Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Psicologia em Pesquisa
versão On-line ISSN 1982-1247
Psicol. pesq. vol.12 no.3 Juiz de Fora set./dez. 2018
https://doi.org/10.24879/2018001200300492
Artigo Original
10.24879/2018001200300492
Risco psicossocial familiar, coping do tratamento da obesidade infantil e controle parental da alimentação
Family psychosocial risk, coping with child obesity treatment and parental feeding control
Kainara Silva da Cunha I; Wagner de Lara Machado II; André Luiz Monezi Andrade I; Sônia Regina Fiorim Enumo I;
I Pontifícia Universidade Católica de Campinas
II Pontifícia Universidade Católica do Rio Grande do Sul
Resumo
Este estudo analisou variáveis parentais relacionadas ao tratamento do sobrepeso/obesidade de crianças em tratamento ambulatorial, como o controle alimentar, estressores e enfrentamento (coping) da doença, e risco psicossocial familiar. Dezenove cuidadores responderam os instrumentos: Caracterização do Participante, Entrevista de Coping Parental, Psychosocial Assessment Tool 2.0 (PAT 2.0) e Comprehensive Feeding Practices Questionnaire (CFPQ). A maioria das famílias apresentou risco psicossocial médio-alto (Alvo = 52,6%; Clínico = 21,1%) e as práticas parentais de controle alimentar mais comuns foram o Incentivo ao Equilíbrio e à Variedade de alimentos, e a Restrição da alimentação. O controle alimentar é o maior estressor para os cuidadores, que reagem com raiva e tristeza, apesar de apresentarem um coping mais adaptativo. Os resultados indicam a necessidade de intervenções específicas para essa população em risco.
Palavras-chave: Obesidade Infantil, Práticas de Criação Infantil, Fatores Psicossociais, Coping, Comportamento Alimentar.
Abstract
This study evaluated parental variables involved in the outpatient treatment of overweight/obese children, in variables included food control, stressors and coping, as well as family psychosocial risk. Nineteen caregivers filled out instruments such as Participant Characterization, Parental Coping Interview, Psychosocial Assessment Tool 2.0 (PAT 2.0) and Comprehensive Feeding Practices Questionnaire (CFPQ). Most families showed medium-high psychosocial risk (Targeted = 52.6%, Clinical = 21.1%) and the most common parental practice of food control was to Encourage Balance and Variety, and the Restriction of food. Food control is the major stressor for caregivers, who react with anger and sadness, despite having a more adaptive coping. The results indicate the need for specific interventions for this population at risk.
Keywords: Obesity in Children, Childrearing Practices, Psychosocial Factors, Coping, Eating Behavior.
Childhood obesity is a health problem in Brazil and worldwide. It is estimated that 75 million children will be obese in 2025 (Brasil, Ministério da Saúde, 2014; World Health Organization, 2014). For adults, overweight is defined as a relative weight ratio higher than desirable to height whereas obesity is excessive fat accumulation in the body, with body mass index (BMI) higher than 25 kg/m2 (World Health Organization, 2017). In children and adolescents, obesity is considered from the BMI classification above the 97th percentile, following the growth curves, and the values are exposed in z-score and median percentile of the reference sample, according to WHO (2006). In 2013, children and adolescents obese in developed countries were 12.9% for boys and 13.4% for girls (Ng et al., 2014). In Brazil, in the age group 5 to 9 years, the percentage of overweight children reached an alarming 33.5%, according to the last Survey of Family Budgets/Pesquisa de Orçamentos Familiares (POF 2008-09), conducted by the Brazilian Institute of Geography and Statistics/Instituto Brasileiro de Geografia e Estatística (IBGE, 2008).
Overweight and obesity are considered physical health risk factors for children and adolescent development, increasing the risk of cardiovascular diseases, abnormal glucose metabolism, liver and gastrointestinal disorders, sleep apnea and orthopedic complications. There are also psychological consequences, such as depression, anxiety, body image distortion and socialization problems, in children too (Sahoo et al., 2015).
The lack of physical activity is a contributory factor to the problem (Smith et al., 2018; Van Allen, Borner, Gayes, & Steele, 2015; Vázquez-Nava, Treviño-Garcia-Manzo, Vázquez-Rodríguez, & Vázquez-Rodríguez, 2013), and 49.5% of Brazilian people are sedentary (Brasil, Ministério do Esporte, 2015). In this same study, it was found a relationship between higher schooling and exercise in free time.
Additionally, some psychosocial variables seem to be associated with childhood obesity, such as parent overweight and mothers education level (Wang & Lim, 2012), mother’s stress (Tate, Wood, Liao, & Dunton, 2015, and to be a single mother (Grow et al., 2010). Evans and Pilyoung (2013) analyzed these health outcomes in poverty conditions based on the concepts of cumulative exposure to risks and dysregulation in response to stress. Because obesity has a multifactorial etiology, it requires different approach treatments with (Filgueiras & Sawaya, 2018; Smith et al., 2018). A potential area for prevention and treatment of childhood obesity is feeding dynamics which includes two central components (Eneli, Tylka, Watowicz, Hummel, Ritter, & Lumeng, 2015). The first one is the role of the caregiver in feeding (caregiver feeding role) - how, when, where and what the caregiver gives the child. The second is the eating behavior of the child - how much, when, what, and if he/she eats what is offered. Authors consider the parents, especially mothers, as the significant influence in shaping their children’s dietary habits (Hoffmann, Marx, Kiefner-Burmeister, & Musher-Eizenman, 2016; Muhser-Eizenman & Kiefner, 2013).
In this regard, obesity is a difficult disease because there are many proximal biopsychosocial influences (e.g., genetic, child, family, and peer), and processes working together over time (low self-esteem causes consumption of sugary foods which disrupts sleep quality and contributes to obesity, for example), in a developmental cascade model of pediatric obesity (Smith et al., 2018). In this context, adherence to treatment is achieved through lifestyle change (Nguyen & Bera, 2016). It is necessary to evaluate the impact of child feeding practices on dietary patterns, modify parental beliefs and attitudes, perceptions related to children’s health threats to change children dietary practices and therefore and contribute to the prevention of obesity (Campos, Machado, Azevedo, & Silva, 2017). Thus, the manner in which parents are coping with their child’s obesity and the treatment can affect the health outcome, making coping evaluation important for treatment adherence (Bellodi, 2018). Likewise, one should consider the developmental characteristics of the child and the family process (Matwiejczyk, Mehta, Scott, Tonkin, & Coveney, 2018).
One of the approaches to assessing these conditions is the Motivational Theory of Coping (MTC) (Skinner, Edge, Altman, & Sherwood, 2003; Skinner & Zimmer-Gembeck, 2016). The MTC has a human development perspective and focuses on the concept of self-regulation. It proposes coping as a regulatory action of organized patterns of behavior, emotion, attention, cognition, and motivation. The MTC proposes 12 categories of coping, related to adaptive processes directed to the satisfaction of three basic psychological needs - Relatedness, Competence, and Autonomy. If the stressor is perceived to be a threat to these needs, the individual may use several coping strategies functionally related to families of coping, such as Delegation and Isolation (threatening the need for Relatedness), Helplessness and Escape (Competence), Submission and Opposition (Autonomy), all with poorly adaptive outcomes in terms of physical and mental health in the medium and long-term. On the other hand, if the stressor is perceived as a challenge, six coping families with more adaptive outcomes, are included as follows: Self-Reliance and Support Seeking (challenge to the need for Relatedness), Problem-Solving and Information-Seeking (Competence), Accommodation and Negotiation (Autonomy) (Skinner et al., 2003; Skinner & Zimmer-Gembeck, 2016). To consider this psychological needs is essential to a family-based lifestyle intervention (Fenner, Straker, Davis, & Hagger, 2013).
This study evaluated the relationships between parental variables associated with the treatment adherence of overweight/obese children such as family psychosocial risks, parental feeding control, stressors and parental coping with the obesity treatment. We hypothesized that those families with higher psychosocial risks would have more stressors and maladaptive coping with regards to their children’s treatment.
METHOD
Sample
In this cross-sectional study, 19 family members were included (16 mothers, two fathers, and one sister who cares the children) of obese or overweight children undergoing outpatient treatment (Pediatric Outpatient Service, City of Campinas. The mean age of the caregivers was 37 years (SD = 6.24), and schooling ranged from incomplete Elementary School to incomplete High School. The majority were married or “living together” (n = 12), while seven were divorced or single mothers. The participants had problems with weight (BMI ≥ 25 kg/m²) according the Body Mass Index (MBMI = 31.93, DP = 5.07), predominantly obesity (n = 13) and overweight (n = 4), however some of them had normal weight (n = 2).
Participants cared for 19 children, 7 female and 12 male, aged 5 to 11 years (Mage = 9.15), enrolled in Elementary School (n = 17) or in Early Childhood Education (n = 2). Prevalent diagnosis was Obesity (n = 17), with BMI between 22.50 to 36.28, followed by Overweight (n = 2) with BMI between 21.49 to 21.83, according to the growth curves, and the values exposed in z-score and median percentile of the reference sample (Cintra, Passos, Santos, Achado, & Fisberg, 2014).
Instruments
The Participant Characterization Form - name, date of birth, schooling, occupational activity, height/weight and BMI, information about the routine (check for obesity in the family and physical activity habits) were recorded. Medical treatment data were also collected (diagnostic hypothesis, specialties that attend it, date of treatment initialization and periodicity).
The Psychosocial Assessment Tool 2.0 (PAT 2.0) (Pai et al., 2008) adapted and validated for Brazilian people by Santos (2012) was administered to the caregivers to assess family psychosocial risk. This instrument has seven subscales and contains information about the caregiver and the child, as follows: 1) Family structure and sources (8 items), 2) Social support (4 items), 3) Child problems (15 items) 4) Sibling problems with (15 items), 5) Family problems (8 items), 6) Stress reactions (3 items) and 7) Family beliefs (4 items) which can range from 0 to 7. The reliability of the total scale was calculated by Kuder-Richardson 20 and is good (KR20 = 0.77). The PAT 2.0 was based on the Pediatric Preventive Health Psychosocial Model, which considers three levels of family psychosocial risk based on the total score - Universal (low; Total score < 1), Targeted (medium; Total score 1.0 – 1.9) and Clinical (high; Total score > 2) levels of risk and need for intervention. The level of risk has implications for treatment recommendations to support family adjustment and problem-solving (Kazak, Schneider, Didonato, & Pai, 2015; Pai et al., 2008).
The Comprehensive Feeding Practices Questionnaire (CFPQ) (Musher-Eizenman, & Holub, 2007, adapted and validated in Brazil by Araújo, 2015) was used to evaluate different parental practices about infant feeding. The CFPQ evaluates nine factors in both versions, 39 items (KMO = 0.83; 56,5% of variance, with adequate criteria, in Brazilian version): 1) Modeling - this factor describes how much the parents report as a model for the child in relation to the consumption of healthy foods; parents actively demonstrate healthy eating for the child (4 items; a = 0.81); 2) Restriction - how much parents report restricting or controlling their children’s nutrition, to maintain health and weight, with restriction of the quantitative and qualitative food choice for health (9 items; a = 0.80); 3) Monitoring - how parents report controlling unhealthy food intake by children (4 items; a = 0.87); 4) Emotion regulation - how much parents report using food to regulate the child’s emotional state (3 items; a = 0.75); 5) Pressure to eat - how much parents report putting pressure on the child to consume more food at mealtimes (3 items; a = 0.66); 6) Involvement - how much the parents report encouraging the involvement of the child in the planning and preparation of meals (4 items; a = 0.65); 7) Food as a reward - how much parents report using food as a reward for their child’s behavior (3 items; a= 0.66); 8) Child control - permissiveness and child control - indicate how parents allow the child to control their eating behavior and the feeding interactions between them and their parents (5 items; a = 0.58); 9) Encourage Balance and Variety - how much parents report encouraging the experimentation of new foods and promoting the consumption of a balanced, varied and healthy diet (4 items; a = 0.743). The CFPQ has two Likert scales, with five points from “never” to “always” (items 1 to 13) and a concordance, with “totally disagree” and “totally agree” responses (items 14 to 39).
To evaluate the parental stressors and coping with overweight/obesity treatment, we used the Interview on Parental Coping with Overweight/Obesity Child adapted from Guimarães (2015) and based on the Motivational Theory of Coping Scale-12 (Lees, 2007). This protocol contains three domains: 1) Caregiver and child identification data, date/time of administration; e) Demand (identification of stressors) and 3) Coping process. This last domain is assessed by a general question: “What have you done to cope with the situation of caring for your child with overweight/obesity?. This nuclear question was complemented by guiding questions to obtain information about: a) what the participant does to cope with the stressor, b) how often are each of the 12 coping families practiced, on a scale of 1 = not at all to 5 = a lot; c) how he/she does it, d) why, e) the associated feeling or emotion, f) the evaluation of the efficacy of the coping strategy (How did this work/help?), and post-copying (If you could, what would you do differently?). After answering the questions on the 12 coping families, the participants answered three additional questions related to emotional reactions (sadness, fear, and anger), answered on a scale of 1 = not at all to 5 = a lot.
The anthropometric evaluation of the participants was done using a scale and stadiometer, available at outpatient clinics, calculating the BMI.
Ethics
This study was approved by Ethics Committee of the Pontifícia Universidade Católica de Campinas (Protocol number 1.436.612).
Data analysis
The Shapiro-Wilk Test was used to evaluate the data normality. The association between treatment stressors (parental control of feeding, family psychosocial risks) and their coping strategies were evaluated by we used Chi-Square Test (?2) or the Fischer Exact. Additionally, we adopted the same procedure to evaluate the association between adaptive and maladaptive coping with the adherence to treatment (BMI, physical activity, diet). For a continuous variable, the Kruskal-Wallis Test was used followed by Games-Howell post-hoc test when significant effects were detected. The significance level in all analyses was 5%, and the software used was SPSS version 23.0.
RESULTS
Most of the family members (73.7%) were considered at medium-high psychosocial risk by PAT 2.0 in which 52.6% of the sample (n = 10) were considered as a “Targeted” for intervention wheres 21.1% (n = 4) as “Clinical” risk (Table 1). The domain that presented the highest average was Child Problems, as discomfort in hospital appointment, sadness or isolation; excessive shyness or unreasonable bond with any member of the family, difficulties in making/keeping friends, and victim of violence. Secondly, they presented problems in Social Support with items as having no help to care for the child, provide emotional support, financial support or information. These families also presented problems with the Family Structure and Resources, with items include parents under 21 years of age, less than two adults in the house in the house over 18 years, more than three children under the age of 18, schooling less than high school completion, marital status single/separated/divorced, transportation to the hospital, many financial difficulties and difficulty to manage the household/car costs/buying food/medical expenses.
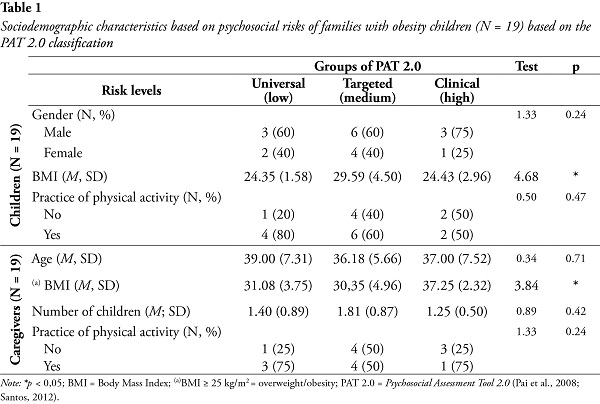
The Targeted level group included those participants with some psychosocial support resources, but with present risk factors, such as parental stress, increasing the risk for the patient. The Clinical level group included those participants with reduced resources for psychosocial support, besides chronic stress with several difficulties already installed. It is the group at a higher risk, is associated with a lower adjustment and adherence to the treatment unless there are interventions. The Universal risk of 26.3% of the participants (n = 5) revealed to be at low psychosocial risk for the child as well as an adequate support network.
Being single mother was more associated with psychosocial risk. Additionally, an association between the levels of psychosocial risk and the mother´s marital status in which those single mothers showed a higher frequency of higher psychosocial risk was found (p < 0.05).
Table 2 shows the most frequent food control strategies. The Spearman test detected a moderate and inverse correlation between the higher family psychosocial risk and the lower involvement of the child in family meals (ρ = -0.488; p = 0.05).
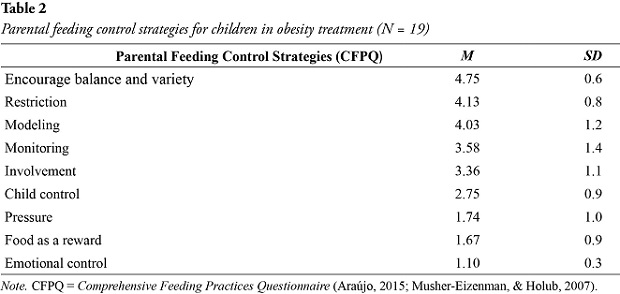
Table 3 shows the most frequent families of coping with the child’s overweight/obesity and the adaptive coping strategies which were most frequent. Additionally, the emotional reactions most reported by participants were sadness. The Games-Howell post hoc test indicated that the mean of the group at “Clinical” psychosocial risk is statistically higher than the average at the “Targeted” level for the Opposition, maladaptive coping (p = 0.05). This means that families at clinical, psychosocial risk present a higher frequency of Opposition, maladaptive coping, as a reaction to a threat perception of Autonomy.
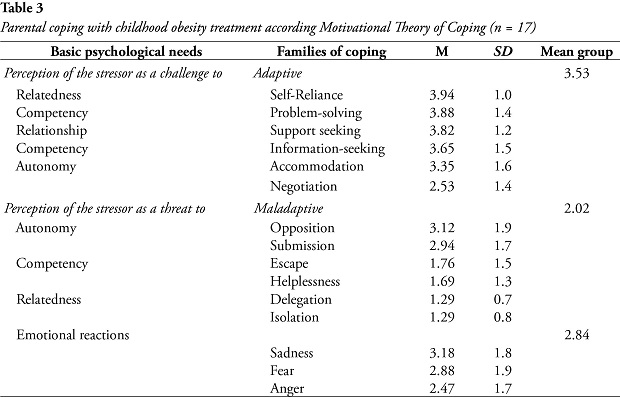
Through the coping interview (Table 4), the most common stressors were identified: food control; the child does not practice physical activities; difficulty in buying clothes for the child; concern about bullying, the child´s health status; dealing with the child´s anxious behavior; concern about weight, and lack of family support. Stressors are perceived by family members more as a challenge to the need for Relatedness, followed by the need for Competence and, finally, Autonomy.
Families referred to as “Targeted” for intervention for family psychosocial risk, coping with the stress of treating the child’s obesity reported a greater variety of coping strategies. The submission was the most common maladaptive coping strategy. Only two mothers presented normal weight, and other family members were obese or overweight. Families at “Universal” psychosocial risk presented more Self-Reliance, an adoptive family of coping.
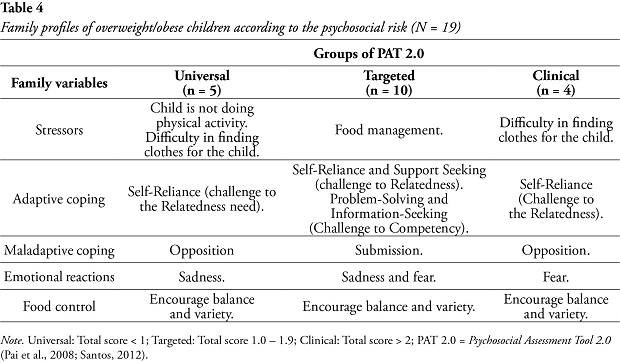
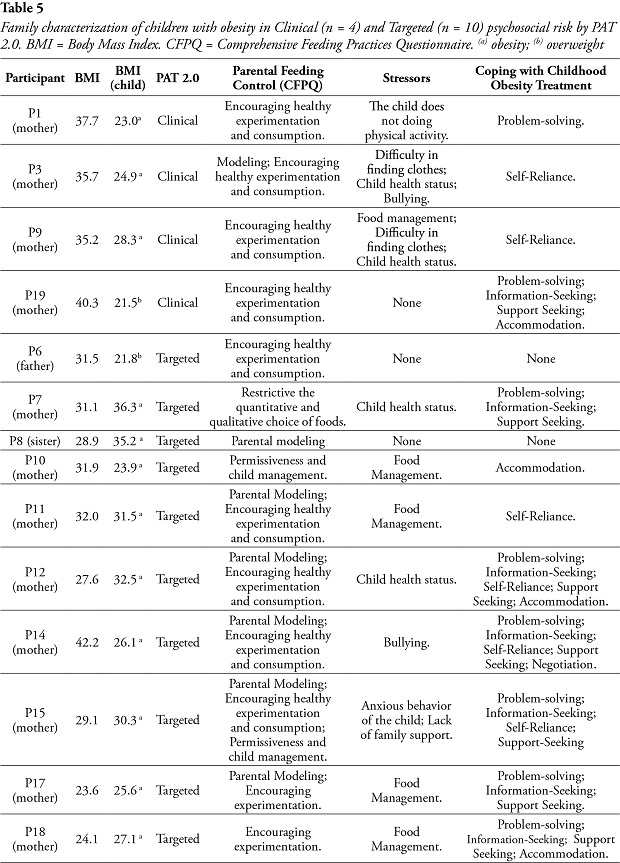
As shown in Table 5, sadness was the most prominent emotional reaction of all caregivers. Additionally, parental control of food is characterized by the encouragement of experimentation and healthy consumption.
DISCUSSION
This study evaluated the relationship between family psychosocial risk and some relevant variables to treatment adherence in overweight/obesity children. Main data indicated that children living in families with higher psychosocial risk had less involvement with the family feeding context. This stressful condition affects parental control of feeding and the relationship with the children, mainly because the responsible family member is the mother (Hoffman et al., 2016). In this sense, is important to know the caregiver feeding plays an important role, as proposed by Eneli et al. (2015). Most families were indicated for professional intervention, such as Targeted and Clinical, like to other study results, such as pediatric patients with cancer (Kazak et al., 2015; Santos, 2012). Similar to family members of children with chronic diseases at psychosocial risk, indicative of specific intervention and directed support, results in this study also revealed that family members of overweight/obesity children also call for this type of intervention and support.
Another psychosocial variable was highlighted in this sample, showing single mothers at higher psychosocial risk. Some studies have shown that those children who live with one or none of the biological parents increase the risk of desadaptative behaviors, such as abnormal eating habits, low school performance and sedentary lifestyle (Vázquez-Nava et al., 2013). Additionally, professional activities of the family member who is responsible for the household do not allow some essential parental functions to be fulfilled. On the other hand, those children from families with married mothers may have a healthier BMI due to low levels of stress and high emotional support in these settings than in families of single mothers (Grow et al., 2010; Tate et al., 2015).
A pattern of repetition of the disease in the family, observed by the obesity of the family members of this sample, makes up another risk factor for the children (Smith et al., 2018; Wang & Lim, 2012). Sedentary family lifestyle maintains this framework and contributes to increasing public health indicators (Brasil, Ministério do Esporte, 2015). However, interesting data were obtained, such as the association between the mother´s physical activity and the child´s, showing how the family model can promote a change in this situation (Van Allen et al., 2015). In this sense, it is noteworthy the meaning of obesity for the family, the patterns of food interaction and control as well as the values transmitted to its members (Hoffmann et al., 2016). It facilitates the intervention of these families to present a more adaptive coping pattern, with problem-solving coping strategies, which is focused on changing eating habits and physical activities (Nguyen & Bera, 2016).
This coping pattern associated with information-seeking coping strategies promotes the perception of competence to deal with the situation (Fenner et al., 2013; Skinner et al., 2003; Skinner & Zimmer-Gembeck, 2016). Once more, the psychosocial issue proved to be relevant, as family members of the group at higher risk presented a maladaptive coping, with opposition coping strategies. This profile is intensified by the emotional coping base present in families with higher psychosocial risk, centered on negative affection (anger, sadness, and fear), making it difficult to collaborate in the treatment of overweight/obesity (Bellodi, 2018; Tate et al., 2015).
Despite the small sample, it was possible to identify a profile of families at higher psychosocial risk - they are typically composed of single mothers who present problems in social support, family structure, and resources, and have problems with the child. This is an example how works the model of pediatric obesity proposed by Smith et al. (2018), and how the cumulative exposure to risks and dysregulation in response to stress contribute to pediatric obesity (Evans & Pilyoung, 2013). This sample presents opposition coping strategies, with emotional reactions of sadness and fear, perceiving the stressors as a threat to their need for autonomy; children are less involved in family meals; present greater difficulty in food control, use food as a reward, being in chronic stress conditions, less likely to be adherent to treatment, and requiring multi-professional interventions with health professionals in the social and mental health spheres (Campos et al., 2017; Fenner et al., 2013; Filgueiras & Sawaya, 2018; Matwiejczyk et al., 2018). Expanding the repertoire of coping, as presented by families at medium psychosocial risk (“Targeted”) may be a way to increase adherence to treatment; as well as encouraging physical activity as a way of promoting health and preventing the child´s overweight.
Therefore, it is possible to understand better the factors that contribute to and hamper health interventions as proposed by Enely et al. (2015) and Musher-Eizenman and Kiefner (2013). The data of this study contribute to identify and classify the family psychosocial risk of these families, showing the association between social support problems and parental control practices of the food and to the way in which the families deal with the problem. The psychosocial risk condition of this sample can be verified, but the differentiation of the risk level, indicative of the need for specific interventions, can subsidize the practices of health professionals in this population.
REFERENCES
Araújo, G. S. (2015). Práticas parentais alimentares e sua relação com o consumo de alimentos na infância. [Parental feeding practices and their relation to food consumption in childhood]. Master Dissertation. Universidade de Brasília, Brasília, DF, Brazil. Retrieved from: http://repositorio.unb.br/bitstream/10482/19004/1/2015_GiovannaSoutinhoAra%C3%BAjo.pdf
Bellodi, A. C. (2018). Obesidade em crianças e adolescentes: Temperamento, estresse, coping e risco psicossocial familiar [Obesity in children and adolescents: Temperament, stress, coping and familiar psychosocial risk]. Doctorate Thesis. Pontifícia Universidade Católica de Campinas, Campinas, SP, Brazil. Retrieved from: http://tede.bibliotecadigital.puc-campinas.edu.br:8080/jspui/handle/tede/1054
Brasil. Ministério da Saúde. (2014). Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico – VIGITEL [Surveillance of Risk Factors and Protection for Chronic Diseases by Telephone Inquiry – VIGITEL]. Brasília, DF. Retrieved from: http://portalms.saude.gov.br/vigilancia-em-saude/indicadores-de-saude/vigilancia-de-fatores-de-risco-e-protecao-para-doencas-cronicas-por-inquerito-telefonico-vigitel
Brasil. Ministério do Esporte. (2015). Diagnóstico Nacional do Esporte – DIESPORTE. [National Survey of Sport – DIESPORTE]. Brasília. Retrieved from: http:// www.esporte.gov.br/diesporte
Campos, M. L. B., Machado, M. M. T., Azevedo, D. V. & Silva, K. A. (2017). Dietary patterns of obese children: Maternal perceptions and experiences. Revista Nutrição, 30(2), 197-207. doi: 10.1590/1678-98652017000200005 [ Links ]
Cintra, I. P., Passos, M. A. Z., Santos, L. C., Machado, H. C., & Fisberg, M. (2014). Waist-to-height ratio percentiles and cutoffs for obesity: A cross-sectional study in Brazilian adolescents. Journal of Health, Population and Nutrition, 32(3), 411-419. Retrieved from: https://www.ncbi.nlm.nih.gov/pubmed/25395904 [ Links ]
Eneli, I. U., Tylka, T. L., Watowicz, R. P., Hummel, J., Ritter, J., & Lumeng, J. C. (2015). Targeting feeding and eating behaviors: Development of the feeding dynamic intervention for caregivers of 2-to 5-year-old children. Journal of Obesity, Article 964249, 1-8. doi: 10.1155/2015/964249 [ Links ]
Evans, G.W., & Pilyoung, K. (2013). Childhood poverty, chronic stress, self-regulation, and coping. Child Development Perspective, 7(1), 43–48. doi: https://doi.org/10.1111/cdep.12013
Fenner, A. A., Straker, L. M., Davis, M. C., & Hagger, M. S. (2013). Theoretical underpinnings of a need-supportive intervention to address sustained healthy lifestyle changes in overweight and obese adolescents. Psychology of Sport and Exercise, 14, 819-829. doi: http://dx.doi.org/10.1016/j.psychsport.2013.06.005 [ Links ]
Filgueiras, A. R., & Sawaya, A. L. (2018). Multidisciplinary and motivational intervention for the treatment of low income Brazilian obese adolescents: Pilot study. Revista Paulista de Pediatria, 36(2),186-191. doi:10.1590/1984-0462/;2018;36;2;00014 [ Links ]
Grow, H. M. G., Cook, A. J., Arterburn, D. E., Saelens, B. E., Drewnowski, A., & Lozano, P. (2010). Child obesity associated with social disadvantage of children´s neighborhoods. Social Science & Medicine, 71(3), 584-591. doi: 10.1016/j.socscimed.2010.04.018 [ Links ]
Guimarães, C. A. (2015). Cuidadores familiares de pacientes oncológicos pediátricos em fases distintas da doença: Processo de enfrentamento. [Family caregivers of pediatric oncology patients in different stages of the disease: Coping process]. Doctorate Thesis, Pontifícia Universidade Católica de Campinas. Campinas, SP, Brazil. Retrieved from: http://tede.bibliotecadigital.puc-campinas.edu.br:8080/jspui/handle/tede/466
Hoffmann D. A., Marx, J. M., Kiefner-Burmeister, A., & Musher-Eizenman, D. R. (2016). Influence of maternal feeding goals and practices on children’s eating behaviors. Appetite, 107, 21-27. Doi: http://dx.doi.org/10.1016/j.appet.2016.07.014
Instituto Brasileiro de Geografia e Estatística (2008). Pesquisa de Orçamentos Familiares (POF 2008–09). Retrieved from: http://www.ibge.gov.br/home/estatistica/populacao/condicaodevida/pof/2008_2009_aquisicao/pof20082009_aquisicao.pdf
Kazak, A. E., Schneider, S., Didonato, S., & Pai, A. L. (2015). Family psychosocial risk screening guided by the Pediatric Psychosocial Preventative Health Model (PPPHM) using the Psychosocial Assessment Tool (PAT). Acta Oncologica, 54(5), 574-580. doi: 10.3109/0284186X.2014.995774 [ Links ]
Lees, D. (2007). An empirical investigation of the motivation theory of coping in middle to late childhood. Doctorate Thesis. Griffity University, USA. Retrieved from: https://www120.secure.griffith.edu.au/rch/items/00104138-8f7b-615f-9719-4d6757976b28/1/
Matwiejczyk, L., Mehta, K., Scott, J., Tonkin, E., & Coveney, J. (2018). Characteristics of effective interventions promoting healthy eating for preschoolers in childcare settings: An umbrella review. nutrients, 10(3), 293. doi: 10.3390/nu10030293 [ Links ]
Musher-Eizenman, D., & Holub, S. (2007). Comprehensive Feeding Practices Questionnaire: Validation of a new measure of parental feeding practices. Journal of Pediatric Psychology, 32(8), 960-972. doi: 10.1093/jpepsy/jsm037 [ Links ]
Musher-Eizenman, D. R., & Kiefner, A. (2013). Food parenting: A selective review of current measurement and an empirical examination to inform future measurement. Childhood Obesity, 9(Suppl 1), S32-S39. doi: 10.1089/chi.2013.0030 [ Links ]
Ng, M., Fleming, T., Robinson, M., Thomson, B., Graetz, N., Margono, C., . . . Gakidou, E. (2014). Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 384(9945), 766-781. doi:10.1016/S0140-6736(14)60460-8
Nguyen, C., & Bera, K. (2016). Bio-psycho-social approach to the treatment of childhood obesity: A novel technique. Journal of Childhood Obesity, 1(4), 16 doi: 10.21767/2572-5394.10016 [ Links ]
Pai, A. L., Patiño-Fernández, A. M., McSherry, M., Beele, D., Alderfer, M. A., Reilly, A. T. . . . Kazak, A. E. (2008). The Psychosocial Assessment Tool (PAT 2.0): Psychometric properties of a screener for psychosocial distress in families of children newly diagnosed with cancer. Journal Pediatric Psychology, 33(1), 50-62. doi: 10.1093/jpepsy/jsm053 [ Links ]
Sahoo, K., Sahoo, B. Choudhury, A. C., Sofi, N. Y., Kumar, R., & Bhadoria, A. S. (2015). Childhood obesity: Causes and consequences. Journal of Family Medicine and Primary Care. 4(2), 187–192. doi:10.4103/2249-4863.154628
Santos, S. S. (2012). Adaptação transcultural e validação do “Psychosocial Assessment Tool (PAT 2.0): Instrumento de avaliação psicossocial de famílias de pacientes pediátricos recém- diagnosticados com cancer. [Cross-cultural adaptation and validation of the Psychosocial Assessment Tool (PAT 2.0): An instrument for the psychosocial evaluation of families of pediatric patients newly diagnosed with cancer]. Master Thesis, Fundação Antônio Prudente, São Paulo, SP, Brazil. Retrieved from: http://www.accamargo.org.br/teses-dissertacoes-em-2012
Skinner, E. A., Edge, K., Altman, J., & Sherwood, H. (2003). Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychological Bulletin, 129(2), 216-69. doi:10.1037/0033-2909.129.2.216 [ Links ]
Skinner, E. A., & Zimmer-Gembeck, M. J. (2016). The development of coping – Stress, Neurophysiology, Social Relationships and Resilience during childhood and adolescence. Switzerland: Springer International Publishing.
Smith, J. D., Egan, K. N., Montaño, Z., Dawson-McClure, S., Jake-Schoffman, D. E., Larson, M., & St. George, S. M. (2018). A developmental cascade perspective of pediatric obesity: Conceptual model and scoping review. Health Psychology Review, 5, 1-23. doi: 10.1080/17437199.2018.1457450 [ Links ]
Tate, E. B., Wood, W., Liao, Y., & Dunton, G. F. (2015). Do stressed mothers have heavier children?: A meta-analysis on the relationship between maternal stress and child body mass index. Obesity Review, 16(5), 351–361. doi:10.1111/obr.12262.
The Global BMI Mortality Collaboration. (2016). Body-mass index and all-cause mortality: Individual participant-data meta-analysis of 239 prospective studies in four continents. The Lancet, 388(20), 776-786. doi:10.1016/S0140-6736(16)30175-1 [ Links ]
Van Allen, J., Borner, K. B., Gayes, L. A., & Steele, R. G. (2015). Weighing physical activity: The impact of a family-based group lifestyle intervention for pediatric obesity on participants’ physical activity. Journal of Pediatric Psychology, 40(2), 193-202. doi:http://dx.doi.org/10.1093/jpepsy/jsu077
Vázquez-Nava, F., Treviño-Garcia-Manzo, N., Vázquez-Rodríguez, C. F., & Vázquez-Rodríguez, E. M. (2013). Association between family structure, maternal education level, and maternal employment with sedentary lifestyle in primary school-age children. Jornal de Pediatria, 89(2), 145-150. doi:http://dx.doi.org/10.1016/j.jped.2013.03.009 [ Links ]
Wang, Y., & Lim, H. (2012). The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. International Review Psychiatry, 24(3), 176-88. doi:http://dx.doi.org/10.3109/09540261.2012.688195 [ Links ]
World Health Organization. Multicentre Growth Reference Study Group. (2006). WHO Child Growth Standards based on length/height, weight and age. Acta Paediatric, 450(Suppl.), 76-85. [PMID: 1681768] [ Links ]
World Health Organization. (2014). Global strategy on a diet, physical activity and health: Childhood overweight and obesity. Geneva: WHO. Retrieved from: http://www.who.int/dietphysicalactivity/childhood/en/ [ Links ]
World Health Organization. (2017). The challenge of obesity in the WHO European Region and the strategies for response. Geneva: WHO Regional Office for Europe. Retrieved from: http://www.publichealth.ie/files/file/WHO%20European%20Ministerial%20Conference%20on%20Counteracting%20Obesity%20-%20Turkey.pdf [ Links ]
Endereço para correspondência:
André Luiz Monezi Andrade
Pontifícia Universidade Católica de Campinas, Centro de Ciências da Vida (CCV).
Pontifícia Universidade Católica de Campinas (PUCC - Campus II)
Jardim Ipaussurama
13060904 - Campinas, SP - Brasil
Telefone: (19) 33437000.
andremonezi@gmail.com
Recebido em 25/05/2018
Aceito em 29/06/2018














