Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Psicologia em Pesquisa
versão On-line ISSN 1982-1247
Psicol. pesq. vol.9 no.2 Juiz de Fora dez. 2015
https://doi.org/10.5327/Z1982-1247201500020007
ARTICLES
Social distance toward people with substance dependence: a survey among health professionals
La distancia social de las personas con dependencia de sustancias: una encuesta entre los profesionales de la salud
Pollyanna Santos da SilveiraI,III; Rhaisa Gontijo SoaresII; Henrique Pinto GomideIII; Gabriela Correia Lubambo FerreiraIII; Ana Luísa Marlière CaselaIII; Leonardo Fernandes MartinsIII; Telmo Mota RonzaniIII
IUniversidade Católica de Petrópolis, Petrópolis , Brasil
IIFaculdade Pitágoras, Divinópolis, Brasil
IIIUniversidade Federal de Juiz de Fora, Juiz de Fora, Brasil
ABSTRACT
The aim of this study was to investigate factors associated with social distance toward people with substance dependence among health professionals. A hundred and eighty-three health professionals from Juiz de Fora, Minas Gerais, Brasil, were interviewed using structured questionnaires with vignettes. The vignettes assessed emotional reactions generated by alcohol, marijuana, and cocaine dependents. Belief in recovery and perception of dangerousness were significantly associated with social distance toward people with cocaine and marijuana dependence. Only belief in recovery was significant with alcohol dependence. This study provides preliminary data on factors related to the desire for social distance among health professionals, improving the understanding of stigmatization, and the development of research and training in the area.
Keywords: social distance; health professionals; stigma; drug dependency; Brazil.
RESUMEN
Este estudio tuvo como objetivo investigar los factores asociados con la distancia social hacia las personas con dependencia de sustancias entre los profesionales de la salud . Ciento ochenta y tres profesionales de la salud de Juiz de Fora, Minas Gerais - Brasil fueron entrevistados mediante un cuestionario estructurado con viñetas . Las viñetas evaluaron las reacciones emocionales generados por el alcohol, marihuana y cocaína dependientes . La creencia en la recuperación y la percepción de peligrosidad fueron significativos asociados con la distancia social hacia las personas con dependencia de la cocaína y la marihuana . Sólo la fe en la recuperación fue significativa con la dependencia del alcohol . Este estudio muestra los datos preliminares sobre los factores relacionados con el deseo de distancia social entre los profesionales de la salud , la mejora de la comprensión de la estigmatización y el desarrollo de la investigación y la formación en el área .
Palabras clave: distancia social; profesionales de la salud; estígma; dependencia a drogas; Brasil.
Introduction
The perception of the population about a disease inflences the willingness to seek help, commitment to treatment, and the reintegration into the community (Peluso & Blay, 2004). Even when health resources and facilities are made available, many people may avoid them, or quit treatment prematurely in an attempt to avoid stigmatization (Corrigan, 2004; Rüsch, Angermeyer & Corrigan, 2005).
Studies showed that the negative perception of a health condition could be a predictor of stigma. Stigma affcts several life domains including housing, employment, interpersonal relationships, and recovery, which leads to social isolation and an increased desire for social distance (Angermeyer & Matschinger, 1997; Dietrich et al., 2004; Lauber, Nordt, Falcato & Rössler, 2004; Link, Struening, Neese-Todd, Asmussen & Phelan, 2001). Social distance is defined as the lack of willingness of one person to engage in relationships of diffrent degrees of intimacy with someone who has a spoiled identity. It may be the most stigmatizing factor for those affected with a mental health condition (Link, Cullen, Frank & Wozniak, 1987).
The desire for social distance is often caused by threatening feelings, which are induced by distorted perceptions and differences between groups. Thse distorted perceptions and differences are based on physical characteristics (e.g. scars, disabilities, or anorexia nervosa), personal traits (e.g. criminal background, mental illness, drug dependence), or personal beliefs (e.g. perception of unpredictability, lack of control over the disease) (Blascovich, Mendes, Hunter & Lickel, 2003).
Link, Phelan, Bresnahan, Stueve and Pescosolido (1999) conducted a study on public conceptions of patients with mental illness. Thy found that people had greater desire for social distance from a cocaine user than an alcohol dependent or a person with schizophrenia. Thediffrence in desire for social distance may be due to an association with the belief that a person with a certain characteristic can be violent (Link et al., 1999). Other studies showed that substance users are seen as more responsible for their condition, more violent, and more unpredictable than others affected by diffrent mental illness (Angermeyer & Matschinger, 1997; Link & Phelan, 2013; Pescosolido, Monahan, Link, Stueve & Kikuzawa, 1999).
Alcohol and other drugs dependence is one of the major public health problems in Brazil. Studies pointed out that substance abuse is also a stigmatized behavior by health professionals (Ronzani, Furtado & Higgins-Biddle, 2009; Silveira, Martins & Ronzani, 2009; Soares et al., 2001). This may lead to several implications for substance abuse treatment, once professionals are more willing to give poor and coercive treatment. Attached to this, the process of stigmatization reinforces the exclusion model that secures another aspect of discrimination: compulsory treatment, a method that is becoming popular again in Brazil in relation to drug use (Fortes, 2010; Moreira & Loyola, 2011; Scisleski & Maraschin, 2008). Compulsory treatment involves the exercise of power in placing labeled individuals in separate circumstances and treating them diffrently, and leads to several implications regarding social relationships and integration impairment, and may also compromise chances for recovery (Link, Castille & Stuber, 2008; Schomerus et al., 2011).
Besides that, stigma acts as a barrier to health care (Ahern, Stuber & Galea, 2007). In attempt to avoid stigmatization and discrimination, substance dependents may abstain from seeking help. Ths leads to poor adherence to treatment, aggravation of symptoms, decrease in quality of life, low self-esteem, and low self-efficy (Li, Lee, Thammawijaya, Jiraphongsa & Rotheram-Borus, 2009; Ssebunnya, Kigozi, Lund, Kizza & Okello, 2009; Verhaeghe, Bracke & Bruynooghe, 2008). Threfore, the study of the desire for social distance from health professionals regarding alcohol and other drugs dependents can contribute to the management of appropriate strategies for changing professionals' attitudes and improve quality of care for these patients (Palm, 2006; Ronzani, 2007).
Considering the fact that many alcohol and other drugs dependents attend diffrent types of health services, which leads to a direct contact between them and health professionals, this study aimed to investigate which factors were associated with the desire for social distance of people who are substance dependents, among health professionals in Juiz de Fora city, Minas Gerais, Brazil.
Method
Study design and participants
This was a cross-sectional study conducted in a sample of 183 health professionals. Thesample consisted of 183 professionals from 2 general hospitals and 1 outpatient mental health service in Juiz de Fora, in the state of Minas Gerais, Brazil. Thse hospitals are linked to the universal health care system as secondary and tertiary care facilities. Thefist is affiated with Universidade Federal de Juiz de Fora and the second with the state of Minas Gerais. Thse services cover a population of approximately 516,247 people.
Owing to the large number of health professionals working in the two hospitals (786 and 336), a stratifid sampling was performed. Five professionals' categories were used to perform the sampling: physicians, nurses, nursing technicians, other technicians, and other graduated health professionals (e.g. psychologists, physiotherapists). Thesample size estimated was 131 people, in order to have a precision of 1.5 points with a 95% confience interval. In case of refusals or not being able to fid the professional, a replacement list was created, expanding the sample size in 20%. Owing to the small number of health professionals in the outpatient mental health service (70), we tried to interview all professionals. Theresponse rate was 74% (52 of 70).
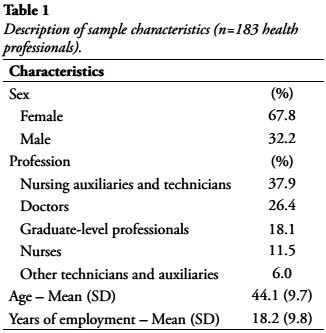
The sample was composed mostly by women (67.8%), with a mean age of 44.1 years old (SD=9.8). The number of years employed in any area of the health fild ranged from 1 to 38, with a mean of 18.2 years. Most of the professionals were auxiliaries and nursing technicians (37.9%). Doctors represented 26.4% and nurses constituted 11.5% of the sample. Other professionals represented 24.1%. Sample characteristics are described in Table 1.
Procedures and instruments
Participants completed self-reported questionnaires assisted by researchers throughout the data collection process. Instruments used were:
- Questionnaire about Professional Characteristics: This questionnaire characterized study participants in terms of sociodemographic data, such as gender, age, marital status, occupation, and years of employment. It also evaluated whether the health professional had personal or professional contact with substance users (Silveira, 2010).
- Vignettes: The vignettes were adapted from Link et al. (1999) and Peluso and Blay (2008). Thy describe a character that is alcohol, marijuana, or cocaine dependent, according to the DSM-IV criteria for substance dependence. Thevignettes assessed the perception of dangerousness, belief in recovery, and the desire for social distance. Here is an example of the alcohol vignette:
José is 45 years old and always uses alcohol. However, recently, José has been drinking more than usual to achieve the same effects as before. Every time he tries to slow down or stop drinking, he becomes agitated, has nausea, tremors and cold sweats, which are relieved by drinking more alcohol. Even though alcohol is harmful to health, José cannot stop drinking. He has had problems at home with his wife and children. Also, his boss has noticed that he has been quite absent at work and his production is way below normal.
For each vignette, participants were asked to evaluate how much they agreed with the assertions using a 7-point Likert scale ranging from "totally disagree" to "totally agree." Thescore of social distance was obtained through the sum of fie items, representing behaviors of avoiding contact with substance dependents. In the scale, the higher the score, the lower the desire for social distance.
All participants signed a consent form and all the research procedures were approvedby Universidade Federal de Juiz de Fora institutional review board, process number 0015/09.
Data Analysis
To reduce possible systematic errors in data entry, 25% of the questionnaires were randomly selected, and the answers on the hard copy were compared against those in the database. No errors were observed. Data were analyzed in R language (R Core Team, 2014). We used multiple linear regression for analyzing how the explanatory variables were related to the dependent variable. Predictors were selected taking into account the theoretical framework and results from a previous study. Thesample size was suffiient to fid a medium effct in the regression as defined by Cohen (1984) with fie predictors.
Social distance was the dependent variable measured by the social distance scale for each substance, and the explanatory variables were sex, age, contact, years working on profession, perception of dangerousness, and belief in patient recovery. Assumption of independence and multicollinearity were checked by the Durbin–Watson test and VIF. Residuals and inflence cases were checked using graphics. For each analysis, alpha level was set at 0.05.
Results
Among the sample of 183 health professionals, 67.4% reported having a professional or personal contact with alcohol or other drugs heavy users or dependents. Theresults of the regression models for each of the three substances are presented below.
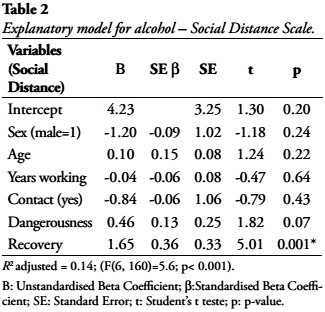
Alcohol
Belief in recovery was the only variable able to explain social distance at a statistical significant level as presented in Table 2. Each point on belief in recovery was associated with an increase of 1.65 points in the social distance scale. All the other variables showed no explanatory relationship with social distance. The six predictors accounted for 14% of the variance.
Cocaine
As the alcohol model, belief in recovery was statistically significant for the explanation of social distance. Each point on the belief in recovery variable was associated with an increase of 1.50 points in the social distance scale. The perception of dangerousness was also statistically significant. Each point added on the perception of dangerousness scale was associated with a decrease of -0.54 in the social distance scale. The other variables were not statistically significant as shown in Table 3. The model accounted to 15% of the variance.
Marijuana
Perception of dangerousness and belief in recovery were statistically significant in explaining social distance. The results indicated that each point in the belief in recovery was associated with an increase of 1.43 points in the social distance scale. In contrast, each point added in the perception of dangerousness scale was associated with a decrease of 0.66, indicating greater desire for social distance (B= -0.66). Th other variables were not statistically associated with social distance, as shown in Table 4. The model accounted to 15% of the variance.
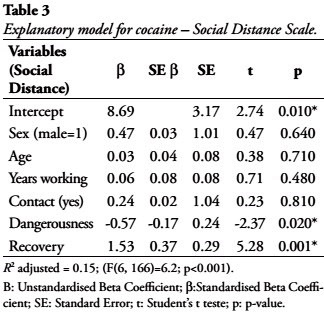
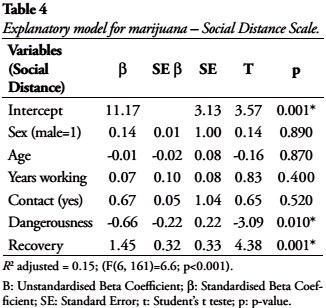
No violations of multicollinearity and independence assumptions for the three regression models were detected. Residuals were normally distributed, and no inflential cases were detected in the alcohol and the marijuana models. The cocaine model had inflential cases and residuals were not normally distributed. Threfore, generalizations about the cocaine model should be interpreted with caution.
Discussion
This study might shed some light on the development of evidence, not only in the Brazilian context, in which few studies were conducted on the topic of stigmatization (Link et al., 1987; Ssebunnya et al., 2009; Verhaeghe et al., 2008), but also to enhance the understanding of the topic more broadly.
Considering the explanatory model for social distance, sex and age were not statistically significant for alcohol, cocaine, or marijuana models. As found in the study developed by Coker (2005), judgments of social distance were also not related to the sample of sociodemographic characteristics.
Contact with substance dependents was not statistically significant in explaining the model for social distance for the three stigmatized conditions. Some studies in the literature indicate that contact with people with stigmatized health conditions can increase or decrease the desire for social distance (Angermeyer & Matschinger, 1997; Corrigan et al., 2005). Our results are in agreement with Pereira (2002), which suggests that only the contact with drug users does not determine the increase or decrease in social distance. Contact may be investigated in a deeper level, considering the quality of interactions between substance dependents and health professionals.
The perception of dangerousness was considered explanatory for social distance related to cocaine and marijuana dependents. In a study conducted in the United States on public conceptions of patients with mental illness (Link et al., 1999), respondents reported more desire for social distance for cocaine dependence, followed by alcohol dependence and schizophrenia. The authors also found an association between the desire for social distance and the belief that people with these conditions can be violent. As the symptoms of mental illness are associated with violence, people suffring from it are negatively affected by rejection and may be reluctant to seek professional help for fear of stigmatization and exclusion. Other studies showed that stigmatization could lead to social distance and exclusion of stigmatized people (Angermeyer & Matschinger, 1997; Dietrich et al., 2004).
The association between the perception of dangerousness and social distance for cocaine and marijuana users leads us to the following question: is social distance related to the illegal status of the substances?
Belief in recovery was statistically significant for all the three models. The greater the belief in recovery, the lower the desire for social distance. Belief in recovery is of great importance, since it can contribute to the expectations of rejection, which leads to poorer treatment outcomes (Angermeyer & Matschinger, 1997; Hebl, Tickle, & Heatherton, 2003). Studies showed that, when substance users perceive treatment as a threat rather than as an advantage, they tend to avoid treatment in order to avoid stigma and its consequences (Link et al., 1999). Threfore, stigma seems to be an important factor influencing the outcomes of health services interventions, and for the improvement of subjective quality of life (Dietrich et al., 2004).
The main strength of this study consists in the utilization of a method consistent with the methodological recommendations for the study of social stigma. The use of vignettes addresses the bias of self-reported measures and interviews, which is a common issue in the fild of social psychology (Goffan, 1978; Kelleher, 2007). Substance abuse is one of the conditions seen in the most negative way (Blascovich et al., 2003), so it is recommended to reorganize services and training professionals in order to meet the needs of patients and achieve better substance abuse treatment outcomes (Hansson, 2006).
Acknowledgement
We thank the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq – Ronzani research fellowship PROCAD 552452/2011-4); the Minas Gerais State Research Foundation, which funded this research with process SHA APQ-1006-5.06/07 and the Pesquisador Mineiro Program, and the Deanery Research of Universidade Federal de Juiz de Fora (Pró-Reitoria de Pesquisa – PROPESQ/UFJF).
References
Ahern, J., Stuber, J., & Galea, S. (2007). Stigma, discrimination and the health of illicit drug users. Drug and Alcohol Dependence, 88(2-3), 188-96. [ Links ]
Angermeyer, M. C., & Matschinger H. (1997). Social distance towards the mentally ill: results of representative surveys in the Federal Republic of Germany. Psychological Medicine, 27(1), 131-141. [ Links ]
Blascovich, J., Mendes, W. B., Hunter, S. B., & Lickel, B. (2003). Stigma, Threat, and Social Interactions. In: Heatherton, T. F., Kleck, R. E., Hebl, M. R., & Hull J. G. (Eds), Thesocial psychology of stigma (pp. 307-33). New York: TheGuilford Press. [ Links ]
Cohen, J. (1984). Statistical power analysis for the behavioral sciences. Third ed. Hillsdale: Lawrence Erlbaum. [ Links ]
Coker, E. M. (2005). Selfhood and social distance: toward a cultural understanding of psychiatric stigma in Egypt. Social Science and Medicine, 61(5), 920-30. [ Links ]
Corrigan, P. (2004). How stigma interferes with mental health care. American Psychologist, 59(7), 614-625. [ Links ]
Corrigan, P., Lurie, B. D., Goldman, H. H., Slopen, N., Medasani, K., & Phelan S. (2005). How adolescents perceive the stigma of mental illness and alcohol abuse. Psychiatric Services, 56(5), 544-50. [ Links ]
Dietrich, S., Beck, M., Bujantugs, B., Kenzine, D., Matschinger, H., & Angermeyer, M. C. (2004).The relationship between public causal beliefs and social distance toward mentally ill people. Australian and New Zealand Journal of Psychiatry, 38(5), 348-354. [ Links ]
Fortes, H. M. (2010). Tratamento compulsório e internações psiquiátricas. Revista Brasileira de Saúde Materno Infantil, 10(Suppl 2), s321-s330. [ Links ]
Goffan, E. (1978).Estigma: notas sobre a manipulação da identidade deteriorada (2nd ed.) Rio de Janeiro: Zahar. [ Links ]
Hansson, L. (2006). Determinants of quality of life in people with severe mental illness. Acta psychiatrica Scandinavica Supplementum,113(s429), 46-50. [ Links ]
Hebl, M. R., Tickle, J., & Heatherton, T. F. (2003). Awkward Moments in interactions between nonstigmatized and stigmatized indivivuals. In: Heatherton, T. F., Kleck, R. E., Hebl, M. R., & Hull, J. G. (Eds), TheSocial Psychology of Stigma (p. 275-306). New York: TheGuilford Press. [ Links ]
Kelleher, S. (2007). Health care professionals' knowledge and attitudes regarding substance use and substance users. Accident and Emergency Nursing, 15(3), 161-5. [ Links ]
Lauber, C., Nordt, C., Falcato, L., & Rössler, W. (2004). Factors influencing social distance toward people with mental illness. Community mental health journal, 40(3), 265-274. [ Links ]
Li, L., Lee, S. J., Thammawijaya, P., Jiraphongsa, C., & Rotheram-Borus, M. J. (2009) Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care, 21(8), 1007-13. [ Links ]
Link, B., Castille, D. M., & Stuber, J. (2008). Stigma and coercion in the context of outpatient treatment for people with mental illnesses. Social Science and Medicine, 67(3), 409-19. [ Links ]
Link, B. G., Cullen, F. T., Frank, J., & Wozniak, J. F. (1987). Thesocial rejection of former mental patients: understanding why labels matter. The American journal of sociology, 92(6), 1461-1500. [ Links ]
Link, B. G., & Phelan, J. C. (2013). Labeling and stigma. In: Aneshensel, C. S., Phelan, J. C., & Bierman, A. (Eds.), Handbook of sociology of mental health (pp. 481-494). New York: Springer. [ Links ]
Link, B. G., Phelan, J. C., Bresnahan, M., Stueve, A., & Pescosolido, B. A. (1999). Public conceptions of mental illness: labels, causes, dangerousness, and social distance. American journal of public health, 89(9), 1328-1333. [ Links ]
Link, B. G., Struening, E. L., Neese-Todd, S., Asmussen, S., & Phelan, J. C. (2001). Stigma as a barrier to recovery: Theconsequences of stigma for the self-esteem of people with mental illnesses. Psychiatric Services, 52(12), 1621-1626. [ Links ]
Moreira, L., & Loyola, C. M. D. (2011). Internação involuntária: as implicações para a clínica da enfermagem psiquiátrica. Revista da Escola de Enfermagem da USP, 45(3), 692-699. [ Links ]
Palm, J. (2006). Moral concerns - treatment staff and user perspectives on alcohol and drug problems. Stockholm: University of Stockholm.
Peluso, E. T. P., & Blay, S. L. (2004). Community perception of mental disorders: A systematic review of Latin American and Caribbean studies. Social Psychiatry and Psychiatric Epidemiology, 39(12), 955-961.
Peluso, E. T. P., & Blay, S. L. (2008). Public Perception of Alcohol Dependence. Revista Brasileira de Psiquiatria, 30(1), 19-24. [ Links ]
Pereira, M. E. (2002). Psicologia social dos estereótipos. São Paulo: Editora Pedagógica e Universitária. [ Links ]
Pescosolido, B. A., Monahan, J., Link, B. G., Stueve, A., & Kikuzawa, S. (1999). The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. American Journal of Public Health, 89(9), 1339-1345. [ Links ]
R Core Team. (2014). R: A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna (AT). Acesso em 10 de Agosto de 2013, em http://www.R-project.org/
Ronzani, T. M. (2007). A reforma curricular nos cursos de saúde: qual o papel das crenças? Revista Brasileira de Educação Médica, 31(1), 38-43. [ Links ]
Ronzani, T. M., Furtado, E. F., & Higgins-Biddle, J. (2009). Stigmatization of alcohol and other drug users by primary care providers in Southeast Brazil. Social science & medicine, 69(7), 1080-1084. [ Links ]
Rüsch, N., Angermeyer, M. C., & Corrigan, P. W. (2005). Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. European Psychiatry, 20(8), 529-539. [ Links ]
Schomerus, G., Lucht, M., Holzinger, A., Matschinger, H., Carta, M. G., & Angermeyer, M. C. (2011). Thestigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol and Alcoholism, 46(2), 105-12. [ Links ]
Scisleski, A. C. C. I., & Maraschin, C. (2008). Internação psiquiátrica e ordem judicial: saberes e poderes sobre adolescentes usuários de drogas ilícitas. Psicologia em Estudo, 13(3), 457-465. [ Links ]
Silveira, P. S. (2010). Estigmatização do uso de álcool e outras drogas entre profissionais de saúde de Juiz de Fora, Dissertação de Mestrado, Universidade Federal de Juiz de Fora, Juiz de Fora, Minas Gerais.
Silveira, P. S., Martins, L. F., & Ronzani, T. M. (2009). Moralização sobre o uso de álcool entre agentes comunitários de saúde. Psicologia: Teoria e Prática, 11(1), 62-75. [ Links ]
Soares, R. G., Silveira, P. S., Martins, L. F., Gomide, H. P., Lopes, T. M., & Ronzani, T. M. (2001). Distância social dos profissionais de saúde em relação à dependência de substâncias psicoativas. Estudos de Psicologia, 16(1), 91-98.
Ssebunnya, J., Kigozi, F., Lund, C., Kizza, D., & Okello, E. (2009). Stakeholder perceptions of mental health stigma and poverty in Uganda. BMC International Health and Human Rights, 9(1), 5. [ Links ]
Verhaeghe, M., Bracke, P., & Bruynooghe, K. (2008). Stigmatization and self-esteem of persons in recovery from mental illness: the role of peer support. International Journal of Social Psychiatry, 54(3), 206-18. [ Links ]
 Corresponding address
Corresponding address
Pollyanna Santos da Silveira
Rua José Lourenço Kelmer, s/n
Campus Universitário – São Pedro
CEP: 36036-900 – Juiz de Fora/MG
E-mail: pollyannassilveira@gmail.com
Received on 23/07/2015
Revised on 11/10/2015
Accepted on 18/11/2015














