Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Psicologia: teoria e prática
versão impressa ISSN 1516-3687
Psicol. teor. prat. vol.22 no.3 São Paulo set./dez. 2020
ARTICLES
CLINICAL PSYCHOLOGY
Characterization and psychological aspects of patients with erectile dysfunction
Caracterización y aspectos psicológicos de pacientes con disfunción eréctil
Pedro Junior R. CoutinhoI ; Carmen Silvia C. E. FernandesI,II
; Carmen Silvia C. E. FernandesI,II ; Fernando N. Facio JrIII
; Fernando N. Facio JrIII ; Maria Cristina de O. S. MiyazakiIII
; Maria Cristina de O. S. MiyazakiIII
IRegional Faculty of Medicine of São José do Rio Preto Foundation (FUNFARME), São José do Rio Preto, SP, Brazil
IIUnion of Schools of Grandes Lagos (UNILAGO), São José do Rio Preto, SP, Brazil
IIIMedical School of São José do Rio Preto (FAMERP), São José do Rio Preto, SP, Brazil
ABSTRACT
This study aimed to characterize patients with erectile dysfunction (ED) evaluated by the psychologist who participates in the Urology team of a teaching hospital. The following data from medical records of patients treated between January / 2011 and April / 2015 were analyzed: 1) the urologist's referral, with diagnosis and the reason for the request for psychological evaluation; 2) the patient's psychological records, filed at the Psychology Service. Data of 233 male patients were analyzed, who had a mean age of .34 ± 1.18 and a high prevalence of ED of organic cause (72.1%). Organic, psychological factors and lifestyle associated with the etiology of ED were identified: behavioral (smoking and alcohol consumption.), advanced age, prostate cancer, premature ejaculation, depression, and anxiety. Data pointed out the importance of psychological assessment associated with the medical diagnosis of ED to provide proper treatment.
Keywords: erectile dysfunction; characterization; psychological assessment; health psychology; outpatients.
RESUMEN
Este estudio tuvo como objetivo caracterizar a pacientes con disfunción eréctil (DE) evaluados por el psicólogo que participa del equipo de urología de un hospital de enseñanza. Se analizaron los siguientes datos de los prontuarios de pacientes atendidos entre enero/2011 y abril/2015: 1. encaminamiento del urólogo, con diagnóstico y motivo de la solicitud para evaluación psicológica y 2. prontuario psicológico del paciente, archivado en el ambulatorio de psicología. Se analizaron datos de 233 pacientes del sexo masculino, con media de edad 57,34 ± 1,18 y alta prevalencia de la DE de causa orgánica (72,1%). Los factores orgánicos, psicológicos y estilo de vida asociados a la etiología de la DE fueron identificados: comportamentales (tabaquismo y etilismo), edad avanzada, cáncer de próstata, eyaculación precoz, depresión y ansiedad. Los datos indican la importancia de la evaluación psicológica asociada al diagnóstico médico de la DE, para proporcionar el tratamiento adecuado.
Palabras clave: disfunción eréctil; caracterización; evaluación psicológica; psicología de la salud; pacientes ambulatorios.
1. Introduction
Erectile dysfunction (ED) is the persistent or recurrent inability to achieve and maintain sufficient penile rigidity for satisfactory sexual intercourse (Yafi et al., 2016). In Brazil, ED affects 45% of the population aged over 18 and 52% of men aged 40 to 70 (Gonzáles et al., 2013).
More than 80% of ED cases have an organic etiology (e.g., vascular, endocrine, neurological, or associated with tissue aging, surgery, or medication). Even when caused by organic factors, ED often involves psychological components due to its negative impact on "interpersonal relationships, mood and quality of life" (Yafi et al., 2016, p. 1). A systematic review on the psychosocial impact of ED concluded that it affects the physical, psychological, and social functioning of patients and that these aspects should be addressed during treatment. When the treatment of ED includes physical and psychological aspects, it tends to be more effective (McCabe & Alhof, 2014).
Psychological factors are responsible for 10% to 20% of cases of ED, in which case it is called psychogenic ED. Although less studied than organic ED, it should always be investigated. Symptoms that aid in the diagnosis of psychogenic ED include abrupt onset, intermittent character, loss of erection maintenance, quality nocturnal erection, and excellent response to phosphodiesterase-5 inhibitors (e.g., sildenafil, tadalafil, vardenafil). Organic ED is gradual and progressive in origin, the low response to stimuli is consistent, and the erection is better when the man is in an upright position (Yafi et al., 2016).
Research on ED evaluation and treatment, regardless of its etiology, suggests that psychological (e.g., depression, anxiety), spouse- or partner-related, situational factors, and daily life stressors should always be investigated (Brotto et al., 2016).
There is a strong association between depressed mood and sexual functioning (Brotto et al., 2016). This association is seen as bidirectional, that is, "depressed affect can impair sexual arousal and cause ED, while decreased sexual activity and lack of satisfaction with one's sexual life can trigger depressive symptoms" (Rajkumar & Kumaran, 2015, p. 114). The use of antidepressants can negatively affect sexual life (Brotto et al., 2016).
The association between anxiety and ED has also been investigated, and men with the problem have higher levels of anxiety than sexually healthy men. Panic disorder and anxiety related to sexual performance are associated with ED, and a prevalence of anxiety disorders ranging from 2.5% to 37% has been identified in men with ED (Brotto et al., 2016).
Several diseases and health-related behaviors are also associated with ED, such as systemic arterial hypertension, diabetes mellitus, smoking, dyslipidemia, neurological diseases, hormonal disorders, chronic use of some medications, and psychological disorders (Sarris et al., 2016). Socioeconomic factors such as low income, low educational level, unemployment, and single marital status have been associated with the presence of erection difficulties (Abdo, Oliveira, Scanavino, & Martins, 2006).
Based on a systematic review of the literature, several recommendations were made to assist in understanding and adequately managing sexual dysfunctions, including ED (Brotto et al., 2016). According to these recommendations, it is necessary to:
• Consider constitutional and developmental variables and use the biopsychosocial model of health; assess early those patients who have undergone hypospadias surgery; provide psychological support to the patient throughout follow-up; address sex identity and sexual orientation; evaluate sexual anxiety associated with childhood experiences; investigate the history of sexual abuse.
• Consider individual traits or lifestyles as personality factors; identify dysfunctional cognitive schemas, use cognitive restructuring to change them; and evaluate patterns of sexual excitation and inhibition.
• Consider the current stage of life and aging, such as sexual function and satisfaction in patients with infertility and during the postpartum period; evaluate sexual health and the presence of diseases and mental disorders that are prevalent in older patients; investigate adverse events throughout life and the resulting symptoms, such as anxiety and depression.
• Analyze factors related to psychological processing, such as causal attributions to negative sexual events; positive and negative efficacy expectations regarding sexual performance; thoughts during sexual activity; anxiety and depressed mood related to sexual activity.
• Evaluate mental health to identify, for example, stress, depression, anxiety disorders, post-traumatic stress disorder, and substance abuse.
• Analyze interpersonal and relationship aspects, including by evaluating the spouse or partner, such as the presence of diseases that can affect sexual functioning and relationship quality.
According to its etiology and severity, three possible lines of treatment are available for ED. The first includes psychotherapy/sex therapy and/or oral medications; the second involves drug-induced erection, intraurethral therapy, and vacuum devices; and the third consists of penile prosthesis implantation. If a treatment line is unsuccessful, the next one is used, after careful evaluation regarding age, the presence of comorbidities, patient and/or partner expectations regarding sexual activity, and the socioeconomic and cultural aspects of the couple (Abdo & Afif-Abdo, 2012). Recommendations based on the effectiveness of ED interventions include the use of couples or group psychotherapy combined with medication (Brotto et al., 2016). Psychologists working in the health field have often integrated different multi- and interdisciplinary teams. At Hospital de Base, Medical School of São José do Rio Preto, a high-complexity teaching hospital, a psychologist is part of the urology team and evaluates and guides patients with ED treated at the Urology Outpatient Clinic. The psychological assessment data are used by the team to understand the functioning of the patient and help him choose a therapy. Based on the literature and the clinical observations about the psychological care performed by the urology team, some hypotheses were formulated: Older patients have ED that is most often organic; ED is associated with symptoms of anxiety and depression; higher educational level is associated with fewer symptoms of anxiety and depression; patients in stable unions and older patients are more vulnerable to symptoms of anxiety and depression.
In this context, the objective of this study was to characterize patients with ED who were seen by the urology team's psychologist between January 2011 and May 2015.
2. Method
This retrospective descriptive study was approved by the Research Ethics Committee of the Medical School of São José do Rio Preto (Faculdade de Medicina de São José do Rio Preto - FAMERP) under Opinion no. 1,385,181.
2.1 Participants
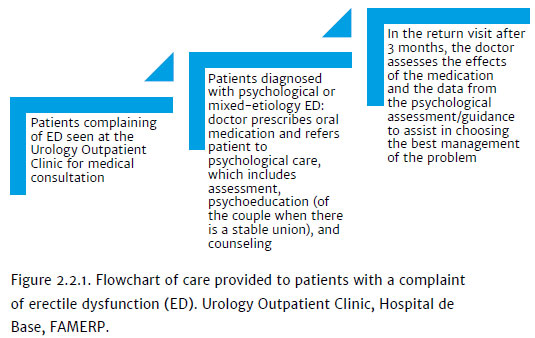
The study included 233 adult men who complained of ED of psychological or mixed origin (organic and psychological) who were treated at the Urology Department of Hospital de Base and were referred to the psychologist member of the team. Figure 2.2.1 shows the flowchart of the care of these patients.
2.2 Procedure
The study data were obtained from the psychological records of patients with ED treated at the referred department between January 2011 and May 2015. After medical consultation, the patient was referred for psychological evaluation, which was immediately scheduled. On the scheduled date, the patient arrived at the Psychology Outpatient Clinic and was seen by the psychologist who was part of the urology team. An initial semi directed interview evaluated the presence of psychogenic sexual disorders, the presence of social support from the partner, and other patient complaints. A new session was then scheduled for the application of the Hospital Anxiety and Depression Scale (HAD) and International Index of Erectile Function (IIEF5). When the patient was in a stable partnership/union, the spouse was invited to attend the outpatient clinic to receive guidance to help manage the problem. The third evaluation session involved a review of the process and guidance on treatment when necessary (e.g., return to a medical consultation with the psychological report included in the medical records; sexual psychotherapy; individual or couples' psychotherapy).
The psychological care of patients whose data were analyzed in this study included the following:
• Semistructured interview: This evaluated the presence of psychogenic sexual disorders, the presence of social support from the partner, and other personal issues that may contribute to the dysfunction. It included 1. personal identification data; 2. complaint; 3. sexual history; 4. history and current presence of diseases and mental disorders; 5. nature of the relationship with the partner; and 6. other issues that may contribute.
• Hospital Anxiety and Depression Scale (HAD). A self-report instrument developed by Zigmond and Snaith (1983), HAD aims to identify cases (possible or probable) of mild anxiety disorder and/or depression in nonclinical populations.
The version of the HAD translated and validated for Brazil has 14 questions, seven of which focus on anxiety and seven on depression. Each item can be scored from 0 to 3, for a maximum score of 21 points for each scale. The cut off scores are 0 to 8, no anxiety; > 9, anxiety; and 0 to 8, no depression; > 9, depression. The HAD scales (anxiety and depression) showed an internal consistency of 0.68 and 0.77, respectively. The 8/9 cut-off score had a sensitivity of 93.7% and 72.6% for anxiety and 84.6% and 90.3% for depression (Botega, Bio, Zomignani, Garcia, & Pereira, 1995).
• International Erectile Function Index (IIEF5): This multidimensional questionnaire has 15 questions addressing relevant points of male sexual function: erectile function, orgasmic function, sexual desire, sexual satisfaction, and general satisfaction. The instrument was translated and validated for Portuguese and had adequate sensitivity and specificity to detect changes related to ED (Gonzáles et al., 2013). According to the responses, ED can be classified from severe to absent. The short version of the questionnaire (including questions 1 to 5 and question 15 from the original questionnaire) was used in this study. It evaluates only the erectile function and the patient's confidence in obtaining an erection. Each question has a value ranging from 0 to 5, and only one alternative can be chosen. The sum of the scores of the chosen options results in a score ranging from 0 to 30, which classifies ED as follows: 0-6, severe; 7-12, moderate; 13-18, mild to moderate; 19-24, mild; and 2530, absent (Rosen, Cappelleri, & Gendrano III, 2002).
The diagnosis of ED was established according to the specialized literature as organic, psychological, or mixed (organic and psychological) (Cavalcanti & Cavalcanti, 2012).
The data were analyzed quantitatively with descriptive statistics and nonparametric tests (Pearson's chi-squared and Fisher's exact tests).
3. Results
In the period between January 2011 and May 2015 (4 years and 5 months), 45,657 patients were treated at the Urology Outpatient Clinic. Of these, 233 arrived at the outpatient clinic with a hypothetical diagnosis of sexual dysfunction not due to an unspecified disorder or organic disease. After consultation with the urologist of the institution, the majority (n = 168; 72.1%) of these patients were diagnosed with ED of organic cause, 45 (19.3%) with psychological ED, and 20 (8.6%) with mixed ED (organic and psychological).
The age ranged from 18 to 83 years (mean: 57.34 ± 1.18). Most patients were white (166; 71.2%), followed by black (5; 2.1%), mixed (28; 12.0%), and those with no data available (34; 14.6%). Regarding marital status, 127 (54.5%) were married, 20 (8.6%) divorced, 38 (16.3%) single, 8 (3.4%) widowed, 9 (3.9%) in a stable relationship, and 31 (13.3%) unknown. Of the 233 patients, 135 (57.9%) had a primary education, 33 (14.2%) had a secondary education, 6 (2.6%) had a higher education, 5 (2.1%) were illiterate, and there were no data on 54 (23.2%).
The different causes of ED were also grouped by patient age. Organic causes were more frequent among patients aged 60 to 69 years (n = 65; 38.7%), psychological causes between 50 and 59 years (n = 15; 33.3%), and mixed causes between 60 and 69 years (n = 10; 50.0%). The main comorbidities of patients with organic ED were prostate cancer, diabetes mellitus, heart disease, and other factors, such as smoking and alcohol consumption. Comparative analysis of the demographic data showed a significant difference in the severity distribution of ED (mild, moderate, severe) between the white and non-white groups (Table 3.1).
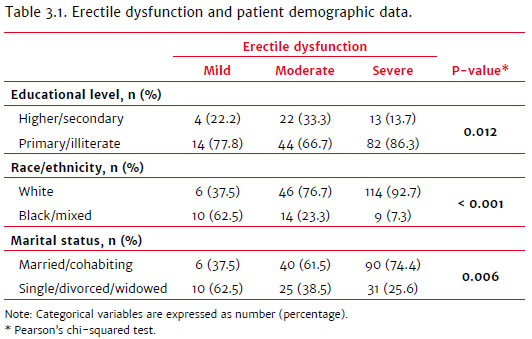
There was a higher frequency of ED of organic cause in older patients (chi-squared: p = 0.0031) and less educated patients (chi-squared: p < 0.0001). Married patients had a higher frequency of ED of organic cause (chi-squared: p < 0.0001).
The prevalence of anxiety symptoms differed significantly by race and marital status. Most patients without anxiety symptoms were white, and among those with anxiety, there was a higher proportion of mixed-race and black patients (Table 3.2). Regarding marital status, in the group with symptoms of anxiety, there was a balance between married (or in a stable union) and single patients. In the group without anxiety, the majority of patients were married (Table 3.2). There was no significant difference between the demographic groups regarding depression symptoms (Table 3.2).
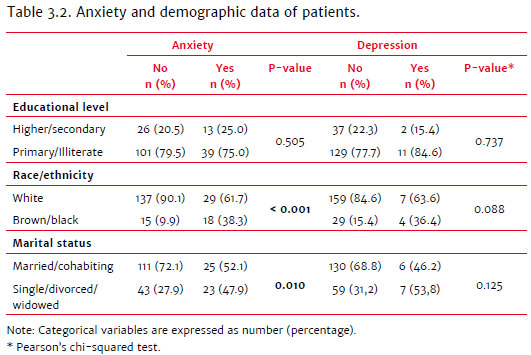
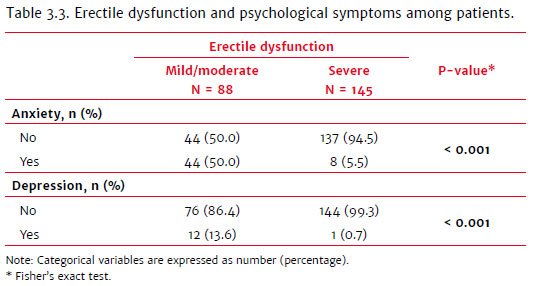
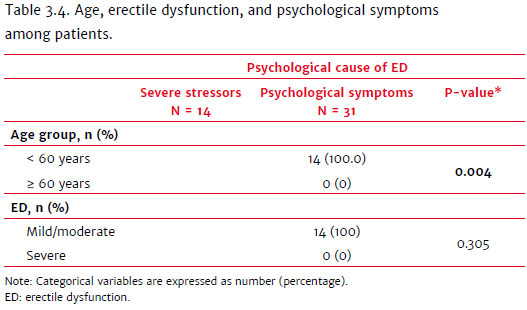
Table 3.3 shows that psychological symptoms (anxiety and depression) were more frequently associated with mild and moderate ED than severe ED. This finding is corroborated by the data in Table 3.4, which shows that patients with severe ED mostly had ED of organic cause rather than psychological or mixed causes.
4. Discussion
The characteristics of the patients who underwent psychological assessment are in accordance with national and international prevalence studies (Moreira, Glasser, Santos, & Gingell, 2005; Gonzáles et al., 2013; Colson, Cuzin, Faix, Grellet, & Huyghes, 2018) that have associated ED with older age. Age, therefore, is an important risk factor for the development of ED, since it is also associated with an increased risk of organic and psychological diseases (Abdo et al., 2006; Sarris et al., 2016). Older patients today seem to be more affected due to their greater vulnerability to chronic diseases, which in turn increases the likelihood of ED (Colson et al., 2018). Organic ED was the most prevalent kind in this study. ED is associated with organic clinical conditions and psychological factors, and it is difficult to classify the percentage of only organic causes.
Even in cases of organic ED, there is an influence of psychological factors as aggravating or maintenance factors of the condition. In most cases, there is a complex interaction of biological, psychological, and social risk factors (Cavalcanti & Cavalcanti, 2012). The presence of ED negatively affects the couple's relationship (Nguyen, Gabrielson, & Hellstrom, 2017). Older age and low educational level may also be related to this finding, as age increases the vulnerability to chronic diseases. In addition, low educational and socioeconomic levels have been consistently associated with worse health conditions and greater vulnerability to diseases.
Mixed-cause ED was associated mainly with chronic diseases, unhealthy habits such as smoking and alcohol consumption, premature ejaculation, anxiety, and depression, all risk factors for the development of ED and all with a predominance in older men. This result is in line with another study that found an association between older age and the causes cited above (Abdo et al., 2006).
Psychological causes were identified in 19.3% of the patients evaluated in this study. According to the literature, this category of cause is present among young men and men older than 50 years and is present in 40% of patients with ED as an exclusive cause (Rosen et al., 2002). Psychological ED is associated with fear of performance failure, sexual violence, difficulties living with the diagnosis of stigmatizing diseases (HIV and cancer), marital and economic difficulties, loss of the spouse or close relatives, long-term premature ejaculation, low self-esteem, depression, and anxiety (Cavalcanti & Cavalcanti, 2012). As in other studies, depression, anxiety, and premature ejaculation were the most common psychological causes among our patients (Abdo et al., 2006; Heiden-Rootes et al., 2017). Although young patients with psychological ED were identified, most patients with this etiology were older. The urologist referred all of them to the psychologist since the study was conducted in the outpatient clinic of a high-complexity hospital by a multidisciplinary urology team that had a psychologist.
Understanding the etiology of the problem is essential to defining the most appropriate treatment. For patients with ED of mixed or psychological etiology, psychotherapy is the therapeutic modality that should be indicated (Cavalcanti & Cavalcanti, 2012). Psychotherapeutic techniques have been improving at helping these patients and preventing depression resulting from erectile difficulties. Psychotherapy is part of the first-line treatment for this problem. The established objectives of psychotherapy are to identify and address resistance to medical intervention that results in treatment abandonment; reduce performance anxiety; understand the context in which the patient has sex; promote psychoeducation; and adjust the patient's "sexual script." The effectiveness of therapy depends on focusing on pleasure, reducing anxiety, decreasing the emphasis on sexual acts, and promoting awareness of sexual sensations. The following can optimize the results: therapeutic bond, partner's motivation/support, and establishment of goals for the patient and partner. The focus of sex therapy should be not only performance improvement but also sexual comfort and pleasure (Abdo & Afif-Abdo, 2012).
Organic ED occurred mainly in men older than 40, mostly in those aged 60 to 69 years. ED related to organic diseases usually affects men aged 40-70 years; therefore, aging is strongly associated with the increased prevalence of organic ED. These data are in line with findings that indicate that ED is an age-dependent condition (Nicolosi et al., 2004).
The most frequent comorbidities were diabetes, heart disease, prostate cancer, and depression, and they were considered risk factors for the development of ED, a finding also confirmed by other studies (Abdo et al., 2006; Gonzáles et al., 2013; Heiden-Rootes et al., 2017). Patients diagnosed with chronic diseases become vulnerable populations with a high risk for ED (Colson et al., 2018).
Prostate cancer treatment was identified in this study as a main cause of ED. Its incidence was similar to that in another study (Abdo et al., 2006). The association of prostate cancer treatment with ED is related to the sequelae of radical prostatectomy surgery. One study showed that ED incidence after radical prostatectomy reached 60% (Reis, Rodrigues Netto, Reinato, Thiel, & Zani, 2004).
The mean age of patients treated for prostate cancer in this study was 42 years (± 1.18), a mean age considered uncommon for the development of the disease, which is more prevalent in men over 65 (Goulart, 2012). It is possible that the diagnosis of prostate cancer in younger patients was due to frequent campaigns to prevent the problem. In addition, older patients treated by the multidisciplinary urology team receive instructions for their children to attend the outpatient clinic for prostate cancer prevention and early diagnosis, given the hereditary nature of the disease.
It is important to note the possible association between ED and low education, a result found in this study and Abdo et al. (2006). Low educational level may be associated with prostate cancer progression, i.e., lack of early identification of the problem, less access to health care, and lack of adequate information about prostate cancer, in such forms as taboos and misconceptions about the prevention of the disease.
Most patients did not present psychological symptoms associated with ED (72%), but the psychological evaluation was important to strengthen and guide the treatment and follow-up of possible causes. The available therapeutic alternatives are subdivided depending on the causes (curable or incurable) and the severity of ED (Melnick, 2011). In patients with an organic etiology, the existence of concomitant psychological etiology, before the established medical condition or not, is possible, especially in patients under treatment for prostate cancer.
In patients with associated organic risk factors (smoking, diabetes, altered cholesterol levels, alcohol consumption, among others), guidance on lifestyle change is fundamental. In combination with organic investigation, the psychosexual anamnesis of patients with ED is a critical component of the differential diagnosis. Whenever possible, the participation of the partner should be suggested. A detailed history can capture how the patient faces his difficulty, as well as his expectations and needs (Rosen et al., 2002).
We can conclude that our study population had a predominance of ED in men aged over 50 and a high prevalence of organic ED. The study was conducted at the urology outpatient clinic of a high-complexity teaching hospital in a medium-sized city. As the hospital is a referral center for a large region of the state of São Paulo and neighboring states, patients in various stages of the disease are referred to this institution. Organic, psychological, and lifestyle factors associated with ED were identified, including unhealthy habits (e.g., smoking and alcohol consumption), advanced age, prostate cancer, premature ejaculation, depression, and anxiety, factors that have a great impact on self-esteem, quality of life, and interpersonal relationships, which makes ED an important public health marker.
Flaws in the annotations in the patients' medical records were found and show the need for professionals to improve their recording of information in medical records. Future studies on ED should identify the specific needs of this population. It is important to develop prevention and education plans aimed at men. The data demonstrate the importance of psychological evaluation associated with the medical diagnosis of ED in determining the proper treatment.
References
Abdo, C. H. N., & Afif-Abdo, J. (2012). Disfunção Erétil. In A. Carmita, Sexualidade Humana e seus transtornos (pp. 107-142). São Paulo: Leitura médica. [ Links ]
Abdo, C. H. N., Oliveira, W. M. Jr., Scanavino, M. T., & Martins, F. G. (2006). Disfunção Erétil: Resultados do estudo da vida sexual do Brasileiro. Revista Associação Médica Brasileira, 52(6),424-429. doi: 10.1590/S0104-42302006000600023 [ Links ]
Botega, N. J., Bio, M. R., Zomignani, M. A., Garcia, C. Jr., & Pereira, W. A. B. (1995). Transtornos do humor em enfermaria de clínicamédica e validação de escala de medida (HAD) deansiedade e depressão. Revista de Saúde Pública, 29(5),355-363. doi: 10.1590/S0034-89101995000500004 [ Links ]
Brotto, L., Atallah, S., Johnson-Agbakwu, C., Rosenbaum, T., Abdo, C., Byers, E. S., ... Wylie, K. (2016). Psychological and Interpersonal Dimensions of Sexual Function and Dysfunction. Journal of Sexual Medicine, 13,538-571. [ Links ]
Cavalcanti, R., & Cavalcanti, M. (2012). Disfunção Erétil. In R. Cavalcanti & M. Cavalcanti (Eds), Tratamento clínico das inadequações sexuais (pp. 251-286). São Paulo: Roca. [ Links ]
Colson, M. H., Cuzin, B., Faix, A., Grellet, L., & Huyghes, E. (2018). Erectile dysfunction, twenty years after. Sexologies, 27(1),1-6. doi: 10.1016/j.sexol.2018.01.016 [ Links ]
Gonzáles, A. I.,Sties, S. W., Wittkopf, P. G., Mara, L. S., Ulbrich, A. Z., Cardoso, F. L., & Carvalho, T. (2013). Validação do Índice Internacional de Função Erétil (IIFE) para Uso no Brasil. Arquivo Brasileiro de Cardiologia, 101(2),176-182. doi: 10.5935/abc.20130141 [ Links ]
Goulart, D. M. M. (2012). Qualidade de vida em pacientes submetidos à prostatectomia Radical (Master's Dissertation, Uberaba, MG, Universidade Federal do Triângulo Mineiro). Retrieved from http://bdtd.uftm.edu.br/handle/tede/170 [ Links ]
Heiden-Rootes, K. M., Salas, J., Gebauer, S., Witthaus, M., Scherrer, J., Mcdaniel, K., & Carver, D. (2017). Sexual dysfunction in primary care: An exploratory descriptive analysis of medical record diagnoses. The Journal of Sexual Medicine, 14(11),1318-1326. doi: 10.1016/j.jsxm.2017.09.014 [ Links ]
McCabe, M. P., & Althof, S. E. (2014). A systematic review of the psychosocial outcomes associated with erectile dysfunction: Does the impact of erectile dysfunction extend beyond a man's inability to have sex? Journal of Sexual Medicine, 11,347-363. [ Links ]
Melnik, T. (2011). Disfunção erétil. Revista Diagnóstico e Tratamento, 16(2),91-92. [ Links ]
Moreira, E. D. A. C., Glasser, D., Santos, D. B., & Gingell, C. (2005). Prevalence of sexual problems and related help-seeking behaviors among mature adults in Brazil: Data from the Global Study of Sexual Attitudes and Behaviors. São Paulo Medical Journal, 123(5),234-241. doi: 10.1590/S1516-31802005000500007 [ Links ]
Nguyen, H. M. T., Gabrielson, A. T., & Hellstrom, W. J. G. (2017). Erectile dysfunction in young men: A review of the prevalence and risk factors. Sexual Medicine Reviews, 5(4),508-520. doi: 10.1016/j.sxmr.2017.05.004 [ Links ]
Nicolosi, A., Laumann, E. O., Glasser, D. B., Moreira, E. D. Jr., Paik, A., & Gingell, C. (2004). Sexual behavior and sexual dysfunctions after age 40: The global study of sexual attitudes and behaviors. Urology, 64(5),991-997. doi: 10.1016/j.urology.2004.06.055 [ Links ]
Rajkumar, R. P., & Kumaran, A. K. (2015). Depression and anxiety in men with sexual dysfunction: A retrospective study. Comprehensive Psychiatry, 60,114-118. doi: 10.1016/j.comppsych.2015.03.001 [ Links ]
Reis, F., Netto, N. R. Jr., Reinato, J. A., Thiel, M., & Zani, E. (2004). The impact of prostatectomy and brachytherapy in patients with localized prostate cancer. International Urology and Nephrology, 36(2),187-190. doi: 10.1023/B:UROL.0000034686.55747.a5 [ Links ]
Rosen, R. C., Cappelleri, J. C., & Gendrano III, N. (2002). The International Index of Erectile Function (IIEF): A state-of-the-science review. International Journal of Impotence Research, 14(4),226-244. doi: 10.1038/sj.ijir.3900857 [ Links ]
Sarris, A. B., Nakamura, M. C., Fernandes, L. G. R., Staichak, R. L., Pupulim, A. F., & Sobreiro, B. P. (2016). Fisiopatologia, avaliação e tratamento da disfunção erétil: Artigo de revisão. Revista de Medicina, 95(1),18-29. doi: 10.11606/issn.1679 9836.v.95i1p18-29 [ Links ]
Yafi, F. A., Jenkins, L., Albersen, M., Corona, G., Isidori, A. M., Goldfarb, S., ... Hellstrom, W. J. G. (2016). Erectile dysfunction. Nature Reviews. Disease Primers, 2,16003. doi: 10.1038/nrdp.2016.3 [ Links ]
Zigmond, A. S., & Snaith, R. P. (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67,361-370. [ Links ]
 Correspondence:
Correspondence:
Maria Cristina de Oliveira Santos Miyazaki
Faculdade de Medicina de São José do Rio Preto-SP
Avenida Brigadeiro Faria Lima, 5.416, Vila São Pedro
São José do Rio Preto, SP, Brazil. CEP: 15090-000
E-mail: cmiyazaki@famerp.br
Submission: 05/02/2019
Acceptance: 06/25/2020
Authors notes
Pedro Junior R. Coutinho, Psychology Service (FUNFARME), Psychology Department (FAMERP) and Union of the Faculties of the Great Lakes (Unilago); Carmen Silvia C. E. Fernandes, Psychology Service (FUNFARME) and Psychology Department (FAMERP), Psychology Service at Hospital de Base; Fernando N. Facio Jr., Department of Surgical Specialties Faculty of Medicine of São José do Rio Preto (FAMERP) and Urology Service (FUNFARME); Maria Cristina de O. S. Miyazaki, Department of Psychology and Labo ratory of Psychology and Health Faculty of Medicine of São José do Rio Preto (FAMERP).














