Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Journal of Human Growth and Development
versão impressa ISSN 0104-1282
Rev. bras. crescimento desenvolv. hum. vol.22 no.2 São Paulo 2012
ORIGINAL RESEARCH
Correlation between neurofunctional profile and sensory-motor skills of children with cerebral palsy
Fernanda Dorneles de MoraisI; Joyce Cristina FreitasII; Fabiana Pavan VianaIII; Cibelle Kayenne Martins Roberto FormigaIV
IFisioterapeuta graduada pela Pontifícia Universidade Católica de Goiás (PUC-GO); Bolsista de Iniciação Científica PIBIC/CNPq
IIFisioterapeuta graduada pela Pontifícia Universidade Católica de Goiás (PUC-GO); Bolsista de Iniciação Científica BIC/PUC
IIIProfessora Doutora do Departamento de Enfermagem, Nutrição e Fisioterapia e do Mestrado em Ciências Ambientais e Saúde da Pontifícia Universidade Católica de Goiás (PUC-GO)
IVProfessora Doutora da Escola Superior de Educação Física e Fisioterapia da Universidade Estadual de Goiás (UEG)
ABSTRACT
OBJECTIVE: to investigate the correlation between the profile neurofunctional and sensory motor skills of children with cerebral palsy.
METHODS: the sample comprised 27 children with cerebral palsy. We used a neurological evaluation form to obtain the neurofunctional profile and Portage Inventory to evaluate sensorimotor development.
RESULTS: the functional impairment is related to the greater degree of disability, change in tone and a deficit of body reactions of children. The body reactions correlate with each other and sensory changes. There was also a correlation between the five areas of development (motor, language, socialization, self-care and cognitive), indicating the importance of each to the overall performance of the human being.
CONCLUSION: it was found that the deficit in the skills of these children is mainly related to the functional level, degree of disability, changes in the sensory system and flaws in bodily reactions. It is important to identify the correlation of these data in order to improve treatment and improve the physical functional performance of these children.
Key words: cerebral palsy; physical therapy; rehabilitation; functional performance; psychomotor profile.
INTRODUCTION
Cerebral Palsy (CP) is defined as a Non-Progressive Chronic Encephalopathy the Childhood (NPCEC), defined as a group of non-progressive motor disorders. It is primarily characterized by a persistent, though not invariable disorder, which appears in early childhood and that is not only secondary to not evolutionary brain injury, but it is also due to the influence that such injury has on the structure and function of the body1.
The CP is a disorder characterized by the presence of spasticity and lower performance on functional abilities and broad motor function2. Although the main feature of CP is the motor deficit, it is often associated with one or more disorders resulting from neurological injuries such as seizures, cognitive impairment, hearing impairment, visual impairment, language and swallowing disorders, changes in the cardio respiratory and gastrointestinal systems3.
The increase in survival rates of premature babies has increased the risk of brain lesions that potentially cause CP. The CP has high economic impact, with interference related to health as well as to the social and psychological aspects.4
Data in the literature report that the neurofunctional profile can interfere with motor skills of children with CP. The tonus changes and the presence of abnormal movement patterns hinder the maintenance of posture and movement performance. This results in preventing the acquisition of normal postural reactions. The child cannot maintain alignment, correction to perform activities of daily living and finds it difficult to maintain himself against gravity in many different postures5.
The present study is justified once it has not been found anything in literature about the correlation of the profile with the sensory-motor skills of children with cerebral palsy. Moreover, the subject is relevant so that the multidisciplinary team can have more information about the characteristics and capabilities of the patient and may more precisely define the behavior of treatment and guidelines for the care of those children.
Thus, taking into consideration the fact that the sensory-motor skill is a factor of re-establishment of children's healthy development, this study aims to investigate the correlation between the neurofunctional profile and sensorimotor skills of children with cerebral palsy.
METHODS
This is a longitudinal study which contains observations and analysis of children with cerebral palsy who attend the Department of Physical Therapy at Pestalozzi Association in Goiânia ("Renascer" branch). This study has been approved by the Ethics Committee in Research of the Catholic University of Goiás (Protocol - CAAE: 0769.0.000.168-07).Sample: Twenty-seven children of both sexes diagnosed with cerebral palsy have been included in this study. They are aged 1-12 years and attend the Department of Physical Therapy at Pestalozzi Association in Goiânia and whose parents have signed the consent form.
The neurofunctional profile was obtained by analyzing the child's neurological evaluation form used in the institution, which is composed of gestational data, evaluation of superficial and deep reflexes, involuntary movements, body assessment, functional level (GMFCS), level of disability (mild, moderate and severe), sensory systems (vision, hearing and proprioception), body righting reactions, protective reactions and equilibrium reactions.
The evaluation of the sensorimotor skills was performed using Operational Portage Inventory (OPI).6 Such instrument allows to describe the behaviors of infants and toddlers (0-6 years old), the five domain areas (motor, cognitive, linguistics, self-care and social skills), as well as the children's stimulation area. The motor skills include postural reactions, psychomotor development and use of hands. The cognitive skills refer to adjustments when facing problems, solution of practical problems; sensorimotor adjustments; decomposition of the whole into parts, reintegration and perception of relationships. The language area covers facial expressions, use of gestures,vocalizations, words and phrases; imitation and understanding. The social skills include social expressions and cooperation in regular and self-care activities and refer to independence in daily activities. The area of child stimulation refers to the tactile, visual and auditory sensibility as well as to the visual and auditory location and neuropsychomotor development7.
The OPI was adopted as an instrument of data collection once it covers almost all areas of child development for being a practical and easy-to-use instrument to be used in intervention services to infants and children. In this study, the children had a severe impairment of sensory-motor development and, therefore, remained the use of OPI within the age group. The instrument was translated and its items were operationalized for Brazilian researchers and can be used in research with children with cerebral palsy aged six years and above in contribution with professionals and families6.
Data analysis was performed by a software program named Statistical Package for Social Science (SPSS) 10.0 version and the data were analyzed by analytical statistics. Pearson's correlation coefficients were calculated between continuous variables and Spearman's for variable categories. Correlations between variables were analyzed using boxplots.
RESULTS
Of the 27 children participating in this study, 12 (44%) were female and 15 (56%) were male.The mean age was 7.4.
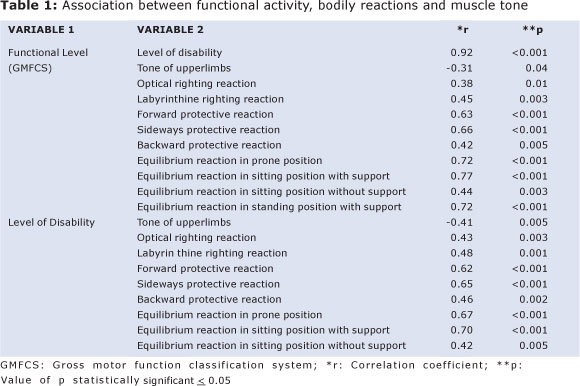
It can be seen in Table 1 that the major functional impairment is related to the higher degree of disability of children, with a change of tonus in the upper limbs and a deficit or even the absence of bodily reactions of normal sensorimotor development (Table 1).
DISCUSSION
It can be seen in Table 1 that the major functional impairment is related to the higher degree of the children's disability, with a change of tone in the upper limbs and the deficit or even the absence of bodily reactions of normal sensorimotor development (Table 1).
According to Table 2, the delayed righting reaction is associated with delayed protection and balance reactions of the child. In turn, the delay in the protective body reactions associated with the absence or reduction of equilibrium reactions in anti-gravity postures (Table 2).
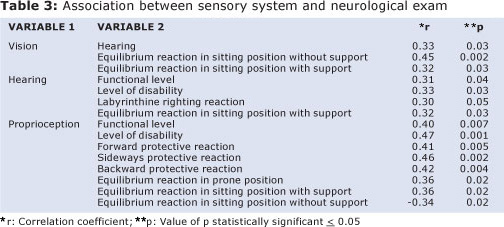
According to Table 3, children who showed a change in vision had associated changes in hearing and balance in sitting and standing positions. In turn, the change in hearing was associated with greater functional impairment, higher degree of disability and deficit in righting reactions and balance in sitting position. Regarding changes in proprioception it has been found that proprioceptive deficit was associated with greater functional impairment, greater degree of disability and delayed acquisition of protective reactions (forward, sideways and backwards) and the equilibrium reactions in anti-gravity postures.
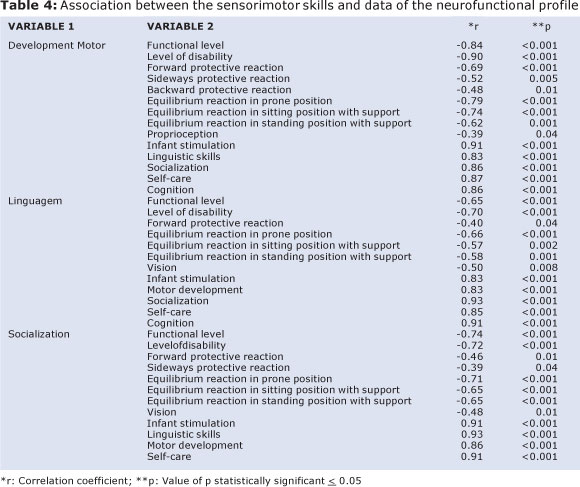
Considering the areas of development assessed by the Operational Portage Inventory as well as the items of the neurofunctional profile, it can be seen that the low scores found in children's performance was mainly related to the worst functional level and degree of impairment, deficits in bodily reactions and visual and proprioceptive changes. There was also a correlation among the five sections of development (motor, linguistic and social skills, self-care and cognitive), indicating that the delay in an area was associated with delay in the acquisition of behavior in other areas (Table 4).
According to the results obtained it can be observed a correlation between functional capacity and bodily reactions and muscle tone. These data agree with the study of Stevens et al8, once children with a greater degree of disability had greater functional impairment, and the latter may be related with age, indicating that the older the child, thelower the physical performance and greater the degree of disability. 8
As for the functional activity it is possible that it may be impaired mainly due to changes in tone and to deficit in bodily reactions. For the body to readjust and reorganize in face of various postures it is necessary that the tonus is developed and might allowthe mechanical equilibrium, which is essential for the coordination of movements in body segments9.However, it is known that postural control is also affected by environmental factors10. The absence of environmental facilitators represent a barrier to the functionality of the child. Thus, the facilitating factors are relevant to promoting function and prevention of inabilities11.
It was found that the delay in righting reactions was associated with the delay in the reactions of protection and balance. Delays in righting and equilibrium reactions are associated with deficits in functional abilities of children with brain palsy. Although the stable control of posture and balance is automatic for healthy individuals, this is often a challenge for patients with brain palsy12. According to Guimarães & Tudella13 Zafeiriou14 the deficit in the development of balance mechanisms and changes in postural reactions may be indicative of neuro-sensory-motor changes, such as the brain palsy.
The development of the righting and equilibrium reactions allows the individual to maintain his posture and balance of head, trunk and lower extremities in all normal circumstances against the gravitational action, while the arms and hands remain free to explore the environment15.
Shumway-Cook & Woolacott16corroborate it by stating that the emerging equilibrium reactions are precursors required for the acquisition of developmental milestones associated with them.
The difficulty of maintaining the body balance in children with brain palsy is mainly related to the deficits of the central nervous system and mechanical changes in the body alignment. The muscle activation can also be cited as one of the factors involved in the correct body stability, as well as the difficulties of maintaining a certain posture and/ or positioning of body segments and articular mobility17.
Regarding those children with visual impairment, they presented hearing losses and balance disorders in standing and sitting postures. This relation occurs because the vision is closely correlated with other sensory activities.After the capture and recognition of images, it occurs the cortical integration with all the other senses18. Several authors have reported that in the event of sensorial failures, there may be changes in the development, postural control, and consequently in the function itself19,20,21.The vision is of extreme importance for the maintenance of body balance, acquisition of information and adequate stimulation22. In addition to its basic function, the vision plays a key role in the late stabilization of postural corrections and in the planning of anticipatory reactions23. While evaluating 12 children with visual impairment, Okai et al. 20 found that all the children had shown failures in the protective reactions and balance deficit.
As for the proprioceptive deficit it was observed its correlation with a greater functional impairment, a higher degree of disability and delayed acquisition of protective reactions (forward, sideways and backwards) and in the equilibrium reactions in antigravitational postures. The proprioceptive system is of neurological type that receives information from multiple sensors in our body. Such system integrates and adjusts all these information and issues the necessary orders to the muscle fibers in order to make them perform a certain action24.
The worst functional level, degree of disability, and deficits in bodily and visual changes were related to impaired performance of the evaluated children. As Mancini et al.25 compared the impact of functional severity to the neuromotor profiles of 36 children with brain palsy, it was observed that there is functional superiority in those with a lower impairment. According to the literature, the brain palsy occurs in the period in which the child has a fast pace of development, impairing the acquisition of fundamental motor skills. Such impairment may interfere with the function, impairing the performance of activities commonly performed by children with typical motor development26.
The neuropsychomotor delay may impair other areas, once it limits the child's action in his/her environment, as well as the refinement of motor acts, the repetition of actions, experimentation and interactive activities with objects and people, i.e.,in the environment in which the learning process is developed27. It is necessary that all the people involved in the rehabilitation process of patients with CP understand the priorities and needs of those children and encourage them continuously in their everyday life28.
The deficit in the skills of these children is mainly related to the functional level, level of disability, changes in the sensory system and fails in protectiveand equilibrium reactions. It is noted the correlation between areas of development assessed by means of OPIwhich indicate their importance to the overall performance of the human being.
Thus, both family members and professionals may be advised to pay greater attention to the presence of sensory changes in order to improve vision, hearing and proprioception, as they are interfering in the abilities of the children. It can also be enhanced the activities offered, especially stimulating protective and equilibrium reactions, as well as the activities for tonus adequacy, which encourage environment experimentation and greater independence in order to extend the sensorimotor performance of those children.
REFERENCES
1. Peixoto ES, Mazzitelli C. Evaluation of Major Deficits and Proposed Treatment of Roll Motor Acquisition in Cerebral Palsy. Rev Neuroc. 2004, 12 (1): 46-53. [ Links ]
2. Assumpção MS, Piucco EC, ECR Corrêa, Ries LGK. Coactivation, spasticity, motor and functional performance in cerebral palsy.Motriz; 2011; 17 (4): 650-659. [ Links ]
3. Brasileiro IC, Moreira TMM. Prevalence of bodily functional changes in children with cerebral palsy, Fortaleza, Ceará, 2006.ActaFisiatr. 2008, 15 (1): 37-41. [ Links ]
4. Faria AV, Hoon A, Stashinko E, Xin Li, Jiang H, Mashaqekh A et al. Quantitative analysis of brain pathology based on MRI brain atlases and Applications for cerebral palsy. Neuro Image. 2011, 54 (3): 1854-1861. [ Links ]
5. Herreiro D, Monteiro CBM. Verification of functional abilities and need of a caregiver assistance in children with cerebral palsy early in life. Rev Bras Growth Hum Dev 2008; 18 (2): 163-169. [ Links ]
6. Williams LCA, Aiello ALR. The OperationalPortage Inventory: Intervention with families. 1st edition,São Paulo: Memnon / FAPESP, 2001. [ Links ]
7. Gejão MG, Lamônica DAC. Development skills in children with congenital hypothyroidism: focus on communication. Pró-FonoR Atual Cient. 2008, 20 (1): 25-30. [ Links ]
8. Stevens SL, Holbrook EA, DK Fuller, DW Morgan. Influence of age on step activity patterns in children with cerebral palsy and typically developing children. Arch Phys Med Rehabil. 2010, 91 (1) :1891-1896. [ Links ]
9. Alves F. Psychomotricity: body, action and emotion. 3rd edition, Rio de Janeiro: Wak, 2003. [ Links ]
10. Rodby-Bousquet E, Hägglund, G. Sitting and standing performance in a total population of children with cerebral palsy: a cross-sectional study. BMC Musculoskeletal Disorders .2010; 11(1):131-138. [ Links ]
11. PetersonMOA,Ferreira FO, Vasconcelos AG, Lima EPL, Haase VG. Cognitive profile, motor deficits and the influence of facilitators in the rehabilitation of children with neurological disorders.Rev Paul Pediatr. 2011, 29 (3): 320-327. [ Links ]
12. Borges MBS, Werneck MJS, Smith ML, Gandolfi LR. Pratesei Therapeutic effects of a horse riding simulator in children with cerebral palsy. Arq. Neuro-Disord.2011; 69 (5): 799-804. [ Links ]
13. Guimarães, EL, Tudella E. Primitive reflexes and postural reactions as signs of neurosensorimotor changes in babies at risk. Pediatrics (São Paulo) 2003, 25: 28-34. [ Links ]
14. Zafeiriou D. Primitive reflexes and postural reactions in the neurodevelopmental examination. Pediatr Neurol. 2004, 31(1): 1-8. [ Links ]
15. Val DC, Limongi SCO, Flabiano FC, Silva KCL. Stomatognathic system and body posture in children with sensorimotor disorders. Pró-FonoR Atual Cient. 2005; 17(3): 345-354. [ Links ]
16. Shumway-Cook A, Woolacott MH. Motor control: theory and practical applications. 2nd edition.Barueri, SP: Manole, 2003. [ Links ]
17. Clarissa ST, Rudi FA, SP Fleming. Body balance in children with cerebral palsy.Salusvita. 2010, 29 (2): 69-81 [ Links ]
18. Figueira MMA. Physiotherapeutic care to children with congenital blindness.Rev Benjamin Constant 2000, 17 (1): 14-34. [ Links ]
19. Rey B, Fereira CL. Occupational Therapy and Phonoaudiology: an interdisciplinary approach on multiple disabilities. Cad TerOcup. 2000; 8(2): 94-102. [ Links ]
20. Okai LA, Kitadai, SPS, Lopes, MCB. Physiotherapy assessment and treatment of motor disorders present in visually impaired children. Bras J Ophthalmol. 2004, 63 (3): 155-161. [ Links ]
21. Mochizuki L Amadio AC. Sensory information to postural control. Fisioter mov. 2006, 19 (2): 11-18. [ Links ]
22. Priscilla AJ, Liana MOV, Cínthia RT, Andrea GLS, Patricia RSR. Clinical and ophthalmologic characteristicsof individuals with special needs who are institutionalized in the state of Pernambuco, Brazil. Rev bras ophthalmol. 2011, 70 (2): 93-98. [ Links ]
23. Vallis LA, Patla AE, Adkin AL. Control of steering in the presence of unexpected head yaw Movements. Exp Brain Res 2001, 138 (1): 128-134. [ Links ]
24. Antunha ELG, Sampaio P. Proprioception: a concept in the forefront of diagnosis and therapeutics. Boletim AcadPaulista de Psicol. 2008: 278-283. [ Links ]
25. Mancini MC, Alves ACM, Schaper C, Figueiredo EM, Sampaio RF, Coelho ZA et al. Severity of cerebral palsy and functional performance. Rev Bras Fisioter. 2004, 8 (3): 253-260. [ Links ]
26. Bonomo LMM, Castro VC, Ferreira DM, Miyamoto ST. Hydrotherapy in the acquisition of the functionality of children with cerebral palsy. Rev Neurocienc. 2007, 5 (2): 125-130. [ Links ]
27. Miller G, Clark GD. Cerebral palsy: causes, consequences and management. New York: Manole, 2002. [ Links ]
28. Chiarello LA, Paralisano RJ, Maggs JM, Orlin MN, N Almasri, LJ Kang et al. Priorities for Family Activity and Participation of Children and Youth With Cerebral Palsy. PhysTher. 2010, 90 (1):1254-1264. [ Links ]
 Corresponding author:
Corresponding author:
fernandadmorais@gmail.com
Manuscript submitted Aug 09 2011
Accepted for publication May 05 2012.













