Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Aletheia
versão impressa ISSN 1413-0394
Aletheia no.42 Canoas dez. 2013
ARTIGO INTERNACIONAL
Intervenções educacionais e psicológicas para psoríase: uma revisão sistemática
Educational and psychological interventions on psoriasis: a systematic review
Leonardo Machado da SilvaI; André Vicente Esteves de CarvalhoII; Gabriel José Chittó GauerIII
I Faculdade de Psicologia da Pontifícia Universidade Católica do Rio Grande do Sul
II Universidade Federal de Ciências da Saúde de Porto Alegre
III Faculdade de Direito da Pontifícia Universidade Católica do Rio Grande do Sul
RESUMO
Introdução: Psoríase em placas é uma dermatose crônica que tem um impacto importante nas dimensões social e psicológica nos pacientes. Estudos anteriores sugeriram que intervenções educacionais e psicológicas podem ser efetivas no gerenciamento da psoríase. Objetivos: Examinar as intervenções educativas e psicológicas para psoríase em período de 20 anos (1992 a 2012). Método: revisão sistemática de literatura nas bases de dados: PubMed/Medline, PsycInfo (APA), ProQuest e Pepsic. Resultados: 1359 artigos foram primeiramente selecionados por busca computadorizada, dos quais 36 foram analisados por dois revisores. Sete (n=7) estudos foram posteriormente selecionados para análise detalhada, sendo um artigo (n=1) de intervenção educativa individual, dois (n=2) envolvendo intervenções psicológicas e quatro (n=4) programas de gerenciamento de sintomas. Conclusão: Embora a literatura aponte para um crescente número de estudos de intervenção para psoríase e variáveis psicológicas, são necessários estudos de maior rigor para ajudar os pacientes a lidar com a doença.
Palavras-chave: Psoríase, Estresse, Intervenções.
ABSTRACT
Background: Plaque psoriasis is a chronic skin disorder that has a major impact on patient´s social and psychological abilities. Preliminary studies have suggested that educative and psychological interventions may be effective in the management of psoriasis. Objectives: To examine the educative and psychological interventions for psoriasis in the last 20 years (1992-2012). Methods: A systematic review of literature was conducted in medical and psychological databases: PubMed / Medline, PsycInfo (APA), ProQuest and Pepsic. Results: 1359 articles were first selected by computerized search, from which 36 were examined by two revisers. Seven studies (n=7) were selected to a more in depth analysis, one (n=1) was a single educative intervention, two (n=2) involved psychological interventions and four (n=4) were symptom management programmes. Conclusion: Although the recent literature shows an increase number of interventions targeting psoriasis and psychosocial variables, stronger studies are necessary to help patients deal with the disease.
Keywords: Psoriasis, Stress, Interventions.
Introduction
The skin is the organ that serves as a boundary between the person and the environment. By having the same embryonic origin of the central nervous system (ectoderm), it represents an important role in emotions, since its innervations are linked to several body systems and reacts even to the smallest physical and emotional stimulations. It is no wonder that chronic dermatosis demonstrates a significant impact on patients' quality of life (QoL), as their diseases are internal and public at the same time. Among the chronic dermatosis, psoriasis is one of the most representatives, whether for its western incidence (around 2%) or because of the psychosocial impact caused by the symptoms.
Among the various forms of the disease, psoriasis vulgaris – or plaque-like psoriasis – is the most representative and can cover approximately 90% of diagnoses (Griffiths & Baker, 2007). The plaque psoriasis is an inflammatory disease, with immunological and genetic mediation, chronic course and possible periods of remission and relapse (Pereira, Brito & Smith, 2012). It is clinically characterized by well-delineated erythematous plaque with a silvery-white scale, which may have different sizes and thicknesses (Griffiths & Baker, 2007). In more severe cases, the lesions tend to be uncomfortable, disfiguring and itchy, with frequent reports of bleeding and a burning sensation. Although there is no precise physiopathological definition of psoriasis, it is believed that there is an inflammatory disorder of T lymphocytes, involving cellular differentiation flaws of the keratinocytes and epidermal hyperproliferation (Griffiths & Baker, 2007; Buske-Kirschebaum, Kern, Ebrecht & Hellhammer, 2006).
Although psoriasis is a dermatological disease, the growing body of evidence presented by the scientific community in recent years points to the multifactorial impact of the disease, making it the focus of psychodermatology and psychosomatic studies. Among the most common comorbidities are: obesity/metabolic syndrome (Noori, Trash & Menter, 2010) cardiovascular diseases (Schmitt & Ford, 2009; Christophers, 2007) autoimmune diseases (Christophers, 2007), such as Crohn's disease, cancer and lymphomas, alcohol intake (Schmitt & Ford, 2009; Kirby et al., 2007; McAleer et al., 2011) and psychiatric disorders (Schmidt & Ford, 2009; Biljan, Laufer, Filakovic, Situm & Brataljenovic, 2009; Russo, Ilchef & Cooper, 2004) such as Major Depression, Obsessive Compulsive Disorder and Post Traumatic Stress. Reports of conditions that affect the day-to-day lives of patients are also common, such as sexual dysfunction (Gupta & Gupta, 1997; Sapogna, Gisondi, Tabolli & Abeni, 2007), suicidal ideation (Gupta & Gupta, 1998; Kurd, Troxel, Crits-Christiph & Gelfand, 2010), poor conjugal/family relationships (Pereira et al., 2012; Campolmi et al., 2012) and low perceived social support (Picardi, Gaetano, Baliva & Biondi, 2005). Other studies involving several psychiatric comorbidities of psoriasis are discussed by the authors of a recent systematic review (Rieder & Tausk, 2012). The results point to a significant overall decrease of stress, and that there is need for further studies so that they can improve existing treatments.
Psychosomatic factors, psychoneuroimmunology, stress and psoriasis
The latest studies on psychosomatics try to rely increasingly on a recent interdisciplinary area of research: Psychoneuroimmunology (PNI). An example of this is the research on the role of negative emotions in the various body systems. It is known that the individual that experiences negative emotions in the face of stressors, over a long period, tends to have his nervous system affected, causing the breakdown of the body's harmony (homeostasis) to result in agitation and inhibition in the search for resolution of the stressor (allostasis), which consequently changes the balance of neurotransmitters and hormones.
Throughout the literature, there having been reported conflicting results concerning the relation between stress and psoriasis. Reports noted by these authors in clinical practice corroborate with some studies (Fortune, Richards, Main & Griffiths, 1998; Zachariae et al., 2004), where patients with psoriasis reported that the exacerbation of their symptoms was linked to the occurrence of stressful events. Comparing the stressful events of psoriasis patients with other dermatosis, other researches reports (Mahlotra & Mehta, 2008; Verhoeven et al., 2009) pointed to a number of everyday situations significantly higher for the former. The extent of the injuries measured through clinical PASI (Psoriasis Area and Severity Index) was positively correlated to the level of perceived stress in another study (Kotrulja, Tradinac, Jokic-Begic & Gregurek, 2010), which also showed positive correlations between depression, anxiety state and trait anxiety. The reported history of traumatic events in childhood, such as emotional abuse, alcohol / drugs and family secrets, was also brought in a greater number of patients with psoriasis compared with other dermatosis (Simonic et al., 2010), although the presence of these events did not foretell the severity of the injuries.
Under the interdisciplinary perspective of PNI, the interaction between the various body systems related stress and psoriasis deserves to be elucidated. The stress response activates the hypothalamic-pituitary-adrenal axis (HPA) and the autonomic nervous system, which interact with the immune system, allowing it to exacerbate inflammatory responses, such as those occurring in psoriasis (Evers et al, 2010). The activation of the HPA axis has as a result of the glucocorticoid cortisol which, besides collaborating with the circulatory and muscular reaction in response to the acute stress, also promotes the proliferation of mast cells and proinflammatory cytokines, which could promote the reaction of inflammatory diseases, such as psoriasis. This mechanism may explain the relative worsening of the lesions in stressful events, formerly referred, although we have the influence of individual variables mediating this process.
The pathogenesis linked to psoriasis is also implicated in the reaction to stress (Gulliver, 2008). T-cell activation in the skin promotes an increase in of the traffic of proinflammatory cytokines, such as the tumor necrosis factor (TNF-α), interleukin 2 (IL2) and interferon-γ, which promote other proinflammatory secretions. At the end of the cascade, there is a migration of inflammatory cells towards the skin, possibly resulting in a hyperproliferation of keratinocytes, contributing to the psoriasis' phenotype. The inflammatory processes linked to the pathogenesis of psoriasis are also common to a number of symptoms of the previously commented comorbidities, such as obesity, metabolic syndrome, cardiovascular disease and depression (Schmitt & Ford, 2009; Schmidt-Ott, Jacobs & Jaeger, 1998). A detailed explanation of the connection between the neuroendocrine-immune circuits and the skin is brought by Ralf Paus and colleagues in an important literature review (Paus, Theoharis & Arc, 2006).
Concerning the professionals: how much do healthcare professionals know about the psychosocial implications of psoriasis
There is sufficient evidence for psoriasis to be faced as a serious disease, one that affects a wide variety of aspects in the life of individuals, regardless of age, and that has links with serious comorbidities. Given the possible involvement of psychosomatic factors in the etiology as well as in the progression of the disease, there is a growing need to embrace the psychosocial variables in current treatments and also develop strategies that involve other health professionals in an interdisciplinary manner, such as psychologists and psychiatrists. Currently, the main recommendations for the treatment of the disease and management of its symptoms have taken into account broader aspects of the subject's life, focusing on how to face this disease.
It appears, however, that most of the literature reviews involving pathogenic and clinical aspects of the disease (Griffiths & Barker, 2007; Noori et al., 2010; Gottlieb & Dann, 2009) rarely mention the need for referral to professionals from the "psy" field, except in cases of severe depression and suicidal ideation (Russo et al., 2004). The overspecialization (focus on symptoms, rather than the person) can hypothetically be one of the major reasons for this neglect with the emotional aspects, since frequently professionals – especially dermatologists – who accept the patient at first, are not qualified enough to cope with such demands (Picardi et al., 2004; Richards, Fortune, Weidmann, Sweeney & Griffiths, 2004). Patients with psoriasis, acne and eczema were interviewed qualitatively to access their relationship with their dermatologists. The results indicate that the doctors were considered insensitive, had poor comprehension of the implications of the disease and tended to trivialize the patient's disease (Magin, Adams, Heading & Pond, 2009). In another study involving questionnaires sent by post to dermatologists from a U.S. state dermatology association (Jafferany, Stoep, Dumitrescu & Hurnung, 2010), of the 102 who responded to the survey, only 18% expressed clear understanding about psychodermatology and 42% of them felt comfortable treating psychodermatosis. However, perhaps the most surprising data is the fact that only 32% of doctors had received some sort of training to deal with psychodermatosis.
While the need for more training and improvement in the formation of some professionals is questioned, some health professionals, usually psychiatrists, psychologists and nurses, indicate interdisciplinary referrals and treatments. In a recent guide for diagnosis and clinical management of psoriasis (Cohenm Baron & Archer, 2012), sponsored by the British Association of Dermatologists, the authors recommend a comprehensive assessment of psychosocial factors of patients accessing the impairment of QoL. For the treatment, the first step would be to educate the patient about the disease, emphasizing the management of symptoms – and not the cure – , clarifying doubts and possible myths about the disease and teaching the subjects how to apply the medication. Furthermore, it is suggested to the clinician to verify the social impact of the disease, whether the patient has social support to aid in the treatment, verifying the best treatment for each case. However, the guide recommends treatment / psychological assistance only when it is decisive to the exacerbation of psoriasis symptoms.
In addition to conventional medical therapies for symptom management, which involve pharmacological treatments (topical, systemic, biological) and phototherapy, the concern in the literature generally focuses on secondary aspects of psoriasis and its associated comorbidities. Although psoriasis is considered a psychodermatosis with relevant morbidity and their physiopathological mechanisms are increasingly involved in multi factorial processes (for example, inflammatory mechanisms and their connection to stress), one realizes that the recommendations for treatment are reduced to the forms described above. Accordingly, the aim of this work is to verify the psychological and educational interventions performed in the treatment of psoriasis, whether used as the sole treatment or as an adjunct to other therapies. As far as we are concerned, no other study attempted to systematically search this kind of intervention involving psoriatic patients.
Method
A systematic review in English and Spanish including the last 20 years (1992 through June 30, 2012) was performed in the databases of PubMed / Medline, PsycInfo (APA), and ProQuest Pepsic (Psychology Journals) including the term psoriasis combined with psychological intervention, educative intervention, psychotherapy and psychotherapy protocol. The searches were performed by a research assistant under de supervivion of a library technician from PUCRS University, who was specialized in database search. Interventions designed for psoriasis and other chronic dermatosis were included, provided that psoriasis was also included in the study. The exclusion criteria were: language other than the chosen, exclusively pharmacological interventions or phototherapy, literature review articles, case studies and cross-sectional studies evaluating psychosocial variables without psychological or educational intervention. It is considered psychological intervention treatments involving some techniques or approaches of cognitive/emotional/psychological change, such as stress management and guided imagery; the educational interventions did not involve changes on cognitive variables, only informational or behavioral variables.
Results
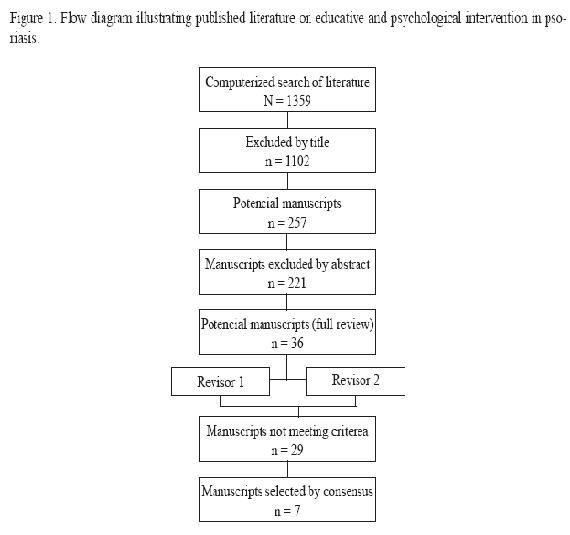
Initially, the computerized search indicated a total of 257 items, which were subsequently selected to have their abstracts read. Exclusion criteria at this stage involved correlational and review studies. Among these, 36 manuscripts were selected to be fully read by two assessors, all written in English language; after being completely read, 29 articles were excluded (22 were medical/physiological interventions and seven were not empirical psychological interventions) only seven studies were subsequently selected for the final analysis. Figure 1 shows the flow diagram of selected studies). The full review of potentially eligible articles were examined independently by two authors who were not blinded for the study´s criteria. Disagreements were resolved by consensus.
A brief appreciative review on the seven studies is presented as follows.
Individual cognitive-behavioral intervention – Zachariae et al, 1996
In this Danish study patients with psoriasis were randomly assigned to two groups: experimental and control. Experimental group consisted of 25 patients and underwent seven sessions of cognitive-behavioral intervention involving stress management, relaxation techniques and symptom control imagery training. The patients underwent a washout period of 14 days before the start of the study and were monitored at baseline and at the weeks four, eight and 12. The experimental group of 23 patients who completed the intervention showed a reduction of lesions compared to the control group by PASI (p = 0.06), the difference being that the percentage reduction in the PASI group was significant (p <.05). The results showed a satisfactory effect of psychological intervention, since there was no significant difference in the measurements obtained in the control group. Overall, 74% of patients in the experimental group improved symptoms, whereas the improvement was 43% for the controls.
A pilot hypnosis intervention – Tausk & Whitmore, 1999
This is a pilot study involving 11 patients with stable plaque psoriasis in the 12 months prior to the start of the study, without medication, divided into two groups. In the experimental group (n = 5) patients received suggestions for improvement of symptoms of psoriasis during hypnosis sessions. The control group (n = 6) received neutral hypnosis interventions, consisting only of suggestions aimed at relaxation. In the group that received the suggestions of symptom improvement, three subjects showed lesion improvement through PASI, decreased 81, 43 and 8%, respectively, all of which were among those who achieved the highest scores in the Stanford Scale of Hypnotizability. Of the six patients in the control group, the two persons who had the greatest reduction in lesions (31 and 18%, respectively) also had a higher score on the degree of hypnotizability, while moderately hypnotizable worsened 36 and 18%, respectively. Despite the modest sample presented, the study indicates that people with higher levels of suggestibility by hypnosis tend to get greater benefits in the clinical symptoms of psoriasis.
Study with the aid of audio tapes adjunct to phototherapy (UVB) and photochemotherapy (PUVA) – Kabat-Zinn et al., 1998
Patients with moderate and severe psoriasis (n = 37) were divided by medical indication into two groups, one receiving the phototherapy intervention only and another group with the use of psoralen added to phototherapy. The subjects were notified that the research was testing whether the experience of listening to relaxing music during the sessions of phototherapy would be nicer. The intervention for the experimental group included mindfulness meditation instruction, involving breathing, awareness of sensations, sounds, lights and air streams. At the end of the tape, they were also instructed to imagine that UV rays would be decreasing the growth and division of the skin. Four indicators for monitoring the reduction of lesions were created: first response point (first perceived change in lesions), turning point (plate begins to decrease area), halfway point (halfway through the initial injury) and clearing point (less than 5% of the initial lesions). The results point to differences between the groups with and without the use of relaxation tapes, the first 3.8 x more likely to reach the half point (p = 0.013) and point of whitening (p = 0.033). Furthermore, individuals in the tape group showed higher scores of positivity towards the sessions, a greater degree of relaxation and greater optimism towards treatment.
Symptom-management program – Fortune et al, 2002
This manuscript refers to the adaptation of the symptom management program offered by the NHS (National Health System) in the UK, previously structured for chronic pain, now adapted for psoriasis (PSMP – Psoriasis Symptom Management Programme). Amongst the psoriasis patients who were offered the program, 93 subjects were randomized into two groups by preference, one with conventional medical treatment (control) and the other with a multidisciplinary program. The intervention consisted of six cognitive-behavioral sessions, with 2.5h each, performed by doctors, nurses and psychologists. Measures taken at baseline, six weeks and six months were the following: extent of lesions (PASI), anxiety and depression (HADS – Hospital Anxiety and Depression Scale), stress (PLSI – Psoriasis Life Stress Inventory) and degree of disability (PDI – Psoriasis Disability Index). Of the 93 people who agreed to participate in the study, 40 participated in the PSMP and 53 were part of the control group. The results showed that the PASI significantly reduced at six weeks and six months (p <0.001), as well as the levels of anxiety (p <0.001) and depression (p <0.001) and disability (p = 0.04). Another finding reveals that, from the patients who participated in the program, 64% obtained clearance (> 75%), compared with only 23% of the control group.
Multidisciplinary educational program for chronic dermatosis – Lambert et al., 2011
This article was referring to a pilot study of the department of dermatology at the Hospital Ghent, Belgium, to test a multidisciplinary program aimed at improving the quality of life of patients with chronic dermatosis. The program lasted 12 weeks (2 meetings / week), and the psychological and educational activities were included in the following topics: skin care, Stress Reduction techniques, life style factors and psychodermatology information. A multidisciplinary team was composed of physical educator, dermatologist, nurse, teacher of yoga and mindfulness meditation, psychiatrist, psychologist and philosopher. Patients with psoriasis (n = 17) showed significant improvement in measures of quality of life after the intervention of the DLQI (p = 0.015), Skindex-29 (p = 0.020) and decreased their disability index with the PDI (p = 0.019).
Single Educative Intervention – Lora, Gisondi, Calza, Zanoni & Girolomoni, 2009
This manuscript portrays an educational intervention designed by a team of dermatology of Verona, Italy. Participants (n = 123) were randomized by computer to receive educational intervention of two hours by a dermatologist (educational group) or the psychoeducational group, where a psychologist accompanied the same 2h of intervention. The part that was up to the doctor was to explore the various information about psoriasis with the patient, such as the mechanisms of the disease, precipitating factors, course of disease, preventive measures and daily skin care. The group that had the presence of psychologists during the intervention received the same information, however, the end of the consultation was reserved so that they could be worked on possible negative emotions and coping strategies. Measures of quality of life (Skindex-29) and severity of pruritus were taken before and after the intervention, in addition to a six-month follow-up, where a telephone interview sought to verify that the information had been retained. The results showed an improvement in items that measured knowledge about the disease after six months (p <0.001) and a significant increase in the perception that professionals have enough to treat the disease (p <0.001). The items that measured how the person felt comfortable with psoriasis or to deal with the symptoms revealed no significant differences in both groups and in all outlets. The average PASI of the educational groups and psychoeducational groups were 9.8 and 10.8, respectively.
Randomized controlled trial using a multidisciplinary program – Bostoen, Bracke, Keuser & Lambert, 2012
The Ghent Program intervention, previously mentioned, was again applied in patients with psoriasis and atopic dermatitis. This study involved 29 patients with psoriasis, previously randomized by computer, and divided into control and experimental group. The former continued to receive conventional medical treatment alone, while the second received the multidisciplinary approach of the program. The measures of extent and severity (PASI), quality of life (Skindex-29), level of disability (PDI) and depression (BDI – Beck Depression Inventory) were assessed at baseline and three, six and nine months later. The results of PASI indicated a significant reduction of lesions in the experimental group compared to controls at three months (P = 0.036) and six months post-intervention (p = 0.017), although the reduction has not been maintained at nine months (p = 0.116). Psoriasis disability index showed a reduction at all times, three months (p = 0.015) and six months (p = 0.020) and nine months (p = 0.021), whereas the average overall rates of depression decreased significantly after nine months (p = 0.029).
Discussion
We performed a systematic review of the past 20 years about the psychological and educational interventions presented for the treatment of psoriasis. Although we have a consolidated scientific literature in the fields of psychosomatic and psychodermatology pointing to the importance of including psychological therapies and educational interventions for psoriasis, there is a noteworthy low number of articles found. Of the seven articles analyzed, five of them were created especially for the treatment of psoriasis, while two of them were aimed at the chronic dermatosis most commonly linked to psychosomatic aspects. Overall, we observed a reduced number of subjects who participated in the studies, which, on one hand, may indicate the difficulties of conducting interventional research, such as the high dropout rates. On the other hand, these data can hypothetically show poor adherence of patients for this type of intervention, since traditional treatments are offered on a larger scale and are part of the current medical standard. Only one study had a randomized clinical trial, which reflects the need to conduct further research with more rigorous methodologies. Due to the nature of the intervention, double-blind studies were not found, but only four of the seven manuscripts reported that either the professionals that performed medical tests or some of the patients' choices were blind.
In all selected studies the results were satisfactory in almost unanimity of the psychological variables. Clinical examination in one study (Zachariae et al., 1996) showed no significant improvement of the lesions in the control group, although this has shown close to significant levels. More recent studies have accessed instruments to evaluate health-related variables, such as quality of life and degree of disability of the disease, which shows a recent trend in studies with psoriasis. The variables depression and anxiety, that have long been associated with psoriasis, were measured in only two studies (Fortune et al., 2002; Bostoen et al., 2012), which may reflect a recent trend of researchers seeking broader tools that allow accessing psychosocial variables. In this sense, we can see as well the specialization of scales used in more recent studies, which showed instruments specifically designed for use in psoriatic patients, such as the DLQI, PDI and PLSI. The degree of specialization of instrumentation used and the small number of studies involving psychological and educational interventions may reflect the emphasis in studies that focus on cross-cutting research designs.
The individual interventions have proved to be the majority and the modality of choice in four of the seven studies. Techniques were used in these various interventions, such as psychotherapy, hypnosis, guided imagery and psychoeducation, but all these were not accompanied by further studies that could confirm the results with a larger sample and in other populations. It is clear, also, a tendency of recent literature on the use of the group modality and the use of multidisciplinary interventions involving the management of symptoms. In the United Kingdom, as seen in Fortune and colleagues (Fortune et al., 2002), management programs for chronic symptoms have long been developed, as this program has been adapted for pain. Another European program with twice the time of intervention, developed by the Ghent Hospital from Belgium (Lambert et al., 2011; Bostoen et al., 2012), is another example of the tendency of interventions having a multidisciplinary and educational nature. The three manuscripts have applied these two programs used at least four different health professionals, reflecting the interdisciplinary nature of these approaches. It can be hypothesized that the low investment of recent research on individual interventions is due to satisfactory results and to government support for the development of such programs, which would be contemplating the results brought by multidimensional literature.
Although most studies use clinical and psychological variables to measure aspects of psoriasis in the evaluation of interventions, none of the studies used biological variables. The markers used in biological studies involving psoriasis are often related to stress effects, such as: serum cortisol (Evers et al., 2010), salivary cortisol (Remrod et al., 2007), interleukin1β (Mastrolonardo, Alicino, Zefferino, Pasquini & Picardi, 2007) and NK cells (Schmidt-Ott et al., 2009). It is believed that this discrepancy in relation to intervention studies may be related to the fact that PNI is a relatively new area of research, and the education of health professionals are not yet contemplating interdisciplinary aspects, focusing only on their specialty. Perhaps this explains both the difficulty of conducting interdisciplinary intervention studies as well as the professional lack of preparation (Picardi et al., 2004; Richards et al., 2004; Jefferany et al., 2010) and disappointment by some patients in an outpatient level (Magin et al., 2009), since psoriasis is a chronic disease that affects individuals in their multiple dimensions. Likewise, none of the analyzed studies took into account important individual variables such as gender, age of onset of psoriasis and coping strategies.
Conclusion
This was the first review article that, among its range of 20 years, intended to analyze the psychological and educational interventions available for psoriasis, including interventions for chronic dermatosis where there were patients with psoriasis. However, several limitations of this manuscript could be pointed. Exclusion criteria may have left some manuscript not contemplated for analysis in this review, as well as the limitation of these authors in understanding other languages. The limited data and the reduced number of articles prevented a quantitative analysis of the results, which affected the quality of the systematic review. Brief comments were made on each study due to the limited information available and little methodological strictness, which makes this analysis somewhat limited.
Prospective studies could benefit from the use of biological variables, contributing to the etiopathogenic understanding of psoriasis as to the validation of different intervention techniques. There is a clear need for investment in interdisciplinary interventions for psoriasis, given the degree of commitment of the individuals affected by the disease and the amount of data that point to different psychosocial variables as important matters both in genesis, exacerbation and injury. Other studies could bring the importance of the inflammatory nature of diseases as psoriasis and may be involved in a chain of inflammatory illnesses in the long term, as Christophers (2007) brings. Accordingly, psoriasis would have an even greater importance, not only for its damage itself, but by the inherent risk of developing more severe inflammatory diseases, subject to early intervention.
References
Biljan D., Laufer D., Filakovic, P., Situm, M., Brataljenovic, T. (2009). Psoriasis, mental disorders and stress. Collegium Antropologicum, 3(2), 889-892. [ Links ]
Bostoen, J., Bracke, S., de Keuser, S., Lambert, J. (2012). An educational programme for psoriasis and atopic dermatitis. British Journal of Dermatology. Sep. [captured 2012 Sep 12]; [20 screens] Available: http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2133.2012.11113.x/full [ Links ]
Buske-Kirschebaum, A., Kern, S., Ebrecht, M. & Hellhammer, D. H. (2006). Endocrine Stress Responses in Th1-mediated Chronic Inflammatory Skin Disease (psoriasis vulgaris) – Do They Parallel Stress-induced Changes in Th2-mediated Inflammatory dermatosis (atopic dermatitis)? Psychoneuroendocrinilogy, 31(4), 439-446.
Campolmi, E., Zanieri, F., Santosuosso, U., Déreme, A. M., Betti, S., Lotti, T. & Cossidente, A. (2012). The importance of stressful family events in psoriatic patients: a retrospective study. Journal of the European Academy of Dermatology and Venereology, 26(10), 1236-1239. [ Links ]
Christophers E. (2007). Comorbidities in psoriasis. Clinics in Dermatology, 25(1), 529-34. [ Links ]
Cohen, S. N., Baron, S. E. & Archer, C. B. (2012). Guidance on the diagnosis and clinical management of psoriasis. Clinical and Experimental Dermatology, 37(1), 13-18. [ Links ]
Evers, A. W. N., Verhoeven, E. W. M., Kraaimat, F. W., de Jong, E. M. G. J., de Brower, S. J. M., Schalkwijk, J., Sweep, F. C. G. J. & van der Kerkhof, P. C. M. (2010). How stress gets under the skin: cortisol and stress reactivity in psoriasis. British Journal of Dermatology, 163(6), 986-91. [ Links ]
Fortune, D. G., Richards, H. L., Main, C. J. & Griffiths, C. E. (1998). What patients with psoriasis believe about their condition. Journal of American Academy of Dermatology, 39(2), 196-201. [ Links ]
Griffiths, C. E. M. & Barker, J. N. W. N. (2007). Pathogenesis and clinical features os psoriasis. The Lancet, 370(4), 263-271. [ Links ]
Gulliver, W. (2008). Long-term prognosis in patients with psoriasis. British Journal of Dermatology, 159(2), 2-9. [ Links ]
Gupta, M. A. & Gupta, A. K. (1997). Psoriasis and sex: a study with moderately to severely affected patients. International Journal of Dermatology, 36(2), 259-62. [ Links ]
Gupta, M. A. & Gupta, A. K. (1998). Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis. British Journal of Dermatology, 139(8), 846-50. [ Links ]
Gottlieb, A. B. & Dann, F. (2009). Comorbidities in patients with psoriasis. The American Journal of Medicine, 122(1150), 1-9. [ Links ]
Jafferany, M., Stoep, A. V., Dumitrescu, A. & Hurnung, R. L. (2010). The knowledge, awareness, and practice patterns of dermatologists toward psychocutaneous disorders: results of a survey study. International Journal of Dermatology, 49(2), 784-789. [ Links ]
Kabat-Zinn, J., Wheeler, E., Light, T., Skillings, A., Scharf, M. J., Cropley, T. G., Hosmer, D. & Bernhard, J. D. (1998). Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA). Psychosomatic Medicine, 60(1), 625-32. [ Links ]
Kotrulja, L., Tadinac, M., Jokic-Begic, N. & Gregurek, R. (2010). A multivariate analysis of clinical severity, psychological distress and psychological traits in psoriatic patients. Acta Dermato-Venereologica, 90(4), 251-256. [ Links ]
Kirby, B., Richards, H. L., Mason, D. L., Fortune, D. G., Main, C. J. & Griffiths, C. E. M. (2007). Alcohol consumption and psychological distress in patients with psoriasis. British Journal of Dermatology, 158(1), 138-140. [ Links ]
Kurd, S. K., Troxel, A. B., Crits-Christoph, P., Gelfand, J. M. (2010). The risk of depression, anxiety and suicidality in patients with psoriasis: a population-based study. Achives of Dermatology, 146(8), 891-5. [ Links ]
Lambert, J., Bostoen, J., Geusens, B., Bourgois, J., Boone, J., De Smedt, D. & Annemans, L. (2011), A novel multidisciplinary educational programme for patients with chronic skin diseases: Ghent pilot project and first results. Archives of Dermatological Research, 303(2), 57-63. [ Links ]
Lora, V., Gisondi, P., Calza, A., Zanoni, M. & Girolomoni, G. (2009). Efficacy of a single educative intervention in patients with chronic plaque psoriasis. Dermatology, 219(2), 316-21. [ Links ]
Magin, P. J., Adams, J., Heading, G. S. & Pond, C. D. (2009). Patients with skin disease and their relationships with their doctors: a qualitative study of patients with acne, psoriasis and eczema. The Medical Journal of Australia, 190(2), 62-64. [ Links ]
Malhotra, S. & Mehta, V. (2008). Role os stressful life events in induction or exacerbation of psoriasis and chronic urticaria. Indian Journal of Dermatology, 74(6), 594-8. [ Links ]
Mastrolonardo, M., Alicino, D., Zefferino, R., Pasquini, P. & Picardi, A. (2007). Effect of Psychological stress on salivary interleukin-1β in psoriasis. Archives of Medical Research, 38(1), 206-11.
McAleer, M. A., Mason, D. L., Cunningham, S., O´Shea, S. J., McCormick, P. A., Stone, C., Collins, P., Rogers, S. & Kirby, B. (2011). Alcohol misuse in patients with psoriasis: identification and relationship to disease severity and psychological distress. British Journal of Dermatology, 164(4), 1256-61. [ Links ]
Noori, K. B. S., Thrash, B. & Menter, A. (2010). Comorbidities in psoriasis. Seminars in Cutaneous Medicine and Surgery, 26(1), 10-15. [ Links ]
Paus, R., Theoharis, T. C. & Arc, P. C. (2006). Neuroimmunoendocrine circuintry of the brain-skin connection. Trends in Immunology, 27(1), 32-39. [ Links ]
Pereira, M. G., Brito, L. & Smith, T. (2012). Dyadic adjustment, family coping, body image, quality of life and psychological morbidity in patients with psoriasis and their partners. International Journal of Behavioral Medicine, 19(3), 260-269. [ Links ]
Picardi, A., Amerio, P., Baliva, G., Barbieri, C., Teofoli, P., Bolli, S., Salvatori, V., Mazzotti, E., Pasquini, P. & Abeni, D. (2004). Recognition of depressive an anxiety disorders in dermatological outpatiens. Acta Dermato-venereologica, 84(1), 213-17. [ Links ]
Picardi, A., Gaetano, P., Baliva, G. & Biondi, M. (2005). Stress, social support, emotional regulation and exacerbation of diffuse plaque psoriasis. Psychosomatics, 46(1), 556-64. [ Links ]
Richards, H. L., Fortune, D. G., Weidmann, A., Sweeney, S. K. & Griffiths, C. E. (2004). Detection of psychological distress in patients with psoriasis: low consensus between dermatologist and patient. British Journal of Dermatology, 151(1), 1227-33. [ Links ]
Rieder, E. & Tausk, F. (2012). Psoriasis, a model of dermatologic psychosomatic disease: psychiatric implications and treatments. International Journal of Dermatology, 51(4), 12-26. [ Links ]
Russo, P. A. J., Ilchef, R. & Cooper, A. J. (2004). Psychiatric morbidity in psoriasis: a review. Australian Journal of Dermatology, 45(7), 155-161. [ Links ]
Sapogna, F., Gisondi, P., Tabolli, S. & Abeni, D. (2007). Impairment of sexual life in patients with psoriasis. Dermatology, 214(4), 144-50. [ Links ]
Schmidt-Ott, G., Jacobs, R. & Jaeger, B. (1998). Stress-induced Endocrine and Immunological Changes in Psoriasis Patientes and Healthy Controls. Psychotherapy and Psychosomatics, 67(2), 37-42. [ Links ]
Schmid-Ott, G., Jaeger, B., Boehm, T., Langer, K., Stephan, M., Raap, U. & Werfel, T. (2009). Immunological effects of stress in psoriasis. British Journal of Dermatology, 160(2), 782-85 [ Links ]
Schmitt, J. & Ford, D. E. (2009). Psoriasis is independently associated with psychiatric morbidity and adverse cardiovascular risk factors, but not with cardiovascular events in a population-based sample. Journal of the European Academy of Dermatology and Venereology, 24(1), 885-92. [ Links ]
Simonic, E., Kastelan, M., Peternel, S., Pernar, M., Brajac, I. & Kardum I. (2010). Childhood and adulthood traumatic experiences in patients with psoriasis. Journal of Dermatology, 37(4), 793-800. [ Links ]
Tausk, F. & Whitmore, E. S. (1999). A pilot study of hypnosis in the treatment of patients with psoriasis. Psychotherapy and Psychosomatics, 68(1), 221-25. [ Links ]
Verhoeven, E. W. M., Kraaimaat, F. W., de Jong, E. M. G. J., Schalkwijk, J., van de Kerkhof, P. C. M. & Evers, A. W. M. (2009). Individual differences in the effect of daily stressors on psoriasis: a prospective study. British Journal of Dermatology,161(8), 295-99. [ Links ]
Zachariae, R., Oster, H., Bjerring, P. & Kragballe, K. (1996). Effects of psychologic intervention on psoriasis: a preliminary report. Journal of The American Academy of Dermatology, 34(1), 1008-15. [ Links ]
Zachariae, R., Zachariae, H., Blomqvist, K., Davidsson, S., Molin, S., Mork, C. & Sigurgeirsson, B. (2004). Self-reported stress reactivity and psoriasis-related stress of Nordic psoriasis sufferers. Journal of the European Academy of Dermatology and Venereology, 18(3), 27-36. [ Links ]
 Endereço para contato
Endereço para contato
E-mail: leonardo.silva@pucrs.br
Recebido em fevereiro de 2014
Aceito em abril de 2014
Leonardo Machado da Silva: psicólogo, mestre em Psicologia da Saúde (Bath University/UK), doutor em Psicologia Clínica (PUCRS). Professor Adjunto da Faculdade de Psicologia da PUCRS e sócio do Instituto Brasileiro de Psicologia da Saúde (IBPS).
André Vicente Esteves de Carvalho: médico dermatologista, mestre em Patologia pela UFCSPA e doutorando em Patologia pela UFCSPA. Médico do Complexo Hospitalar Santa Casa, onde é chefe do ambulatório de psoríase e orientador de residência médica.
Gabriel José Chittó Gauer: médico psiquiatra, Doutor em Medicina e Ciências da Saúde (PUCRS) e pós-doutor em Medicina (Maryland, USA). Professor titular e pesquisador da Faculdade de Direito da PUCRS (nível 1D).














