stress - IPCS)
IIDoutorado em Medicina - (Prof. Unicamp)
IIIPhD e pós-doutorado - (diretora do IPCS) - São Paulo - SP - Brasil
ABSTRACT
Maria, aged 35, began psychological treatment after referral by her psychiatrist, presenting severe obsessive-compulsive symptoms [OCs] which had a significantly adverse impact on her social and occupational function and on her health. Her obsessions were associated with the idea of infection and illness and her compulsions were cleanliness and hygiene. She also presented avoidance behaviors associated with these obsessions and deficit in social skills. Maria's life history and her psychological assessment enabled us to understand the development of her symptoms and to identify the predisposing, precipitating and maintaining aspects of the obsessive-compulsive disorder [OCD]. Based on the records kept during the cognitive-behavioral treatment, a reduction in the frequency of her compulsive behavior was observed. The client's self-assessment and the clinical observations also pointed towards improvement in social function and physical condition. Future efforts should include a follow-up to check for the maintenance of these gains.
Keywords: Obsessive; Behavior; Therapy
RESUMO
Maria, 35 anos, iniciou tratamento psicológico por indicação de seu médico psiquiatra e apresentava sintomas obsessivo-compulsivos [OCs] severos, com significativo prejuízo no seu funcionamento social, ocupacional e na sua saúde. Suas obsessões eram associadas à ideia de contaminação e doença, e suas compulsões eram de limpeza e higiene. Apresentava também comportamentos de esquiva associados às obsessões e reduzido repertório social. A história de vida e a avaliação psicológica de Maria permitiram compreender a evolução de seu quadro sintomatológico e a identificação dos aspectos predisponentes, precipitadores e mantenedores do transtorno obsessivo-compulsivo [TOC]. Baseado no registro realizado durante os atendimentos psicológicos, com o tratamento cognitivo-comportamental, observou-se uma redução na frequência dos comportamentos compulsivos. A auto avaliação da cliente e a observação clínica também apontaram uma melhora no funcionamento social e em sua condição física. No entanto, não foi possível realizar o follow-up para averiguar permanência dos ganhos obtidos durante o tratamento.
Palavras-chave: Comportamento; Obsessivo; Terapia
CASE CONTEXT AND METHOD
The Rationale for Selecting This Particular Client Study
There were four main reasons that determined the choice of Maria's case for this study: the OCD diagnosis, the severity of the OC symptoms, the lack of prior psychological treatment, and the cognitive-behavioral treatment carried out. This case illustrates the incapacitation caused by OC symptoms and the influence of life history on the development and permanence of the disorder. An analysis of the records kept during the psychological therapy session also allowed us to ascertain the progress made with the cognitive-behavioral treatment.
The Methodological Strategies Employed for Enhancing the Rigor of the Study Case Setting
The case progress was examined based on the frequency of compulsive behaviors recorded during the intervention process. During the first stage of intervention, records were made of the frequency with which the client would clean the house, as well as the frequency with which she washed her hands. In the second stage, a record was made of the quantity of cleaning and hygiene products purchased on a monthly basis and the bills for water consumption. The client's self-reports were also taken into account in respect of her progress and the clinical observations made by the therapist. As neither a final assessment nor a follow-up took place, it was not possible to make a comparison of the results obtained in the tests applied at the time of the initial assessment.
Case Setting
Maria first sought psychiatric help with the encouragement of her husband and mother. She went to the psychiatrist by way of referral by family members and used her health insurance plan to finance the treatment. She began drug treatment using 20 ml of Paroxetine, an antidepressant that inhibits serotonin reuptake. She was referred for psychological care by her psychiatrist and was assisted by the company where her husband worked in order to finance the expense of psychological treatment. The psychotherapy sessions were carried out in the same clinic in which the sessions with the psychiatrist were carried out.
Sources of data available concerning the client
The records made during Maria's psychological sessions were used as a source of data for the case study. These records contained the client's life history, her initial assessment, the interventions carried out and the development of her clinical picture over the course of the treatment.
Confidentiality
In order to ensure client confidentiality, her identity was altered.
THE CLIENT
Maria was 35 years old and married, and had been educated to high school level. She was born in a small town in upstate Sao Paulo, where she still lived. She had no children, did not work, and lived with her husband to whom she had been married for six years. She had an only brother, aged 23, who was single and lived with his parents. At the time when she started her psychotherapy, she presented with serious symptoms associated with OCD with a significant effect on her social and occupational function and on her health.
GUIDING CONCEPTION WITH RESEARCH AND CLINICAL EXPERIENCE SUPPORT
Introduction
According to the classification by the American Psychiatric Association [APA] (2002), OCD belongs to the group of anxiety disorders, alongside phobias (specific, social and agoraphobia), generalized anxiety, panic and post-traumatic stress. The DSM V (2013) changed this and OCD was classified as obsessive-compulsive related disorder. Its fundamental feature is the existence of recurring obsessions and/or compulsions that consume time and foment significant harm in a variety of contexts (social, professional, family, and affective) of the life of the sufferer.
The obsessions correspond to urges, thoughts, impulses or persistent images which are experienced as intrusive and inappropriate and cause accentuated anxiety and suffering (APA, 2013). They materialize in a person's mind in a repetitive and stereotypical way, even though the person may recognize them as being unnecessary and absurd (Abreu, Cangelli Filho, & Cordás, 2006). As for compulsion, this relates to repetitive behavior (e.g., washing the hands) whose objective is to prevent or reduce anxiety or suffering They are the behavioral counterpart to the obsessions and manifest themselves as an extreme need to act in accordance with a series of repetitive actions in order to avoid or prevent the threats contained in the obsessions (Abreu et al., 2006). Compulsions may present themselves in a number of ways such as the excessive washing of hands or objects, excessive checking of things (doors, windows, gas, etc.), a perfectionist attitude (the task of making each detail in a project absolutely perfect), praying, counting or repeating numbers and words in silence, amongst others (Abre et al., 2006).
OCD is considered to be quite a common illness. According to the review of literature conducted by Torres and Lima (2005), it is estimated that, amongst adults, OCD is currently prevalent in around 1% and, over the life span, between 2% and 2.5%, in the most diverse parts of the world. The review also indicated that, while epidemiological studies point to its predominant occurrence in women and to cases of pure obsession, clinical samples have evidenced a similar number of men and women and the majority of cases present with obsessions linked to compulsions which, according to the authors, suggests that the purely obsessive clients of the female sex may be turning less to the help of the health services.
OCD generally presents with a chronic clinical condition, with some fluctuations in severity. According to Cordioli (2008), there are several reasons that make OCD a serious mental disorder, including its early onset (generally at the end of adolescence and sometimes even in childhood), the level of incapacitation and the fact that it rarely exhibits complete remission of the symptoms. Individuals with OCD have many fears. They are superstitious, perfectionists, plodders and get embarrassed about carrying out rituals, all characteristics that provoke constant squabbles and social isolation (Niederauer, Braga, Souza, Meyer, & Cordioli, 2007). In addition to the devastating consequences which the disorder brings to the life of the sufferer, OCD also usually interferes with family life. The family is often obliged to accommodate itself to the symptoms, by altering their routines and having restrictions as to the use of spaces and objects. The expression "Family Accommodation" (Calvocoressi et al., 1995; Ferrão & Florão, 2010) has been given to this phenomenon.
The seriousness of the OCD is also related to the sufferer's capacity for insight into their own OC symptoms. By insight, we mean the ability that a person has to critically evaluate their own mental state, including self-awareness and the acceptance of the existence of a morbid condition and the need for treatment (Fontenelle et al., 2010). The expression "with a high level of insight" is used for those suffering with OCD who demonstrate a good critical level concerning their state, while those having "little or no insight" have a partial or total inability to recognize the irrationality of their symptoms and the need for treatment. It is clear that the greater the client's ability for insight, the better their prognosis.
Studies have shown that a large percentage of clients with OCD present themselves with psychiatric comorbidity, where major depressive disorder and anxiety disorders are the ones most commonly associated with OCD (Torres & Lima, 2005). The results obtained in the study conducted by Miguel et al. (2008), support this association. In his sample, high rates of OCD comorbidity were found with the major depressive disorder (69.7%), social phobia (36.8%), generalized anxiety disorder (35.4%), specific phobias (32.4%) and post-traumatic stress disorders (15.6%).
In a survey carried out by the World Health Organization [WHO] (1998), OCD was considered to be the fourth most common psychiatric disorder, surpassed only by depression, social phobia and substance abuse. It was also included by the WHO (1998) in the list of the ten illnesses (out of all the specialties) having the biggest impact on social incapacitation. The review of literature on the quality of life [QL] of OCD sufferers, conducted by Niederauer et al. (2007), suggested that the risk to the QL of these individuals is evident, to the point of being on a par with clients with schizophrenia, which is regarded as the most debilitating mental illness of all. According to the authors, the areas most affected by this disorder are social and family relationships, followed by occupational performance (ability to work and study), and obsessions were associated with more significant damage to the QL in comparison with compulsions (rituals). In another review of the literature on the same topic, population studies demonstrated indirect results of risk to QL in people with OCD, such as greater levels of unemployment, lower incomes and a lower rate of stable marital union, as well as relatively high rates of ideation and attempts at suicide. As for the clinical studies, these found higher risk to QL with OCD when compared to some chronic clinical illnesses, other anxiety disorders, depressive conditions, and even schizophrenia, in a number of aspects (Torresan, Smaira, Ramos-Cerqueira, & Torres, 2008).
As yet, the causes of OCD are not well known despite the existence of several theories concerning its etiology. There is strong evidence to suggest that biological factors and incidence in the family (genetics) make certain individuals susceptible to developing the disorder, as well as evidence of the involvement of the brain in OCD (Abreu et al., 2006; Cordioli, 2008; Cordioli & Braga, 2011). Factors of a psychological nature such as erroneous learning, life history, distorted beliefs and catastrophic thinking are present in the majority of sufferers, and they also seem to play a significant role in the emergence and permanence of the symptoms (Cordioli, 2008).
Several years ago, OCD was regarded as one of the least treatable illnesses. However, in the last three decades this picture has changed with the development of effective treatment methods such as exposure and response prevention therapy [ERP] and cognitive-behavioral therapy [CBT] as well as anti-obsession medication (Cordioli, 2008; Cordioli & Braga, 2011; Vivan, Bicca, & Cordioli, 2011).
According to Cordioli (2008), in practice, the clinical presentations, the onset of the illness, the cycle, the neurophysiological, neuropsychological and cognitive aspects, as well as response to treatments, vary greatly from individual to individual. While some present a rapid response over just a few sessions of therapy or with the use of medication, others are impervious to any approach. A significant percentage of clients may even achieve full remission of symptoms by employing exclusively psychological means such as ERP therapy or CBT, which, in conjunction with anti-obsessive drugs, comprise the front line of treatment for OCD. The study conducted by Braga, Manfro, Niederauer and Cordioli (2010) highlights the need to develop therapeutic strategies that aim at the full remission of OC symptoms, since, by the end of the treatment, it provides protection against relapse.
According to Cordioli (2008), CBT is effective in reducing OC symptoms in approximately 70% of clients who sign up for treatment. However, he signals as a future challenge the clarification of the reasons for which many sufferers do not respond to the treatment, as well as the development of fresh strategies to increase the effectiveness of treatment.
Behavioral model of OCD
According to this model, OC symptoms are ostensibly acquired through classical conditioning and maintained through operant conditioning (negative reinforcement). As far as Dollard and Miller were concerned (1950, apud Riggs & Foa, 1999) OC symptoms are the result of a process which takes place in two stages, namely, acquisition and maintenance. The first stage, acquisition, occurs by way of classical conditioning where a neutral stimulus (e.g., public toilet, door handle, colors, numbers, images) which is repeatedly paired with an unconditioned stimulus (fear, anxiety, revulsion), acquire the same properties of the unconditioned stimulus and thus begins to provoke the selfsame responses of fear and anxiety. In the second stage, maintenance, it would take place by way of operant conditioning, more specifically through negative reinforcement, where the individual learns that by carrying out this or that ritual (compulsion) or by avoiding contact with certain objects, situations or people (avoidance), they succeed in reducing or eliminating the discomfort (anxiety, fear), albeit temporarily (Cordioli, 2008; Cordioli & Braga, 2011; Vivan et al., 2011).
According to Cordioli and Braga (2011), the biggest drawback of the behavioral model is the lack of support for the hypothesis of a classical conditioning in the origin of the OC symptoms. However, the mechanism suggested as an explanation for the perpetuation of the symptoms (negative reinforcement - relief felt by the clients when carrying out a ritual act) is plausible and exercises a significant influence on the treatment strategy.
ERP therapy was the first effective treatment for OCD, the theory being based on the behavioral model of OCD. The main concept that underpins ERP therapy consist of the idea that compulsions are avoidance responses, and where these are effective (in the sense of managing to defer or eliminate the anticipated, aversive consequences), the only way to eliminate them would be via a reality check (Rangé, Asbahr, Moritz, & Ito, 2001). It is believed that it is through the verification of the reality, that catastrophic consequences do not ensue, that the individual ceases to emit compulsive or avoidance responses. For this test to occur, the individual needs to be exposed to the situation he/she fears (which suggests danger, risk) and at the same time be prevented (response prevention) from expressing the behavior (compulsion, ritual) that for him/her eliminates the possibility of that danger materializing (Rangé et al., 2001).
Despite the success of ERP therapy, with the passing of time it has been found that it was not effective in certain cases. According to Cordioli (2008), clients with a prevalence of obsessive symptoms, with little motivation or who presented with very rigid thoughts associated with OC symptoms, did not benefit from ERP therapy and around 20% to 30% of clients would not keep to the ERP tasks or would abandon treatment. Given these findings, greater attention began being given to thought patterns and to the cognitive model of OCD.
Cognitive model of OCD
According to this model, unpleasant, intrusive thoughts (obsessions) are experienced by the majority of people in the population at large. However, most people regard them as unpleasant and meaningless, as being mental "garbage", with no great implication or impact on their lives (Rachman & Silva, 1978, apud Vivan, et al., 2011). Some studies suggest that these "commonplace" intrusions are transformed into obsessions when evaluated as personally important, unacceptable in the extreme or immoral, and/or when they represent a threat for which the individual feels personally responsible (Abramowitz, Taylor, & McKay, 2009). According to the Obsessive-Compulsive Cognitions Working Group [OCCWG] (1997, apud Vivan et al., 2011), the main beliefs present in OCD are related to exacerbation of risk, exaggerated responsibility, intolerance to uncertainty, perfectionism and an exaggerated importance attached to thoughts and the need to control them. For Cordioli and Braga (2011), people with OCD transform the intrusive thought into an obsession because they experience this image in such a (realistic) way, to the point of believing that it might materialize at a moment of lack of control. As far as the authors are concerned, this proposition helps to understand obsessions that are aggressive, sexual and blasphemous in content, but it does not contribute to the understanding of other OCD symptoms such as infection, symmetry and hoarding.
Based on this model, cognitive techniques began being inserted into OCD treatments with the aim of correcting dysfunctional beliefs associated with the perpetuation of the OC symptoms (Cordioli & Braga, 2011). It is believed that when the modification of distorted beliefs is achieved, there will be a reduction in the fear and anxiety associated with the obsessions.
Despite the contributions of the cognitive model to an understanding of OCD, a variety of criticisms have been leveled. There is a lack of evidence in relation to the idea that dysfunctional beliefs in the OCD sufferer are any different from the beliefs present in other disorders and it is debatable whether intrusive thoughts occurring with OCD also occur in the population in general. Moreover, the model does not explain the motives for which many people carry out rituals without the existence of some cognition (obsession), present in individuals who like to organize objects symmetrically or who carry out their activities in a particular sequence or even those who present with repetitive behaviors such as the clicking of the fingers, looking from side to side or touching objects (Cordioli, 2008).
Cognitive-behavioral treatment of OCD
By bringing together the cognitive and behavioral models of OCD and their respective techniques, cognitive-behavioral treatment has become the one most frequently recommended for OCD, as well as being regarded as the model with the greatest empirical support (Abramowitz et al., 2009). The systematic review conducted by Prazeres, Souza and Fontenelle (2007) on OCD therapies with a cognitive-behavioral foundation, corroborated the effectiveness of ERP therapy and cognitive therapy in the treatment of OCD in children, teens and adults. According to the authors, the association of ERP therapy and cognitive therapy produces significant benefits in clients with a predominance of obsessive thoughts and its use in group mode also produces a significant reduction in OC symptoms.
The cognitive-behavioral treatment of OCD is based on a structured process which is brief and to the point. The aim is to reduce the OC symptoms and break down the factors which perpetuate the symptoms of compulsion and avoidance (Vivan et al., 2011). The therapeutic process can be divided into four stages: client evaluation, psychoeducation, intervention, and relapse prevention.
Psychoeducation is a determining factor in cognitive-behavioral treatment. In the case of OCD, besides providing information about CBT, it aims to inform the client about OC symptoms. This stage also aims to motivate the client in relation to the treatment and promotes greater adherence to the treatment (Cordioli, 2008; Vivan et al., 2011).
The ERP exercises and the modeling have a determining role in the cognitive-behavioral treatment of OCD. The ERP exercises are structured on the basis of identifying and listing compulsive symptoms, which enables the production of a hierarchy of activities to which the client will have to expose himself, at the same time as being prevented from carrying out any behavior which relieves him of the discomfort produced by the stimulus to which he is being exposed. These exercises can be carried out both during the session and as homework. As for the modeling, this corresponds to the performance by the therapist of ERP demonstration exercises in the presence of the client, as it is known that the simple observation of other people undertaking tasks considered as risky is one way to reduce fear (Cordioli & Braga, 2011; Vivan et al., 2011). Cognitive techniques are introduced into the OCD treatment later on, preferably when the client already has a good understanding of the OC symptoms and once the ERP exercises have been initiated (Vivan et al., 2011).
As OCD is a chronic disorder, it is prone to relapses. During the gaps between sessions and the discharge process, the client should be prepared for the possibility of relapse by training the early perception of symptoms (Vivan et al., 2011). According to Braga et al. (2010), whenever there is full remission of OC symptoms at the end of the treatment, the chances of a relapse are significantly reduced.
Summary
In brief, the literature sets out the suffering and incapacitation which the disorder imposes on the life of the sufferer and his/her family, the personal and social costs, as well as the complexity of treatment. The cognitive-behavioral model enables a better understanding of obsessive-compulsive phenomena, and CBT is considered to be the most effective treatment, both in the short and the long term, for OC symptoms. ERP therapy associated with modeling and cognitive techniques plays a central role in the therapeutic process. Full remission of OC symptoms is the objective of OCD treatment and, when achieved, suggests a lower probability of relapse.
ASSESSMENT OF THE CLIENT'S PROBLEMS, GOALS, STRENGTHS AND HISTORY
An anamnesis was carried out in the initial sessions with the aim of verifying the client's life history, family history and the evolution of the symptoms associated with her diagnosis.
Family History
In her childhood, Maria was a very reserved child, shy, fearful and always very sick. She had great difficulty in speaking and was always worried about how others perceived her. She had difficulties in school because of her shyness and felt very uncomfortable because she had no friends and felt she was always the aim of her colleagues' jibes. Her shyness got worse with her teenage years. She was embarrassed to speak to people, to go into a shop, or simply be in the presence of other people. She suffered a lot in this period and felt rejected.
Her father was authoritarian and imposed heavy control over Maria's behavior. He insisted on achievement and excessively monitored her behavior. He also was seen to be excessively concerned with illness and so did not allow his daughter to play with other children or let her invite them over to the house believing that this action would thus avoid infection and the possibility of falling sick. He kept the house exceedingly clean and made Maria clean up as well, mainly after having visitors to the house. Her mother did not have the same excessive concern with cleanliness and illness, but she was very submissive to the demands of her husband.
Maria decided against going to university because she did not want to do the course her father chose for her. She went to work in a school but did not have the ability to deal with the children and she gave it up. Afterwards, she went to work in the administration department of a company, where she remained for several years. Six years ago, shortly after marrying, Maria left her job on account of her health and has not returned to work since.
She went out with her husband for quite a long time before getting married and was subjected for years to her father's rules concerning her dating. It was only as the wedding approached that she was able to impose herself more upon her father, but as a consequence she was unable to count on his support, mainly financially. She had an idealized view of marriage and created exaggerated expectations that her life would be very different after the wedding. She felt she would be happier once free from the rules and demands of her father.
After the wedding, she had difficulty in dealing with her husband's behavior as regards cleaning, which was strict like hers. She also became frustrated with routine, wanting to get out of the house more, go for walks, chat, do everything she was unable to do before, but her husband did not match her expectations. He did, however, encourage Maria to do what she liked doing, but she needed company to be able to go out more because she was controlled by her fears.
Evolution of symptoms
Maria showed compulsive behavior in both her childhood and teenage years. In these phases, the compulsions were more about checking things and did not have a direct impact on her routine. At the beginning of adulthood, however, the compulsions started being more related to cleanliness.
In her teens, Maria demonstrated behavior and symptoms consistent with a diagnosis of social phobia, which, when she entered adulthood and started dating, were minimized. Nevertheless, it produced a significant impact on the development of her social skills. When she was about 29 years old and received a diagnosis of high blood pressure, she got panic attacks which led to her quitting her job. The anxiety attacks fueled the fears that Maria was already presenting (feeling unwell, going out alone, being in enclosed spaces) and led to her isolating herself more at home.
Around the age of 31, now married and without a job, her compulsive behavior associated with cleaning the house and washing her hands took a turn for the worse. The time devoted to cleaning and personal hygiene began to take up the entire day and the obsessions became more frequent and intense.
Presenting Problem & Descriptive Information
Maria arrived for her psychological treatment in an apathetic frame of mind, not believing in the possibility of getting better. Her main complaints were her fears, which included leaving the house, feeling unwell, becoming infected, being judged by others, etc. As she was a shy girl who had lived in an isolated way since she was little, Maria also reported having difficulty in establishing interpersonal relationships. Her complaints embodied an overall dissatisfaction with her life and a lack of future prospects.
Mental Status
In order to carry out the assessment of OC symptoms, the Yale-Brown Obsessive Compulsive Scale [Y-BOCS] was employed (Asbahr et al., 1992, apud Asbahr, 2000), and for the evaluation of Maria's levels of anxiety and depression, the Beck Inventories were used (Cunha, 2001), for Anxiety [BAI] and Depression [BDI].
The data collected enabled the severity of Maria's OC symptoms to be checked. By applying the Y-BOCS, it was possible to ascertain the presence of obsessions with content of aggression, infection, somatic, and others, while her compulsions were cleaning and washing, with the presence of trichotillomania.
Out of the nine obsessions with aggression described in the Y-BOCS, eight were checked off by the client, including: fear of hurting herself, fear of hurting others, imagining violent scenes, fear of being responsible for something terrible that might happen, etc. Of the nine obsessions with infection, again eight were checked off, including: concern about dirtiness, worry and disgust with bodily secretions, with the possibility of getting sick through infection, discomfort with viscous or waste substances, among others. The two somatic obsessions quoted in the scale were checked off, namely being worried about illness and excessive concern over certain body parts or with physical appearance. Of the 10 different obsessions, four were checked off, being: fear of saying particular things, fear of not saying exactly the right thing, fear of losing things, and superstitious fears. In all, of the 43 obsessions, 22 were checked off by the client. As far as compulsions are concerned, of the four concerning cleanliness and washing, two were checked off, namely excessive, ritualized washing of the hands and excessive cleaning of furniture in the house or inanimate objects. Despite the fact that the clientt did not check off the compulsion of ritualized or excessive personal hygiene, she demonstrated through her accounts situations that in fact correspond to the existence of this compulsion.
The evaluation of the client's daily routine corroborated the data obtained by applying the Y-BOCS. Maria spent practically the whole day cleaning her house and objects, washing clothes and taking care of her personal hygiene. Despite living in a small house, she spent 12 hours a day cleaning, even Saturdays and Sundays. When she did go out, on returning home she would wipe down her shoes, bag and cell phone, and also did the same with her husband's belongings. She would buy ready-to-eat meals so as not to dirty the kitchen and domestic utensils, and would also clean objects and utensils without having used or soiled them.
Maria also presented traces of physical injury resulting from overuse of cleaning products and excessive contact with water, such as: excessively dry hands, with cracks, deformed and dried out nails. In terms of her appearance, she was underweight and her skin and hair were damaged.
By using as a reference the US National Institute for Mental Health 15 Point Global Obsessive Compulsive Scale [NIMH Global OC Scale] (Asbahr, 2000), which evaluates the severity of obsessive-compulsive behaviors, it was possible to identify an intense degree of severity in the behaviors in the case studied. The OC symptoms at this level are incapacitating and interfere with a person's life to such an extent that daily activities become a "constant struggle". Generally, the OCD sufferer who presents this intensity of symptoms spends all of their time resisting these symptoms.
By applying the BAI and BDI, the presence of a serious level of anxiety and a moderate level of depression was identified. These data are consistent with the severity of the OC symptoms identified in the client, as these are directly associated with anxious responses. As for the presence of symptoms of depression, this is quite common in OCD, due to the emotional suffering and incapacitation produced by this disorder.
Strengths
Her penchant for reading was considered to be one of the positive points presented by Maria. The recommended reading during treatment helped with the client's understanding of her diagnosis, but she also sought out other material which might help her. Her interest in knowing more about her symptoms benefitted her involvement in the therapeutic process and her efforts in respect of the activities required of her.
Maria also demonstrated a determination to get involved in new activities. Despite her interests being connected with a childhood and adolescence totally devoid of leisure, her motivation was considered positive to the treatment. From the moment that her apathy improved and her confidence in the treatment grew, her interests began to come to the fore. She demonstrated great desire to get out of the house, meet new people, go on trips, travel and go back to studying. This motivation fueled the client's involvement in the therapeutic process and her interests became goals to be achieved.
FORMULATION AND TREATMENT PLAN
Formulation
Maria's life history was considered important to the understanding of the development of the OCD. The father's pattern of behavior is connected with the development of various symptoms presented by the client. The father's excessive concern with the possibility of infection had a direct influence on the learning of exaggerated behavior in respect of cleanliness and hygiene. Very often during the therapy the client would reiterate that she believed that the level of hygiene and cleanliness in her house was what should be strived for by everyone, with any degree of cleanliness below that demonstrated by her being regarded as negligence or a lack of hygiene.
Her father also worried excessively about illness, which caused him to exercise excessive control over Maria's behavior, so that she would not fall ill or bring some illness back home with her. Maria was unable to go out or enjoy the company of other children. She was isolated, involved in cleaning the house for the most part of her time. This isolation had a negative effect on the development of her social repertoire which resulted in shyness and a difficulty in establishing relationships during her teenage years.
Her father was demanding and however much his daughter tried, it was never enough. To be able to exert more control over his daughter, he would emphasize her physical vulnerability, stating that she was very weak (sick) and therefore she would not be able to carry out certain activities or she would need to protect herself more than other people in order not to get sick. These criticisms were internalized by Maria and resulted in self-depreciation. Some of the phrases noted over the course of the sessions illustrated this negative self-assessment, such as, "I am very fragile", "I get sick easily!" and "I am not capable!" These thoughts are also linked to the numerous fears presented by Maria, such as fear of feeling unwell, of going out of the house alone and fear of falling sick.
Within this family context, Maria grew up isolated and with many desires she was unable to realize. The phrase "I wasted my childhood and my youth!" illustrates the client's feelings in regard to these phases of her life. When she started dating, and then after marrying, she felt she would be free of her father's control. This fresh perspective motivated Maria and led her to envision a different future.
Shortly after getting married, the client received a diagnosis of high blood pressure which really frightened her and it heightened her fears of illness. As she could not control her blood pressure, she began to cut back on her daily activities, mainly those she believed generated stress. Given these circumstances, the client gave up her job and began to spend most of her time at home, alone. In this same period, also affected by the diagnosis of hypertension, she began to experience panic attacks. She became afraid of feeling unwell and would avoid doing anything which seemed to trigger symptoms similar to those of the attacks.
Over the last six years, the client has come to be more and more dependent on her husband and would expect of him certain attitudes which would bring her some satisfaction. Her husband, however, did not have the same desires, preferring to stay at home and he rarely suggested going out anywhere. Financial difficulties also limited their potential for leisure activity. This situation was a source of great frustration to Maria who once again saw herself as a prisoner in her own home. In the last six years, her compulsive behaviors have increased, negatively affecting her entire day. At the time when Maria began her treatment, even when there was a possibility of indulging in some leisure activity, she did not do so because she could not desist from cleaning the house and would feel too insecure to go out.
Treatment Goals and Plan
Based on the cognitive-behavioral evaluation and formulation of the case, the therapeutic objectives were defined as follows: reduce the frequency of compulsive behavior in cleaning and hygiene, reduce obsessive thoughts associated with infection and illness, reduce the fear of going out of the house alone and feeling unwell, break down the belief in her vulnerability, incapacity and lack of esteem and further the development of social skills.
The initial aim was to reduce the OC symptoms. By obsession, we mean persistent urges, thoughts or images that are intrusive or inappropriate and which cause intense anxiety and suffering, while compulsions are repetitive behaviors, the aim of which is to reduce or prevent anxiety or suffering (APA, 2002). In Maria's case, the obsessions were thoughts connected with the risk of infection and falling sick, while her compulsions involved repetitive behaviors of cleaning the house and objects as well as hygiene. The client's excessive behavior in cleaning and hygiene afforded her relief from the anxiety and discomfort generated by the obsessions of infection or illness, which might at other moments be carried out to avoid anxiety and suffering. The initial goal was to reduce the frequency of compulsive behaviors in order to subsequently promote the disintegration of her obsessive urges.
As for her fear of going out alone and feeling unwell, this was understood to be the emotional consequence of her obsession with infection and illness. Outside the house, the client was more exposed to infection and illness and thus avoided going out and when she did venture out, she would seek the company of somebody she could trust because she believed she might feel unwell. The behaviors of putting off leaving the house and going out alone were understood to be avoidance responses as they sidestep the anxiety and suffering occasioned by the obsessions.
Literature points to the ERP technique as being the most effective in the treatment of OCD. It is based on the behavioral model of OCD that consists of the idea that compulsions are avoidance responses that can only be performed by means of the reality check (Rangé et al., 2001). With the confirmation of the reality, that the catastrophic consequences do not ensue, the individual ceases to transmit compulsive or avoidance responses. For this test to take place, the individual needs to be exposed to the situation that is feared (which suggests danger, risk) and at the same time be prevented (response prevention) from transmitting the behavior (compulsion, ritual) which for her eliminates the possibility of that danger materializing (Rangé et al., 2001). By using this technique, it is sought to reduce compulsive symptoms and avoidance responses and consequently the fears presented by Maria.
The disintegration of the beliefs, i.e., the client's rigid, inflexible thoughts connected with the idea of physical vulnerability, incapacity and lack of esteem, were also regarded as goals of therapy. In the evaluation of the client's thought patterns, a tendency was noted towards the catastrophizing of risk and danger as well as a lack of appreciation of her resources to deal with them. According to the cognitive model, an individual with psychological suffering has his capacity for self-perception, the environment and the future negatively impacted by distorted thinking which ends up determining tendencies in the way facts are interpreted (Lipp, 2000; Pereira & Rangé, 2011). In states of anxiety, risks are overestimated, both external and internal, linked to a lack of appreciation of one's own resources to deal with them.
The result obtained arising from the presence of the client's exposure to the situations she fears, helped with the cognitive restructuring of her beliefs about vulnerability, incapacity and lack of esteem. The confirmation that stopping cleaning the house did not make you sick created proof that she was not so vulnerable to infection, in the same way that the confirmation that she managed to go out alone without becoming unwell and without getting lost created proof of her capacity and promoted self-appreciation. The quest for proof that would break down the client's beliefs was performed throughout the entire period of treatment.
Based on the clinical observation, which indicated a deficit in the client's social repertoire, and on her own account of her difficulties in establishing interpersonal relationships, the development of these skills was also considered to be a goal of therapy. The process of exposure also assisted with the development of social skills, as it promoted situations of social interaction that facilitated the training. With the objective of the client achieving greater socialization, it was sought to train the following aspects: maintaining eye contact, starting a conversation and expressing personal opinions. Based on the client's interests (e.g., going into a store, making a telephone call, asking questions to a stranger), it was sought to simulate these situations in the session with the aim of training these skills.
The ERP technique and the cognitive restructuring represented the basis for the treatment plan offered to the client. However, other interventions were associated, such as: psychoeducation, modeling, shaping, social skills training, and problem resolution training, with the aim of achieving better results and fulfilling the needs that materialized during treatment.
Summary of formulation of case and description of treatment
Chart 1 shows a summary of the cognitive-behavioral formulation of the case, the objectives of therapy and the interventions carried out during treatment.
COURSE OF THERAPY
Over a period of 15 months, 35 individual sessions of fifty minutes each were conducted based on the cognitive-behavioral model. The procedure included the psychological contract, assessment, and intervention. Due to the therapy being abandoned because of financial difficulties, it was not possible to carry out a final assessment and follow-up.
The proposal was to have weekly sessions, but because of the client's financial difficulties, the sessions were often conducted at intervals longer than a week. After eight months of treatment (27 sessions completed), the client broke off therapy for three months. During this time, she did maintain her medication treatment. Upon her return, she had a further eight sessions over a period of three months, maintaining regular gaps between sessions. In spite of the longer gaps between sessions, the client always advised of any absence in advance, demonstrating her interest in the process of therapy.
In order to better understand the process of therapy, it will be presented in two stages. The first describes the first 27 sessions, while the second describes the eight sessions conducted after the client's three month break.
First Stage
The objectives of the first two sessions held with the client were as follows: the execution of the therapeutic contract, gathering information on the various complaints, psychoeducation about the treatment model being offered (CBT), and the building of a therapeutic bond. In the first session, Maria showed herself to be quite apathetic and disbelieving of the treatment, saying she was only there because of her mother and her husband. She spoke very little during the session and the therapist sought to motivate her in relation to the treatment. In the second session, Maria participated more and managed to better describe her complaints. At the end of this session, the psychological contract was restated and it was possible to see an improvement in the client's level of involvement in relation to the process of therapy.
The psychological evaluation was conducted between the third and sixth sessions. This process started with the collection of data on her life history, followed by a description of her routine and the application of the instruments of evaluation. Maria described her life history in detail and at the same time, as she was saddened by certain episodes, she was motivated by the possibility of a better understanding of the facts in her history that might be associated with her complaints. At the closing of the assessment process, the results feedback was conducted, and, based on these data, the objectives of the therapy were defined.
Up until this point in time, Maria had put her psychological symptoms down to her state of depression. With the feedback, however, it was possible to inform the clientt about her level of anxiety and about OCD. This new information was well received, which gave her a better understanding of her OC symptoms.
Between the seventh and final session of the first stage, psychological interventions were carried out. Even prior to the carrying out of the OC symptom related interventions, the client was already recounting her initiatives to reduce the frequency of house cleaning and hand washing. These initial sessions triggered a good level of insight in the client in respect to her condition, considered to be an indicator of better response to treatment (Raffin, Guimarães, Fachel, Pasquoto de Souza, & Cordioli, 2009).
As Maria demonstrated an intense level of OC symptoms connected with a severe level of anxiety, before commencing the ERP exercises, the introduction of anxiety management strategies was deemed as priority. To this end, psychoeducation was provided about anxiety, followed by training on breathing and muscle relaxation. The breathing training was used as a preliminary step in the muscle relaxation training, but was also recommended as a practice in itself.
Still with the aim of managing anxiety, the ACALME-SE[1] strategy created by Rangé (2001) was applied. This technique aims to promote the acceptance of the symptoms of anxiety. As Maria would get frightened by the initial physical reactions triggered by the anxiety and would associate them with the idea of a serious illness, her level of anxiety would rise even more and her symptoms would be exacerbated. Using this strategy, it was sought to instruct the client to identify and accept the initial symptoms of anxiety, thereby avoiding a worsening of the reaction. The use of anxiety management techniques was encouraged during the whole period of treatment.
Equipped with a better understanding of the anxiety and how to manage it, the focus of the sessions moved to the OC symptoms. The psychoeducation on the OCD, already begun after the assessment feedback, became more intense at this point. Understanding what obsessions and compulsions are is fundamental to the cognitive-behavioral treatment of the OCD (Cordioli & Braga, 2011), and it is also important to understand the possible causes of the development of the disorder and its maintaining aspects. Maria became involved with this process and did a lot of reading on the subject. This knowledge motivated the client to seek change in her pattern of behavior and also made it possible for her to realize a self-assessment.
Around about the eighth session, still during the process of psychoeducation on anxiety, Maria was asked to record the frequency of her cleaning and hygiene behaviors. Based on the description of her daily routine, some of the cleaning behaviors that the client would carry out on a daily basis were selected, such as cleaning all the cupboards, washing the tiles, the floor of the house, the yard, the bathroom and washing clothes by hand, and she was asked to note the frequency with which she performed these tasks during the week. She was also requested to record the frequency with which she would wash her hands during the day.
Based on the initial records presented, the process of exposure and response prevention was planned. In each session, one compulsive behavior was selected and the client was asked to reduce, during the following week, the frequency with which she carried it out. The process of exposure would occur when the client would remain at home but would not clean a particular object or room as she would normally do, despite the obsessive thoughts constantly alerting her to the risk of infection and illness. In order to perform response prevention, the client was instructed not to perform any ritual or act or any other maneuver which might relieve the discomfort, however great the discomfort produced by the obsessions. In these moments of anxiety, the client was asked to try to use anxiety control techniques (breathing and ACALME-SE). The client was also informed that, for each exposure exercise carried out, the anxiety triggered by the exposure situation would be lower. The ERP exercises were started in the tenth session and exposure was being carried out on a gradual basis.
At around session number 20, when the ERP exercises were already showing results, it was sought to introduce cognitive techniques into the therapeutic process. At this moment, as a consequence of the exposure process, obsessive thoughts were materializing and becoming the focus of the intervention. Questions such as "But aren't I more relaxed about cleaning my house?";"Are you sure this is right?"; "Aren't I doing myself some harm!" and "Do you think I will really be able to do this!" became frequent during the session and enabled the process of cognitive restructuring. It was sought to create a more suitable reference with regard to cleaning the house and to hygiene, based on evidence obtained from the exposure process.
At this time, thoughts associated with the client's avoidance responses were also worked on. Maria avoided going out because she was afraid of infection and/or because she felt incapable of doing so. Ideas of vulnerability, incapacity and lack of esteem prevented the client from becoming exposed to new situations, primarily greater social contact.
As the time spent on cleaning the house began to lessen, the client had more incentive to get out of the house alone (which was also regarded as an exposure exercise) and seek out medical assistance for the symptoms she was presenting. Maria was unhappy with her appearance and a part of what bothered her was related to the harm done by the excessive use of cleaning products. The first doctor she saw was a dermatologist, to care for her skin and her nails.
Given the increase in situations of social contact, it was possible to initiate the training of her social skills. Even the appointment with the dermatologist was simulated in one of the sessions as Maria was embarrassed to show her hands to the doctor and she also felt insecure about describing her symptoms. She was constantly worried about what other people thought of her, which inhibited her in various situations.
At the end of this first stage of intervention, the client was showing interest in taking a course (computer studies or English); however, her financial difficulties prevented this. She thought about asking her father for financial help but was afraid of what his reaction might be. The negotiation process with her father became a goal to be achieved and was the theme of several sessions.
Second Stage
After a break of three months, Maria resumed therapy. In the first two sessions, the therapeutic contract and goals were revisited and a fresh assessment of her OC symptoms was performed. The client had experienced a relapse in relation to the OC symptoms in comparison with the last records made, though not with the same severity as when she first began therapy. Despite the relapse, her nails had recovered and she wore her hair down, which she had never done before.
At this time, the client was quite frustrated that she had not been able to embark upon any course, but she did report that she was visiting her mother's house more frequently, where she would use her brother's computer. She also talked of her desire to buy a computer for her own house.
After this initial assessment, the client was asked to record the quantity of cleaning and hygiene products used on a monthly basis and the details of the water bills. The aim was to reduce expenses on these types of product and also of water consumption, which would in turn reduce compulsive cleaning and hygiene behavior. It was proposed to Maria that, with the savings made on these expenses, she could invest in the purchase of a computer.
Given this new proposal, a new type of ERP exercise arose. Maria needed to cut down on the quantity of cleaning products, which would expose her to a situation that produces anxiety because it triggers the idea of infection. A target was established in each session so that gradually the client would reduce the quantity of products that she uses to clean the house and for personal hygiene.
Happy with the savings that she was managing to make, Maria's husband agreed to buy a computer. In the last session she attended, the client was happy about the arrival of the new computer in her home.
THERAPY MONITORING AND USE OF FEEDBACK INFORMATION
In the first stage of treatment, therapy progress was monitored by means of the recording of the frequency of compulsive behaviors carried out by the client. As far as the house cleaning activities were concerned, the initial records showed that the client was performing an extensive cleaning of her house every day that was equivalent to a spring-clean, and some of these cleaning behaviors were performed more than once a day. The initial objective was to eliminate these activities on Saturdays and Sundays, thereby reducing them from seven times a week to five. Subsequently, it was sought to reduce the activity from five to three times a week, with the end target being the performance of a detailed cleaning of the house just twice per week.
In the last record made before her break from therapy, the cleaning of the cupboards and tiles was being performed just twice a week. The cleaning of the floor, bathroom and yard was carried out three times a week. The stove, which was being cleaned more than once a day, was now being cleaned only twice a week and the clothes that were hand washed every day went to being washed three times a week; the washing machine, which had never previously been used, was now being used at least three times a week. These results suggested a reduction in compulsive behaviors linked to the cleaning of the house.
As for the frequency with which she would wash her hands, the initial records showed that the client was washing her hands 46 times a day, on average. In the last record noted during the first stage, Maria was washing her hands an average of 20 times a day. In her accounts, the client mentioned that on the days when she would go out of the house, she would end up washing her hands fewer times, equivalent to 10 times a day. However, on those days that she remained at home, this control was more difficult, the average being 24 times a day.
The clinical observation and the client accounts were also considered in the process of the evaluation of the therapy. The client's physical appearance improved over the course of the sessions; she put on weight and began to look after her hands and nails, even arriving at her therapy with long, varnished nails.
According to the client's own accounts, she never again used pure chlorine to wash her hands and feet. Around session number 23, she also mentioned finishing her domestic duties earlier in the day, at around 2 p.m. (previously she was finishing at 6 p.m.), and that, after this, she would devote her time to reading and listening to music.
In the second stage of the therapeutic process, the progress of the therapy was monitored based on the records of the quantity of cleaning and hygiene products spent each month. It can be seen from Table 2 that there was a drop in the quantity of products used in the three-month period during which the records were kept.
The best results observed related to the reduction in the consumption of detergents, soap powder and bars of soap. Maria had reached a point where she was using more than three units of detergent per day, but by the last month she had managed to reduce this figure to almost one unit a day. Another important result was in regard to the use of chlorine. The client stopped using pure chlorine and started using only bleach. However, the results did indicate a greater difficulty in terms of reducing detergent and shampoo consumption.
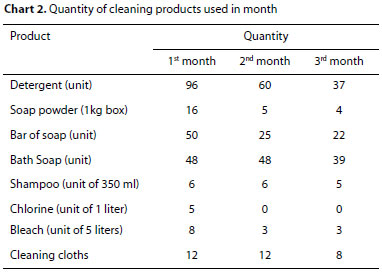
As far as the monthly water bills were concerned, the results demonstrated a good level of saving. The first record showed a water bill of R$ 410 (approx. US$ 200), while the last record, two months later, showed a value of R$ 186 (approx. US$ 90).
Clinically, it was also possible to see an improvement. In addition to the maintenance of gains in terms of health and physical appearance, the client was going out more and sometimes even came by herself to the therapy. Her husband praised the changes in her, which also became evident to other people, according to the client's own accounts.
CONCLUDING EVALUATION OF THE THERAPY'S PROCESS AND OUTCOME
Considering the severity of Maria's clinical picture at the start of treatment, it was possible to observe a significant improvement in her psychological state as a whole after the interventions performed. Overall, the therapeutic objectives were attained.
The primary objective of the therapeutic process was to diminish compulsive behaviors. Based on the results obtained with the records of frequency of compulsive behaviors, it was found that there had been a reduction in this type of behavior, in both stages of the process. These results were the consequence of the psychoeducation on OCD and, primarily, the ERP exercises.
The second therapeutic objective was the reduction in obsessive thoughts. With the reduction in compulsive behaviors, it is thought that a reduction in the obsessions presented by the client also took place; however, there are no objective data that corroborate this outcome. According to the behavioral model of OCD, at the point where an individual exposes himself/herself to the situation that is feared, a reality test is performed which allows them to check if the urges (obsessions) really correspond to reality. Based on the confirmation that one's thoughts are not indeed turning to reality, the obsessions began to weaken. The ERP exercises are thus credited with promoting the reduction in obsessive thoughts.
Despite the reduction in OC symptoms, full remission of the symptoms did not occur by the time the process was suspended, which represents a greater risk of a future relapse.
The third objective was to reduce the fear of going out alone or feeling unwell while out. These fears were the emotional consequences of the obsessive thoughts about cleanliness and hygiene, which would trigger behavioral responses of avoiding the situation of going out alone. Based on the client's own accounts, over the course of the therapeutic process, she began to go out more by herself, which suggested a reduction in these fears. The achievement of this outcome can also be attributed to the ERP exercises. The exposures performed may have promoted the weakening of the obsessions which, in turn, reduced the fear of going out.
The fourth therapeutic objective was the breaking down of beliefs connected with the notion of vulnerability, incapacity and lack of esteem. These beliefs fueled the client's obsessive urges and the process used for their disintegration was that of cognitive restructuring. However, the ERP exercises provided evidence that assisted with the process of cognitive restructuring. Maria's initiatives to carry out new activities suggest a level of change in her thought patterns.
As for the final objective, this corresponded to the development of the client's social skills. Out of all the goals, this was the one that received the shortest period of intervention. Through the training of social skills and modeling, it was sought to raise her social repertoire. Based on clinical observation, Maria improved her eye contact and increased the frequency with which she would ask questions and express opinions.
Due to the suspension of the therapeutic process, the objectives were only partially achieved. It was not possible therefore to perform a final assessment and follow-up.
CONCLUSION
The case illustrates a process of intervention with a cognitive-behavioral basis for the treatment of OCD, within a clinical context. The case description and formulation permitted the identification of aspects which had an impact both on the development and the maintenance of OCD. It was also possible to track the evolution of treatment and analyze the results obtained.
In the case study, the cognitive-behavioral treatment showed itself to be effective with regard to the reduction in OC symptoms. The association of ERP therapy with cognitive restructuring was seen to be effective; however, it was the reality tests promoted by the exposure process that exerted a core role in the process of restructuring the cognitions of vulnerability, incapacity and lack of esteem.
The absence of follow-up made it impossible to analyze the maintenance of the results obtained during the intervention process.
REFERENCES
Abramowitz, J. S., Taylor, S., & McKay, D. (2009). Obsessive-compulsive disorder. Lancet, 374,491-499. DOI: http://dx.doi.org/10.1016/S0140-6736(09)60240-3 [ Links ]
Abreu, C. N., Cangelli Filho, R., & Cordás, T. A. (2006). Transtorno obsessivo-compulsivo. In C. N. de Abreu, F. T. Salzano, F. Vasques, T. A. Cordás, Síndromes psiquiátricas: Diagnóstico e entrevista para profissionais de saúde mental (pp. 65-72). Porto Alegre: Artmed. [ Links ]
American Psychiatric Association (APA). (2014). Manual diagnóstico e estatístico de transtornos mentais: DSM-V-(5ª.ed.) Porto Alegre: Artmed. [ Links ]
Asbahr, F. R. (2000). Escalas de avaliação de transtorno obsessivo-compulsivo na infância e adolescência. In C. Gorenstein, L. H. S. G. Andrade, & A.W. Zuardi (Eds.), Escalas de avaliação clínica em psiquiatria e psicofarmacologia (pp. 167-180). São Paulo: Lemos Editorial. [ Links ]
Braga, D. T., Manfro, G. G., Niederauer, K., & Cordioli, A. V. (2010). Remissão completa e recaídas dos sintomas obsessivo compulsivos depois da terapia cognitivo-comportamental em grupo: Dois anos de acompanhamento. Revista Brasileira de Psiquiatria, 32(2)164-8. DOI: http://dx.doi.org/10.1590/S1516-44462010000200012 [ Links ]
Calvocoressi, L., Lewis, B., Harris, M., Trufan, S. J., Goodman, W. K., McDougle, C. J., & Price, L. (1995). Family accommodation in obsessive-compulsive disorder. The American Journal of Psychiatry, 152(3),441-443. DOI: http://dx.doi.org/10.1176/ajp.152.3.441 [ Links ]
Cordioli, A. V. (2008). A terapia cognitivo-comportamental no transtorno obsessivo-compulsivo. Revista Brasileira de Psiquiatria, 30(Supl. 2),65-72. DOI: http://dx.doi.org/10.1590/S1516-44462008000600003 [ Links ]
Cordioli, A. V., & Braga, D. T. (2011). Terapia cognitivo-comportamental do transtorno obsessivo-compulsivo. In B. Rangé, Psicoterapias cognitivo-comportamentais: Um diálogo com a psiquiatria (2. ed., pp. 325-343). Porto Alegre: Artmed. [ Links ]
Cunha, J. (2001). Manual em português das Escalas Beck. São Paulo: Casa do Psicólogo. [ Links ]
Ferrão, Y. A., & Florão, M. S. (2010). Acomodação familiar e criticismo percebido em pacientes com transtorno obsessivo-compulsivo. Jornal Brasileiro de Psiquiatria, 59 (1),34-43. DOI: http://dx.doi.org/10.1590/S0047-20852010000100006 [ Links ]
Fontenelle, J. M., Santana, L. S., Lessa, L. R., Victoria, M. S. V., Mendlowicz, M. V., & Fontenelle, L. F. (2010). O conceito do insight em pacientes com transtorno obsessivo-compulsivo. Revista Brasileira de Psiquiatria, 32(1),77-82. DOI: http://dx.doi.org/10.1590/S1516-44462010000100015 [ Links ]
Lipp, M. E. N. (2000). O stress está dentro de você. São Paulo: Contexto. [ Links ]
Miguel, E., Ferrão, Y., Rosário, M., Mathis, M., Torres, A., Fontenelle, L.... Silva, E. D. (2008). The Brazilian Research Consortium on Obsessive-Compulsive Spectrum Disorders: recruitment, assessment instruments, methods for the development of multicenter collaborative studies and preliminary results. Revista Brasileira de Psiquiatria, 30(3),185-196. DOI: http://dx.doi.org/10.1590/S1516-44462008000300003 [ Links ]
Niederauer, K. G., Braga, D. T., Souza, F. P., Meyer, E., & Cordioli, A.V. (2007). Qualidade de vida em indivíduos com transtorno obsessivo-compulsivo: Revisão da literatura. Revista Brasileira de Psiquiatria, 29(3),271-278. DOI: http://dx.doi.org/10.1590/S1516-44462006005000050 [ Links ]
Pereira, M., & Rangé, B. (2011). Terapia cognitiva. In B. Rangé, Psicoterapias cognitivo-comportamentais: Um diálogo com a psiquiatria (2. ed., pp. 20-32). Porto Alegre: Artmed. [ Links ]
Prazeres, A. M., Souza, W. F., & Fontenelle, L. F. (2007). Terapias de base cognitivo-comportamental do transtorno obsessivo-compulsivo: Revisão sistemática da última década. Revista Brasileira de Psiquiatria, 29(3),262-270. DOI: http://dx.doi.org/10.1590/S1516-44462006005000046 [ Links ]
Raffin, A. L, Guimarães Fachel, J. M., Pasquoto de Souza, F., & Cordioli, A. V. (2009). Predictors of response to group cognitive-behavioral therapy in the treatment of obsessive-compulsive disorder. European Psychiatry, 24(5),297-306. DOI: http://dx.doi.org/10.1016/j.eurpsy.2008.12.001 [ Links ]
Rangé, B. (2001). Transtorno do pânico e agorafobia. In B. Rangé (Ed.), Psicoterapia comportamental e cognitiva de transtornos psiquiátricos (pp. 67-104). Campinas: Livro Pleno. [ Links ]
Rangé, B., Asbahr, F., Moritz, K., & Ito, L. (2001). Transtorno obsessivo-compulsivo. In B. Rangé, Psicoterapias cognitivo-comportamentais: Um diálogo com a psiquiatria (pp. 230-246). Porto Alegre: Artmed. [ Links ]
Riggs, D. S., & Foa, E. B. (1999). Transtorno obsessivo-compulsivo. In D. H. Barlow, Manual clínico dos transtornos psicológicos (2. ed., pp. 217-272). Porto Alegre: Artmed. [ Links ]
Torres, A. R., & Lima, M. C. P. (2005). Epidemiologia do transtorno obsessivo-compulsivo: Uma revisão. Revista Brasileira de Psiquiatria, 27(3),237-242. DOI: http://dx.doi.org/10.1590/S1516-44462005000300015 [ Links ]
Torresan, R. C., Smaira, S. I., Ramos-Cerqueira, A. T. A., & Torres, A. R. (2008). Qualidade de vida no transtorno obsessivo-compulsivo: Uma revisão. Revista de Psiquiatria Clínica, 35(1),13-19. DOI: http://dx.doi.org/10.1590/S0101-60832008000100003 [ Links ]
Vivan, A. S., Bicca, M. G., & Cordioli, A. V. (2011). Modelo cognitivo-comportamental do transtorno obsessivo-compulsivo. In I. Andretta, & M. S. Oliveira (Eds.), Manual prático de terapia cognitivo-comportamental (pp. 373-388). São Paulo: Casa do Psicólogo. [ Links ]
World Health Organization (WHO). (1993). Classificação de transtornos mentais e de comportamento da CID 10. Porto Alegre: Artmed. [ Links ]
World Health Organization (WHO). (1998). Classificação de transtornos mentais e de comportamento da CID 10.Porto Alegre: Artmed. [ Links ]
 Correspondência:
Correspondência:
Marilda Novaes Lipp
Rua Camargo Paes, 538, Guanabara
Campinas - SP. CEP 13073-350
E-mail: mlipp@estresse.com.br
Este artigo foi submetido no SGP (Sistema de Gestão de Publicações) da RBTC em 14 de junho de 2016. cod. 434.
Artigo aceito em 17 de junho de 2016.
Instituto de Psicologia e Controle do Stress.
[1] An acronym in Portuguese equating to an eight-step strategy to control acute anxiety, adapted from the AWARE technique espoused by Beck, Emery & Greenberg onte aqui o seu manuscrito














