Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Psicologia: teoria e prática
versão impressa ISSN 1516-3687
Psicol. teor. prat. vol.20 no.3 São Paulo set./dez. 2018
https://doi.org/10.5935/1980-6906/psicologia.v20n3p42-59
ARTICLES
PSYCHOLOGICAL EVALUATION
Scales assessing eating behavior in autism spectrum disorder
Escalas de evaluación del comportamiento alimentario de individuos con trastorno del espectro autista
Cristiane Pinheiro LázaroI; Jean CaronII; Milena Pereira PondéI
IBahia School of Medicine and Public Health - BAHIANA, BA, Brazil
IIMcGill University, Douglas Mental Health University Institute, Montreal, Quebec, Canada
ABSTRACT
Autism Spectrum Disorder (ASD) is characterized by impaired social interaction, impaired verbal and nonverbal communication, and repetitive, stereotyped, and restricted patterns of behavior and interests. Mealtime behavioral problems related to food refusal and selectivity were found to affect the health of this population negatively. A systematic literature review was conducted regarding existing evaluation instruments by searching PubMed, Cochrane, SciELO, Lilacs, Science Direct, and Embase databases using combinations of the following Keywords: autism, autism spectrum disorder, eating disorders, selective eating, eating behavior, food selectivity, eating problems, sensory processing disorders, questionnaire, evaluation, scale, inventory, and screening tool. Fifty-two studies were found, five of which met the inclusion criteria. The review identified significant methodological limitations in the studies and revealed the need for a new instrument to take the parents' views and the severity of the disorder into consideration.
Keywords: Autism Spectrum Disorder; scales; eating disorders; feeding behavior; ASD.
RESUMEN
El trastorno del espectro autista (TEA) se caracteriza por déficits en la interacción social, la comunicación verbal y no verbal, por un perfil de patrones de comportamiento repetitivos, estereotipados e intereses restringidos, y problemas de comportamiento durante las comidas, relacionados con la selectividad alimentaria. Para explorar el comportamiento alimentario en TEA se desarrolló una revisión sistemática de los instrumentos de evaluación en la literatura. Se realizó una búsqueda en PubMed, Cochrane, SciELO, Lilacs, Science Direct y Embase con la combinación de palabras clave: autismo, trastorno del espectro autista, trastornos de la alimentación, capricho para comer, comer, la selectividad de alimentos, problemas de alimentación, trastornos el procesamiento sensorial, cuestionario, la evaluación, la escala, la herramienta de seguimiento de inventario. Se encontraron 52 estudios de los cuales cinco satisfacían los criterios de inclusión, sin embargo, se encontraron limitaciones metodológicas en la obra publicada y la necesidad de desarrollar un nuevo instrumento.
Palabras clave: trastorno autista; escala; trastornos de la alimentación; trastornos de la alimentación; TEA.
Introduction
Children diagnosed with Autism Spectrum Disorder (ASD) present deficits related to reciprocal social interaction and verbal and non-verbal communication, as well as repetitive, stereotyped, and restricted patterns of behavior and interests (American Psychiatric Association, 2013). Other behavioral characteristics, such as anxiety, aggressiveness, and obsessive-compulsive responses, hyperactivity, attention deficit, and sleep disorders are also often reported (Novaes, Pondé, & Freire, 2008). In addition to these symptoms, parents and caregivers of children with ASD report peculiar eating behaviors (Lockner, Crowe, & Skipper, 2008). The intrinsic factors of foods may interfere in these children's eating behavior, such as the texture, color, flavor, form, and temperature of foods as well, as the format and color of packages, how the food is presented and utensils used (Mari-Bauset, Zazpe, Mari-Sanchis, Llopis-Gonzalez, & Morales-Suarez-Varela, 2013).
In parallel with the disorders' characteristics, children with typical development, aged between 18 and 24 months, tend to reject new flavors, which may lead to restricted and inadequate consumption of foods (Johnson, 2016). Such behavior, characterized by neophobia and part of typical child development, may be exacerbated in the context of ASD's restrictive behavior.
Refusing certain textures and trying new foods may significantly influence the habits of children with ASD (Bandini et al., 2010), resulting in selective eating behavior. Food selectivity may manifest in the refusal of certain foods, in a restricted repertoire of options or the frequent intake of a single food (Bandini et al., 2010). There is no consensus regarding the classification of food selectivity, but problems related to the intake of foods range from mild, in which behavior does not represent a risk to health, to more severe cases that lead to malnutrition (Hyman et al., 2012). In addition to the foods' intrinsic factors, ASD also presents a severe eating disorder called PICA, which is the recurrent intake of non-food substances or objects (e.g., paint, chalk, paper, dirt, coal, among others) (Call, Simmons, Mevers, & Alvarez, 2015).
Researchers investigating eating problems among people with ASD specifically report that a portion of this population also presents oral motor problems related to chewing and swallowing (Sacrey, Germani, Bryson, & Zwaigenbaum, 2014), gastrointestinal problems (Chaidez, Hansen, & Hertz-Picciotto, 2014), and sensorial dysfunction (Cermak, Curtin, & Bandini, 2010; Green & Ben-Sasson, 2010). Hypo and hyper-reactive problems related to sensorial modulation directly interfere with taste, smell, hearing, sight, touch, the vestibular system, and proprioception (Green & Ben-Sasson, 2010). Hence, sensorial, muscular and gastrointestinal alterations may directly or indirectly affect diet. Additionally, food selectivity may be associated with rigid and restricted interests that are characteristic of autistic behavior. Particularities of the eating behavior of people with ASD can be better investigated and classified using structured assessment instruments addressing the diversity of potential behaviors.
The need to better investigate the eating behaviors of individuals with ASD led some researchers to develop instruments that could be completed by parents or caregivers, in order to identify eating-behavior related information and variables. This study's objective was to perform a systematic review of the instruments assessing the eating behaviors of individuals with ASD available in the literature.
Method
Data search strategy
The search was performed in Brazilian and international scientific periodicals, including papers published up to 2015, using a combination of the following Keywords: Autism, Autism Spectrum Disorder, Eating Disorders, Selective Eating, Eating Behavior, Food Selectivity, Feeding Problems, Sensory Processing Disorders, Questionnaire, Evaluation, Scale, Inventory, and Screening Tool. Researchers with extensive experience in the treatment of ASD chose these descriptors. The search was conducted in the following databases: Pubmed, Cochrane, SciELO, Lilacs, Science Direct and Embase, Google Scholar, and grey literature (CAPES: http://bancodeteses.capes.gov.br/banco-teses/#/; The New York Academy of Medicine: http://www.nyam.org/library/collections-and-resources/grey-literature-report/).
Eligibility criteria
The following criteria were used: (1) papers published in English, Portuguese or Spanish; (2) instruments intended to assess problems related to the eating behavior of individuals with ASD. Papers written in other languages were excluded. The following information was extracted from eligible papers: (1) age groups; (2) study objective; (3) variables assessed. One of the researchers assessed the titles, abstracts or both.
Results
Screening according to these criteria resulted in 52 papers (Figure 1), 40 of which were excluded, either because they did not meet the inclusion criteria or appeared more than once. Of the 12 papers selected during the title and abstract screening, seven were excluded because they did not address assessment instruments. Three of the five papers included were conducted in the USA, one in Switzerland, and the other one in Canada, including children, youth, and adults with ASD, aged from 3 to 25 years old.
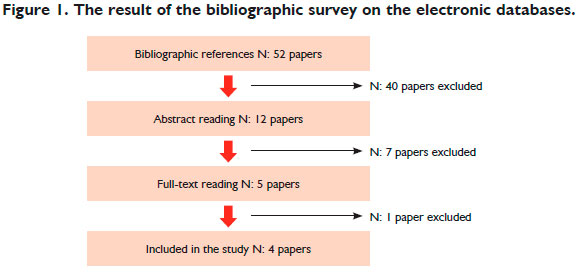
One of these papers was excluded because it did not focus on ASD. The characteristics of the studies included in this review are listed in Table 1 and described as follows:
Brief Autism Mealtime Behavior Inventory (BAMBI)
Lukens and Linscheid (2008) were the first to develop a scale intended to assess the nature of eating behavior problems among children with autism, called Brief Autism Mealtime Behavior Inventory (BAMBI). The sample was composed of 68 children with ASD and 40 children with typical development aged between 3-11 years old. Using a webpage, the children's caregivers were asked to complete: the BAMBI; the "Gilliam Autism Rating Scale" (GARS) (Gilliam, 1995), which is a scale that assesses the frequency and severity of behaviors among children with ASD; the "Behavioral Pediatric Feeding Assessment Scale" (BPFAS) (Crist & Napier-Phillips, 2001), which assesses the eating behavior of children; the "Youth/Adolescent Questionnaire" (YAQ) (Rockett et al., 1997), a questionnaire assessing food frequency; and a 24-hour food recall to estimate the average consumption of foods.
The BAMBI was based on the literature describing and assessing pediatric interventions directed toward autistic children with eating problems. The inventory initially contained 20 items addressing the behavior of children and was supposed to be completed by the caregivers. Each item contained five options, ranging from "never" to "always," in which the highest scores indicated more severe problems. The items were: cries or screams during meals; turns the face or body away from food; spits food; presents disruptive behavior during meals; closes the mouth tightly when food is presented; sits at the table until food is finished; is aggressive during meals; presents self-injurious behavior during meals; is flexible in regard to meal routines; refuses to eat foods that require much chewing; expects to try new foods; does not like certain foods and does not eat them; prefers to repeat the same food in all meals; prefers crunchy foods; accepts or prefers varied foods; prefers foods that are served in a certain way; prefers only sweet foods; prefers foods prepared in a particular way.
The preliminary version with the 20 items was submitted to psychometric analysis in a study with 50 participants (Lukens, 2002) and the analysis revealed a coefficient of 0.61 for the total scale, while factor analysis indicated three factors were responsible for 45% of the variance in the total score concerning the behavioral problem under study. Nine items were related to the factor "refuses foods/disruptive behavior" and corresponded to 20% of the variance. Five items were related to the factor "limited variety," with 18% of the variance. Five items related to the third factor, however, could not be interpreted. Thus, after the analysis, some items were removed, and a final version with 18 items remained.
The internal consistency of the final version with 18 items was 0.88 in the final sample, indicating three factors: "limited variety," "food refusal," and "autism characteristics," which had not appeared in the pilot study with 20 items.
To assess stability, the BAMBI was completed once again seven months later (interval: 5-13 months) with 31% of the initial sample. A test-retest reliability coefficient was calculated between the first and the second application of the inventory, presenting a significant r value (33) = 0.87, p < 0.01. In the inter-rater reliability assessment, eating behaviors assessed via the BAMBI and observed by teachers and caregivers were strong and positive with an r value (16) of 0.78, p < 0.01.
The BAMBI also presented positive correlations among the factors (limited variety, food refusal, autism characteristics) when assessing internal validity. Positive correlations were also found regarding convergent validity. The correlations were calculated between the BAMBI's total frequency score and the BPFAS' score, which assesses the frequency and severity of behaviors of children with ASD ("frequency of children' behavior" r (108) = 0.77, p < 0.01; "parents' feelings/strategies" r (108) = 0.74, p < 0.01; "BFAS total frequency" r (108) equal to 0.82, p < 0.01).
Correlations between individual factor scores and measures of external criteria were also calculated to verify concurrent validity, and the positive values suggest that the BAMBI properly explores the characteristics of autism described in the DSM-IV.
Regarding the BAMBI's discriminatory capacity, statistically significant differences were found using one-way ANOVA (p < 0.01) between the groups in terms of frequency of mealtime behavioral problems, with scores significantly higher for children with autism, compared to children with typical development.
Screening Tool for Feeding Problems (STEP-CHILD)
Seiverling, Hendy, & Williams (2011) developed the STEP-CHILD intending to measure eating problems among children. The authors used the "Screening Tool of Feeding Problems" (STEP) (Matson & Kuhn, 2001), a scale that assesses eating problems among adults with intellectual deficits. The STEP-CHILD was applied in a sample of 142 children aged 6.14 months, on average, 43 of whom had ASD, 51 presented other special needs, and 48 presented no developmental problems but experienced eating problems, all of whom were recruited in a clinic that specialized in eating problems. The parents initially completed the 23 items originally contained in the STEP, and each item refers to one eating characteristic. The items are rated on a three-point Likert scale (0 = absent; 1 = 1 to 10 times a month; and 2 = more than 10 times a month) to indicate the frequency with which children present behaviors. The parents also completed four items assessing problems related to food texture; one inventory addressing food preferences, the "Child Eating Behavior Questionnaire" (CEBQ) (Wardle, Guthrie, Sanderson, & Rapoport, 2001), which assesses eating problems among children; and the "Parent Mealtime Action Scale" (PMAS) (Hendy, Williams, Camise, Eckman, & Hedemann, 2009), which identifies the behaviors of parents and children during meals and the frequency in which parents eat and serve certain foods (such as fruits and legumes).
Factor analysis was used in the first version of the STEP-CHILD to determine its content and construct validity, establishing the items and subscales from the STEP version that would remain. The items of each dimension showed a loading factor of 0.40 a Cronbach's alpha of 0.55 or higher. Factor analysis revealed 15 items distributed into six dimensions: "chewing problems," "eating fast," "refusing food," "food selectivity," "vomiting," and "stealing foods." Internal reliability was assessed with an average Cronbach's alpha of 0.62 for the six subscales already noted.
Concurrent validity was assessed checking for correlations with instruments that had already been validated. Concurrent validity of the STEP-CHILD's six domains was obtained using multiple regression analysis between the CEBQ (Wardle, Guthrie, Sanderson, & Rapoport, 2001) and measuring of problems related to texture. The associations found in the subcategories were: "chewing problems," which was significantly correlated with texture-related problems (Beta: 0.445) and negatively correlated with being a picky eater (Beta: -0.229); "eating fast" was positively correlated with CEBQ's emotional excesses (Beta: 0.467) and negatively correlated with CEBQ's satiety response capacity (Beta: -.434); "food refusal" was positively correlated with being a picky eater from CEBQ (Beta: .296); "food selectivity" was positively correlated with texture-related problems (Beta: .406) and being a picky eater from CEBQ (Beta:.403); "stealing food" was positively correlated with the CEBQ's receptivity to foods (Beta: .442) and being a picky eater (Beta: .314). The subscale "vomiting" was not correlated with any of the factors.
To continue assessing external and construct validity, correlations with other measures were also verified, namely: the sample's demographic variables, anthropometry (BMI calculation), food preferences inventory, and the PMAS (Hendy, Williams, Camise, Eckman, & Hedemann, 2009). Association of the sample's demographic variables with the STEP-CHILD, which was verified using covariance analysis between sexes (boys and girls), age, and three diagnosed groups (children with autism, or with other special needs, and children with no special needs) was significant between the subscales "chewing problems" and age (p = 0.004), while younger children more frequently presented the problems (p = 0.008), and "stealing food" was associated with an ASD diagnosis (p = 0.012). Correlation with anthropometry (weight, height, and BMI) showed significance only with the subscale "eating fast" and with children with a high BMI (p < 0.001). A positive correlation was found concerning data collected with the food preference inventory between the dimension "food selectivity" and a limited variety of foods (p < 0.001). Finally, the results concerning the parents' attitudes during meals, measured by the PMAS (Hendy, Williams, Camise, Eckman, & Hedemann, 2009), revealed that the children who scored higher on the subscale "chewing problems" had parents who rarely limited snacks (p = 0.003); children who ate fast had parents who insisted they eat during meals (p = 0.004); and the parents of children who more frequently selected foods, more often prepared special meals different from those prepared for the remaining of the family and often offered foods their children preferred (p < 0.001).
Regarding the STEP-CHILD discriminatory capacity, the only information available referred to the positive correlation of the subscale "stealing food" with an ASD diagnosis (p = 0.012). "Stealing food" appeared more strongly associated with children with ASD when they were matched with a group of children with other special needs and a group with no special needs.
The Swedish Eating Assessment (SWEAA)
The third instrument identified was the "SWedish Eating Assessment" (SWEAA) (Karlsson, Rastam, & Went, 2013); these authors developed a multidimensional selfreported structured questionnaire with 81 items, based on a literature review and their own clinical experiences, to assess eating disorders in the context of ASD. The participants, aged between 15 and 22 years old, were randomly selected from a pediatric neuropsychiatric clinic of a hospital in Sweden. Of the 202 invited patients, 57 (28%) (males = 38; females = 19) completed the questionnaire. One expert assessed each of the participants, confirming the diagnosis and measuring their intelligence quotient (IQ). An inclusion criterion was that the participants should have an IQ within normal parameters to be able to complete the questionnaire themselves.
The subscales and corresponding items were developed using factor analysis together with Cronbach's alpha coefficient. The final version obtained after analysis retained 60 items comprising eight subscales: "perception," "motor control," "food purchases," "eating behavior," "meal environment," "social situation during meals," "other behaviors associated with eating disorders," and "hunger/satiety," all of which were assessed using a five-point Likert scale with options ranging from "never" to "always."
The SWEAA presented good internal consistency with values above 0.30 for all subscales and 0.40 for six of the eight subscales: "motor control," "food purchase," "mealtime," "social situation during meals," "other behaviors associated with eating disorders," "hunger/satiety." A Cronbach's alpha above 0.70 was observed in all subscales and 0.80 for six subscales: "perception," "motor control," "food purchase," "meal environment," "social situation during meals," and "other behaviors associated with eating disorders."
To assess temporal stability, the mean time between test-retest was 34 days with a good interclass correlation index (0.860), except for the subscale "hunger/satiety." The same test revealed a difference in the subscale "social situation during meals," but it was considered appropriate for the SWEAA due to a small difference presented at the two points in time.
In regard to discriminant validity, all the participants from the clinical group obtained the highest score on the subscale "social situation during meals," while statistically significant differences were found between those with ASD and the control group, not only in this subscale (p < 0.001), but also in the subscales "meal environment" (p < 0.017) and "simultaneous capacity" (p < 0.001), suggesting that these items are the main discriminators between groups.
Behavioral Pediatrics Feeding Assessment Scale (BPFAS)
The "Behavioral Pediatrics Feeding Assessment Scale" (BPFAS), developed by Crist & Napier-Phillips (2001), is a widely used instrument to assess eating behavioral problems in children. Allen et al. (2015) assessed the structure and validity of BPFAS with a sample of 374 preschoolers with ASD (314 were boys) aged 40.89 months on average. The participants were recruited through a longitudinal study using the following inclusion criteria: (1) recent diagnosis of ASD (within 4 months) as reported to the "Autism Diagnostic Observation Schedule" - ADOS (Lord et al., 2000), "Autism Diagnostic Interview-Revised" - ADI-R (Rutter, Le Couteur, & Lord, 2003) and a clinical assessment; and (2) age > 2 and < 5 years old and 0 months. Exclusion criteria were: (1) cerebral palsy or other neuromotor disorder that may interfere in the study's assessment; (2) known genetic or chromosomal anomaly; and (3) severe visual or auditory impairment.
The BPFAS is composed of 35 items: the first 25 items focus on the child's behavior, and the last 10 items provide an index of the parents' attitudes and strategies concerning eating habits, such as mealtime and eating problems. The parents indicated the frequency of behaviors on a five-point Likert scale where 1 = never and 5 = always; the higher the score, the more frequent the behavioral problems occur during meals.
In addition to the BPFAS, the researchers used other scales to verify association of the scale's factors with the variables that involved the behaviors of children and their caregivers: adaptive behavior (from birth to 18 years of age through the domains: communication, socialization, daily life skills and motor skills), using the "Vineland Adaptive Behavior Scales-Second Edition" (VABS-II) (Sparrow, Cicchetti, & Balla, 2005); the presence and intensity of various types of restrictive and repetitive behaviors that are characteristic of ASD, using the "Repetitive Behavior Scale-Revised" (RBS-R) (Bodfish, Symons, Parker, & Lewis, 2000); measurement of various symptoms, including social behavior and ASD traits, using the Social Responsiveness Scale (SRS) (Constantino & Gruber, 2005); children's behavior using the "Child Behavior Checklist" (CBCL) (Achenbach & Rescorla, 2000); sleep problems using the "Children's Sleep Habits Questionnaire" (CSHQ) (Goodlin Jones, Sitnick, Tang, Liu, & Anders, 2008; Owens, Spirito, & McGuinn, 2000); parental stress, using the "Parenting Stress Index-Short Form" (PSI-SF) (Abidin, 1995); symptoms and severity of ASD, using ADOS; level of indexed development, using the M-P-R (motor development, cognition and receptive language); language skills, using the "Preschool Language Scales-Fourth Edition" (PLS-4) (Zimmerman, Steiner, & Pond, 2002); and the child's age at the time the responsible adult completed the BPFAS.
Analyzing the internal consistency of the five factors of the BPFAS proposed by Crist & Napier-Phillips (2001), the scale in general (Cronbach's alpha = 0.82) and three factors showed acceptable coefficients: "picky eater" (Cronbach's alpha = 0.80), "toddler refusal-general" (Cronbach's alpha = 0.70), "children who delay eating" (Cronbach's alpha = 0.75), in contrast with "refuses foods with texture" (Cronbach's alpha = 0.26), "older child general refusal" (Cronbach's alpha = 0.3).
In regard to the construct's validity, factor analysis of the scale's items revealed that three factors represented 43.13% of variance and were labelled "food acceptance" (Cronbach's alpha = 0.71), "oral motor problems" (Cronbach's alpha = 0.71) and "behavior during meals" (Cronbach's alpha = 0.81).
In terms of construct validity, after factor analysis, three factors explained 43.13% of the variance and were labelled "food acceptance" (Cronbach's alpha = 0.71), "oral motor problems" (Cronbach's alpha = 0.71), and "behavior during meals" (Cronbach's alpha = 0.81).
To assess external validity, consequences of the construct and convergent validity, various positive correlations were found, with the effect ranging from small to moderate, among variables of interest involving the children, their parents, autistic symptoms verified with the application of other psychometric scales, and the three new factors noted above.
The factor "behavior during meals" presented six positive correlations of moderate effect: the parents who reported higher levels of autistic symptoms, according to SRS and RBS-R (e.g., social and communication problems, repetitive or restrictive behavior), also reported more problems with eating behavior (r = 0.34; 0.40 respectively). In regard to the behavior of children assessed by CBCL (internalization and externaliza-tion), moderate positive correlations were found for the factors "oral motor problems" (r = 0.44; r = 0.34), "behavior during meals" (r = 0.47; r = 0.48), and a slight correlation with "food acceptance" (r = 0.27; r = 0.20). Thus, children of parents who reported more frequent behavioral problems experienced more eating-related problems. On the other hand, only a slight negative correlation was found between the severity of ASD, as verified by ADOS, and the factor "behavior during meals" (r = -0.10). No important relationship was found between severity of ASD and "food acceptance" (r = 0.04) and "oral motor problems" (r = -0.06) was found.
Sleep problems reported to CSHQ presented moderate correlation with "behavior during meals" (r = -0.35) and low correlation with "food acceptance" (r = 0.19) and "oral motor issues" (r = -0.27). Parental stress assessed through PSI-SF showed moderate positive correlations with "oral motor problems" (r = 0.33) and "behavior during meals" (r = 0.38). Hence, the parents who reported their children as presenting frequent eating problems also reported their children to present many sleep-related problems and, as a consequence, the parents experienced higher levels of stress.
Low negative correlations between daily living skills and motor skills assessed through VABS-II were found between "food acceptance" (r = -0.22) and "oral motor issues" (r = -0.11), suggesting that the poorer a child's adaptive functioning, the more frequently s/he refuses food and presents oral motor problems.
No significant correlations were found between the child's age at the time the BPFAS was completed and cognitive functioning, assessed by the MPR, in regard to the factor "food acceptance" and "oral motor problems." Additionally, no significant correlations were found between the BPFAS and the child's language skills, measured by the PLS-4. Nevertheless, a low correlation was found between "behavior during meals" (r = -0.19), child's age, and cognitive level, indicating that the parents of older or more developed children reported higher levels of problem behavior during meals and more frequent eating-related problems.
Discussion
Adequate feeding during infancy, from birth and during the first years of life, is essential to ensuring a child's normal growth and development. Child growth is generally associated with bone growth that is reflected in height, but each of the organic systems is developing, including the central nervous system. The growth of the body as a whole depends on appropriate nutrition. Inadequate nutrition and malnutrition in the first and second phase of childhood may negatively affect child development, as overeating leads to obesity (Drewett, 2010). As a consequence, eating behavior in ASD is an important dimension because, in many cases, it may endanger the health of individuals. Accurate propaedeutic of the eating behavior of this population allows a more individualized and complex therapeutic approach. This paper presents an important contribution, as it presents a literature review of the instruments available to assess the eating behavior of children with ASD, identifying the limitations of existing instruments and proposing more appropriate and comprehensive alternatives regarding the diagnosis of ASD as it currently exists.
The BAMBI (Lukens & Linscheid, 2008) was the first instrument specifically developed to assess the eating problems of children with autism. The initiative to develop a specific scale was important and initiated the concept of measures that could discriminate between the problems presented by individuals with autism compared to those presented by children with typical development. This instrument focuses on eating-related behaviors, disregarding sensorial and gastrointestinal problems frequently found in ASD and that can influence one's eating behavior. The sample used to validate the instrument was composed of only 68 children with ASD, and the method presented some limitations: the participants' diagnoses were not established by a psychiatrist, but rather through a scale of symptoms completed by the caregivers; the investigation of eating problems did not consider the severity of ASD; the scale and remaining instruments used were posted on a webpage without the presence of someone to clarify potential doubts; the instrument was assessed using a convenience sample: the participants were those registered on a specific site, who consented to take part in the study. This last aspect specifically reveals an important limitation because the individuals who opted not to participate in the study may possibly differ in some ways from those included in the sample. Reliability analysis revealed high internal consistency for the factors "limited variety" and "food refusal"; however, the factor "autism characteristics" presented moderate consistency. In the assessment of temporal stability, less than half (31%) of the original sample completed the instrument a second time, an aspect that may have interfered in the result. Positive correlations between the BAMBI and a previously validated instrument that measures behavioral problems during meals were found. The differences between the groups' total scores obtained on the BAMBI support construct validity and correlations among factors, supporting its convergent validity. Specifically, the BAMBI's factor "limited variety" was negatively correlated with portions of beef, fruits, and vegetables, supporting the idea that children with ASD prefer unhealthy snacks and mainly carbohydrates (Ahearn, Castine, Nault, & Green, 2001).
In addition to behavioral aspects, the STEP-CHILD (Seiverling, Hendy, & Williams, 2011) assesses food selectivity, oral motor problems, eating-related skills, and food refusal. These elements allowed other intervenient factors in the eating dynamics of individuals with ASD to be mapped. Both studies, the BAMBI (Lukens & Linscheid, 2008) and the STEP-CHILD (Seiverling, Hendy, & Williams, 2011), showed rigorous psychometric criteria when they positively associated the subscales with clinical variables (weight, body mass index/BMI and limited variety of foods). Additionally, the STEP-CHILD (Seiverling, Hendy, & Williams, 2011) made an important contribution to the scientific literature, as it suggests that there is an association between the child's variables (weight and BMI) and those of the parents (parents' attitudes during meals) with increased eating problems. The parents' excessively permissive attitudes, such as not insisting the child eat during meals, or frequently preparing meals different from those prepared for the remaining members of the family, may influence eating problems among children. Hence, in addition to physiological and sensorial problems, factors linked to the parents' attitudes may also interfere in eating behaviors among those with ASD. Other studies also reinforce the importance of family dynamics to eating behaviors. Parents who are overweight and those who had problems controlling their own intake of foods (Birch & Davison, 2001) negatively influence the eating habits of their children (Hendrie, Sohonpal, Lange, & Golley, 2013; Scaglioni, Arrizza, Vecchi, & Tedeschi, 2011; Scaglioni, Salvioni, & Galimberti, 2008). Another contribution of the STEP-CHILD (Seiverling, Hendy, & Williams, 2011) was the introduction of the item "stealing food" as another behavioral aspect of ASD, which had been previously reported only in adults with special needs (Matson & Kuhn, 2001). Some limitations should be highlighted in regard to the STEP-CHILD (Seiverling, Hendy, & Williams, 2011). First, there was no significant correlation among all the factors. Additionally, the sample size was small, considering that only 43 of the 142 children who participated in the study had ASD; the scale did not widely explore sensorial or gastrointestinal problems or ritualistic and repetitive behaviors that are characteristic of the disorder, nor did it assess eating problems as a consequence of the severity of ASD. The paper does not clarify various aspects, such as: how the participants were recruited; how the diagnosis was established; whether the control group differed from the remaining participants; and did not mention assessments concerning the scale's temporal stability.
Even though the SWEAA (Karlsson, Rastam, & Went, 2013) presented good validity and internal reliability based on statistical parameters, the study did not consider the heterogeneity of the disorder. When a cutoff point for the participants' IQ was established, the researchers imposed an important limiting factor to the study and, as a consequence, the scale was predominantly tested (72%) among autistic individuals with high-performanceand Asperger's syndrome diagnosed prior to the Diagnostic Statistical Manual of Mental Disorders (DSM-V) (American Psychiatric Association, 2013). In regard to the factors assessed, this instrument assesses important topics related to eating behavior, such as motor control, the environment in which meals are served, ritualistic behaviors, social aspects at mealtime, and certain eating disorders, such as the desire to eat non-edible items (pica). Comorbidities associated with the disorder, such as depression, attention deficit disorder with hyperactivity (ADHD) and obsessive-compulsive disorder (TOC), were also investigated. However, gastrointestinal disorders and the severity of ASD were not verified. Some biases were found in the validation process, namely: adherence to the study and the sample size were small; only 28% of the individuals who were invited consented to participate in the study; education levels differed between the control and intervention groups; the IQ of the group with ASD was not measured, but was rather collected from medical records, while the IQ of the control group was not verified. There are other questionable particularities of the SWEAA, such as a minimum age of 15 years old. The authors themselves reported that the fact the questionnaire was a self-reported instrument and the fact there was no one to clarify potential doubts represented a disadvantage. Another potential limitation reported by the authors is that, in the scale's retest, most participants completed the questionnaire one year earlier than expected.
The BPFAS (Crist & Napier-Phillips, 2001) is a comprehensive measure widely used to detect eating behavioral problems based on competencies. It is a valid, reliable measure that efficiently discriminates between children with eating problems among populations with typical development and those with clinical problems. Even though the BPFAS (Crist & Napier-Phillips, 2001) was not properly validated, it has been used in studies involving ASD (Lukens & Linscheid, 2008; Martins, Young, & Robson, 2008), and in some cases as an instrument to assess the construct of other scales. Validation procedures and verification of the BPFAS' structure in an ASD sample (Allen et al., 2015) revealed inadequacy in the structure of five factors, while the factors "refusal of foods with texture" (Cronbach's alpha = 0.26) and "older child, general refusal" (Cronbach's alpha = 0.3) presented low internal consistency. The same occurred in other studies in which the sample of children had the diagnosis of chronic disease, were overweight or obese (Davis, Canter, Stough, Gillette, & Patton, 2014). In regard to the validation of the BPFAS' construct, the researchers found only a few correlations with a small to moderate effect. None of the three factors that remained after the factor analysis showed a strong correlation with the variables under study. Despite the fact it was developed to assess eating problems among 1- to 8-year-old children, the BPFAS (Crist & Napier-Phillips, 2001) did not take into account specific characteristics of ASD, such as sensorial problems or gastrointestinal disorders. Another point to highlight is that temporal stability was not assessed.
There are two aspects common among the instruments: all of them used the diagnosis according to the DSM-IV in the validation process, and none of them considered the eating-related complaints reported by the parents. The DSM-IV included under the heading Pervasive Developmental Disorders, autism, childhood disintegrative disorder, Asperger's syndrome, Rett syndrome, and pervasive developmental disorder not otherwise specified. The DMS-5, however, reflects the scientific view that these disorders (except for Rett syndrome and disintegrative disorder) are in reality the same condition, ASD, only with distinct symptomatic severity in relation to a deficit in communication and social integration and behavioral patterns, interests, and restricted and repetitive activities (American Psychiatric Association, 2013). Hence, new instruments to assess the eating behavior of children with ASD should contemplate different levels of these disorders as established by the DSM-5. Another aspect that is common to all the instruments found in the literature is that the starting point for asking questions is always the clinical experience of the professionals who develop the scale or scientific literature addressing the topic. None of the studies address what the parents of individuals with ASD consider to be problem-eating behavior. Therefore, we believe there is a need to develop an instrument that assesses the eating behaviors of people with ASD addressing these two aspects.
References
Abidin, R. R. (1995). Parenting stress index (3rd ed.). Odessa, FL: Psychological Assessment Resources. [ Links ]
Achenbach, T. M., & Rescorla, L. A. (2000). Manual for ASEBA preschool forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth & Families. [ Links ]
Ahearn, W. H., Castine, T., Nault, K., & Green, G. (2001). An assessment of food acceptance in children with autism or pervasive developmental disorder-not otherwise specified. Journal of Autism and Developmental Disorders, 31,505-511. doi:10.1023/A:1012221026124 [ Links ]
Allen, S. L., Smith, I. M., Duku, E., Vaillancourt, T., Szatmari, P., Bryson, S., Fombonne, E., Volden, J., Waddell, C., Zwaigenbaum, L., Roberts, W., Mirenda, P., Bennett, T., Elsabbagh, M., & Georgiades, S. (2015). Behavioral Pediatrics Feeding Assessment Scale in young children with autism spectrum disorder: psychometrics and associations with child and parent variables. Journal of Pediatric Psychology, 40,581-90. doi:10.1093/jpepsy/jsv006 [ Links ]
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM-V) (5th ed.) Washington, DC: American Psychiatric Association. [ Links ]
Bandini, L. G., Anderson, S. E., Curtin, C., Cermak, S., Evans, E. W., Scampini, R., Maslin, M., & Must, A. (2010). Food selectivity in children with autism spectrum disorders and typically developing children. The Journal of Pediatrics, 157,259-264. doi:10.1016/j.jpeds.2010.02.013 [ Links ]
Birch, L. L., & Davison, K. K. (2001). Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatric Clinics of North America, 48,893-907. doi:10.1016/S0031-3955(05)70347-3 [ Links ]
Bodfish, J. W., Symons, F. J., Parker, D. E., & Lewis, M. H. J. W. (2000). Varieties of repetitive behavior in autism: comparisons to mental retardation. Journal of Autism and Developmental Disorders, 30,237-243. doi:10.1023/A:1005596502855 [ Links ]
Call, N. A., Simmons, C. A., Mevers, J. E. L., & Alvarez, J. P. (2015). Clinical outcomes of behavioral treatments for pica in children with development disabilities. Journal of Autism and Developmental Disorders, 45,2105. doi:10.1007/s10803-015-2375-z [ Links ]
Cermak, S. A., Curtin, C., & Bandini, L. G. (2010). Food selectivity and sensory sensitivity in children with autism spectrum disorders. Journal of the American Dietetic Association, 110,238-246. doi:10.1016/j.jada.2009.10.032 [ Links ]
Chaidez, V., Hansen, R. L., & Hertz-Picciotto, I. (2014). Gastrointestinal problems in children with autism, developmental delays or typical development. Journal of Autism and Developmental Disorders, 44,1117-1127. doi:10.1007/s10803-013-1973-x [ Links ]
Constantino, J. N., & Gruber, C. P. (2005). Social responsiveness scale. Los Angeles: Western Psychological Services. [ Links ]
Crist, W., & Napier-Phillips, A. (2001). Mealtime behaviors of young children: a comparison of normative and clinical data. Journal of Developmental and Behavioral Pediatrics, 22,279-286. doi:10.1097/00004703-200110000-00001 [ Links ]
Davis, A. M., Canter, K. S., Stough, C. O., Gillette, M. D., & Patton, S. (2014). Measurement of mealtime behaviors in rural overweight children: an exploratory factor analysis of the Behavioral Pediatrics Feeding Assessment Scale. Journal of Pediatric Psychology, 39,332-339. doi:10.1093/jpepsy/jst089 [ Links ]
Drewett, R. (2010). Psicologia nutricional da infância (S. Vieira, Trad.). Curitiba: Ibpex. [ Links ]
Gilliam, J. E. (1995). Gilliam autism rating scale: examiner's manual. Austin, TX: Pro-Ed. [ Links ]
Goodlin Jones, B. L., Sitnick, S. L., Tang, K., Liu, J., & Anders, T. F. (2008). The Children's Sleep Habits Questionnaire in toddlers and preschool children. Journal of Developmental and Behavioral Pediatrics, 29,82-88. doi:10.1097/DBP.0b013e-318163c39a [ Links ]
Green, S. A., & Ben-Sasson, A. (2010). Anxiety disorders and sensory over-respon-sivity in children with autism spectrum disorders: is there a causal relationship? Journal of Autism and Developmental Disorders, 40,1495-1504. doi:10.1007/s10 803-010-1007-x [ Links ]
Hendrie, G., Sohonpal, G., Lange, K., & Golley, R. (2013). Change in the family food environment is associated with positive dietary change in children. International Journal of Behavioral Nutrition and Physical Activity, 10,4-11. doi:10.1186/1479-5868-10-4 [ Links ]
Hendy, H. M., Williams, K. E., Camise, T. S., Eckman, N., & Hedemann, A. (2009). The Parent Mealtime Action Scale (PMAS) development and association with children's diet and weight. Appetite, 52,328-339. doi:10.1016/j.appet.2008.11.003 [ Links ]
Hyman, S. L., Stewart, P. A., Schmidt, B., Cain, U., Lemcke, N., Foley, J. T., Peck, R., Clemons, T., Reynolds, A., Johnson, C., Handen, B., James, S. J., Courtney, P. M., Molloy, C., & Ng, P. K. (2012). Nutrient intake from food in children with autism. Pediatrics, 130,S145-153. doi:10.1542/peds.2012-0900L [ Links ]
Johnson, S. L. (2016). Developmental and environmental influences on young children's vegetable preferences and consumption. Advances in Nutrition, 7(1),220S-231S. doi:10.3945/an.115.008706 [ Links ]
Karlsson, L., Rastam, M., & Went, E. (2013). The SWedish Eating Assessment for Autism spectrum disorders (SWEAA) - validation of a self-report questionnaire targeting eating disturbances within the autism spectrum. Research in Developmental Disabilities, 34,2224-2233. doi:10.1016/j.ridd.2013.03.035 [ Links ]
Lockner, D. W., Crowe, T. K., & Skipper, B. J. (2008). Dietary intake and parents' perception of mealtime behaviors in preschool-age children with autism spectrum disorder and in typically developing children. Journal of the American Dietetic Association, 108,1360-1363. doi:10.1016/j.jada.2008.05.003 [ Links ]
Lord, C., Risi, S., Lambrecht, L., Cook, E. H., Jr., Leventhal, B. L., Di Lavore, P. C., & Rutter, M. (2000). The autism diagnostic observation schedule - generic: a standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30,205-223. doi:10.10 23/A:1005592401947 [ Links ]
Lukens, C. T. (2002). Assessing eating and mealtime behavior problems in children with autism. Unpublished master's thesis, The Ohio State University, Columbus, OH. [ Links ]
Lukens, C. T., & Linscheid, T. R. (2008). Development and validation of an inventory to assess mealtime behavior problems in children with autism. Journal of Autism and Developmental Disorders, 38,342-352. doi:10.1007/s10803-007-0401-5 [ Links ]
Mari-Bauset, S., Zazpe, I., Mari-Sanchis, A., Llopis-Gonzalez, A., & Morales-Suarez-Varela, M. (2013). Food selectivity in autism spectrum disorders: a systematic review. Journal of Child Neurology, 29,1554-1561. doi:10.1177/0883073813498821 [ Links ]
Martins, Y., Young, R. L., & Robson, D. C. (2008). Feeding and eating behaviors in children with autism and typically developing children. Journal of Autism and Developmental Disorders, 38,1878-1887. doi:10.1007/s10803-008-0583-5 [ Links ]
Matson, J. L., & Kuhn, D. E. (2001). Identifying feeding problems in mentally retarded persons: development and reliability of the screening tool of feeding problems (STEP). Research in Developmental Disabilities, 22,165-172. doi:10.1016/S0891-4222(01)00065-8 [ Links ]
Novaes, C. M., Ponde, M. P., & Freire, A. C. C. (2008). Control of psychomotor agitation and aggressive behavior in patients with autistic disorder: a retrospective chart review. Arquivos de Neuro-Psiquiatria, 66,646-651. doi:10.1590/S0004-282 X2008000500008 [ Links ]
Owens, J. A., Spirito, A., & McGuinn, M. (2000) The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep, 23,1043-1052. doi:10.1111/j.1746-1561.2009.00402.x [ Links ]
Rastam, M. (2008). Eating disturbances in autism spectrum disorders with focus on adolescent and adult years. Clinical Neuropsychiatry, 5,31-42. [ Links ]
Rockett, H. R. H., Breitenbach, M., Frazier, A.L., Witschi, J., Wolf, A. M., Field, A. E., & Colditz, G. A. (1997). Validation of a youth/adolescent food frequency questionnaire. Preventive Medicine, 26,808-816. doi:10.1006/pmed.1997.0200 [ Links ]
Rutter, M., Le Couteur, A., & Lord, C. (2003). Autism diagnostic interview revised. Los Angeles, CA: Western Psychological Services. [ Links ]
Sacrey, L. A., Germani, T., Bryson, S. E., & Zwaigenbaum, L. (2014). Reaching and grasping in autism spectrum disorder: a review of recent literature. Frontiers in Neurology, 5,1-12. doi:10.3389/fneur.2014.00006 [ Links ]
Scaglioni, S., Arrizza, C., Vecchi, F., & Tedeschi, S. (2011). Determinants of children's eating behavior. The American Journal of Clinical Nutrition, 94,2006S-2011S. doi:10.3945/ajcn.110.001685 [ Links ]
Scaglioni, S., Salvioni, M., & Galimberti, C. (2008) Influence of parental attitudes in the development of children eating behaviour. British Journal of Nutrition, 99,S22-S25. doi:10.1017/S0007114508892471. [ Links ]
Seiverling, L., Hendy, H. M., & Williams, K. (2011). The Screening Tool of Feeding Problems applied to children (STEP-CHILD): psychometric characteristics and associations with child and parent variables. Research in Developmental Disabilities, 32,1122-1129. doi:10.1016/j.ridd.2011.01.012 [ Links ]
Sparrow, S. S., Cicchetti, D. V., & Balla, D. A. (2005). Vineland adaptive behavior scales (2nd ed.). Livonia. MN: Pearson Assessments. [ Links ]
Wardle, J., Guthrie, C. A., Sanderson, S., & Rapoport, L. (2001). Development of the children's eating behavior questionnaire. Journal of Child Psychology and Psychiatry, 42,963-970. doi:10.1111/1469-7610.00792 [ Links ]
Zimmerman, I., Steiner, V., & Pond, R. (2002). Preschool language scale (4th ed.). San Antonio, TX: The Psychological Corporation. [ Links ]
 Mailling address:
Mailling address:
Cristiane Pinheiro Lázaro
Laboratório Interdisciplinar de Pesquisa em Autismo (LABIRINTO)
Av. Dom João VI, 275, Brotas
Salvador, Bahia, Brazil. CEP: 40290000
E-mail: lazarocris@hotmail.com
Submission: 28.09.18
Acceptance: 04.06.18
Author's note: This study was supported by a scholarship provided by FABESB (Bahia Research Foundation) # 029/2012 – PET: 0012/2013. The primary author received a Prosup/Capes scholarship.















