Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Journal of Human Growth and Development
versão impressa ISSN 0104-1282
Rev. bras. crescimento desenvolv. hum. vol.22 no.3 São Paulo 2012
ORIGINAL RESEARCH
Analysis of the rate of perceived exertion in the assessment of maximal respiratory pressures in children and adolescents
Juliana Souza de OliveiraI; Tania Fernandes CamposII; Raíssa de Oliveira BorjaI; Raphaella Oliveira Elias da SilvaI; Diana Amélia de FreitasI; Laíse Chaves de OliveiraIII; Karla Morganna Pereira Pinto de MendonçaII
IPrograma de Pós-Graduação em Fisioterapia, Universidade Federal do Rio Grande do Norte - UFRN. Avenida Senador Salgado Filho, 3000, Departamento de Fisioterapia, Campus Universitário, Lagoa Nova, Natal, RN, Brasil
IIProfessora Adjunta, Departamento de Fisioterapia - UFRN. Avenida Senador Salgado Filho, 3000, Departamento de Fisioterapia, Campus Universitário, Lagoa Nova, Natal, RN, Brasil
IIIFisioterapeuta graduada pela Universidade Federal do Rio Grande do Norte. Avenida Senador Salgado Filho, 3000, Departamento de Fisioterapia, Campus Universitário, Lagoa Nova, Natal, RN, Brasil
ABSTRACT
OBJECTIVE: To analyze the rate of perceived exertion in assessing maximal respiratory pressures in children and adolescents.
METHODS: We evaluated 144 healthy children and adolescents from seven to eleven years old, 63 boys and 81 girls, students from public and private schools. The instrument used was a digital manovacuometer MVD300 (Globalmed ®, Porto Alegre-RS, Brazil). A maximum of nine maneuvers were carried out, with one minute rest between each maneuver and five minutes between the measurement of maximal inspiratory and expiratory pressures. The rate of perceived effort was determined by Borg scale and was used at four different moments: before measuring maximal inspiratory and expiratory pressures, previously drawn; immediately after the first measurement; after five minutes of rest and immediately after the last assessment.
RESULTS: The children and adolescents' perceived exertion before, immediately after and five minutes after assessment was 7.8 ± 1.8, 9.6 ± 2.5 and 8.5 ± 2.3, respectively. There was a significant increase after measuring maximal inspiratory and expiratory pressures (p < 0.001). The amount of effort decreased significantly with five minutes of rest after maximal respiratory pressures (p < 0.05). The perceived exertion was similar for children and adolescents who underwent up to five or more maneuvers.
CONCLUSION: The assessment of maximal respiratory pressures in children and adolescents proved to be a safe method regarding perceived exertion. It is suggested that the analysis of the rate of perceived exertion may be a common practice during the evaluation of respiratory muscle strength.
Key words: child; adolescent; muscle strength; respiratory muscles; exercise test; perception.
INTRODUCTION
The evaluation of the respiratory muscle strength is an important parameter in clinical practice, since the respiratory muscles are responsible for proper functioning of the respiratory system1,2. The evaluation of respiratory muscle strength is a widely used method to measure respiratory muscle strength3, which can be performed directly by the manometer4-6.
The measurement of maximal respiratory pressures is a rapid, simple, low-cost and noninvasive method6-8 to obtain an index of respiratory muscle strength and specifically involves the measurement of maximal inspiratory pressure (PImax) and maximal expiratory pressure (PEmax)6,9,10. Over the years, maximal respiratory pressures have been conducted in different populations, including being well accepted and reproducible in the juvenile population. The realization of the manometer is useful in monitoring patients of different ages with respiratory and neuromuscular disorders6,7, since these diseases can affect both the respiratory muscle strength and quality of life in this population11. Often in rehabilitation programs, individual training of respiratory muscles is based on measurement of maximal respiratory pressures10.
The PIMax and PEMax are voluntary tests and the efforts are dependent, meaning that, results depend on the efforts of the individual that is being tested. Therefore, the rate of muscle strength can be trusted if the effort is truly maximum12,13. Thus, there is a need for a good understanding of the maneuvers to be performed and the individual's will to cooperate to actually achieve maximum respiratory effort13,14.
Because it is a stress test, it becomes necessary an analysis of subjective responses regarding their perception of effort. The perceived exertion is a concept defined as the subjective evaluation that indicates the person's opinion on the intensity of work and it has been a subject of attention in the literature since 195015,16. The rate of perceived exertion (RPE) may be measured by various measuring instruments, for example, perceived effort by the Borg scale (Borg RPE)17.
The Borg RPE scale is the most commonly used for tests of perceived exertion. It contains 15 points, ranging from 6 to 20 to measure the perception of effort during an exercise18. The advantage of this scale is that the ratings given grow linearly with exercise intensity, frequency rate and oxygen consumption (VO2)16-19. The Borg RPE scale increases safety during tests that depend on effort and also in other interventions that are required while conducting these tests. The perceived exertion have been used for this purpose in different populations20-22.
Thus, an investigation of the perceived exertion during the evaluation of respiratory muscle strength is important in clinical practice, since it is unclear how much effort is been required from the individual who is being tested. Because it is performed in children and adolescents with chronic respiratory or neuromuscular diseases, and it is important to quantify this effort in order to increase the security of the test. Thus, the objective is to analyze the subjective perception of effort in the evaluation of maximal respiratory pressures in children and adolescents aged between seven and eleven years old.
METHODS
Characterization of the research and ethical aspects
This is a cross-sectional study. The procedures were approved by the Ethics Committee in Research of Universidade Federal do Rio Grande do Norte (approval no. 278/2009), in accordance with Resolution 196/96 of the National Health Council. Data were collected after the signing of Terms of Consent by parents and/or guardians. The population consisted of children and adolescents of both sexes, aged from 07 to 11 years old23, and enrolled in public and private schools.
Inclusion criteria
Children and adolescents eligible for the study could not have: a diagnosis of chronic lung, cardiovascular or neuromuscular disease 24; history of recent trauma of the upper airways, chest or abdomen14; fever (three weeks)6,14, flu or cold the week before the procedure5,14; history of smoking5,6,14; evident chest deformity5,14; acute problem of the middle ear14, abdominal hernia, glaucoma or retinal detachment14; neurological and/or cognitive problems14,24; reported use of medications such as inhaled or systemic glucocorticoids, mineralocorticoids, central nervous system stimulants, muscle relaxants or barbiturate medicines24; less than 5 percentile or greater than or equal to 85 based on the curve of BMI for age and sex of children / adolescents between 2 and 20 years of age proposed by the National Center for Health Statistics (NCHS) in 200025.
Exclusion criteria
The following exclusion criteria were adopted: unable to perform the necessary procedures; give up participating on the search; displays any acute respiratory tract disease during the collection period; or absent from class during the entire period of evaluation in school.
Selection of the participants
Data were collected from 27 schools randomly selected by drawing lots. After the random selection of the participant schools, 50 students were randomly selected in each school, 10 in each age (7-11 years old) and among these, five males and five females in each group.
It was sent to the students parents: 1) a letter of presentation of the study, explaining that the documents were received and how they should proceed, 2) the consent term for parents, containing explanations about the objectives, importance and procedures of study, 3) a questionnaire should be answered by those responsible, which contained questions about general health status of the student. After the documentation returned from the parents, the eligible children and adolescents for the study were identified. Those who were able to participate in the study were asked about their willingness to participate.
Evaluation of Maximal Respiratory Pressures
To measure maximal respiratory pressures, it was used the MVD300 digital manometer (Globalmed®, Porto Alegre - RS, Brasil), calibrated from -300 to +300 cmH2O, with a precision of 1 cmH2O, connected to a computer that provided the participant a visual and auditory feedback. The digital manometer was attached to a biological filter disposable and single use.
Initially, after the agreement of the child or adolescent considered able to participate in the study, it was determined which respiratory pressure would be performed first, i.e., PIMax or PEMax. After the draw, the instructions were given regarding the achievement of maximal respiratory pressures, and then the test was started.
The maneuvers were demonstrated and explained verbally in order to get as much understanding as possible from participants. Because the tests were effort-dependent, the participant was asked to undertake as much effort as possible, and associated with this; the examiner provided verbal encouragement during the measurement.
The measurement of PIMax or PEMax was performed according to the method proposed by Souza14, by two trained raters previously assigned. For measurement of PIMax, participants were asked to breathe normally (tidal volume) during three respiratory cycles and after the evaluator's command, they should perform a maximal expiration (residual volume to approximately - VR). The volunteer indicated the end of expiration by a prearranged gesture. At this point, the evaluator occluded the hole that connects the system with ambient air and asked to be made a maximum inspiration (to approximately total lung capacity - TLC).
To the PEMax, guidelines were similar, differing in the fact that the individual first performed a maximum inspiration and then a maximum expiration and that during this measurement was carried out by the evaluator, a manual cheek support of the participants to ensure a lower pressure loss due to the compliance of the oral cavity26.
There were within nine maneuvers to PIMax or PEMax as suggested by Domènech-Clar et al.7 From these, it was obtained at least three acceptable maneuvers (without leakage and lasting at least 2 seconds) and among the acceptable ones it was necessary to have at least two reproducible maneuvers (with values that did not differ from each other by more than 10% of the highest value). However, the last measurement could not be the highest, in which case another measurement was performed14.
It was given one minute of rest between the completion of each maneuver and five minutes between the measurement of maximal inspiratory and expiratory pressures27. Throughout the test the volunteer sat comfortably at an angle of 90° hip and his back against the chair. Importantly, the evaluations occurred within the time range of schools, to be avoided that children and adolescents perform maneuvers after they are fed and carried out physical effort.
Evaluation of perceived exertion
The perceived effort was determined by the Borg RPE scale17, which is a vertical scale quantified 6-20, where 6 represents no symptoms and 20 represents the maximum extent providing an individual, and momentary direct perception of effort. The scale has verbal attributes next to the numbers for a better understanding ("no effort"; "lightweight", "very light" "mild," "somewhat hard", "intense", "very intense"; "extremely intense", "maximum effort")15,17. All children and adolescents were educated about the purpose of the scale, as would be performed, and had enough time to observe it and adapt to the amplitudes of the numbers.
The Borg scale was used in four stages: 1) before measurements of PIMax or PEMax, initially drawn by the participant, 2) immediately after the first drawn measurement, 3) five minutes after the first drawn assessment (PIMax or PEMax); 4) immediately after the last evaluation.
Data analysis
The sample data were analyzed using SPSS 17.0 (Statistical Package for Social Science) by assigning the significance level of 5%. Descriptive statistics were performed using standard deviations. The Kolmogorov-Smirnov test was used to test the normality of the data.
According to the Kolmogorov-Smirnov test, we observed that only the rates of perceived exertion of PEMax had a non-normal distribution, in which case the nonparametric Wilcoxon test was used to compare the feeling of effort at first, immediately after the completion of PEMax and after five minutes of rest. For comparison between rates of perceived exertion in children and adolescents who initially performed PIMax was used paired Student t test. The unpaired Student t test was used to assess the amount of effort required among participants who performed up to five maneuvers with those who held more than five maneuvers of maximal respiratory pressures (PIMax and PEMax).
RESULTS
Among the students who initially returned the documentation, 157 were eligible to participate. From these, 04 were excluded because they refused to participate, 05 did not understand the command, 03 for failing to perform acceptable and reproducible maneuvers within the maximum number of measures set out in the study and 01 for presenting fever in the week of the evaluation. Therefore, the final sample consisted of 144 children and adolescents, 63 boys and 81 girls, with a mean age of 8.8 ± 1.2 years old. The participants had an average weight of 30.2 ± 1.2 kg, height of 1.3 ± 0.1, and BMI of 16.4 ± 1.5 kg / m2.
On average it took approximately five maximal efforts to obtain reproducible and acceptable measurements for PIMax and PEMax from the children and adolescents evaluated. These results were 4.6 ± 1.7 and 4.7 ± 1.5 maneuvers to measure the PIMax and PEMax, respectively.
Table 1 describes the data on the perceived effort of the participants before, immediately after conducting the maneuvers of maximal respiratory pressures and five minutes after the rest. These values are described regardless of which maneuver was performed first. Table 2 compares the rate of perceived exertion initially observed with the results observed immediately after the maximal respiratory pressures. Table 3 compares the perception of effort immediately after the manometer with the one observed after five minutes of rest. Table 4, then, compares the rate of initial perceived effort with the one observed after five minutes of rest. The comparisons are shown separately for children and adolescents who had initially assessed PIMax or PEmax.
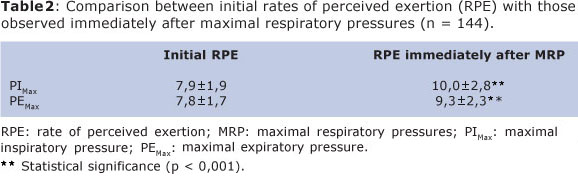
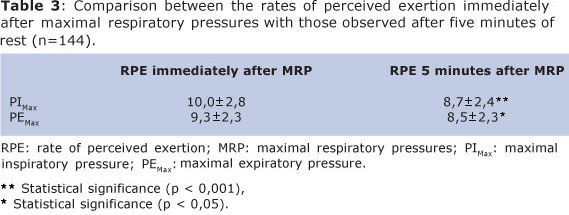
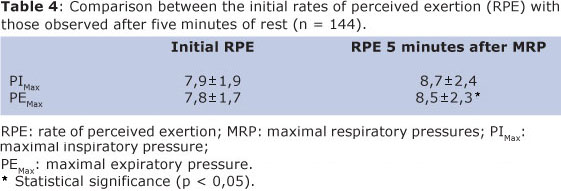
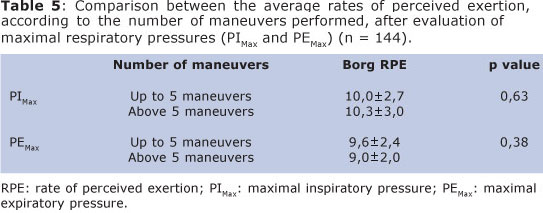
Table 5 presents the amount of perceived exertion by participants who performed up to five maneuvers compared with those who held more than five maneuvers for assessment of maximal respiratory pressures.
DISCUSSION
The evaluation of respiratory muscle strength by the manometer consists of a well-tolerated method by children and adolescents, since on average the rate of perceived exertion was classified as a "very light" effort17 on the Borg RPE scale.
According to Borg, a rule adopted by many clinicians is to stop an exercise test in an RPE of 14 or 15 ("intense"). For this author, the monitoring of the index of perceived exertion during a stress test is important for facilitating the safety of the test, being interrupted by any complication, especially in the case of patients and elderly17. Jones and Killian28, in further studies, showed that in the case of cardiopulmonary stress tests, despite the perceived exertion of exercise and the perception of respiratory effort (measured by dyspnea) increase during the test, this should be stopped when it reaches values classified as "intense" to "very intense" on the modified Borg scale.
The results of this study indicate a significant increase in the rate of perceived exertion immediately after the test, compared with the amount of initial effort, i.e., with the participant at rest before performing any of the maneuvers evaluated. This increase can be a consequence of the fact that the assessment of maximal respiratory pressures is a test that actually requires maximum efforts12.13. Coelho et al.29 when comparing the assessment of perceived exertion in fibrocystic children with healthy children after performing cardiopulmonary stress test, the shuttle walk test, noted that there was an increase in the amount of work performed after the test. However, fatigue was higher in healthy children. Aquino et al.30, when assessing the six-minute walk test on a sample of healthy children and adolescent, did not find significant differences in the subjective feeling of effort assessed by the Borg scale before and after this test.
When analyzing the rest interval between the completion of the PIMax and PEMax, we observed that this is a safe time interval regarding the perceived exertion. The results showed a significant reduction of effort between the index immediately after the completion of the manometer and five minutes afterwards. The perceived exertion after rest can be classified as "extremely light"17 on the Borg scale and close to the rate of initial effort, i.e., before the assessment of maximal respiratory pressures. Volianitis et al.4 used one minute of rest between PIMax maneuvers and three minutes of rest after the performance of maximal inspiratory pressure, to avoid the effects of fatigue. Nascimento et al.27 used a five-minute interval between maximal inspiratory and expiratory efforts in assessing respiratory muscle strength of Brazilian children 7-10 years old. The results of this study suggest that at least five minutes between the PIMax and PEMax is sufficient for the perceived exertion to return to values close to rest.
Comparatively evaluating the perceived effort of participants who have realized up to five maneuvers with those who required a number greater than five maneuvers for a valid and reproducible PIMax and/or PEMax, it is noted that similar values were obtained. According to Wen et al9, the greater the number of maneuvers, the more accurate assessment of respiratory muscle strength. Domenech-Clar et al7 found appropriate a limit of nine maneuvers to assess respiratory muscle strength in children and adolescents. In contrast, Alexander et al.2 advocated the holding 3-5 maximal respiratory maneuvers to assess respiratory muscle strength. However, taking into account the subjective perception of effort, the similarity between the observed values of effort is suggestive that the limit of nine maneuvers is safe to assess respiratory muscle strength of individuals from the age of seven.
Some limitations were found during the study, and among them stands out the difficulties in using the Borg RPE scale with children. Some children, especially those who were aged between 7 and 8 years, had difficulty in understanding the numerical scale 6-20, as well as its relationship with the associated verbal concepts. In a recent study on accuracy the modified Borg scale exercise in children and adolescents aged from 6 to 18 years with cystic fibrosis, Hommerding18 found that the subjective perception of dyspnea went through the modified Borg scale, showed greater accuracy with children at the age of 9 years old. Previous studies16,17 had considered age as an aspect able to influence the responses to the index of perceived exertion.
The lack of previous studies that have examined the perceived effort during the evaluation of respiratory muscle strength can be considered another limitation, since it made difficult the discussion of this study. However, this served as an incentive to achieve this study, since the evaluation of the perceived effort is very simple and provides greater safety on realizing tests that depend on effort and must be used in diverse populations, including children and adolescents.
Thus, the evaluation of respiratory muscle strength in children and adolescents by maximal respiratory pressures shows up as a safe method regarding the perceived effort. The five-minute interval between the completion of PIMax and PEMax was considered adequate and the limit of nine maneuvers for measuring pressure does not change significantly the perception of effort on children and adolescents.
REFERENCES
1. Costa D, Gonçalves HA, Lima LP, Ike D, Cancelliero KM, Montebelo MIL. Novos valores de referência para pressões respiratórias máximas na população brasileira. J Bras Pneumol. 2010;36(3):306-12. doi: 10.1590/S1806-37132010000300007. [ Links ]
2. Alexandre BL, Araújo SG, Machado MGR. Pressões respiratórias máximas. In: Machado, MGR. Bases da fisioterapia respiratória: terapia intensiva e reabilitação. Rio de Janeiro: Guanabara Koogan; 2008. p. 111-24. [ Links ]
3. Simões RP, Deus AP, Auad MA, Dionísio J, Mazzonetto M, Borghi-Silva A. Pressões respiratórias máximas em indivíduos saudáveis sedentários de 20 a 89 anos da região central do Estado de São Paulo. Rev Bras Fisioter. 2010;14(1):60-7. doi: 10.1590/S1413-35552010000100010. [ Links ]
4. Volianitis S, McConnel AK, Jones DA. Assessment of maximum inspiratory pressure. Respiration. 2001;68(1):22-7. doi: 10.1159/000050458. [ Links ]
5. Parreira VF, França DC, Zampa CC, Fonseca MM, Tomich GM, Britto RR. Pressões Respiratórias Máximas: valores encontrados e preditos em indivíduos saudáveis. Rev Bras Fisioter. 2007;11(5):361-8. doi: 10.1590/S1413-35552007000500006. [ Links ]
6. Neder JA, Andreoni S, Lerarioet MC, Nery LE. Reference values for lung function tests. II. Maximal respiratory pressures and voluntary ventilation. Bras J Med Biol Res. 1999;32(6):719-27. doi: 10.1590/S0100-879X1999000600007. [ Links ]
7. Domènech-Clar R, López-Andreu JA, Compte-Torrero L, De Diego-Damiá A, Macián-Gisbert V, Perpiñá-Tordera M, et al. Maximal static respiratory pressures in children and adolescents. Pediatr Pulmonol. 2003;35(2):126 - 32. doi: 10.1002/ppul.10217. [ Links ]
8. Freitas DA, Borja RO, Ferreira GMH, Nogueira PAMS, Mendonça KMPP. Equações preditivas e valores de normalidade para pressões respiratórias máximas na infância e adolescência. Rev Paul Pediatr. 2011;29(4):656-62. doi: 10.1590/S0103-05822011000400028 [ Links ]
9. Wen AS, Woo MS, Keens TG. How many maneuvers are required to measure maximal inspiratory pressure accurately. Chest. 1997;111(3):802-7.doi:10.1378/chest.111.3.802. [ Links ]
10. Tomalak W, Pogorzelski A, Prusak J. Normal values for maximal static inspiratory and expiratory pressures in healthy children. Pediatr Pulmonol. 2002;34(1):42-6. doi: 10.1002/ppul.10130. [ Links ]
11. Trinca MA, Bicudo IMP, Pelicione MCF. A interferência da asma no cotidiano das crianças. Rev Bras Crescimento Desenvolv Hum. 2011;21(1):70-84. [ Links ]
12. American Thoracic Society/European Respiratory Society. ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166(4):518-624. doi: 10.1164/rccm.166.4.518. [ Links ]
13. Aldrich TK, Spiro P. Maximal inspiratory pressure: does reproducibility indicate full effort? Thorax. 1995;50(1):40-43. doi: 10.1136/thx.50.1.40. [ Links ]
14. Souza RB. Pressões respiratórias estáticas máximas. J Pneumol. 2002;28 Suppl 3:S155-165. [ Links ]
15. Burkhalter N. Evaluación de la escala Borg de esfuerzo percibido aplicada a la rehabilitación cardiaca. Rev Latinoam Enferm. 1996;4(3):65-71. doi: 10.1590/S0104-11691996000300006. [ Links ]
16. O'Sulivan SB. Perceived Exertion: A Review. Phys Ther. 1984;64(3):343-6. [ Links ]
17. Borg G. Escalas de Borg para a dor e o esforço percebido. São Paulo: Manole; 2000. [ Links ]
18. Hommerding PX. Acurácia da escala de Borg modificada no exercício de crianças e adolescentes com fibrose cística [dissertação]. Porto Alegre: Universidade Federal do Rio Grande do Sul, Faculdade de Medicina; 2008. [ Links ]
19. Chen MJ. Criterion-related validity of the Borg ratings of perceived exertion scale in healthy individuals: a metaanalysis. J Sports Sci. 2002; 20(11):873-99.doi: 10.1080/026404102320761787 [ Links ]
20. Carlsen KH, Engh G, Mørk M. Exercise-induced bronchoconstriction depends on exercise load. Respir Med. 2000;94(8):750-5. doi: 10.1053/rmed.2000.0809. [ Links ]
21. Macedo TMF, Oliveira KMC, Melo JBC, Medeiros MG, Medeiros Filho WC, Ferreira GMH, et al. Treinamento muscular inspiratório em crianças com leucemia aguda: resultados preliminares. Rev Paul Pediatr. 2010;28(4):352-8. doi: 10.1590/S0103-05822010000400011. [ Links ]
22. Ziegler B, Rovedder PM, Oliveira CL, de Abreu e Silva F, de Tarso Roth Dalcin P. Repeatability of the 6-minute walk test in adolescents and adults with cystic fibrosis. Respir Care. 2010;55(8):1020-5. [ Links ]
23. WHO, World Health Organization. Young People's Health - a Challenge for Society. Report of a WHO Study Group on Young People and Health for All. Technical Report Series 731. Geneva: WHO, 1986. [ Links ]
24. Harik-Khan RI, Wise RA, Fozard JL. Determinants of maximal inspiratory pressure: the Baltimore longitudinal study of aging. Am J Respir Crit Care Med. 1998;158(5 Pt 1):1459 - 64. [ Links ]
25. Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC growth charts for the United States: Methods and development. National Center for Health Statistics. Vital Health Stat. 2002;11(246): 1-190. [ Links ]
26. Oliveira KMC, Macêdo TMF, Borja RO, Nascimento RA, Medeiros Filho WC, Campos TF et al. Força muscular respiratória e mobilidade torácica em crianças e adolescentes com leucemia aguda e escolares saudáveis. Rev Bras Cancerol. 2011;57(4):511-7. [ Links ]
27. Nascimento RA, Campos TF, Melo JBC, Raíssa de Oliveira Borja, Freitas DA, Mendonça KMPP. Obtained and predicted values for maximal respiratory pressures of Brazilian children. J Hum Growth Dev. 2012;22(1): 166-72. [ Links ]
28. Jones NL, Killian KJ. Exercise limitation in health and disease. N Engl J Med. 2000;343(9): 632-41. [ Links ]
29. Coelho CC, Aquino ES, Almeida DC, Oliveira GC, Pinto RC, Rezende IMO, et al. Análise comparativa e reprodutibilidade do teste de caminhada com carga progressiva (modificado) em crianças normais e em portadoras de fibrose cística. J Bras Pneumol. 2007;33(2):168-74. doi: 10.1590/S1806-37132007000200011. [ Links ]
30. Aquino ES, Mourão FAG, Souza RKV, Glicério BM, Coelho CC. Análise comparativa do teste de caminhada de seis minutos em crianças e adolescentes saudáveis. Rev Bras Fisioter. 2010;14(1):75-80. doi: 10.1590/S1413-35552010000100012. [ Links ]
 Corresponding author:
Corresponding author:
kmorganna@ufrnet.br
Manuscript submitted Mar 25 2012
Accepted for publication Aug 30 2012













