Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Journal of Human Growth and Development
versão impressa ISSN 0104-1282versão On-line ISSN 2175-3598
J. Hum. Growth Dev. vol.25 no.3 São Paulo 2015
https://doi.org/10.7322/JHGD.106013
ORIGINAL RESEARCH
"Those who love, vaccinate": parental perceptions of HPV vaccination
Ellen Dias de Oliveira Chiang BSI; Misha L. Baker MPHII; Daniella Figueroa-Downing MPHIII; Maria Luiza Baggio BAIV; Luisa Villa PhDV; Jose Eluf Neto MDVI; Craig Hadley PhDVII; Robert A. Bednarczyk PhD MSVIII; Dabney P. Evans PhD MPHIX
IDepartment of Anthropology, Emory College, Atlanta, GA, USA
IIEmory University, Rollins School of Public Health, Department of Behavioral Science and Health Education, Atlanta, GA, USA
IIIEmory University, Rollins School of Public Health, Departments of Epidemiology & Global Health, Atlanta, GA
IVInstituto do Câncer do Estado de São Paulo, ICESP, São Paulo, Brazil
VInstituto do Câncer do Estado de São Paulo, ICESP; Department of Radiology and Oncology, School of Medicine, University of São Paulo, Brazil
VIDepartment of Preventive Medicine, School of Medicine, University of São Paulo, Brazil; Fundação Ococentro de São Paulo, FOSP, São Paulo, Brazil
VIIEmory University, Department of Anthropology
VIIIEmory University, Rollins School of Public Health, Departments of Epidemiology & Global Health; Cancer Prevention and Control Program, Winship Cancer Institute; Emory Vaccine Center, Atlanta, GA
IXEmory University, Rollins School of Public Health, Departments of Behavioral Science and Health Education & Global Health, Atlanta, GA, USA
ABSTRACT
INTRODUCTION: In March 2014, Brazil began its national HPV immunization campaign targeting girls ages 9-13
OBJECTIVE: Describe determinants of parental decisions to vaccinate their daughters against HPV
METHODS: In this qualitative study, thirty semi-structured interviews were conducted at five health posts in São Paulo, Brazil. Interview questions explored parental opinions of disease prevention methods, vaccines in general, and the HPV vaccine. Interviews were analyzed using grounded theory
RESULTS: Overall, parental knowledge about HPV and the vaccine was low, yet most eligible daughters had been vaccinated. Parents perceived the HPV vaccine to be normal, preventative, and protective. Parents viewed themselves as accountable for their children's health, and saw the vaccine as a parenting tool for indirect control. Trust in healthcare professionals and an awareness of the dangers of "nowadays" (uncertainties regarding disease and sexual behavior) were also important in vaccine decision-making. These factors held more explanatory power for decisions to vaccinate than parental knowledge levels. This was the first study to qualitatively examine the perception of publically provided HPV vaccination among parents with eligible daughters in Brazil. The findings help interpret the greater than 90% coverage for the first HPV vaccine dose in Brazil. The results indicate that attempts to understand, maintain, or modify vaccination rates require the consideration of context specific factors, which influence both parent perspectives and vaccination decisions
CONCLUSION: HPV knowledge levels are not predictive of parental decisions to vaccinate daughters. Context specific factors from the sociocultural dimensions of parenting, sexuality, gender, and the healthcare system are more influential in vaccine decision-making
Keywords: Brazil, papillomavirus, vaccination, parental perceptions, adolescent health.
RESUMO
INTRODUÇÃO: em Março de 2014 o Brasil lançou uma campanha nacional de vacinação contra o HPV para meninas de idades 9 a 13. : Descrever determinantes das decisões dos pais para vacinar as filhas contra HPV
MÉTODO: neste estudo qualitativo foram realizadas trinta entrevistas semi-estruturadas em cinco UBSs em São Paulo. A entrevista examinou as opiniões dos pais sobre métodos de prevenção de doença, vacinas em geral e a vacina contra o HPV. As entrevistas foram analisados utilizando grounded theory
RESULTADOS: no geral os pais demonstraram baixo conhecimento sobre HPV e a vacina contra o HPV. Apesar disso a maioria das meninas elegíveis foram vacinadas. Os pais consideraram a vacina contra o HPV normal, preventiva e protetora e se identificaram como os responsáveis pela saúde dos filhos e descreveram a vacina comouma forma indireta de controle dos pais. Confiança em profissionais de saúde e os perigos de "hoje em dia" (dúvidas em termos de doenças e relações sexuais) mostraram-se importantes nas decisões de vacinação. Estes fatores tiveram maior poder explicativo para as decisões de vacinação do que os níveis de conhecimento dos pais.Este foi o primeiro estudo que examinou qualitativamente o propósito da vacinação contra o HPV entre pais de meninas elegíveis no Brasil. Os resultados ajudam a interpretar acobertura superior a 90% para a primeira dose da vacina contra o HPV no Brasil. Estes resultados indicam que esforços direcionados a entender ou modificar taxas de vacinação exigem a consideração destes fatores que são específicos ao contexto e direcionam perspectivas e decisões de vacinação
CONCLUSÃO: conhecimento dos pais sobre HPV talvez não seja preditivo para a vacinação das filhas. Fatores específicos ao contexto sociocultural de parentalidade, sexualidade, gênero e o sistema de saúde influenciaram na decisão de vacinação
Palavras-chave: Brasil, papillomaviridae, vacinação, percepções de pais, saúde do adolescente.
INTRODUCTION
Vaccination is a hallmark of public health and is revered as a cost effective intervention for combating the burden of infectious diseases in a population through prevention. Significant vaccine uptake within a population creates herd immunity in which individual protection from immunization extends to the community level thus maximizing vaccination benefits. Coverage rates for the Human Papilloma Virus (HPV) vaccine have varied both within and between different countries, even in countries with funding sufficient for widespread vaccination1.
HPV has been identified as a necessary cause for cervical cancer2. HPV, types 16 and 18 are found in about 70% of cervical cancer cases and are classified as human carcinogens3. Cervical cancer is the third most common cancer among women ages 14-55 with an estimated 527,624 new cases and 265,653 deaths per year4.For women in Latin America and the Caribbean, cervical cancer is the second most common cancer and the second leading cause of cancer deaths5. Brazil has an estimated 18,503 annual cervical cancer diagnoses of which 68.5% are attributable to HPV-16 or -184.
The prophylactic HPV vaccines help prevent HPV infections. The bivalent vaccine targets HPV types 16 and 18, whereas the quadrivalent vaccine also protects against HPV types 6 and 11, which are associated with genital warts. In March 2014, Brazil began its national HPV immunization campaign targeting girls aged 9-13; by 2016, the quadrivalent HPV vaccine will be available free of charge to all nine year old girls through the Brazilian National Immunization Program (PNI). The first phase of the HPV vaccination campaign occurred through in-school vaccination days and catch up immunizations took place in Basic Health Units (UBSs), which are the primary care centers of the Brazilian Unified Health system (SUS). Prior to the campaign, HPV vaccines were only available through private clinics and just 2.4%, 2.0% and 0.4% of girls ages 10-14 had received the first, second, or third doses respectively6. As of December 2014, coverage for the first HPV vaccine dose among 11-13 year olds reached 99%, surpassing the 80% target level7. The high uptake suggests that the HPV vaccination campaign mitigates some of the barriers to HPV vaccine access that stem from social inequalities (e.g., access to private clinics). Administration of the second dose began in September 2014 and the third dose will be available 5 years after the first dose, following an extended vaccination schedule8. However, access alone is not sufficient for significant uptake if parents are not receptive to vaccination.
Few studies have assessed the levels of HPV knowledge in Brazil prior to the 2014 HPV immunization campaign. In a group of college students from São Paulo, 69% of males and 76% of females knew that HPV is sexually transmitted. These percentages were lower relative to knowledge levels for HIV, syphilis, genital herpes, and gonorrhea9. Similarly, among 283 Brazilian students surveyed between the ages of 18 and 23 in São Paulo, the majority had heard of HPV, but had a limited understanding of HPV transmission and its related diseases10. Among low income primiparous women in São Paulo, only 37% had reported ever hearing of HPV, 19% knew that HPV is an STI, 7% knew HPV could lead to cervical cancer, and only 0.7% knew that HPV could cause genital warts. Despite these low HPV knowledge levels, all of the participants said they would accept the HPV vaccine if it were offered11.
In a study conducted in Barretos, Brazil prior to the national campaign, 88.2% of parents with eligible daughters from a sample of schools agreed to participate in an in-school HPV vaccination program. Of their daughters, 87.5%, 86.3%, and 85.0% received the first, second, and third HPV doses respectively12.Another study prior to the campaign examined the intentions of 538 parents to vaccinate their children against HPV in Campinas, Brazil. Only 40% of parents had heard of HPV and of these parents, less than 30% had adequate HPV knowledge levels. Additionally, only 8.6% of parents had heard of the HPV vaccine. Of those that knew about the HPV vaccine, 95% said they would vaccinate their children if it were publically available13. Thus these studies suggest recepti-veness to HPV vaccination prior to the campaign despite limited knowledge of HPV.
Another study explored childhood vaccination decisions within a sample of parents from the highest socioeconomic strata in São Paulo. Parents were classified as either vaccinators, selective vaccinators, or nonvaccinators. All parents based their vaccination decisions on the intention of protecting their children, but differed in how they interpreted the harms of vaccination. Parents that either selectively vaccinated or did not vaccinate at all acknowledged that their decisions not to vaccinate threatened their reputations as parents due to the prevailing cultural consensus in which a vaccinated child is indicative of a good parent14.
Several studies have examined the associa-tion between parental knowledge of HPV and adolescent HPV vaccination coverage. Some studies suggest a positive relationship between parental knowledge of HPV and the vaccine with HPV vaccine acceptance15,16. To the contrary, studies among parents in Turkey, the US, Indonesia, the UK, and the Netherlands have found that knowledge of the HPV vaccine is not necessarily correlated with vaccine acceptance or uptake17-23. Beliefs about vaccines in general may be more strongly associated with HPV vaccine acceptability.
Perceiving vaccination as beneficial was associated with increased acceptability of the HPV vaccine in various studies20, 23,24.Additionally, trust in vaccine recommenders (i.e. healthcare professio-nals) might outweigh parents' vaccine safety concerns. The provision of information is not always enough to motivate vaccination and trust in health care providers mediates how parents assess the validity of healthcare recommendations and biomedical information25.
Proximate causes of vaccination such as an individual's HPV knowledge level are situated within larger social conditions. These social influences include both the values that contextualize the meaning of vaccination and the conditions that impact health and access to health care. Understanding vaccination behavior and implementing any intervention to increase vaccination coverage requires the consideration of these distal influences26.
The biomedical framework only partially contributes to the understanding of vaccination. Local vaccination culture encompasses other factors like personal and familial histories of disease, previous healthcare experiences, beliefs about parenting, beliefs about the body and health, gender roles, and trust in health professionals and biomedicine - all of which shape the view of a vaccine and its target disease. The cross-cultural variation in these factors explains why different patterns in vaccine uptake can occur even though the biomedical or scientific presentation of the vaccine is consistent27.
HPV vaccination is not just a matter of biomedicine; it intersects the realms of parenting, sexuality, gender roles, power structures, stigma, and social inequality. With these considerations in mind the objectives of this study are to: (1) Explore the meaning of HPV vaccination for this sample of parents (2) Identify the distal factors that shape this meaning (3) Determine whether HPV knowledge levels are predictive of HPV vaccination within this sample.
METHODS
This study was part of a larger research project, Human Papillomavirus Vaccination in São Paulo, Brazil: Perceptions and Implementation, which includes a quantitative assessment of health care provider knowledge, attitudes, and practices about HPV vaccination. For the present study, we designed an original semi-structured interview guide with a demographics section and qualitative questions on six major themes. These questions explored parent opinions of disease prevention methods, the HPV vaccine, and vaccines in general. This guide was translated into Portuguese and back translated into English before its implementation.
The study took place in five Basic Health Units (UBS) that are part of Projeto Região Oeste (PRO), a network of UBSs managed by the University of São Paulo (USP).Upon arrival, individuals in the waiting areas were screened for eligibility. Inclusion criteria included being over the age of 18; being Brazilian and a resident of São Paulo; and having at least one female child between the ages of 9-13. Once each participant was recruited and taken to the private interview location, both verbal and written consent were obtained. The first author conducted the semi-structured interviews in Portuguese. All interviews were conducted over two weeks from the end of July to the beginning of August 2014.
Each interview recording was transcribed directly in Portuguese. All 30 transcripts were uploaded into MAXQDA in Rich Text Format for coding. Interview text was analyzed inductively following the principles of Grounded Theory. Open coding involved line-by-line examination of the transcripts and helped conceptualize the themes present in the interviews. During this phase, all new identified concepts were coded. Focused coding then collapsed these specific codes into broader, overarching thematic codes.
To maintain confidentiality, each participant was assigned a unique identifier and only these identifiers appear in the results section. All research materials were stored or uploaded to a secure location. This study protocol was reviewed and approved by the city of São Paulo (CAAE 31.771.314.6.3001.0086) and the Institutional Review Boards from Emory University and USP (CAAE 31.771.314.6.0000.0065).
RESULTS
Participant demographics
A total of 30 parents were interviewed with no exclusions from data analysis. The participants were mainly female (87%) and half of them lived with a significant other (50%). The average age of the parents was 38 years and many had 1-2 children (46.7%). The average monthly household salary for this sample was about USD 630 (BRL 2,033.57), and the median income was USD 495.66 (BRL 1,600.00). Based on the categorization of the Brazilian Institute of Geography and Statistics, households with this income belong to the socioeconomic Class D based on a ranking of A through E with Class A being the highest.
Low knowledge of HPV
Participants were asked to describe every-thing they knew about HPV during the interview. Their responses were then scored on a knowledge scale of 0 to 4 based on the criteria listed in Table 1.
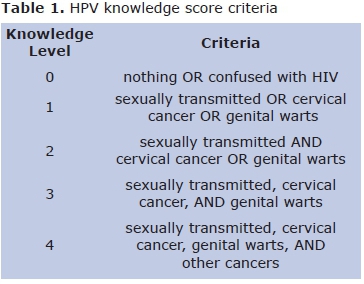
Only one parent had the highest possible knowledge score of 4 and eight (26.7%) of the parents reported no knowledge of HPV. Four of the latter had vaccinated their daughters. The average HPV knowledge scores among this sample of 30 parents were similar and all below a score of 2.
Two of the parents could not distinguish HPV from human immunodeficiency virus (HIV). Several parents knew that HPV is primarily sexually transmitted, but also proposed incorrect, alternative modes of HPV transmission. However, lack of knowledge did not determine support for vaccination as portrayed by one parent's comment about the HPV vaccine: "HPV, I still don't know what that means, but I think if something can prevent a disease, then of course that's a good thing and not a bad thing."
HPV vaccination status
The majority (87.5%) of the participants' daughters that met the age criteria of the campaign's first year had been vaccinated at the time of the interview. The two parents with eligible daughters that had not yet been vaccinated were not aware of the immunization campaign before the interview, but expressed interest in vaccinating their daughters after learning that the vaccine was publicly available. Two of the parents with eligible and vaccinated daughters realized their daughters had received the HPV vaccine through the interview conversation. One daughter had gone to the health post to receive the vaccine even though her parent did not know specifically what vaccine she received:
"She got vaccinated here, downstairs. I think it was for the HPV virus. I don't know. They were vaccinating adolescents through a campaign that was held here. Oh, I don't know if it was for HPV. I don't know. I know it was in the vaccination room, here in this health post, that she was vaccinated. A lot of adolescents came here that day so I brought her."
The second parent was uncertain of her daughter's vaccination status because her husband had taken their daughter to be vaccinated. After discussing the timing and specifics of the vaccination with both parents, it was concluded that both girls had indeed been vaccinated against HPV.
All but one of the parents of unvaccinated and ineligible daughters expressed interest in vaccinating their daughters through the public sector once the age criteria was met. Although supportive of HPV vaccination for both girls and boys in general, the one hesitant parent of this group worried about her daughter's ability to handle the vaccine:
"I am afraid that she will have a reaction because she is very delicate, you know, with vaccines. She has bronchitis so I am afraid. I am afraid that she will get tired, that the asthmatic bronchitis will be triggered... that a reaction will stop her heart."
These concerns existed even though the parent reported that her daughter had never experienced adverse reactions to other vaccines outside of once developing a cold after flu vaccination. The parent believed that vaccination is an effective way to prevent disease, but vaccinating at a time when her daughter is already "big", or grown up, seemed strange.
A parent with personal experience with HPV associated genital warts and cervical cancer intended to purchase the vaccine for her nine-year-old daughter if the vaccine was to become no longer publicly available:
"If I have the financial means, I will pay for her to be vaccinated because I am aware of its importance and of the importance of my daughter in my life and of the life she has ahead of her. For her to have a good adolescence...for her to climb the steps in her life with health because without health, you go nowhere. I would have preferred it a thousand times more to have paid, to have been able to pay to have myself vaccinated, than to have gone through the entire process I went through."
Perceptions of vaccination
Normal: "It's just another vaccine."
Among the 30 parents interviewed, the HPV vaccine was generally perceived as fitting into the existing vaccine framework:
"It's just another vaccine".
One parent's words:
"... I agree with all the terms of vaccination,"
reflects the prevailing stance on vaccination among the interviewed parents. For some parents, witnessing the benefits of previous vaccination initiatives, such as the campaign against polio, contributed to the normalization and positive perception of HPV vaccination.
The general approval of vaccination continuously reemerged throughout the interviews. For example, when asked why a parent might choose not to vaccinate a daughter against HPV, several participants expressed surprise at the notion that a parent would actively choose not to vaccinate their daughter. One parent stated that it would be impossible for a parent to know that the HPV vaccine is available at the health post and choose not to vaccinate his or her daughter. In agreement with this sentiment, yet another parent expressed:
"...if the health posts have the [HPV] vaccine, why not vaccinate?"
The following quote exemplifies the notion that vaccination generally goes unquestioned in this population:
"Are there cases where parents refuse [vaccination]?
A reason to refuse a vaccine for your child, gosh, I've never thought about this before."
The opinions that "every vaccine should be taken" and "...if you don't vaccinate, I think you are acting incorrectly" further demonstrate that vaccination is highly regarded and expected. One parent went so far as to say that vaccine refusal reflects stupidity:
"They must be a bunch of idiots. A bunch of idiots that don't want their daughters to be vaccinated. Vaccines don't cause any problems, it's for the good of the child, it doesn't harm an adolescent or a child."
In general, several parents called for increased investment in vaccine development. Accordingly, new vaccines seem to be well received among the majority of these parents: "Every time there is a vaccine to be given, I always come to this health post to vaccinate them. My children's vaccinations are all up to date." Some participants mentioned that the introduction of the vaccine was well accepted in their communities. One parent recounted that several daughters, who had missed in-school vaccination administration, were taken by their mothers to receive the vaccine at the health post. Likewise, most parents did not know of anyone who is against the HPV vaccine or vaccination in general. The positive perceptions of vaccination that extended to the HPV vaccine were also supported by the fact that some parents believed the vaccine should be available to everyone (regardless of age and gender) and specifically, some mothers wished that they themselves were eligible for vaccination.
Preventative & protective
The significance of vaccination was often attributed to its preventative use, for example:
"It's better that you prevent a disease so I believe the vaccine is important, yes, I believe that... The invention of the vaccine is a wonderful thing."
The need to plan for the future was intertwined within these discussions about vaccination for prevention:
"... she's taking it so that nothing happens tomorrow."
Opposite to the worry that HPV vaccination might increase risky sexual behavior, one parent said that the vaccine could increase an adolescent's awareness of the need to prevent sexually transmitted diseases.
Vaccination for protection also emerged as a theme throughout the interviews. One mother commented on the protective role of vaccination and the inequalities in health care services:
"I've always thought that the best way for us to defend ourselves from all diseases is only through vaccination, but not every disease has a vaccine, only some do. I think the ideal would be to have a vaccine for all types of disease but that doesn't exist and if it does exist, we have to pay for it and the poor can't afford it."
Parental responsibility for preserving health
Preservation of a child's health fell into the domain of parenting for all of the interviewed parents. This parental concern and sense of responsibility leads many parents to identify themselves as having the final say in their children's healthcare decisions. This mother reiterated her authority over her child's health:
"In regards to my daughters, I am the one who decides what they will or won't do. No one changes my opinion. I change my opinion, no one changes it for me so I don't care about what other people say. I'm very decisive. Once I decide, I stick to my decision."
Parental authority applied to girls eligible for HPV vaccination, who were described as reliant on their parents for healthcare decisions:
"...in terms of her health, I, her father, am the greatest authority over her."
Thus the practical decision of whether or not to vaccinate against HPV is the decision of the parent, not the daughter.
Vaccines: A parenting tool
Disease prevention through vaccination was seen as an effective tool for carrying out the parental duty of maintaining health. One parent said:
"... parental involvement influences the child's well-being. Prevention and care are part of love. If you take care of your child, you love. If you love, you take care of your child."
Likewise, another parent stated: "Those who love, vaccinate. We love our children so we vaccinate them."Vaccination "is a precaution that every parent has with their children, not just with the HPV vaccine, but with any other vaccine."
Along these lines, some parents said that a parent's decision not to vaccinate his or her daughter against HPV results from a lack of concern for the daughter's health. Thus choosing to vaccinate was overall portrayed as a straightforward decision for any parent. For this parent the vaccination decision process is obvious:
"I don't think you need to be a genius. You don't need to be very knowledgeable in order to understand [the importance of vaccina-tion]... do you want your child sick?... Do you want your child with cancer... with a bunch of warts everywhere? If not, then this [vaccination] is the way to avoid it. End of discussion."
Sick child, bad parent
A sick child becomes a reflection of parental shortcoming. This parental accountability creates a situation in which a sick child can make parents feel "a type of guilt I don't want to experience." or fearful of blame. The decision to vaccinate operates within this guilt/blame paradigm. For example, if her child were to one day become sick from a vaccine preventable disease, one mother said she would only blame herself for "letting this happen" to her daughter by not having her vaccinated. Decisions to vaccinate thus mediate any future blame or guilt that would emerge from a sick child. The strict adherence to the recommended childhood vaccinations provides some protection from possible blame:
"So if she does get one of these diseases, no one can tell me that I didn't keep my daughter's vaccination card up to date. I will be able to say that she is sick as a consequence of their incompetence. I would have the right to say that. This is why I prefer to always keep their vaccinations up to date. For this very reason, both to protect them and so that others don't have anything to say about me in the future."
One parent noted that future blame could come from the daughter herself because of her dependence on her parents during the HPV vaccination age:
"Your daughter will be independent in the future. She is going to make her own choices. You make them now, but in the future, she will. Then what? What if she has sex and gets HPV? She's going to ask you: mom, why didn't you vaccinate me? Then what?"
Indirect parental control
A daughter's future independence was a recurring theme in the dialogues supporting vaccination. This independence results in a loss of parental control over a daughter's actions, which adds another layer of uncertainty to the already unknown domain of adolescent thought. Because of the sexually transmissible nature of HPV, a girl's sexual independence was the focus of these conversations:
"You can't look at the situation and say: why vaccinate if the child won't have sex? Do I know that? Does she know that? We know and live with our daughters and everything, but we don't know their thoughts and sometimes it's completely different [from ours]."
Across the board, parents acknowledged that they only have indirect control over their daughters' sexual lives. This control was primarily implemented through sex education at home, which could direct their children to approach sex more cautiously.
According to the participants, the suggested age for sex education ranged from 10 to 17 years. Many parents described the ideal time not in terms of age, but in terms of the transition into becoming a mocinha. A mocinha represents a phase between being a child and becoming a woman, which encompasses both elements of adolescence and puberty. Characteristics of a mocinha include menstruation, sexual curiosity, and discovering one's body.
Vaccines: Insurance for the unknown
The HPV vaccine is perceived as crucial for addressing these shortcomings and becomes another tool for indirect control over a child's future. Through this interpretation, the HPV vaccine protects the parent's conscience and reputation by protecting the child's health. Parents stated that they did not know whom their daughter would choose as a sexual partner and since you "can't see the disease," you don't know who has the virus, which is why you should "at least be vaccinated." Factoring in the daughter's unknown future state of immunity also increased the push for vaccination. Since sexual activity was presented as inevitable, the role of the parent was not to prevent sexual activity, but to prevent possible consequences of sexual activity. Thus, HPV vaccination was considered "... a protection for when they become sexually active, because no one is free from having their children [become sexually active]."
Nowadays
Almost all of the parents reflected on how things are "nowadays", which reinforced the need for vaccination to protection against growing risks and uncertainties of the present day. Two points were repeated among the parents. Firstly, nowadays there are more diseases to protect against and old ones are reemerging in stronger forms. Secondly, society today is more "advanced":
"Today's generation is too advanced so I think there is a need for the [HPV] vaccine. Today's youth doesn't care about anything. They get drugged up, they drink, all to lie with anyone. It's much easier to do so nowadays. Everything is more visible, easier."
The general consensus among participants was that children nowadays are initiating their romantic and sexual lives sooner, and sometimes carelessly. Parents referred to pregnant adolescents as justification for their perceptions of the sexual behavior of the youth. Adolescents of this generation were said to be unconcerned with prevention. For most parents, this meant not wearing condoms or using birth control. When specifically talking about their children, some parents expressed trust in their daughters. Uncertainty in these cases came from not knowing the sexual history of their daughter's sexual partner.The HPV vaccine acts as a safeguard against this perceived contemporary trend of risky sex among adolescents.
Males should be vaccinated against HPV
All participants were in favor of having the HPV vaccine available for adolescent boys as well. Even those who did not previously know that males are also susceptible to HPV infection or viewed women as more susceptible to infection, voiced support for vaccinating boys. Many parents believed that boys are more prone to risky sexual behavior and less likely to be health conscious. These attitudes did not appear to differ between parents with only daughters and parents with both sons and daughters. Boys focus their concerns on maximizing their sexual experiences, without much thought to their sexual health:
"Boys aren't concerned with who they have sex with. Today's adolescents don't think about quality, they only pay attention to quantity. It's very much like this these days. They count how many women they got with."
In agreement to the previous statement, women were described as not only being more health conscious, but also being more interested in disease prevention. According to one parent, men only seek healthcare services when they are out of options:
"Men don't prevent anything. Men are more afraid than women...if you come to a health post you see almost no men. There are more women around then men. Men only come when they are seriously ill and have to come because they don't want to die. They only come in these types of situations."
Some parents believe this difference exists because women are more susceptible to disease and/or HPV infection. The multitude of health exams for women supported this perceived difference in disease susceptibility for one father. In contrast, men were primarily described as disease transmitters; it is perceived that men are less likely to get sick and more likely to pass diseases to women. Likewise, the health consequences of HPV infection seemed less severe to one parent: "for men it [HPV] doesn't change much because the most that they could get are those warts so it [HPV] is more harmful for women."
Trust in health professionals
Within the interviews (fix idention) trust in health professionals emerged as a theme.For one parent, trust in biomedicine contributed to her trust in health workers: "...I think that medicine is evolving more and more each day, looking for disease cures. I think it's great." According to another parent, HPV vaccine skeptics should be directed to a professional from a health post:"...I believe in vaccines, I believe in the information so if someone tells me otherwise, I would say: I'm sorry, but you should inform yourself, look for a health professional, someone that can help inform you." A mother whose daughter was vaccinated against HPV received criticism from a coworker, but stood by her decision due to her faith in the health professionals:
"She [coworker] said: 'If I had a daughter the same age as yours, I wouldn't take her.' But I didn't pay attention to her comment. I ignored it and didn't care. If the doctor, the nurse said that this vaccine will prevent my daughter from having the disease in the future, then it isn't going to harm my daughter."
In addition to a trust in health profes-sionals, some parents also trust vaccination recommen-dations from the Ministry of Health. Exposure to the topic of HPV at a health post incentivized one mother to accept having her daughter vaccinated. Health posts may serve as credible sources of health information for these parents. When asked about her belief in the efficacy of HPV vaccination, another parent mentioned the Ministry of Health's TV advertisement about the campaign: "...I saw something on TV...but I don't really know anything about it [the HPV vaccine]...so I'm sure that if they say it is [effective], then it is." One parent's commentary focused on the notion of compliance rather than trust, noting that if the government mandates a certain vaccination, then the public will comply and go to the posts to get vaccinated.
The results from this research identify some of the distal influences on HPV vaccination decisions by characterizing the local HPV vaccination culture based on the perceptions of a subset of parents from São Paulo, Brazil. In doing so, the strength of HPV knowledge levels for predicting vaccination was also investigated. This was the first study to qualitatively examine the meaning of HPV vaccination among parents with eligible daughters in Brazil and the role of HPV knowledge in vaccination decisions. The findings provide part of the foundation necessary for interpreting the greater than 90% coverage for the first HPV vaccine dose in Brazil.
DISCUSSION
HPV knowledge is not predictive of vaccination
Knowledge of HPV was low among all parents and was not predictive of vaccination within the interviewed sample. Compellingly, half of the parents with vaccinated daughters had HPV knowledge scores of 0, implying that knowledge, in these cases, was not at all part of their decision to vaccinate. The poor predictive value of HPV knowledge aligns with several studies that found no association between parental HPV knowledge and HPV vaccine uptake among their daughters17, 18,20-22
A culture of vaccination
The interviews reflected a prominent culture of vaccination, where the decision to vaccinate appears to be less of an independent decision and more of a cultural expectation. The overwhelming majority of participants supported all vaccinations, although a couple mentioned having doubts about the flu vaccine. Previous positive experiences with vaccination, including childhood vaccinations, perpetuate current positive perspectives of vaccines and subsequently, the normalization of vaccination. Additionally, in-school vaccination could have further normalized HPV vaccination, especially since vaccine administration was set up as an opt-out choice.
The HPV vaccine and vaccines in general were described as normal, preventative, and protective. Other studies have also identified that confidence in the benefits of vaccination is associated with HPV vaccine acceptance17, 20, 23,24. It is critical to recognize that the preventative and protective aspects of vaccination described within this sample were not confined to the biomedical realm. In addition, many parents desired greater vaccine access in terms of both new vaccine development and a broader target population for the HPV vaccine. All of the positive perceptions and actions mentioned above become part of a cyclical relationship that maintains the culture of vaccination from which they originated.
Trust in biomedicine
The culture of vaccination within this sample is linked to trust in biomedicine and the health care system. The majority of parents expressed their reliance on the healthcare professionals in the health posts for their health related questions. Trust in biomedicine extends to trust in the Ministry of Health and its guidelines. For the HPV immunization campaign, the Ministry of Health produced advertisements about the campaign. Trust in these messages effect how parents evaluate the validity of health information and the effectiveness of health services.As other studies have found, the persistence of trust in these recommending bodies minimizes the need for parents to personally research and evaluate the claims because they trust that recommendations are based on credible information25,28,.
Although the overall high trust level has proven beneficial to reaching high vaccine uptake, this degree of trust could have negative implications if the interests of the government or biomedicine were to no longer align with the public's best interest. This trust might also prevent individuals from gaining a better understanding of the health services they receive.
Everyone should be protected
Perceived gender differences within the realm of health and sexuality contributed to the acceptance of HPV vaccination for both boys and girls. Boys and men, according to the participants, function as disease transmitters in society, which is supported by similar results among a survey of Brazilian students10. For some participants, the difference in disease susceptibility translated into differences in health care utilization. Parents identified women as more cautious and involved in disease prevention whereas men were portrayed as careless and reluctant to visit health posts.
Likewise the consequences of HPV infection appeared to affect women more severely than men and, consequently, HPV vaccination for women is critical. Nonetheless, all participants favored HPV vaccination for boys as well as girls, which is a new finding. The normalization of vaccination and its preventative and protective functions contributed to approval of HPV vaccination for boys. Learning that HPV has health consequences for men from the educational blurb has likely further strengthened parental support for vaccinating "both sides." Presently the HPV vaccine is available at all Basic Health Units to girls aged 9-13 and to HIV positive girls and women aged 9-26.
HPV vaccination: Parental insurance
Parents described themselves as responsible for both maintaining their child's health and making their healthcare decisions. Vaccination, in general, was perceived as effective for preserving health and as a tool for exerting parental duty. Thus a child's vaccination status is used to evaluate parental ability because choosing not to vaccinate is widely perceived as putting the child's health at risk.
The dependency on parents for healthcare decisions also introduces the possibility that the blame for a sick child will be directed towards the parent, which has emerged as a theme in related research14. Parents used this blame/guilt paradigm to explain their support for the HPV vaccine. From this perspective, it appears likely that the HPV vaccine will shift part of the blame for cervical cancer from the affected individual to the individual's parents and/or the health care system providing the vaccine.
The need for vaccination to provide parental insurance is amplified by the unknowns and conditions of "nowadays". Several parents mentioned that there currently seems to be a greater number of diseases to protect against or a resurgence of previously controlled diseases. The unknown future health status of the child amplifies these disease risks. A daughter's sexual life is seen as inevitable and largely out of direct parental control. Girls will therefore become sexually active based on the social conditions nowadays and not because of HPV vaccination.
This perspective differs from concerns that HPV vaccination and risky sexual behavior are not independent from one another, which have been reported in some studies among parents from the U.S.29.These parents perceived that HPV vaccination protects against the unknown specifics of sexual activity such as with whom and when the sexual activity will begin. Sex education from home, school, or the health post was portrayed as a critical preventative tool as well. The HPV vaccine therefore adds another layer of protection from the uncertainties that can lead to sickness and subsequent parental blame and guilt.
This study suggests that parental decisions to vaccinate against HPV can be better understood by examining the culture of vaccination from which the vaccine gains more than just a biomedical identity. The strength of the PNI in mitigating socioeconomic inequalities in health by providing the HPV vaccine in public clinics increases vaccine uptake not only through increasing access, but also through its role in the normalization of vaccination. The social, political, and cultural context in which HPV vaccination occurs determines the meaning of the vaccine to parents and consequently influences their vaccination decisions. The results show that for the majority of the interviewed parents, HPV vaccination is an act of parental love that provides both health and social protection against the many unknowns that affect a child's health. This interpretation of vaccination is driven by the prevailing culture of vaccination acceptance, which is mediated by trust in the Ministry of Health and healthcare workers and has normalized vaccination. HPV vaccination encompasses not just issues of health, but also includes the sociocultural dimensions of parenting, sexuality, gender, and government responsibility. These factors held more explanatory power for decisions to vaccinate than parental knowledge levels of HPV. The results indicate that attempts to understand or modify vaccination coverage require the consideration of these distal factors, which are context specific. Major changes in parental perspectives of HPV vaccination could be tracked if similar interviews were conducted after the administration of the 2nd and 3rd doses of the HPV vaccine and then compared to results of this baseline study.
The conclusions from this study are limited by the size and representativeness of the study participants; however thematic saturation was reached among this sample. A larger sample size would reduce potential biases and might capture a wider range of perspectives. The study results were largely shaped by the opinions of mothers since there were only four interviewed fathers. Because sampling took place in health posts, the results also do not capture the opinions of those that do not visit or are unable to get to health posts. Thus, barriers to accessing healthcare are not addressed in this study.
Additionally, those attending health posts may have felt more positively overall towards the publicly administered health system. The perspectives of parents who are against HPV vaccination or choose to vaccinate in private clinics are also important for understanding HPV vaccination in Brazil, but were not present in this study. Access to the HPV vaccine and the meaning of vaccination may also differ across different Brazilian populations. Future studies should therefore address these issues of represen-tation and capture a wider range of the Brazilian population in order to provide a more accurate depiction of the dialogue surrounding HPV vaccination in Brazil. The impact of media coverage on adverse HPV vaccination events on the coverage rate of the second HPV dose should also be examined in future studies.
CONCLUSION
HPV knowledge levels are not predictive of parental decisions to vaccinate daughters. Context specific factors from the sociocultural dimensions of parenting, sexuality, gender, and the healthcare system are more influential in vaccine decision- making.
ACKNOWLEDGEMENTS
The authors would like to acknowledge INCT-HPV, FFM-USP, and Ricardo Góes Stanys for providing local support. The authors also thank Dr. Marcia Couto for her suggestions regarding the interview instrument.The authors would also like to acknowledge Ms. Samantha Luffy for her review of the manuscript prior to submission. This work was funded by the Emory University Global Health Institute and a Scholarly Inquiry and Research at Emory (SIRE) Grant. The Scholarly Writing and Academic Publishing program of the Emory University Center for Faculty Development and Excellence and grant INCT-HPV, FAPESP Proc. Nr. 2008/57889-1; CNPq Proc. 573799/2008-3 also supported this research.
Author's contributions:
All authors contributed extensively to the work presented in this manuscript. EC, MLB, DF, RB, CH and DPE jointly designed the study. EC and MLB performed data collection and data analysis. EC wrote the manuscript with significant input from MLB, DF, RB, CH and DPE. MLBaggio, LV, JEN, RB, CH and DPE also provided support and supervision throughout the study.
LV is a Board Member for the Quadrivalent HPV vaccine and collaborated with several clinical trials of the vaccine. All oither authors declare that they have no competing interests.
REFERENCES
1. Hopkins TG, Wood N. Female human papillomavirus (HPV)vaccination: global uptake and the impact of attitudes. Vaccine. 2013;31(13):1673-9. DOI: http://dx.doi.org/1016/j.vaccine.2013.01.028 [ Links ]
2. Bosch FX, Lorincz A, Munoz N, Meijer CJLM, Shah KV. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol. 2002; 55(4):244-65. [ Links ]
3. Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsagué X, Shah K V, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 348(6): 518-27. DOI: http://dx.doi.org/10.1056/NEJMoa021641 [ Links ]
4. Bruni L, Barrionuevo-Rosas L, Albero G, Aldea M, Serrano B, Valencia S, et al. ICO Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in India. Summary Report; 2015. [ Links ]
5. Organização Pan-Americana da Saúde (OPAS). Organização Mundial da Saúde. (OMS). Cervical Cancer. [cited 2014 aug 26] Available from: http://www.paho.org/hq/index.php?option=com_content&view= category& layout=blog&id=3595&Itemid=3637 [ Links ]
6. Sistema de Informação do Programa Nacional de Imunizações (SI-PNI). Estratégia de vacinação contra HPV: Percentual da população de 10 a 14 anos vacinada contra HPV em anos anteriores a implantação da vacina HPV pelo PNI-total Brasil-2013. [cited 2014 aug 26] Available from: http://pni.datasus.gov.br/consulta_hpv_14_C07.php [ Links ]
7. Sistema de Informação do Programa Nacional de Imunizações (SI-PNI). Estratégia de vacinação contra HPV: vacinômetro D1; total Brasil-2014. [cited 2014 aug 26] Available from: http://pni.datasus.gov.br/consulta_hpv_ 14_C01.phphttp:///h [ Links ]
8. Ministério da Saúde. Secretaria de Vigilância em Saúde Departamento de Vigilância de Doenças Transmissíveis. Guia pratico HPV perguntas e respostas. Brasília: Coordenação Geral do Programa Nacional de Imunizações; 2014. [ Links ]
9. Caetano ME, Linhares IM, Pinotti JA, da Fonseca AM, Wojitani MD, Giraldo PC. Sexual behavior and knowledge of sexually transmitted infections among university students in Sao Paulo, Brazil. Int J Gynecol Obstet. 2010;110(1):43-6. DOI: http://dx.doi.org/10.1016/j.ijgo.2010.02.012. [ Links ]
10. Costa LA, Goldenberg P. Human papillomavirus (HPV) among youth: a warning sign. Saúde Soc. 22(1):249-61. DOI: http://dx.doi.org/10.1590/S0104-12902013000100022 [ Links ]
11. Rama CH, Villa LL, Pagliusi S, Andreoli MA, Costa MC, Aoki AL, et al. Awareness and knowledge of HPV, cervical cancer, and vaccines in young women after first delivery in São Paulo, Brazil- a cross-sectional study. BMC Women's Health. 2010;10:35. DOI: http://dx.doi.org/10.1186/1472-6874-10-35 [ Links ]
12. Fregnani JH, Carvalho AL, Eluf-Neto J, Ribeiro Kde C, Kuil Lde M, da Silva TA, et al. A school-based human papillomavirus vaccination program in barretos, Brazil: final results of a demonstrative study. PLoS One. 2013;8(4):e62647. DOI: http://dx.doi.org/10.1371/journal.pone.0062647 [ Links ]
13. Osis MJD, Duarte GA, de Sousa MH. SUS users' knowledge of and attitude to HPV virus and vaccines available in Brazil. Rev Saúde Publica. 2014;48(1):123-33. DOI: http://dx.doi.org/10.1590/S0034-8910.2014048005026 [ Links ]
14. Couto MT, Barbieri CLA. Care and (non)-vaccination in the context of highincome and well-schooled families in São Paulo in the state of São Paulo, Brazil. Ciênc Saúde Coletiva. 2015;20(1):105-14. DOI: http://dx.doi.org/10.1590/1413-81232014201.21952013 [ Links ]
15. Davis K, Dickman ED, Ferris D, Dias JK. Human papillomavirus vaccine acceptability among parents of 10-to 15-yearold adolescents. J Low Genit Tract Dis. 2004;8(3):188-94. [ Links ]
16. Kahn JA, Rosenthal SL, Hamann T, Bernstein DI. Attitudes about human papillomavirus vaccine in young women. Int J STD AIDS. 2003;14(5):300-6. DOI: http://dx.doi.org/10.1258/095646203321605486 [ Links ]
17. Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med. 2007;45(2-3):107-14. DOI: http://dx.doi.org/10.1016/j.ypmed.2007.05.013 [ Links ]
18. Dursun P, Altuntas B, Kuscu E, Ayhan A. Women's knowledge about human papillomavirus and their acceptance of HPV vaccine. Aust N Z J Obstet Gynaecol. 2009;49(2):202-6. DOI: http://dx.doi.org/10.1111/j.1479-828X.2009.00947.x. [ Links ]
19. Jaspers L, Budiningsih S, Wolterbeek R, Henderson FC, Peters AAW. Parental acceptance of human papillomavirus (HPV) vaccination in Indonesia: a cross-sectional study. Vaccine. 2011;29(44): 7785-93. DOI: http://dx.doi.org/10.1016/j.vaccine.2011.07.107 [ Links ]
20. Lenselink CH, Gerrits MM, Melchers WJ, Massuger LF, van Hamont D, Bekkers RL. Parental acceptance of Human Papillomavirus vaccines. Eur J Obstet Gynecol Reprod Biol. 2008;137(1):103-7. DOI: http://dx.doi.org/10.1016/j.ejogrb.2007.02.012 [ Links ]
21. Perkins RB, Pierre-Joseph N, Marquez C, Iloka S, Clark JA. Why do lowincome minority parents choose human papillomavirus vaccination for their daughters? J Pediatr. 2010; 157(4): 617-22. DOI: http://dx.doi.org/10.1016/j.jpeds.2010.04.013 [ Links ]
22. Walsh CD, Gera A, Shah M, Sharma A, Powell JE, Wilson S. Public knowledge and attitudes towards Human Papilloma Virus (HPV) vaccination. BMC public Health. 2008;8:368. DOI: http://dx.doi.org/10.1186/1471-2458-8-368 [ Links ]
23. Dempsey AF, Zimet GD, Davis RL, Koutsky L. Factors that are associated with parental acceptance of human papillomavirus vaccines: a randomized intervention study of written information about HPV. Pediatrics. 2006;117(5): 1486-93. DOI: http://dx.doi.org/10.1542/peds.2005-1381 [ Links ]
24. Lazcano-Ponce E, Rivera L, Arillo-Santillán E, Salmerón J, Hernández-Avila M, Muñoz N. Acceptability of a humanpapillomavirus (HPV) trial vaccine amongmothers of adolescents in Cuernavaca, Mexico. Arch Med Res. 2001;32(3): 243-7. [ Links ]
25. Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers' decisionmaking about vaccines for infants: the importance of trust. Pediatrics. 2006; 117(5):1532-41. DOI: http://dx.doi.org/10.1542/peds.2005-1728 [ Links ]
26. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;(esp): 80-94. [ Links ]
27. Streefland P, Chowdhury AM, Ramos-Jimenez P. Patterns of vaccination acceptance. Soc Sci Med. 1999;49(12): 1705-16. [ Links ]
28. Cover JK, Nghi NQ. LaMontagne DS, Huyen DTT, Hien NT, Nga LT. Acceptance patterns and decision-making for human papillomavirus vaccination among parents in Vietnam: an in-depth qualitative study post-vaccination. BMC Public Health. 2012;12:629. http://dx.doi.org/10.1186/1471-2458-12-629 [ Links ]
29. Marlow LA, Forster AS, Wardle J, Waller J. Mothers' and adolescents' beliefs about risk compensation following HPVvaccination. J Adolesc Health. 2009; 44(5):446-51. DOI: http://dx.doi.org/10.1016/j.jadohealth.2008.09.011 [ Links ]
Manuscript submitted Oct 22 2014
Accepted for publication Dec 19 2014.
Corresponding author: Dabney P. Evans, PhD, MPH. E-mail: Dabney.Evans@emory.edu












 Curriculum ScienTI
Curriculum ScienTI

