Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Estudos de Psicologia (Natal)
versão impressa ISSN 1413-294Xversão On-line ISSN 1678-4669
Estud. psicol. (Natal) vol.25 no.3 Natal jul./set. 2020
https://doi.org/10.22491/1678-4669.20200029
DOI: 10.22491/1678-4669.20200029
SOCIAL WORK PSYCHOLOGY
COVID-19: clinical and epidemiological indicators of mental health in frontline professionals – a systematic review of the literature
COVID-19: indicadores clínicos e epidemiológicos de impactos à saúde mental em profissionais da linha de frente – uma revisão sistemática de literatura
COVID-19: indicadores clínicos y epidemiológicos de los impactos en la salud mental en profesionales de primera línea – una revisión sistemática de la literatura
Rafaela Luiza TrevisanI,II; Mariana Bonomini Fogaça de AlmeidaI; Davi BaaschIII; Paola Barros DelbenI; Karen Rayany Ródio-TrevisanI,IV; Roberto Moraes CruzI
IUniversidade Federal de Santa Catarina
IISecretaria de Estado da Administração de Santa Catarina
IIIUniversidade do Estado de Santa Catarina
IVFaculdade CESUSC
ABSTRACT
Workers, who work on the front line to combat the COVID-19 pandemic, in special health professionals, are exposed to more risks of mental health problems. The objective of this article was to identify clinical and epidemiological aspects of the mental health of health workers, without facing COVID-19. A systematic literature review of articles published between January 1 and May 14, 2020, was carried out in the Web of Science, Scopus, Pubmed and Medline databases. 58 studies were selected, of which 10 empirical articles met all inclusion requirements. The research models involved, on the one hand, demographic and occupational variables and, on the other, mental health problems, as dependent variables, highlighting: depression, anxiety, fear, insomnia and medical symptoms. In the discussion, the main consequences for the mental health of the professionals stand out, as well as the coping and application strategies.
Keywords: health workers; COVID-19; mental disorders; frontline.
RESUMO
Os trabalhadores, que atuam na linha de frente de combate à pandemia da COVID-19, em especial profissionais de saúde, estão expostos a mais riscos de agravos à saúde mental. O objetivo desse artigo foi identificar aspectos clínicos e epidemiológicos da saúde mental de trabalhadores da saúde, no enfrentamento à COVID-19. Foi realizada uma revisão sistemática de literatura de artigos publicados entre 1 de janeiro a 14 de maio de 2020, nas bases de dados Web of Science, Scopus, Pubmed e Medline. Foram identificados 58 estudos, dos quais 10 artigos empíricos preencheram todos os critérios de inclusão definidos. Os modelos de pesquisa envolviam, de um lado, variáveis demográficas e ocupacionais e, de outro, agravos à saúde mental, como variáveis dependentes, destacando: depressão, ansiedade, medo, insônia e sintomas físicos. Na discussão destacam-se as principais consequências à saúde mental destes profissionais, bem como estratégias de enfrentamento e intervenções.
Palavras-chave: trabalhadores da saúde; COVID-19; transtornos mentais; linha de frente.
RESUMEN
Los trabajadores que trabajan en la primera línea para combatir la pandemia de COVID-19, en profesionales de la salud especiales, están expuestos a más riesgos de problemas de salud mental. El objetivo de este artículo fue identificar aspectos clínicos y epidemiológicos de la salud mental de los trabajadores de la salud, sin enfrentar COVID-19. Se realizó una revisión sistemática de la literatura de los artículos publicados entre el 1 de enero y el 14 de mayo de 2020 en las bases de datos de Web of Science, Scopus, Pubmed y Medline. Se seleccionaron 58 estudios, de los cuales 10 artículos empíricos cumplieron con todos los requisitos de inclusión. Los modelos de investigación incluyeron, por un lado, variables demográficas y ocupacionales y, por otro, problemas de salud mental, como variables dependientes, destacando: depresión, ansiedad, miedo, insomnio y síntomas médicos . En la discusión se destacan las principales consecuencias para la salud mental de los profesionales, así como las estrategias de afrontamiento y aplicación.
Palabras clave: trabajadores de la salud; COVID-19; desordenes mentales; primera línea,
On December 31, 2019, in Wuhan, China, cases of pneumonia with unknown etiology were reported (Huang et al., 2020; Li et al., 2020; World Health Organization [WHO], 2020a). The disease quickly spread across the country, arising as a global health emergency, and the new virus was called Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the etiological agent of Coronavirus Disease 2019 [COVID-19] (Lai et al., 2020). On March 11, 2020, the World Health Organization declared COVID-19 as a pandemic, when there were 118,319 confirmed cases worldwide (WHO, 2020a).
The overwhelming advance of the new virus exceeded 5,500,000 registered cases of the disease, and more than 550,000 deaths worldwide, in May 2020 (WHO, 2020b). The first case of COVID-19 in Brazil (and in Latin America), was disclosed on February 26, 2020 (Ministério da Saúde [MS], 2020a), although some reports mention positive records as early as January. Brazil is expected to become the new disease epicenter, with more than 430,000 cases and almost 27,000 deaths (MS, 2020b), ranking second in absolute numbers, just behind the USA, with 30% of world cases. Brazil is also the country with the highest number of daily deaths due to COVID-19, despite an important amount of underreporting and insufficient testing of the population, over 200 million people (European Centre for Disease Prevention and Control, n.d; WHO, 2020b).
Hence, there is an exponential spread of a new disease, with many questions still unanswered by science, such as the lack of knowledge about its course, the extent of effects, and the absence of vaccine/drugs to protect or cure exposed people (MS, 2020c). Given this critical scenario of emergency, uncertainty, and high probability of contamination, frontline workers, especially health professionals directly involved in the diagnosis, care, and treatment of patients, are at risk of showing symptoms of mental disorders (Lai et al., 2020), and tend to be one of the groups most affected by emotional, cognitive, and behavioral impairments (Brooks et al., 2020). Such disorders can lead to work leaves, functional disability, and even deaths, further reducing the number of staff needed to meet the demands of health services. There is a set of efforts by government authorities to make emergency contracts, move teams to less assisted communities and with higher levels of contamination, and advance graduations, among other measures, in order to strengthen coping with the public health crisis.
In 2003, in Asia, in face of the Severe Acute Respiratory Syndrome [SARS] epidemic, P. Wu et al. (2009) mentioned adverse psychological reactions among health professionals, with about 10% of employees reporting symptoms of Post-traumatic Stress Disorder [PTSD], with a persistence rate of 40% up to three years after the epidemic outbreak. The health and social problems caused by SARS, as well as work overload, unleashed feelings of vulnerability, helplessness, loss of control, uncertainty, and life threat in many frontline workers. Some showed somatic, depressive, and anxiogenic symptoms, together with difficulties for interpersonal relationships, in addition to a psychiatric morbidity rate three times higher when compared to the general population (Chong et al., 2004).
Fear of contamination, or of contaminating close people, was also an important stress factor, especially among health workers (Brooks et al., 2020; Rocha, Freire, Reis, Vieira, & Sousa, 2020), because unlike what is asked to the majority of the population – to stay at home -, health professionals and of other essential services need to do the opposite. Given this context, the campaign "We stay here for you, please stay home for us" went viral, repeated in several languages by teams working in hospitals. Therefore, in addition to concerns about their personal safety, they also fear contamination of their family members and colleagues, cope with stigmas and prejudice, hostility, and even aggressiveness, in contrast to the recognition and tributes to the "heroes in white".
In Brazil, there are over six million health professionals, three million only in the Unified Health System [SUS], 75.75% in healthcare functions and 24.25% in administrative functions. Indicators on exposure to contagion, lethality, and morbidity by COVID-19 among these professionals are still being processed. National data published so far show that between 4 and 12% of health professionals will be infected; that is, considering only SUS professionals, there will be between 122 thousand and 365 thousand workers away from work due to contagion, illness, or death by the disease (MS, 2020c). The group of health workers is at high risk of infection, since its activities put them routinely on the frontline in assisting suspected and confirmed cases. In addition, estimates show that between 8% and 12% of them might be prevented from exercising the profession due to mental health impairments, together with those on leave by physical health issues.
The relevance and number of health professionals, in the pandemic scenario, indicate the need to collect evidence on their mental health, especially for providing contingency plans and mobilizing efforts for prevention, besides targeting resources for specialized intervention. This article aims to identify the clinical and epidemiological aspects of the mental health of frontline health workers in coping with COVID-19, through a systematic literature review.
Method
Our literature review covered articles published between January 1st and May 14, 2020. We accessed international journals and defined the inclusion criteria, such as empirical articles, full texts, and peer-reviewed, with the following terms in the title:
Line 1: COVID OR Sars-Cov OR Coronavirus;
Line 2 (AND): employee OR worker OR servant OR military OR "front line" OR front-line OR physician OR medical OR frontline OR healthcare OR caregiver OR staff OR professional OR service OR actor OR agent OR practitioner OR nurse OR medic OR nursing;
Line 3 (AND): "mental health" OR psychological OR "mental disorder" OR panic OR depression OR stress OR strain OR suicide OR post traumatic OR anxiety.
We accessed the following databases (access through a public university's VPN): Medline, PubMed, Scopus, and Web of Science. The flowchart in Figure 1 describes the steps and results of each stage:
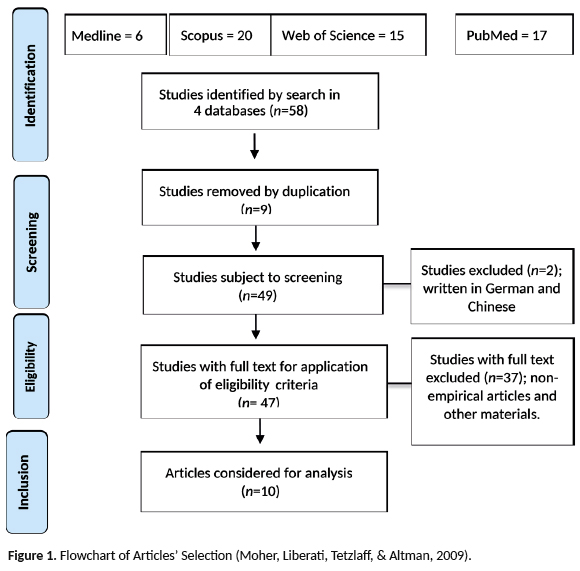
We examined the articles according to the following guidelines: a) identification of the article: journal, authors and date of publication; b) methodology: objective, origin (country/region of data collection, variables (independent and dependent), data collection methods (instruments and techniques used, approach), analysis methods, sample size, main results, and limitations. These criteria were means of guidance for an initial description and analysis of the subject, aiming at a future deepening of the studies, in order to understand clinical and epidemiological aspects of the mental health of health workers, at the frontline of the fight against COVID -19, especially in Brazil.
Results
The 10 articles analyzed had 122 authors, among 100 different names, and an average of 12.2 authors per article. They were published in nine journals: Brain, Behavior, and Immunity; Medical Science Monitor; JAMA Network Open; Psychiatry Research; Journal of Nursing Management; International Journal of Nursing Sciences; American Journal of Infection Control; Journal of Medical Virology; and Frontiers in Psychiatry.
Data collection for the referred studies were carried out in hospitals that received patients with COVID-19. Three studies gathered data from only one institution: Tertiary General Hospital - Wuhan, Fujian Provincial Hospital, and Henan's First Affiliate Hospital - University of Science and Technology. Another study did not mention where data collection took place, but declared that working in Wuhan was the condition for participating in the research, with the approval of the Ethics Committee for Clinical Research, of the Wuhan University's Renmin Hospital.
In one article, all cities in the Province of Hunan, where data were collected, appeared on an explanatory map, approved by the Ethics Committee of the 3rd Xiangya Hospital, at Central University of the South. One of the surveys collected data from 180 nurses, at Guangxi City, who assisted Wuhan during the COVID-19 pandemic, and another collected data from 34 hospitals, with 60.5% of the participants working in Wuhan. One study comprised hospitals and universities in Wuhan and in areas outside the city; and another called for the participation of professionals from hospitals all over China; in that case, the Ethics Committee of the Nanfang Hospital, at Southern Medical University, approved it. Only one study collected data outside China - in India and Singapore, in the five major hospitals that received COVID-19 patients.
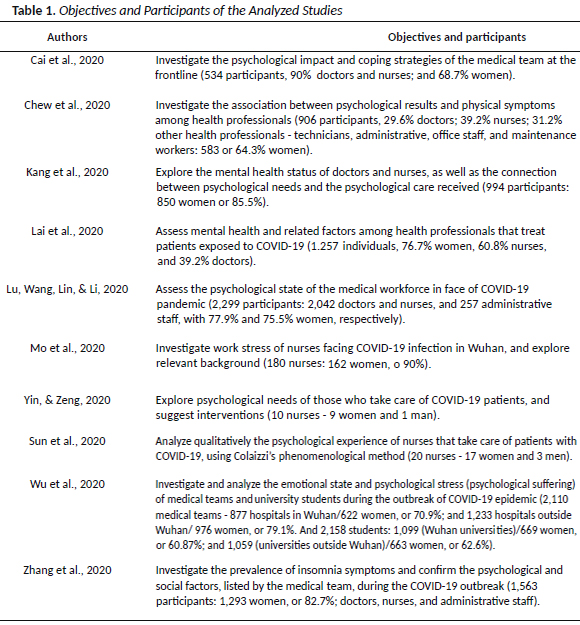
The articles were mainly descriptive (4), addressed associations (5), and only one presented proposals for interventions. As for the samples, doctors and nurses comprised the majority of participants. Table 1 describes the objectives and samples' specificities.
In the eight articles that adopted a quantitative approach, the participation of women prevailed, with percentages above 60%; and even in the qualitative studies, the number of female participants was higher. It would be necessary to know the general profile and population of the three countries included in the studies, where the samples of participants were taken from, in order to determine if the predominance of women related directly to those data, or even to formulate other hypotheses. Considering the short time for data collection, quantitative surveys achieved expressive sample sizes (average of 1,500.1 participating workers).
The reviewed publications adopted analysis models that mostly addressed demographic variables (gender, age or education level, family status) and occupational variables (professional category, service time, type of occupation, and level of exposure) as independent variables. And mental health problems (emotions/feelings or psychological suffering, personal coping strategies, motivational factors, stress, insomnia or sleep quality, depression, anxiety, fear or trauma, physical or general symptoms, or those related to breathing) as dependent variables. Qualitative studies related demographic and occupational variables to the psychological needs of nurses, and to four phenomenological topics.
For data collection, surveys used their own or adapted questionnaires, and mental health scales validated by specific literature. Six of the ten instruments used are validated in Brazil:
1) Depression Scales for Anxiety and Stress (DASS-21) (Vignola, 2013; Vignola & Tucci, 2014), used in one study;
2) Hamilton Anxiety Scale (HAMA) and Hamilton Depression Scale (HAMD) (Freire et al., 2014), also used in a study;
3) Impact of Events Scale-Revised (IES-R) (Silva, Nardi, & Horowitz, 2010), used in four of the ten articles analyzed;
4) Patient Health Questionnaire 9 - item depression module (PHQ-9) (Caputo & Menezes, 2016; Santos et al., 2013);
5) Generalized Anxiety Disorder (GAD) or GAD-7 - translated into Portuguese by Pfizer (Copyright © 2005, Pfizer Inc., New York, NY), with registration of evidence of validity in Brazil - Mapi Research Institute (2006) (Bergerot, Laros, & Araujo, 2014); and
6) Insomnia Severity Index (ISI) (Castro, 2011).
These last three instruments were used to make up the data collection method for three studies.
The studies also used different strategies for data analysis. The eight quantitative studies used descriptive statistics. Other strategies used in these articles were: Student's t; Chi-square; Odds Ratios; Multiple logistic regression; Linear regression; Cluster analysis and Structural Equation Modeling (SEM); Mann – Whitney U test and Kruskal – Wallis H test for independent samples, and Mann – Whitney U test; Correlations and ANOVA; Bonferroni correction. Both qualitative articles used in-depth interviews (Yin & Zeng, 2020) and Colaizzi's phenomenological method (Sun et al., 2020).
Discussion
Since it is the pandemic's country of origin, all studies were done in China, except for one - carried out in close countries, in a scientific collaboration (India and Singapore). An immediate production of Chinese studies was expected, given the short time since the emergence of the disease, its magnitude, and the notification of the initial outbreak in China. The other countries, once affected, have conducted important studies; however, the majority in the form of brief communications, letters to the editors, editorials, and preliminary results, which were not peer-reviewed or are in the process of publication, in addition to others that will certainly be published in the short, medium and long term.
As observed in studies referring to the SARS epidemic in 2003 (Chong et al., 2004; P. Wu et al., 2009), adverse emotional reactions, such as anxiety, depression, feelings of helplessness and vulnerability, or somatic symptoms, are frequent in frontline health professionals of the COVID-19 pandemic. Confirming findings from previous studies, almost a third of the professionals in a medical team had moderate to severe emotional disorders, especially young women (Kang et al., 2020) and those who worked in Wuhan, the first pandemic epicenter. Health professionals showed more severe degrees in all measures of mental health symptoms, when compared to workers outside the province of Hubei (Lai et al., 2020), and to university students (W. Wu et al., 2020).
The medical teams from Wuhan, and from outside the region, when compared to university students, showed significantly higher results for all items of the Psychological Stress Questionnaire (QEP) and for poor sleep quality, with the worst scores among professionals from Wuhan and region. These also showed cognitive impacts and negative emotions, related to the "exposure effect", that is, for being at the front, under great work and psychological pressure (W. Wu et al., 2020).
These workers involved in the diagnosis, treatment, and care of patients with COVID-19 had a higher risk of symptoms of depression, anxiety, insomnia, and stress (Lai et al., 2020). Among the clinical and epidemiological aspects of frontline workers' mental health, the following stand out: concerns about personal safety, their families' safety, patients' mortality, and inadequacy, or even the lack of personal protective equipment (PPE) (Cai et al., 2020; W. Wu et al., 2020; Yin & Zeng, 2020; Zhang et al., 2020).
There was also a significant association between the prevalence of physical symptoms and psychological results in these professionals. Evidence of depression, anxiety, stress, and psychological distress (from moderate to very severe levels) has been associated with physical symptoms, with headache being the most common (Chew et al., 2020). Poor sleep quality (difficulty of sleeping, waking up easily, nocturnal behavior, like turning around a lot), as well as insomnia, were also symptoms mentioned by workers (Lai et al., 2020; Zhang et al., 2020).
These were the risk factors for insomnia, related to COVID-19 epidemic: low educational level, working in an isolation unit, concern about being infected, perception of inefficient psychological support (news and social media), and extreme uncertainty regarding the effective control of the disease. The team that worked in an isolation unit was 1.71 times more likely to experience insomnia (Zhang et al., 2020).
In addition to these factors, Cai et al. (2020) mention exhaustion, due to long working hours, and the extra biosafety procedures required before and after a potential exposure to the virus, which enhance a state of hypervigilance (Barros-Delben et al., 2020). Zhang et al. (2020) describe the new work routine: it is necessary to stay with PPEs (masks, gloves, coats, and glasses) for more than 12 hours, and to avoid being infected you cannot eat, drink, or use the bathroom during work, because there are insufficient human resources, and they are expensive and essential. Many even get dehydrated from excessive sweating, and develop cystitis or skin rashes. In addition to these conditions, they keep close contact with suspicious or infected cases. Under such conditions, the medical team is exhausted, physically and mentally. Fatigue and a feeling of impotence in the face of the epidemic (W. Wu et al., 2020) were also mentioned among the clinical and epidemiological aspects of frontline workers' mental health.
Regarding other health professionals, doctors and nurses were unhappier with overwork during the COVID-19 outbreak. Nurses were more concerned with financial compensation, during or after the epidemic, and felt more nervous and anxious (Cai et al., 2020). Compared to doctors, nurses were more prone to insomnia due to higher stress levels, which indicates a higher workload, added to the fact that they commonly work on night shifts and have a more direct contact with patients (Zhang et al., 2020). Among nurses, stress was mainly related to three factors: the history of being an only child, hours worked per week, and anxiety (Mo et al., 2020), which highlights the cultural specificities involved. When frontline workers were compared to the non-clinical team, direct contact with infected patients was related to 1.4 times more chance of being afraid and twice the chance of suffering from anxiety and depression (Lu et al., 2020).
With regard to nurses' psychological needs, Yin & Zeng (2020) observed, in addition to (1) general health and safety necessities, (2) needs related to relationship. a) With the community itself, given that they required care, support from management and from the outside world; b) with family, friends, and colleagues, meaning a desire for close interpersonal relationships; and c) family affection, temporarily eliminated by the epidemic, became stronger than usual. Finally, the (3) need for growth or development, expressed as a strong need to know about prevention and control of COVID-19, especially from official reports. These three central needs coexist and interact with each other, converging to nurses' health needs.
Given the current situation and working scenario, so adverse and challenging - including in Brazil, with the necessary considerations and adaptations -, and in view of the psychological needs, described in the aforementioned study, along with the presented clinical and epidemiological aspects of health workers' mental health, it is possible to outline strategies and directions to improve their health and well-being.
Self-control and psychological growth are important traits to keep mental health (Sun et al., 2020), and must be strengthened in professionals that work in epidemics such as COVID-19. Among the findings of this review, ensuring family safety was the factor with greatest impact in reducing stress (Cai et al., 2020). Support from family, friends, and co-workers, as well as a positive attitude within the work team were also significant (Cai et al., 2020; W. Wu et al., 2020). Correct guidance and effective caution to prevent disease transmission have decreased anxiety among female workers (Cai et al., 2020).
It is important to comply with protection measures; to know about the use of PPEs, about virus prevention and spread; and about social isolation measures. These health strategies result in adapting to the new work routine, as well as in exhaustion; both are part of the clinical and epidemiological aspects of mental health. The more trained a professional is, the better he deals with the demands of the job, mobilizing perception, memory, and ability for reasoning. Furthermore, in times of health emergency (Rego & Palácios, 2020), there are some essential measures to take: seek qualification for understanding the disease and incorporating biosafety procedures; establish limits for the work routine; try not to feel guilty about patients that could not be saved; do not work long hours alone; rest; practice physical activity; diet; look out of the window; take a deep breath; and seek constructive feedback from patients (W. Wu et al., 2020).
Frontline professionals mentioned social and moral responsibility as a reason to keep on working, and hoped to receive recognition from hospital and government authorities (Cai et al., 2020). It is worth mentioning the countless honors they have received for their work during the pandemic, in Italy, Spain, Israel, India, USA, and Brazil, among others (Health Management, 2020; Oliva, 2020; Pandey & Sharma, 2020; WHO, 2020c). This appreciation is important to motivate their practice and improve mental health.
According to W. Wu et al. (2020), the feeling of trust, a relevant factor in this context, was higher in medical teams, when compared to university students. Although they were more exposed, they counted on strong preventive and control measures, unrestricted support from people across the country, patients' improvement, and decreasing numbers of cases. Thus, with knowledge for understanding the epidemic, professionals were able to strengthen their energy and confidence for work.
The need to keep on working on intense journeys, the difficulty of adapting to the use of PPEs for the prevention of contagion by the virus, as well as the perception that colleagues start to get sick have led professionals to present signs and symptoms of fatigue. Therefore, in order to avoid illness and absence from work, some strategies have emerged. To reduce physical and mental workload (anguish, fear, feeling of displeasure or discomfort), such as alternative transport schemes; articulation with hotels and inns to accommodate these workers - even assisting in their families' safety; providing objective safety conditions (PPEs); providing spaces for sharing experiences; encouraging the formation of online groups with their peers, to think about ways of organizing work, reducing queues, creating new flows, resizing spaces, and giving due attention to work routines, with regular breaks for rest; and information on mental health in times of pandemic (Rego & Palácios, 2020). An unusual scenario imposes unusual solutions as well.
Mental health care services, although limited, were important strategies to alleviate emotional losses and improve perceptions on physical health (Kang et al., 2020). However, Chinese medical teams are less prone to seek help from psychologists or express their emotions, when compared to Western countries' teams (Cai et al., 2020), due to their cultural attributes. Access to psychological materials, like books on mental health, psychological resources available online (motivational messages related to methods of self-care and coping with mental health), and counseling or psychotherapy were the strategies reported to meet the psychological needs and care received (Kang et al., 2020).
In Brazil, a large number of psychologists have volunteered for free online assistance to mental health care, for both frontline professionals and the general population affected by COVID-19. They named the initiative "everything will be fine". In addition to groups of volunteer professionals, platforms were created to connect psychologists and clients (Consiglio, 2020; Instituto de Psicologia – USP, 2020; Rede de Apoio Psicológico [Psychological Support Network], n.d; Simon, 2020).
Final remarks
Frontline health workers showed more serious emotional disorders compared to non-clinical teams and the general population. Symptoms frequently mentioned were depression, anxiety, fear, insomnia, stress, and physical symptoms. Concern with their personal safety and their families', in the face of COVID-19 pandemic, was the most important stress factor. They also mentioned worry about patient mortality, inappropriate or lack of PPEs, exhaustion, and work overload.
Among the factors that contributed to minimize stress were protection measures, knowledge about virus prevention and transmission, measures of social isolation, confident attitude, positive attitude from colleagues, support from family and friends, in addition to mental health care. Social and moral responsibility established the purpose of continuing to work through the epidemic chaos, and recognition proved to be something expected and favorable to these workers' mental health.
Mental health services, although limited, were relevant in alleviating emotional damage. Books, online resources, and psychotherapy were suggested strategies. Thus, we emphasize the relevance of this additional type of access, at risk of further harming workers in such a situation. The insufficient number of professionals to deal with mental health in the workplace can increase the risk of emotional damage in distressed professionals, and still cause disorders to those emotionally "integrated" workers, who would welcome this demand even in a context of huge work overload.
As limitations of this review, we recall that all studies were done in China, except for one (in nearby countries). Therefore, comprising only Asian workers is a restriction for applying these results to other countries' reality. On the other hand, such studies can serve as a basis for similar research, addressing workers' populations from other countries, who are at the frontline of COVID-19, such as Brazilian workers, since there are no empirical studies published in the country. In other words, Chinese studies can guide Brazilian research. We highlight that other sources of evidence confirm the mental health conditions of professionals in situations of epidemics, as shown in the study.
We also mention the massive participation of women in the samples, as well as the predominance of large-scale quantitative studies. There are more quantitative studies, national and international, and those that deal with illness due to mental disorders, or address their relationship with work, often identify a higher prevalence of these emotional disorders among women. The number of studies, which grows exponentially, also reflects the speed and magnitude of the pandemic. The short-term period considered in this review is also a limitation. However, we can later update it, for further deepening.
By being atypical, compared to other emergencies and disasters already experienced in Brazil and across the world, it is difficult to measure the effects and damages of COVID-19 pandemic. Even so, we notice the movement of researchers for exchanging knowledge, searching for a basis to design intervention projects related to the pandemic, its risks, consequences, possibilities of prevention, and coping with vulnerabilities.
This article sought to analyze clinical and epidemiological evidence of mental health disorders experienced by health professionals, regarding the COVID-19 pandemic. The analysis of this evidence allows highlighting concerns and efforts to avoid contamination and mitigation of its effects, as well as the need to minimize traumatic situations through the organization of health care services, aiming to offer support, welcome, and follow-up of health professionals affected by the pandemic.
References
Barros-Delben, P., Cruz, R. M., Trevisan, K. R. R., Gai, M. J. P., Carvalho, R. V. C., Carlotto, P.A.C., ... Malloy-Diniz, L. F. (2020). Saúde mental em situação de emergência: COVID-19. Revista Debates in Psychiatry, 10, 2-12. doi: 10.25118/2236-918X-10-2-3 [ Links ]
Bergerot, C. D., Laros, J. A., & Araujo, T. C. C. F. (2014). Avaliação de ansiedade e depressão em pacientes oncológicos: comparação psicométrica. Psico-USF, 19(2), 187-197. doi: 10.1590/1413-82712014019002004 [ Links ]
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, J. G. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence (2020). The Lancet, 395(10227), 912-920. doi: 10.1016/S0140-6736(20)30460-8 [ Links ]
Cai, H., Tu, B., Ma, J., Chen, L., Fu, L., Jiang, Y., & Zhuang, Q. (2020). Psychological impact and coping strategies of frontline medical staff in Hunan between january and march 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Medical Science Monitor, 26:e924171-16. doi: 10.12659/MSM.924171 [ Links ]
Caputo, L. M. C., & Menezes, P. R. (2016). Validação do Patient Health Questionnaire-9 (PHQ-9) para a população idosa brasileira (Research Project - Undergraduate Research Fellowship Program, Universidade de São Paulo, Faculdade de Medicina, São Paulo). Retrieved from https://bv.fapesp.br/pt/bolsas/157355/validacao-do-patient-health-questionnaire-9-phq-9-para-a-populacao-idosa-brasileira/ [ Links ]
Castro, L. S. (2011). Adaptação e validação do Índice de Gravidade de Insônia (IGI): Caracterização populacional, valores normativos, aspectos associados (Master's thesis). Retrieved from http://repositorio.unifesp.br/handle/11600/23193 [ Links ]
Chew, N. W. S., Lee, G. K. H., Tan, B. Y. Q., Jing, M., Goh, Y., Ngiam, N. J. H., ... Sharma, V. K. (2020). A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behavior, and Immunity, 88, 559-565. doi: 10.1016/j.bbi.2020.04.049 [ Links ]
Chong, M-Y., Wang, W-C., Hsieh, W-C., Chong, M-Y., Wang, W-C., Hsieh, W-C., ... Chen, C-L. (2004). Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. British Journal of Psychiatry, 185(2), 127-133. doi: 10.1192/bjp.185.2.127 [ Links ]
Consiglio, M. (2020, April 08). Psicanalistas oferecem atendimento gratuito online, saiba onde encontrar. Folha de São Paulo. Retrieved from https://www1.folha.uol.com.br/equilibrioesaude/2020/04/psicanalistas-oferecem-atendimento-gratuito-online-saiba-onde-encontrar.shtml [ Links ]
European Centre for Disease Prevention and Control (n.d). COVID-19 situation update worldwide, as of week 10, updated 18 March. Retrieved March, 24, 2021, from https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases [ Links ]
Freire, M. A., Figueiredo, V. L. M., Gomide, A., Jansen, K., Silva, R. A., Magalhães, P. V. S., & Kapczinski, F. P. (2014). Escala Hamilton: estudo das características psicométricas em uma amostra do sul do Brasil. Jornal Brasileiro de Psiquiatria, 63(4), 281-289. doi: 10.1590/0047-2085000000036 [ Links ]
Health Manangement (2020, March 18). Top 5 Tributes to COVID-19 Healthcare Staff from Around Globe. Retrieved from https://healthmanagement.org/c/hospital/news/top-5-tributes-to-covid-19-healthcare-staff-from-around-globe [ Links ]
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., ... Cao, B. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet, 395(10223), 497-506. doi: 10.1016/S0140-6736(20)30183-5 [ Links ]
Instituto de Psicologia – USP. (2020). Serviço de atendimento psicológico online em função da pandemia COVID-19. Retrieved from http://www.ip.usp.br/site/servicos-a-comunidade/ [ Links ]
Kang, L., Ma, S., Chen, M., Yang, J., Wang, Y., Li, R., ... Liu, Z. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain, Behavior, and Immunity, 87(5), 11-17. doi: 10.1016/j.bbi.2020.03.028 [ Links ]
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., ... Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e203976. doi: 10.1001/jamanetworkopen.2020.3976 [ Links ]
Li, Q., Guan, X., Wu, P., Wang, X. , Zhou, L. Tong, Y., ... Feng, Z. (2020). Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. The New England Journal of Medicine, 382(13), 1199-1207. doi: 10.1056/NEJMoa2001316 [ Links ]
Lu, W., Wang, H., Lin, Y., & Li, L. (2020). Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Research, 288(112936), 1-5. doi: 10.1016/j.psychres.2020.112936 [ Links ]
Mapi Research Institute. (2006). Certificate of linguistic validation certificate: General anxiety disorder-7 (GAD-7). Lyon: Mapi Research Institute. [ Links ]
Ministério da Saúde. Secretaria de Vigilância em saúde. (2020a). Centro de operações em emergência em saúde pública. Boletim epidemiológico especial COE-COVID19. Retrieved from https://portalarquivos.saude.gov.br/images/pdf/2020/April/27/2020-04-27-18-05h-BEE14-Boletim-do-COE.pdf [ Links ]
Ministério da Saúde. (2020b). Painel de casos de doença pelo coronavírus 2019 (COVID-19). Retrieved from https://covid.saude.gov.br/ [ Links ]
Ministério da Saúde. Conselho Nacional de Saúde. (2020c). Recomendação nº 020, de 07 de abril de 2020. Recomenda a observância do Parecer Técnico nº128/2020, que dispõe sobre as orientações ao trabalho/atuação dos trabalhadores e trabalhadoras, no âmbito dos serviços de saúde, durante a Emergência em Saúde Pública de Importância Nacional em decorrência Doença por Coronavírus - COVID-19. Retrieved from https://conselho.saude.gov.br/recomendacoes-cns/1103-recomendac-a-o-no-020-de-07-de-abril-de-2020 [ Links ]
Mo, Y., Deng, L., Zhang, L., Lang, Q., Liao, C., Wang, N., Qin, M., & Huang, H. (2020). Work stress among Chinese nurses to support Wuhan for fighting against the COVID-19 epidemic. Journal of Nursing Management, 1-8. doi: 10. [ Links ]1111/jonm.13014
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & The PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(6): e1000097. doi: 10.1371/journal.pmed.1000097 [ Links ]
Oliva, G. (2020, March 18). Coronavírus: Cristo Redentor projetará bandeiras de países com casos da doença em celebração pelos infectados. O Globo. Retrieved from https://oglobo.globo.com/rio/coronavirus-cristo-redentor-projetara-bandeiras-de-paises-com-casos-da-doenca-em-celebracao-pelos-infectados-24312024 [ Links ]
Pandey, S. K., & Sharma, V. (2020). A tribute to frontline corona warriors - Doctors who sacrificed their life while saving patients during the ongoing COVID-19 pandemic. Indian Journal of Ophthalmology, 68(5), 939-942. Retrieved from http://www.ijo.in/text.asp?2020/68/5/939/282896 [ Links ]
Rede de Apoio Psicológico. (n.d). Precisamos cuidar de quem cuida, plataforma que conecta trabalhadores da saúde da linha de frente a psicólogos. Retrieved from https://www.rededeapoiopsicologico.org.br/ [ Links ]
Rego, S., & Palácios, M. (2020). Pesquisador da ENSP aborda questões sobre a saúde mental dos trabalhadores de saúde em tempos de COVID-19. Retrieved from https://portal.fiocruz.br/sites/portal.fiocruz.br/files/documentos/saude_mental_dos_trabalhadores_de_saude_em_tempos_de_coronavirus.pdf [ Links ]
Rocha, M. E., Freire, K. P., Reis, W. P. D., Vieira, L. T. Q., & Sousa, L. M. (2020). Fatores que ocasionam o índice de transtornos depressivos e de ansiedade em profissionais de enfermagem: uma revisão bibliográfica. Brazilian Journal of Development, 6(2), 9288-9305. Retrieved from http://www.brazilianjournals.com/index.php/BRJD/article/view/7192/6272 [ Links ]
Santos, I. S., Tavares, B. F., Munhoz, T. N., Almeida, L. S. P., Silva, N. T. B., Tams, B. D., ... Matijasevich, A. (2013). Sensibilidade e especificidade do Patient Health Questionnaire-9 (PHQ-9) entre adultos da população geral. Caderno de Saúde Pública, 29(8), 1533-1543. doi: 10.1590/0102-311X00144612 [ Links ]
Silva, A. C. O., Nardi, A. E., & Horowitz, M. (2010). Versão brasileira da Impact of Event Scale (IES): tradução e adaptação transcultural. Revista de Psiquiatria do Rio Grande do Sul, 32(3), 86-93. Retrieved from https://www.scielo.br/pdf/rprs/v32n3/v32n3a05 [ Links ]
Simon, G. (2020, April 17). Psicólogas de SC criam serviço gratuito para atender pessoas afetadas pela COVID-19. Diário Catarinense. Retrieved from https://www.nsctotal.com.br/noticias/psicologas-de-sc-criam-servico-gratuito-para-atender-pessoas-afetadas-pela-covid-19 [ Links ]
Sun, N., Shi, S., Jiao, D., Song, R., Ma, L., Wang, H., ... Wang, H. (2020). A qualitative study on the psychological experience of caregivers of COVID-19 patients. American Journal of Infection Control, 48(2020), 592-598. doi: 10.1016/j.ajic.2020.03.018 [ Links ]
Vignola, R. C. B. (2013). Escala de depressão, ansiedade e estresse (DASS): adaptação e validação para o português do Brasil (Master's thesis). Retrieved from http://repositorio.unifesp.br/handle/11600/48328 [ Links ]
Vignola, R. C. B., & Tucci, A. M. (2014). Adaptation and validation of the depression, anxiety and stress scale (DASS) to Brazilian Portuguese. Journal of Affective Disorders, 155, 104-109. doi: 10.1016/j.jad.2013.10.031 [ Links ]
World Health Organization. (2020a). Coronavirus disease 2019 (COVID-2019) Situation Report-51 [Highlights]. Geneva: Author. Retrieved from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10 [ Links ]
World Health Organization. (2020b). Coronavirus disease (COVID-19) Situation Report-121 [Highlights]. Geneva: Author. Retrieved from dhttps://www.who.int/docs/default-source/coronaviruse/situation-reports/20200520-covid-19-sitrep-121.pdf?sfvrsn=c4be2ec6_2 [ Links ]
World Health Organization. (2020c, April 18). 'One World: Together At Home' Global Special. Retrieved from https://www.who.int/news-room/events/detail/2020/04/18/default-calendar/one-world-together-at-home-global-special [ Links ]
Wu, P., Fang, Y., Guan, Z., Fan. B., Kong, J., Yao, Z., ... Hoven, C. (2009). The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry, 54(5), 302-311. doi: 10.1177/070674370905400504 [ Links ]
Wu, W., Zhang, Y., Wang, P., Zhang, L., Wang, G., Lei, G., ... Luo, M. (2020). Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. Journal of Medical Virology, 92(10), 1962-1970. doi: 10.1002/jmv.25914 [ Links ]
Yin, X., & Zeng, L.(2020). A study on the psychological needs of nurses caring for patients with coronavirus disease 2019 from the perspective of the existence, relatedness, and growth theory. International Journal of Nursing Sciences, 7, 157-160. doi: 10.1016/j.ijnss.2020.04.002 [ Links ]
Zhang, C., Yang, L., Liu, S., Ma, S., Wang, Y., Cai, Z., ... Zhang, B. (2020). Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Frontiers in Psychiatry, 11(306), 1-9. doi: 10.3389/fpsyt.2020.00306 [ Links ]
Received in 31.may.20
Revised in 01.dec.20
Accepted in 31.dec.20
Rafaela Luiza Trevisan, Mestra em Psicologia pela Universidade Federal de Santa Catarina (UFSC), Doutoranda pelo Programa de Pós-graduação em Psicologia da Universidade Federal de Santa Catarina (UFSC), é Psicóloga da Secretaria de Estado da Administração de Santa Catarina. Endereço para correspondência: Rua Joaquim José Antunes, 448 – casa 02. Vivendas do Campeche. Bairro Campeche. Florianópolis – SC. CEP: 88.065-160. Email: rafaelaluiza79@gmail.com
Mariana Bonomini Fogaça de Almeida, Mestra em Saúde Mental e Atenção Psicossocial pela Universidade Federal de Santa Catarina (UFSC), Doutoranda em Psicologia pela Universidade Federal de Santa Catarina (UFSC). Email: mariana.bonomini@gmail.com
Davi Baasch, Doutor em Psicologia pela Universidade Federal de Santa Catarina (UFSC), Pós-doutor em Administração Pública pela Universidade do Estado de Santa Catarina (UDESC), é Professor Substituto da Universidade do Estado de Santa Catarina (UDESC). Email: davibaasch@gmail.com
Paola Barros Delben, Mestra em Psicologia Organizacional e do Trabalho pela Universidade Federal de Santa Catarina (UFSC), Doutoranda da Universidade Federal de Santa Catarina (UFSC). Email: p.barros.delben@gmail.com
Karen Rayany Ródio-Trevisan, Mestra em Psicologia pela Universidade Federal de Santa Catarina (UFSC), Doutoranda da Universidade Federal de Santa Catarina (UFSC), Docente na Faculdade CESUSC. Email: karenrtpsico@gmail.com
Roberto Moraes Cruz, Doutor em Engenharia de Produção pela Universidade Federal de Santa Catarina (UFSC), Pós-doutor pela Universidade Federal de Minas Gerais (UFMG), é Professor e pesquisador da Universidade Federal de Santa Catarina (UFSC). Líder do Laboratório Fator Humano (UFSC) e pesquisador do Núcleo de Pesquisa em Neuropsicologia em Saúde (hospital Universitário-UFSC). Email: robertocruzdr@gmail.com














