Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Interamerican Journal of Psychology
versão impressa ISSN 0034-9690
Interam. j. psychol. v.40 n.2 Porto Alegre ago. 2006
ARTÍCULOS
Cognitive-behavioral group therapy for depression in adolescents with diabetes: a pilot study
Terapia cognitivo-conductual grupal para la depresión en adolescentes con diabetes: un estudio piloto
Jeannette M. Rosselló1, 2 ; María I. Jiménez-Chafey
University of Puerto Rico, Río Piedras, Puerto Rico
ABSTRACT
The purpose of this study is to adapt and pilot test a group Cognitive-Behavioral Therapy (CBT) model which has been proven to be effective in treating depression in Puerto Rican adolescents, to treat depressive symptoms and improve glycemic control in adolescents with diabetes. Eleven adolescents aged 13-16 participated in a 12 session group CBT intervention. Indicators of outcome effects (depressive and anxious symptomatology, self-esteem, hopelessness, diabetes self-efficacy, self-care and glycemic control) were assessed pre and post therapy using self-report instruments and a measure of glycosilated hemoglobin. Depressive symptomatology, self-concept and diabetes self-efficacy significantly improved after the intervention, and reductions in anxious symptoms and hopelessness were also observed. There were no significant changes in glycemic control or self-care behaviors. The findings of this pilot study suggest that group CBT is a feasible intervention for adolescents with diabetes and depressive symptomatology. However, further research is needed in developing interventions that improve self-care and glycemic control.
Keywords: Cognitive behavioral therapy, Diabetes, Major depression, Adolescents.
RESUMEN
El propósito de este estudio es adaptar y hacer un estudio piloto de una intervención de Terapia Cognitivo-Conductual (TCC) grupal que ha sido efectivo en tratar la depresión en adolescentes puertorriqueños/as, para tratar los sintomatología depresiva y mejorar el control glucémico en adolescentes con diabetes. Once adolescentes entre las edades de 13 y 16 participaron en 12 sesiones de la intervención. Indicadores de los efectos de la intervención (sintomatología depresiva y ansiosa, auto-estima, desesperanza, auto-eficacia y auto-cuido en diabetes, control glucémico), fueron evaluados pre y post terapia usando instrumentos de auto-reporte y una medida de hemoglobina glicosilada. Los síntomas de depresión, el auto-concepto y la auto-eficacia mejoraron significativamente luego de la intervención, y se observaron reducciones en los síntomas de ansiedad y la desesperanza. No se observaron cambios significativos en el control glucémico ni conductas de auto-cuido. Estos hallazgos sugieren que la TCC grupal es una intervención viable para adolescentes con diabetes y sintomatología depresiva. Sin embargo, se necesita más investigación para desarrollar intervenciones que aumenten el auto-cuido y el control glucémico.
Palabras clave: Terapia cognitivo-conductista, Diabetes, Depresión, Adolescente.
Over the past years, research has evidenced a high prevalence of depression in patients with diabetic patients and its deleterious relationship to the metabolic control of this disease (Anderson, Freedland, Clouse, & ; Lustman, 2001; Lustman et al., 2000). Although the reasons for this are not clear, most researchers agree that an interaction of both physiological (neurochemical and neurovascular changes) and psycho-social factors (decreased quality of life, chronic stress associated with daily diabetes management) interact to increase psychological vulnerability to depression (Talbot & ; Nouwen, 2000). This is particularly true for adolescents with type 1 diabetes mellitus (T1DM) who because of the characteristics inherent to their developmental stage, often find diabetes self-care and management overwhelming. In addition, it is well documented that during adolescence glycemic control and adherence to treatment regimen tend to deteriorate significantly due to a combination of physiological, psychological and social factors such as hormonal changes that can affect insulin resistance, need for peer acceptance, increased search for independence and increased risk-taking behavior (Ruggiero & ; Javorsky, 1999).
Numerous studies suggest that youth with diabetes are at a greater risk of presenting psychiatric disorders, particularly depression (Blantz, Rensch-Jacobson, Fritz- Sigmund, & Schmit, 1993; Dantzer, Swendsen, Maurice- Tison, & Salamon, 2003; Kovacs, Obrosky, Goldston, & Drash, 1997; Lavigne & Faier-Routman, 1992). Also, depression in adolescents has been linked to poor glycemic control in various studies (Bryden et al., 2001; Martínez- Chamorro, Lastra-Martínez, & Luzuriaga, 2002; Daviss et al., 1995; Lernmark, Persson, Fisher, & Rydeluis, 1999). Thus, adolescents with T1DM appear to be at high risk for medical complications associated with having diabetes, due to both their developmental stage and higher vulnerability to depression, which in turn, affect self-care behaviors and consequently, glycemic control.
Puerto Rico has one of the highest incidences of type 1 diabetes mellitus (T1DM) in children and adolescents in America and the Caribbean, and the highest registry of minority children in the U.S. (Frazer de Llado, González de Pijem, & Hawk, 1998; Karvonen et al., 2000). Despite this, there is a lack of studies on the psychological status of this population. One study of a sample of 101 Puerto Rican children and adolescents with DMT1 found that almost half (45.5%) reported symptoms of depression ranging from mild to severe (Rosselló & Jiménez-Chafey, 2005) and approximately 62% expressed symptoms of anxiety (Rosselló & Pérez, 2003). Over half (60%) of the youth in this sample presented poor glycemic control. These results suggest that this population is at a high health risk and in need of interventions that address both glycemic control and depressive symptomatology.
Most psychological interventions for adolescents with T1DM have focused on increasing self-care adherence, glycemic control, and psycho-social variables such as stress management and coping skills (Delamater et al., 2001; Hampson et al., 2000). A systematic review of the literature on behavioral interventions for adolescents with T1DM was performed by Hampson et al. (2000) that found that most interventions had larger effect sizes on psycho-social variables such self-efficacy and communication skills, than on glycemic control. They also found that interventions that were theoretically driven (i.e. behavioral principles, social learning theory, family therapy) were significantly more effective than those that were not.
The purpose of this study was to adapt and pilot test a Cognitive-Behavioral group therapy model which has been proven to be effective in treating depression in Puerto Rican adolescents (Rosselló & Bernal, 1999), to treat depressive symptoms and improve glycemic control in adolescents with T1DM in a group format. Cognitive Behavioral Therapy (CBT) is based on the theory that there is a relationship between a persons thoughts (cognitions), actions and mood (Beck, Rush, Shaw, & Emery, 1979). People who suffer from depression generally present negative thoughts, isolation, decreased pleasant activities and difficulties in interpersonal relationships. CBT is a highly structured therapy that focuses on teaching patients how to use cognitive techniques to identify maladaptive negative thought patterns and replace them with more adaptive and healthy ones. It also focuses on behavior and its effect on mood, and works with increasing the patients pleasant activities in order to improve their mood. CBT has been used successfully to treat depression in Puerto Rican adolescents (Rosselló, 1993; Rosselló & Bernal, 1996, 1999, 2005).
CBT for depression in adults with diabetes has been shown to be effective in reducing depressive symptoms (Lustman, Griffith, Freedland, Kissel, & Clouse, 1998). CBT has also been used effectively for poorly controlled adults with T1DM (Snoek, Van der Ven, & Lubach, 1999). Hains, Davies, Parton and Silverman (2001) used a CBT intervention for six adolescents with elevated levels of anxiety, anger and diabetes stress and found that four of the six adolescents showed improvement in one or more variables measured at baseline. No other studies using CBT with adolescents with T1DM were identified. This study will evaluate the feasibility of a group CBT intervention for Puerto Rican adolescents with T1DM. Indicators of outcome effects, including depressive and anxious symptomatology, self-esteem, hopelessness and glycemic control will also be examined.
Method
Sample
Recruitment for participation in the study began after obtaining the approval of the protocol by the Universitys Institutional Review Board. Potential participants were recruited from the patient population of two diabetes clinics in the metropolitan area, as well as through Diabetes Associations. Adolescents were eligible to participate if: a) they were between the ages of 13 and 17; b) had type 1 diabetes; c) presented symptoms of depression; and, d) did not present psychological symptoms that would interfere with their participation in therapy (i.e. active suicidal ideation, cognitive deficits).
Forty seven phone calls were received from parents interested in having their son/daughter participate in the study. Twenty three of these were excluded because they did not meet the study’s requirements. Twenty of the remaining 24 eligible participants agreed to attend a two hour screening assessment. The four who did not come expressed difficulty due to lack of transportation or time restraints.
After obtaining verbal and written informed consent from adolescents and their parents, both participated in an assessment interview and completed questionnaires. Four adolescents had to be excluded from the study: three did not present depressive symptoms and one had a co-morbid Pervasive Developmental Disorder. Sixteen adolescents were included in therapy at baseline and eleven adolescents completed therapy. Three adolescents failed to attend the first session; two expressed lack of interest and the other was admitted to an inpatient psychiatric facility. Two adolescents terminated the study prematurely after the fifth session; one was interned into an inpatient program and the other we were unable to contact.
A total of eleven participants completed therapy; two males and nine females. Their ages ranged from 12 to 16 years (M=14.1; SD=1.3). Almost all participants attended public school (n=10). The duration of diabetes for this sample ranged from one to eight years (M=3.1; SD=2.8). Two participants were on the insulin pump. Nine participants were on regimens of between two and four daily insulin injections (M=2.2; SD=0.6). The number of self-monitoring blood glucose tests ranged from one to four in the sample (M=2.6; SD=0.8).
Measures
The following measures were administered pre and post intervention:
Childrens Depression Inventory (CDI).This is a 27 item self-rated symptom-oriented scale suitable for school-aged children and adolescents (Kovacs, 1992). The CDI quantifies a wide range of depressive symptoms including disturbances in mood and capacity to enjoy activities, vegetative functions, self-evaluations, and interpersonal behavior. Kovacs (1992) reported a reliability coefficient of.86 for the scale and has found it to be a valid measure when compared with other instruments. The instrument was selected because it provides a self-report measure able to differentiate mild and severe depression (cutoffs values of 12 and 19, respectively). It was translated into Spanish and culturally adapted in Puerto Rico (Rosselló, Guisasola, Ralat, Martínez, & Nieves, 1992). Its semantic content and technical equivalence with the original instrument were considered (Flaherty, 1987). The use of this instrument in Puerto Rican samples suggests that it is a highly internally consistent instrument (alpha=.83) and has acceptable concurrent validity (Rosselló et al., 1992).
Diabetic Management Information Sheet (Kovacs et al., 1990). This semi-structured interview schedule was adapted and translated into Spanish. It is used to obtain diabetes related information from parents, such as age of onset, reactions to diagnosis, adherence (exercise, insulin use, diet, frequency of blood glucose monitoring), responsibility of management, number of hospitalizations and emergency room visits related to T1DM, as well as other information.
Glycemic Control Measure. Glycosylated hemoglobin (HbA1c) levels were obtained at pre and post intervention. HbA1c provides a measure of glycemic control for the previous 2-3 months. Values above 8% are classified as being an indicator of inadequate or poor metabolic control.
Beck Anxiety Inventory (BAI). This is a 21-item inventory that presents anxiety symptoms to be rated on a severity scale (Beck & Steer, 1993). It has high reliability (ranging from.92 to.94). Validity testing reflects adequate content, concurrent, construct, discriminant, and factorial validity. A previous study with Puerto Rican sample of adolescents revealed an alpha of.89 (Rosselló & Jiménez-Chafey, 2005).
Hopelessness Scale for Children (HSC). The HSC is a 17- item scale designed to measure cognitions of hopelessness defined as negative expectations about oneself and the future (Kazdin, French, Unis, Esveldt-Dawson, & Sherick, 1983). A back translation method was used to translate this scale for use in this study. This scale has demonstrated acceptable reliability coefficients and validity (alpha=.70). Previous studies with Puerto Rican adolescents have yielded an alpha of .80 (Rosselló & Jiménez-Chafey, 2005).
Piers-Harris Childrens Self Concept Scale (PHCSCS). This scale consists of 79 items to be answered yes or no (Piers & Harris, 1984). The assertions are answered according to what the student likes or dislikes about him or herself. The general score offers an index of self-concept and increasing values represent better self-concept. The reliability coefficient has been reported to be .94. This instrument was translated and adapted in a previous study, considering its semantic, content and technical equivalence with the original version (Rosselló & Bernal, 1999). Its internal consistency in a Puerto Rican sample has been tested (alpha=+.94); (Ramos, 1984).
Summary of Self-Care Activities (SSCA). This self-report instrument is used to measure adherence to type 1 diabetes treatment (Schafer, Glasgow, McCaul, & Dreher, 1983). Since it is a short instrument (seven items) it is ideal for use in repeated measure designs. It has good psychometric characteristics: a reliability index of.79 and high correlation with another self-report measure (Bond, Aiken, & Somerville, 1992). An alpha of.80 was obtained in a recent study with a sample of Puerto Rican adolescents (Rosselló, Jiménez- Chafey, & Díaz, 2005).
Self-Efficacy for Diabetes Scale (SED). The SED is a 35-item scale designed to measure the self-perception or expectations of competence, power and resources for successful management of type 1 diabetes (Grossman, Brink, & Hauser, 1987). It offers a self-evaluation of an individuals ability to cope with diabetes. The authors have reported adequate psychometric properties with a reliability coefficient of between 0.90 and 0.92. In a recent study with a sample of Puerto Rican adolescents an alpha of.91 was obtained (Rosselló et al., 2005).
Procedure
Phase I
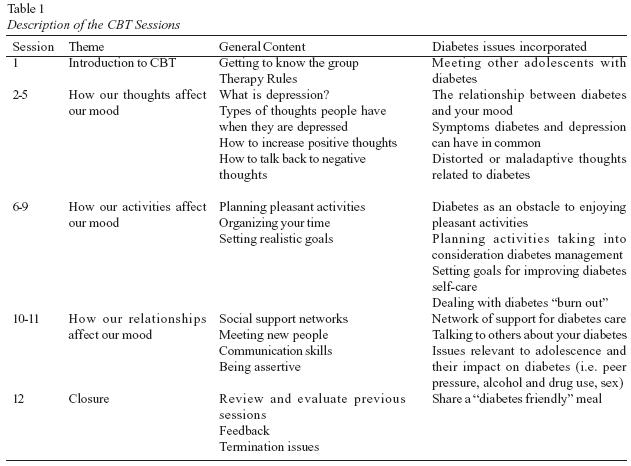
The first phase of this study consisted of adapting a Cognitive-Behavioral Therapy (CBT) treatment manual which has proven to reduce depressive symptoms in Puerto Rican adolescents for use with adolescents with T1DM (Rosselló & Bernal, 1999). Issues relevant to diabetes management and control were integrated into the treatment manual, as well as strategies for dealing with common worries and difficulties presented by adolescents in Puerto Rico based on previous studies with this population (Rosselló & Maysonet, in press). Table 1 presents the general content areas for each therapy session.
Cognitive Behavioral Group Therapy Intervention
The main goals for CBT therapy are to reduce depressive symptoms and the length of time the adolescent is depressed, teach ways to prevent becoming depressed, feel more in control of their lives and their diabetes, and improve diabetes care and glycemic control. The CBT intervention integrates educational and discussion segments to provide the adolescents with information about coping with depression and diabetes, as well as an opportunity to address concerns and questions. Various strategies are used to facilitate discussion, including games, role-playing exercises, group discussion, and worksheets. Each session follows a basic format of: 1) week-in-review; 2) review weekly mood rating scales, blood glucose monitoring and home practice assignments; 3) summary of previous session; 4) presentation of new material; 5) group discussion and exercises; and, 6) home practice assignment or exercise.
The first session focuses on getting acquainted and introducing CBT and weekly home practice assignments using group discussion and ice breaking exercises. The first module consisting of four sessions focuses on how our thoughts affect our mood. The first sessions of this module focus on defining depression and the types of thoughts people have when they are depressed. The relationship between how diabetes and mood affect each other, as well as symptoms that diabetes and depression can have in common, are discussed. The following sessions work with identifying maladaptive or negative thought patterns, including thoughts about diabetes, and ways of changing or debating these thoughts. The last session provides strategies for increasing positive thoughts and reducing unhealthy thoughts in order to improve mood.
The next module contains four sessions devoted to discussing how our activities affect our mood. The cycle between having depressive symptoms and participating in fewer activities is presented. These sessions focus on the importance of establishing a balance between pleasant activities and responsibilities, as well as strategies for maintaining an appropriate balance such as organizing our time and setting realistic and clear goals. Barriers to enjoying pleasant activities, including having diabetes, and ways to overcome them are discussed. These sessions also work with defining and coping with diabetes burnout, as well as setting personal goals for improving diabetes self-care.
The sessions in the last module focus on how our relationships affect our mood. The importance of having a social support network to help us deal with difficult circumstances, including managing diabetes is presented, as well as ways to strengthen and maintain that network. Communication skills for meeting new people, maintaining healthy relationships and being assertive are discussed and practiced. Also, how and what to tell others about having diabetes is discussed, as well as what you should tell and ways to feel comfortable doing it. Issues related to adolescence and diabetes management such as peer pressure, alcohol and drug use, and sex are discussed and integrated into the sessions in this module.
During the final session, therapists and participants offer the group members feedback on their participation in the group and progress in therapy. Previous meetings and material are reviewed. Current functioning is assessed and when necessary, referrals for continuation in therapy are made. At the end of this session, a farewell diabetes friendly meal is shared with the participants and an individual parent and adolescent session is scheduled. During this session, parents and adolescents are given individualized feedback and recommendations based on participation in therapy and the therapists observations of the adolescent.
Phase II
The second phase consisted of the feasibility study. Three consecutive cycles of 12 two hour sessions of group CBT were co-led by two doctoral level psychologists using the adapted CBT treatment manual. Participants were given a workbook with a summary of the material presented in each session and worksheets used in sessions and for home practice assignments. All sessions were carried out on Saturday mornings at the University Center for Psychological Studies and Research. Weekly ongoing supervision was provided by the P.I. All sessions were videotaped and 80% were evaluated for treatment integrity by and independent rater; integrity ranged from 82-92%. All participants attended 8 sessions or more. Participant assessments were performed pre and post-therapy.
Results
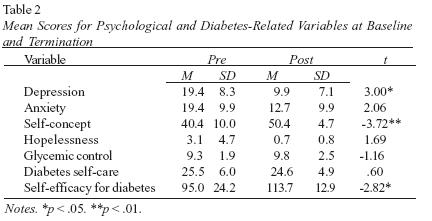
Table 2 presents the mean scores for the group on psychological variables (depression, anxiety, hopelessness and self-concept) and diabetes related variables (self-care, self-efficacy and glycemic control) before and after the CBT intervention. Participants self-reports of depressive symptoms significantly improved after the intervention moving from moderate depressive symptoms to an absence of depressive symptoms upon termination. Self-concept improved significantly as well. Reductions (although nonsignificant) in anxious symptoms and hopelessness were also observed at termination. There were no significant changes in glycemic control or self-care behaviors posttherapy, however diabetes self-efficacy improved significantly at termination.
Discussion
This pilot study was designed to evaluate the feasibility of a group CBT intervention for Puerto Rican adolescents with T1DM in reducing depressive symptoms and improving glycemic control. Upon completion of the study, a group CBT manual for therapists and a participant workbook were adapted for adolescents with diabetes. Our experience with this adapted group CBT intervention suggests that it is a feasible intervention; it could be implemented in its entirety, there was low absenteeism and the intervention was well accepted by the participants. However, recruitment proved to be difficult mostly due to lack of transportation and time restraints as expressed by the potential participants families. School and various medical appointments throughout the year present further limits on the time adolescents with T1DM have available. Offering the intervention in a more convenient setting such as the home, community center or a health clinic could be a possible solution, as well as integrating therapy to routine medical checkups.
Outcome indicators reveal that the group presented significant improvement in depressive symptoms, selfconcept and diabetes self-efficacy, as well as reductions in anxiety and hopelessness. However, no changes were observed in glycemic control or self-care behaviors. These outcome effects on psychological variables, particularly depression and self-concept, are consistent with the results of other studies of CBT where it has been shown to reduce depression in Puerto Rican adolescents (Rosselló & Bernal, 1996, 1999, 2005). The results of this study are also are consistent with the results of various studies using group psycho-social interventions for youth with diabetes where changes were observed in psychological variables such as coping skills, communication and self-efficacy, but not in glycemic control (Boardway, Delamater, Tomakowsky, & Gutai, 1993; Delamater et al., 2001; Hampson et al., 2000; Méndez & Beléndez, 1997; Wysoki, Greco, Harris, Bubb, & White, 2001). Psycho-social interventions that work individually such as motivational interviewing, have shown some promising results in improving glycemic control (Channon, Smith, & Gregory, 2003). Also, interventions such as coping skills training that are based in diabetes clinics and embedded in intensive diabetes management treatment settings appear to have greater effects on adherence and glycemic control (Grey et al., 1998).
The lack of impact on glycemic control can be attributed to various factors. Adolescence in itself is a time when glycemic control tends to deteriorate due to physiological changes and developmental characteristics that tend to decrease self-care behaviors or adherence. Also, stress has been known to increase blood sugar levels in many patients. The presence of depressive symptoms in our sample could have acted as a bodily stressor that contributed to poor glycemic control. Secondly, we observed that most adolescents in our study were not on intensive diabetes management regimens which have become the standard of care after the DCCT trials. Lack of knowledge of diabetes care as well as economic hardship related to the high cost of diabetes treatment and supplies were observed as possible reasons for poor glycemic control as well. This made interventions geared at increasing adherence and self-care behaviors more difficult to implement as most participants lacked basic knowledge of diabetes care. All participants were referred to diabetes education programs after the intervention.
For example, one participant was hospitalized several times throughout the intervention for diabetic ketoacidosis; it became apparent that neither the patient nor his/her parents knew how to manage high blood sugars and ketones at home or through contact with the doctor. Several participants did not know to test for ketones when their blood sugars were high. Also, many participants did not adjust insulin doses according to blood sugar level, activity or food consumption. Almost all participants tested their blood sugar no more than twice daily which is also beneath recommendations of standards of care.
The lack of changes in self-care behaviors as reflected on the SSCA are somewhat disappointing. However, upon closer examination of individual scores overall the group initially reported high levels of adherence to self-care behaviors which would leave little room for improvement according to the scale. The SSCA consists of seven items which might not be sufficient to pick up significant changes in self-care behaviors. The use of weekly random 24 hour recall phone interviews to assess self-care could help evaluate self-care behavior more in a more comprehensive manner. Also, the main focus of the intervention was on depressive symptoms, so even though improving self-care behaviors was a component of intervention, it was not the primary focus. The significant changes in diabetes selfefficacy observed in this sample are promising and suggest that perhaps the intervention served to move participants who were in a pre-contemplation stage of behavior change to a contemplation stage or even a preparation stage (Ruggiero & Prochaska, 1993). It would be interesting to evaluate the stage of change in the participants pre and post intervention in future studies to test this hypothesis.
We recommend performing six, nine and 12 month follow up assessments to determine whether reductions in depressive and anxious symptoms were maintained as well as to see if there were improvements in self-care and glycemic control post-therapy. Since glycemic control as measured by HbA1c reflects glycemic control during the past three months and the intervention lasted exactly three months, not enough time had lapsed between HbA1c assessments to detect significant changes.
Adding more sessions that work specifically with self-care behaviors or integrating more related material to each session could help address the lack of improvement in glycemic control and self-care. In addition, designing interventions that are administered by a multidisciplinary (i.e. education, nutrition, behavior modification) team can help target more specifically the educational, behavioral and emotional needs of distressed adolescents in poor glycemic control. Further research is needed in developing interventions that can effectively target and improve both psychological and metabolic outcomes for youth with diabetes.
Therapists did observe however, some qualitative improvements in self-care behaviors and cognitions related to diabetes as expressed by participants during therapy sessions. Several participants expressed satisfaction in achieving their goal of choosing healthier snacks. Others presented less worry about complications, and myths and misconceptions about diabetes were clarified in therapy. Many adolescents expressed feeling more comfortable in managing parental nagging to perform self-care behaviors. Changes in negative thought patterns regarding diabetes (i.e. I cant stand living with diabetes, I am a failure if I dont take perfect care of my diabetes, I cant control my blood sugars) were also observed in several participants as expressed verbally during therapy or through their home practice assignments. The impact of the CBT intervention on other psychological variables in this sample such as quality of life and family dynamics will be examined in future studies.
Based on our experience and our findings related to this intervention, we recommend that future CBT interventions actively involve parents. In our groups we observed inconsistent parental supervision of diabetes self-care activities, frequent parent-child conflicts regarding responsibility for diabetes care and high anxiety levels among parents. It is well documented that active parental involvement in diabetes care until adolescence is associated with better treatment adherence and glycemic control (Anderson, Ho, Brackett, Finkelstein, & Laffel, 1997). In addition, cultural characteristics of Latinos/as, and Puerto Ricans in particular, of familism and greater dependence on parents during development can be important to take into consideration when designing interventions (Bernal, Bonilla, & Bellido, 1995).
One of the main limitations of this study was a lack of a control group. There was a large gender disparity among the participants. Most participants were female and two of the three groups that were led consisted entirely of females. It would be important to see whether the intervention would have the same outcome effects for more gender equivalent groups. Another limitation was the use of self-report instruments which can be associated with biased responding. The use of interviews and 24-hour recall for self-care behavior phone interviews could alleviate some of the risks of biased responding. Although the small sample size was a limitation in the interpretation of our findings, this pilot study contributes to creating the conditions for a future randomized controlled trial.
References
Anderson, B., Ho, J., Brackett, J., Finkelstein, D., & Laffel, L. (1997). Parental involvement in diabetes management tasks: relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes. Journal of Pediatrics, 130(2), 257-265. [ Links ]
Anderson, J., Freedland, K., Clouse, R., & Lustman, P. (2001). The Prevalence of comorbid depression in adults with diabetes. Diabetes Care, 24(6), 1069-1077. [ Links ]
Beck, A. T., Rush, A.J, Shaw, B.F., & Emery, G. (1979). Cognitive therapy for depression. New York, USA: Guilford Press. [ Links ]
Beck, A. T., & Steer, R. A. (1993). Beck Anxiety Inventory. San Antonio: The Psychological Corporation. [ Links ]
Bernal, G., Bonilla, J., & Bellido, C. (1995). Ecological validity and cultural sensitivity for outcome research: Issues for cultural adaptation and development of psychosocial treatments with Hispanics. Journal of Abnormal Child Psychology, 23, 67-82. [ Links ]
Blantz, B., Rensch-Jacobson, B., Fritz-Sigmund, D., & Schmidt, M. (1993). IDDM is a risk factor for adolescent psychiatric disorders. Diabetes Care, 16, 1579-1587. [ Links ]
Boardway, R., Delamater, A. M., Tomakowsky, J., & Gutai, J. (1993). Stress management training for adolescents with diabetes. Journal of Pediatric Psychology, 18(1), 29-45. [ Links ]
Bond, G., Aiken, L., & Somerville, S. (1992). The health belief model and adolescents with insulin-dependent diabetes mellitus. Health Psychology, 11, 190-198. [ Links ]
Bryden, K., Neil, A., Peveler, R., Mayou, R., Stein, A., & Dunger, D. (2001). Clinical and psychological course of diabetes from adolescence to young adulthood. Diabetes Care, 24(9), 1536- 1540. [ Links ]
Channon, S., Smith, V., & Gregory, J. (2003). A pilot study of motivational interviewing in adolescents with diabetes. Archives of the Disabled Child, 88, 680-683. [ Links ]
Dantzer, C., Swendsen, J., Maurice-Tison, S., & Salamon, R. (2003). Anxiety and depression in juvenile diabetes: A critical review. Clinical Psychology Review, 23, 787-800. [ Links ]
Daviss, W., Coon, H., Whitehead, P., Ryan, K., Burkley, M., & McMahon, W. (1995). Predicting diabetic control from competence, adherence, adjustment, and psychopathology. Journal of the Academy of Child and Adolescent Psychiatry, 34(12), 1629-1636. [ Links ]
Delamater, A., Jacobson, A., Anderson, B., Cox, D., Fisher, L., Lustman, P., et al. (2001). Psychosocial therapies in diabetes. Diabetes Care, 24(7), 1286-1292. [ Links ]
Flaherty, J. (1987). Appropriate and inappropriate research methodologies for Hispanic Mental Health. In M. Gaviria (Ed.), Health and behavior: Research agenda for Hispanics (pp. 177- 186). Chicago, USA: University of Illinois Press. [ Links ]
Frazer de Llado, T., González de Pijem, L., & Hawk, B. (1998). Incidence of IDDM in children living in Puerto Rico. Diabetes Care, 21(5), 744-751. [ Links ]
Grey, M., Boland, E., Davidson, M., Yu, C., Sullivan-Bolyai, S., & Tamborlane, W. (1998). Short term effects of coping skills training as adjunct to intensive therapy in adolescents. Diabetes Care, 21(6), 902-908. [ Links ]
Grossman, H., Brink, S., & Hauser, S. (1987). Self-efficacy in adolescent girls and boys with insulin-dependent diabetes mellitus. Diabetes Care, 10(3), 324-329. [ Links ]
Hains, A., Davies, W., Parton, E., & Silverman, A. (2001). Brief Report: A Cognitive-Behavioral intervention for distressed adolescents with type 1 diabetes. Journal of Pediatric Psychology, 26(1), 61-66. [ Links ]
Hampson, S., Chas Skinner, T., Hart, J., Storey, L., Gage, H., Foxcroft, D., et al. (2000). Behavioral interventions for adolescents with type 1 diabetes: How effective are they? Diabetes Care, 23(9), 1416-1421. [ Links ]
Karvonen, M., Viik-Kajander, M., Moltchanova, E., Libman, I., LaPorte, R., & Tuomilehto, J. (2000). Incidence of childhood type I diabetes worldwide. Diabetes Care, 23, 1516-1532. [ Links ]
Kazdin, A., French, N., Unis, A., Esveldt-Dawson, K., & Sherick, R. (1983). Hopelessness, depression, and suicidal intent among psychiatrically disturbed children. Journal of Consulting and Clinical Psychology, 51, 504-510. [ Links ]
Kovacs, M. (1992). Childrens Depression Inventory (CDI) Manual. New York, USA: Multi-Health Systems. [ Links ]
Kovacs, M., Iyengar, S., Goldston, D., Steward, T., Obrosky, D., & Marsh, J. (1990). Psychological functioning of children with insulin-dependent diabetes mellitus: A longitudinal study. Journal of Pediatric Psychology, 15, 619-632. [ Links ]
Kovacs, M., Obrovsky, D., Goldston, D., & Drash, A. (1997). Major depressive disorder in youths with IDDM: A controlled prospective study of course and outcome. Diabetes Care, 20, 45-51. [ Links ]
Lavigne, J., & Faier-Routman, J. (1992). Psychological adjustment to pediatric physical disorders: A meta-analytic review. Journal of Pediatric Psychology, 17, 133-157. [ Links ]
Lernmark, B., Persson, B., Fisher, L., & Rydeluis, P. (1999). Symptoms of depression are important to psychological adaptation and metabolic control in children with diabetes mellitus. Diabetic Medicine, 16, 14-22. [ Links ]
Lustman, P., Anderson, R., Freedland, K., de Groot, M., Carney, R., & Clouse, R. (2000). Depression and poor glycemic control: A meta-analytic review of the literature. Diabetes Care, 23, 934- 942. [ Links ]
Lustman, P., Griffith, L., Freedland, K., Kissel, S. S., & Clouse, R. (1998). Cognitive behavior therapy for depression in type 2 diabetes Mellitus. Annals of Internal Medicine, 129(8), 613- 621. [ Links ]
Martinez Chamorro, M., Lastra Martínez, I., & Luzuriaga Tomás, C. (2002). Psicopatología y evolución de la diabetes mellitus tipo 1 en niños y adolescentes. Actas Españolas de Psiquiatria, 30(3), 175-181. [ Links ]
Méndez, F., & Beléndez, M. (1997). Effects of a behavioral intervention on treatment adherence and stress management in adolescents with IDDM. Diabetes Care, 20(9), 1370-1375. [ Links ]
Piers, E., & Harris, D. (1984). The Piers-Harris Childrens Self- Concept Scale. Los Angeles, USA: Western Psychological Services. [ Links ]
Ramos, G. (1984). El trato de menores y su relación con el autoconcepto. Unpublished Masters Thesis, University of Puerto Rico, San Juan, Puerto Rico. [ Links ]
Rosselló, J. (1993). Acercamientos terapéuticos para la depresión en adolescentes puertorriqueños: Dos estudios de casos. Interamerican Journal of Psychology, 27, 163-180. [ Links ]
Rosselló, J., & Bernal, G. (1996). Cognitive-behavioral and interpersonal treatments For depressed Puerto Rican adolescents. In E. Hibbs & P. Jensen (Eds.), Psychosocial treatments for children and adolescent disorders: Empirically based approaches (pp.187-218). Washington, DC, USA: American Psychological Association. [ Links ]
Rosselló, J., & Bernal, G. (1999). The efficacy of Cognitivebehavioral and Interpersonal treatments for depression in Puerto Rican adolescents. Journal of Consulting and Clinical Psychology, 67, 734-745. [ Links ]
Rosselló, J., & Bernal, G. (2005). A randomized clinical trial of CBT and IPT in individual and group format for depression in Puerto Rican adolescents. In E. Hibbs & P. Jensen (Eds.), Psychosocial treatments for depressed Puerto Rican adolescents disorders: Empirically based approaches (2nd ed., pp. 187-218). Washington, DC, USA: American Psychological Association Press. [ Links ]
Rosselló, J., Guisasola, E., Ralat, S., Martínez, S., & Nieves, A. (1992). La evaluación de la depresión en niños/as y adolescentes puertorriqueños. Revista Puertorriqueña de Psicología, 8, 155- 162. [ Links ]
Rosselló, J., & Jimenez-Chafey, M. I. (2005). Depressive and anxious symptomatology in Puerto Rican adolescents with type 1 diabetes and their relationship to glycemic control. Manuscript submitted for publication.Universidade de Puerto Rico, Río Piedras, Puerto Rico. [ Links ]
Rosselló, J., Jimenez-Chafey, M. I., & Díaz, M. (2005). Autoeficacia, auto-cuido y control glucémico en adolescentes puertorriqueños/as con diabetes tipo 1. Manuscript submitted for publication. Universidad de Puerto Rico, Río Piedras, Puerto Rico. [ Links ]
Rosselló, J., & Maysonet, M. (in press). Dificultades e inquietudes identificadas por jóvenes puertorriqueños/as con diabetes mellitus insulino-dependiente: Su relación con control metabólico, desesperanza, apoyo social y sintomatología depresiva. Puerto Rico Health Sciences Journal. [ Links ]
Rosselló, J., & Perez, D. (2003). Ansiedad y apoyo social en niños/ as y adolescente con diabetes insulino-dependiente. Boletín de la Asociación Médica de Puerto Rico, 95, 7-15. [ Links ]
Ruggiero, L., & Javorsky, D. (1999). Diabetes self-management in children. In A. J. Goreczny & M. Hersen (Eds.), Handbook of Pediatric and Adolescent Health Psychology (pp.49-70). Boston, USA: Ally & Bacon. [ Links ]
Ruggiero, L., & Prochaska, J. O. (1993). From research to practice: Readiness for change. Diabetes Spectrum, 6, 21-60. [ Links ]
Schafer, L. C., Glasgow, R., McCaul, K., & Dreher, M. (1983). Adherence to IDDM regimens: Relationship to psychosocial variables and metabolic control. Diabetes Care, 6, 493-498. [ Links ]
Snoek, F., Van der Ven, N., & Lubach, C. (1999). Cognitive behavioral group training for poorly controlled Type 1 Diabetes patients: A psychoeducational approach. Diabetes Spectrum, 12(3), 147- 152. [ Links ]
Talbot, F., & Nouwen, A. (2000). A review of the relationship between depression and diabetes in adults: Is there a link? Diabetes Care, 23(10), 1556-1562. [ Links ]
Wysocki, T., Greco, P., Harris, M., Bubb, J., & White, N. (2001). Behavior therapy for families of adolescents with diabetes. Diabetes Care, 24, 1270-128. [ Links ]
Received 12/11/2005
Accepted 30/03/2006
1 Address: University Center of Psychological Services and Research (CUSEP), University of Puerto Rico, Río Piedras Campus, P.O. Box 23174, San Juan, Puerto Rico 00931-3174. E-mail: jmross@prtc.net
2 Acknowledgements: This work was supported by The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Grant # 5R21DK064747-02 and the University Center of Psychological Services and Research, University of Puerto Rico, Río Piedras Campus.
Jeannette Rosselló, Ph.D. University Center of Psychological Services and Research (CUSEP), University of Puerto Rico, Río Piedras Campus. Current Interests: Evaluation, treatment and prevention of adolescent depression; Cognitive-Behavioral Therapy; Type 1 Diabetes in youth, Eating Disorders, Mind-Body Interventions, Psychoballet, Minorities and Mental Health.
María I. Jimenez Chafey, Psy.D. University Center of Psychological Services and Research (CUSEP), University of Puerto Rico, Río Piedras Campus. Current Interests: Type 1 and Type 2 diabetes in youth and adults; Evaluation, treatment and prevention of depression; Cognitive-Behavioral Therapy; Health Psychology; Behavioral interventions for Obesity.













