SMAD. Revista eletrônica saúde mental álcool e drogas
ISSN 1806-6976
SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. port.) vol.9 no.2 Ribeirão Preto ago. 2013
ORIGINAL ARTICLE
Profile of patients with personality disorder diagnosis at a mental health services clinic
Perfil de los usuarios con diagnóstico de trastornos de personalidad de un servicio de salud mental
Leonardo Naves dos ReisI; Emilene ReisdorferII; Edilaine Cristina da Silva Gherardi-DonatoIII
IDoctoral student, Escola de Enfermagem de Ribeirão Preto, Universidade de São Paulo, WHO Collaborating Centre for Nursing Research Development, Ribeirão Preto, SP, Brazil
IIPost-doctoral fellow, University of Alberta, Edmonton, AB, Canada
IIIPhD, Associate Professor, Escola de Enfermagem de Ribeirão Preto, Universidade de São Paulo, WHO Collaborating Centre for Nursing Research Development, Ribeirão Preto, SP, Brazil
ABSTRACT
Personality disorders are a persistent pattern of inner experience or behavior dissonant from the social norms and prevailing culture. The aim of this study was to determine the prevalence of patients with personality disorders in an outpatient mental health services clinic, as well as to identify their social-demographic characteristics, employing a cross-sectional descriptive and exploratory methodology. Personality disorder was the main diagnosis for approximately 16% of the sample. The most prevalent type was the emotionally unstable personality disorder or borderline personality disorder (BPD) in young women with low educational levels, and about 16% has required hospital confinement in their lifetime. The results obtained in this study allow a better understanding of the patients´ needs, and they can help define strategies to meet them.
Descriptors: Personality Disorders; Cross-Sectional Studies; Health Services.
RESUMEN
Los trastornos de personalidad constituyen una calidad persistente de vivencia íntima o comportamiento distinto de las normas sociales y de la cultura vigente. El objetivo de este trabajo fue verificar la superioridad de portadores de trastornos de personalidad en un servicio de ambulatorio de salud mental, así como identificar sus características socio-demográficas. Se realizó un estudio transversal descriptivo y exploratorio. Aproximadamente 16% presentaron como diagnóstico principal trastorno de personalidad. El tipo más prevalente fue el trastorno de personalidad emocionalmente inestable o borderline, en mujeres, jóvenes, con baja escolaridad y cerca del 16% ya necesitaron una internación hospitalaria en la vida. Los resultados logrados en eses estudio permiten una mejor comprensión de las necesidades de los usuarios y pueden auxiliar en la definición de estrategias de servicio.
Descriptores: Trastornos de la Personalidad; Estudios Transversales; Servicios de Salud.
Introduction
Mental disorders belong to the chronic non-communicable class of diseases; they are a global health problem and a threat to the health and human development, especially in underdeveloped and developing countries. In 2001, 450 million people suffered from mental disorders, caused by the interaction between genetic and environmental factors(1).
Among mental disorders, the personality and adult behavior distortions category is distinctive because it contains the different types of personality disorders, such as habit and impulse disorder, gender identity and sexual preference disorders(2).
Personality disorders are a persistent pattern of inner experience or behavior dissonant from the social norms and prevailing culture. They begin in adolescence or early adulthood, and they can be damaging and cause much suffering(3).
In Brazil, a study conducted in 1985, demonstrated a 0.9% prevalence of personality disorders over the lifetime, and a predominance of females among those affected by the disease(4).
Among the subtypes, the estimate for the prevalence of antisocial personality disorder in the general population is about 3% for men and 1% for women. As for the schizoid personality disorder, the estimated prevalence was between 3 and 7.5%. With regard to the schizotypal personality disorder, an estimated 3% of the populations suffer from it, and that between 2 and 3% are borderline; and it is twice as higher in women than men(3).
The creation of the National Health System in 1988, brought changes to the health care model, including the field of mental health(5), with increasing efforts toward deinstitutionalization of patients with psychiatric disorders. In this changing context, one of the main challenges is to identify the profile of the patients, searching for a characterization that allows the better employment of the service(6).
The epidemiological survey is a powerful strategy to increase knowledge regarding a population; it can provide data to pinpoint specificities of the public serviced and to demonstrate their health requirements. The importance of epidemiological studies in health services results from its ability to produce knowledge in the decision making process involved in the formulation of health policies, the organization of the system, and interventions aimed at solving specific problems(7).
In this context of action planning in mental health, it is necessary to know the actual demands that each disorder places in the service, considering the peculiarities of each pathology, such as the course of the disease, its social damages, and the treatment recommended. This perspective allows for improvements in the mental health services, especially at the secondary care levels, in the case of this work, in terms of physical and human resources.
The need to provide comprehensive and equitable care to patients of mental health services; the lack of information on the epidemiological profile of the population served, and particularly the possibility of increasing the chances of interventions targeted to patients with personality disorders, motivated this work. The objective was to determine the prevalence of patients with personality disorders in an outpatient mental health services clinic, as well as to identify their social-demographic characteristics.
Methodology
The project was approved by the ethics committee on research of the Ribeirão Preto School of Nursing from the University of São Paulo (protocol 1446/2011), meeting the standards established by Resolution 196/96 of the National Health Council
The study employed a cross-sectional descriptive and exploratory methodology. The population consisted of all individuals under treatment at the Center for Mental Health (NSM) of the Health Center School at the Ribeirão Preto School of Medicine, from April to May 2012.
The NSM is a specialized outpatient care unit, formed by physicians, nurses, Psychiatry residents, nurse aides and psychologists, providing free mental health care to the population over 18 years of age, from the Western Sanitary District of the municipality of Ribeirão Preto.
The services provided by the NSM consist of physicians scheduled appointments and the occasional psychotherapy appointment, nursing consultations, supervised medication for some patients with difficulties adhering to the therapy. In addition to home visits conducted by undergraduate and graduate students since the health service provides theoretical and practical teaching scenarios and study site for research.
Access to the service is by primary care, by referral, or transfers from other second-level mental health services.
The NSM was chosen as the study site because it constitutes of an outpatient mental health service clinic located in a highly populated area of the municipality (about 170,000 inhabitants, representing about 25% of the total population). In addition to being a teaching campus for Undergraduate and Graduate students attending the Ribeirão Preto School of Nursing, USP.
The analysis of the study population resulted in 244 patients with personality disorder as the main diagnosis (inclusion criterion). The data analysis consisted of a descriptive statistics on the social demographic characteristics of patients with a personality disorder diagnosis. In this study, personality disorder had a wide definition to include all patients with a CID-10 F60 diagnosis.
The independent variables were as follows: age (18-29, 30-39, 40-49, 50-59, 60-69, 70-79 and 80 or older); gender (male or female); educational level (illiterate, an elementary school dropout, finished elementary school, high school dropout, high school graduate, college dropout, college graduate), and most prevalent psychiatric diagnoses, divided according to chapter V of the CID-10.
In addition to the variable called "hospital confinement", divided into "yes" if the patient has been admitted to the psychiatric unit at least once and "no" for never has been subjected to hospital confinement. Finally, a comparison was performed between two groups of patients with diagnoses of personality disorders and the other patients of NSM.
It is known that psychiatric diagnosis depends on several factors, including the professional interpretation. Considering that 93% of patients at the NSM were attended by psychiatrists and 7% were attended by Psychiatry residents, the following bias relating to the variable "diagnosis" was inserted, the most recent diagnosis contained in the patient's records, regardless of the attending professional(8).
Results
There were 1,281 patients receiving treatment at the NSM during the study. Approximately 16% had as main diagnosis a personality disorder (244); therefore, it became necessary to study all the different types of personality disorders diagnosed at the NSM.
Figure 1 shows the most frequent types of personality disorders treated at the service clinic. The most prevalent is the F 60.3 diagnoses, emotionally unstable personality disorder, or borderline. Followed by the histrionic personality and the nonspecific personality disorders. The other disorders had a low prevalence, being grouped in the "others" category (F60, F60.2, F60.6, F60.7, F61, F61.0, F63.3, F64.0, F65, F68.1, and F68.2).
As observed in the overall population of NSM patients, the women were also the majority among those diagnosed with personality disorders; however, their percentages are even higher, constituting almost 81% of the total compared with about 69% of the NSM profile.
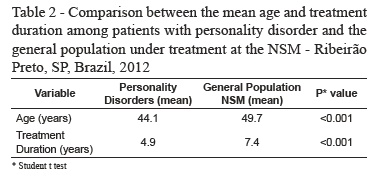
Regarding the age distribution, the average age of patients with personality disorders is lower than in the general population of patients at the NSM. This difference is even more evident when comparing the mean age calculated; for those diagnosed with personality disorders the mean was about 44.1 years and in the overall picture of the NSM 49.7 years (Table 2), this difference is statistically significant. It is also relevant that less than 10% of those with personality disorder are 60 years or older.
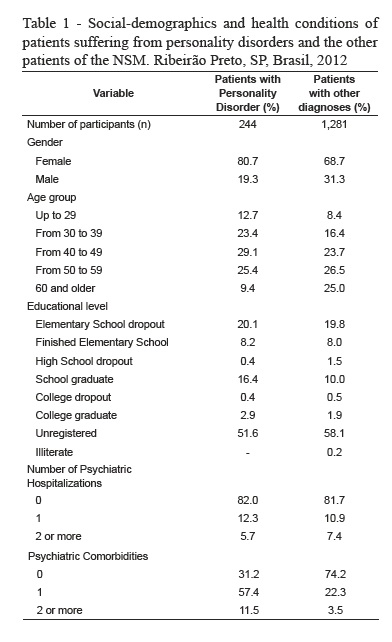
In relation to the distribution by educational levels, there is a certain similarity between the profiles of diagnosed personality disorder patients and the overall picture of the NSM. About 58% of those diagnosed with personality disorders have at the most elementary education. However, in general, patients with personality disorders have higher educational levels compared to the general profile of the NSM, concentrated in the secondary and tertiary levels.
Regarding the need for hospitalization, the vast majority of patients with personality disorders never required hospitalization, similar to the results from the general population of patients at the NSM.
The duration of the psychiatric treatment also showed a statistically significant difference between the two groups. Patients with personality disorders have a lower mean for the treatment duration compared with the general population of patients (Table 2).
Discussion
This study examined the prevalence of personality disorder diagnosis in a secondary service of mental health care in a large city, in the state of São Paulo. The outcome prevalence was 16%, with the main disorder being identified as emotionally unstable personality disorder or BPD (approximately 70%) with a higher prevalence among women, ages between 40 and 49 years, and lower levels of education. Furthermore, 18% of the patients have required hospitalization at some point in life.
Their profiles were epidemiologically compared with the other patients attending the service clinic. Patients with personality disorders have a gender distribution similar to the other patients; they are younger, with a slightly higher educational level, with the hospitalization prevalence similar to the other patients, and the duration of psychiatric treatment is lower.
One of the difficulties encountered during this study was the diversity of diagnoses. Because, this is a service that employs medical students and residents, a lot of times patients are seen by a diverse number of professionals throughout the years; thus, resulting in several modifications of the diagnosis. As inclusion criteria, the choice was for the last diagnosis registered in the medical records.
Furthermore, it was a challenge to find similar studies for the comparison of the results. A systematic search performed in the SciELO, PubMed, and Medline databases, using the keywords "personality disorders", and "prevalence", resulted in only a few articles related to the topic of this study. However, there were some similar articles related to borderline emotionally unstable personality disorder. Thus, greater focus will be given to this diagnosis because it was the most prevalent in the study.
The prevalence of personality disorders was about 16%, similar to the 13.4% results from a 2001 Norwegian study(9) conducted with a community sample.
Among the various types of personality disorders, the most frequent in this study was the emotionally unstable personality disorder or borderline, which is consistent with the available literature(10). The expected prevalence of this disorder in patients from outpatient clinics is around 10%(11).
With regard to the gender, the sample presented distribution similar to the literature(12). Studies show a prevalence of about 75% of women affected by the disorder(10), close to the 81% found in this study.
Despite of the difficulties in determining the causes of the disease, studies show that gender plays an essential role. Researchers have reported substantial differences in the serotonergic function between men and women, which may be related to the development of this disorder(13).
Regarding the age of the subjects studied, there was an inverse relationship to results usually found in the literature. Studies have found a higher prevalence among young adults(9 to 10, 14) , whereas in the present study, there is a larger number of cases among the 40-49 age group.
This difference could be related to the fact that many people can live with this disorder for many years and only search for medical help at a later stage of life. This need for intervention may be caused by a catastrophic occurrence such as a major loss, a highly confrontational situation, among others(10).
Approximately 58% of individuals surveyed have low educational levels, i.e., finished elementary school was the highest level achieved. A study found in the literature demonstrated that the prevalence of personality disorders is greater in individuals with lower educational levels (9). One possible explanation for this finding is the frequent early onset of the disease, hindering their participation in school activities. In addition, there is a sub-recording of this information and this data refers to information collected for the study.
As for the need for hospitalization during their lifetime, there is a prevalence of about 16%. A comparison with the remaining individuals with different pathologies, demonstrated that patients with personality disorders required more hospitalization than patients suffering from depression (5%), and less than the schizophrenic patients (37%).
These findings are in agreement with a study conducted among patients that were confined to a general hospital for 10 years(15). It shows a 15% prevalence of personality disorders, 19% of schizophrenia, and 30% of mood disorders.
At this point, it is essential to make a comparison between the data from this study and the results from a similar survey conducted in the United States, where 72% of the patients required hospitalization(11). The author states that traditionally, outpatient services in that country focus their attention on individuals with mood disorders and schizophrenia, presenting difficulties in dealing with crises situations of patients with personality disorders. Individuals with this disorder tend to exhibit aggressive and impulsive behaviors, and self-destructive attitudes, including suicide attempts, of which around 10% of patients succeed in ending their lives(16).
Despite all the controversies surrounding the topic, psychiatric hospitalization remains an indispensable resource, especially for individuals in crises or who suffers from drug treatment complications. In the specific case of hospital admissions for people with personality disorders, this feature is indispensable in cases of suicidal thoughts or attempted suicide.
The analysis of the epidemiological profile traced in this study demonstrated the importance of a better understanding of the patients using the health care services. It is necessary to consider that in addition to the specific services for mental health care, these patients also use the outpatient, primary health care and general hospital services.
Final Considerations
The results of this study add to the knowledge of the epidemiological characteristics of patients with personality disorders treated at public health services in Brazil. The availability of only a few studies demonstrates the need for greater emphasis in this area of psychiatry.
The knowledge of the profiles of these patients and a better understanding of their needs can assist in the strategies for finding and keeping them in the service; thus, improving the quality of care. It is hoped that the findings from this study will contribute to increase the visibility of people with personality disorders being attended at the different health services, providing care targeted to their specific needs.
References
1. Volcan SM, Sousa PL, Mari JJ, Horta BL. Relationship between spiritual well-being and minor psychiatric disorders: a cross-sectional study. Rev Saúde Pública. 2003 Aug;37(4):440-5. [ Links ]
2. WHO. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic criteria for research. Geneve: WHO; 1993. [ Links ]
3. Sadock B, Sadock V. Compêndio de psiquiatria: ciência do comportamento e psiquiatria clínica. 9 ed. Porto Alegre: Artmed; 2007. [ Links ]
4. Morgado AF, Coutinho ESF. Dados de epidemiologia descritiva de transtornos mentais em grupos populacionais do Brasil. Cad Saúde Pública. 1985;1:327-47. [ Links ]
5. Campos CMS, Soares CB. A produção de serviços de saúde mental: a concepção de trabalhadores. Ciênc Saúde Coletiva. 2003;8:621-8. [ Links ]
6. Nunes M, Jucá VJ, Valentim CPB. Ações de saúde mental no Programa Saúde da Família: confluências e dissonâncias das práticas com os princípios das reformas psiquiátrica e sanitária. Cad Saúde Pública. 2007;23:2375-84. [ Links ]
7. Paim JS. Epidemiologia e planejamento: a recomposição das práticas epidemiológicas na gestão do SUS. Ciênc Saúde Coletiva. 2003;8:557-67. [ Links ]
8. Dalgalarrondo P. Psicopatologia e semiologia dos transtornos mentais. Porto Alegre: Artmed; 2000. [ Links ]
9. Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Arch Gen Psychiatry. 2001 Jun;58(6):590-6. [ Links ]
10. APA. Diagnostic and Statistical Manual of Mental Disorders. 4 ed. Washington: American Psychiatric Press; 1994. [ Links ]
11. Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M. Borderline personality disorder. Lancet. 2004 Jul 31-Aug 6;364(9432):453-61. [ Links ]
12. Widiger TA, Weissman MM. Epidemiology of borderline personality disorder. Hosp Commun Psychiatry. 1991 Oct;42(10):1015-21. [ Links ]
13. Soloff PH, Kelly TM, Strotmeyer SJ, Malone KM, Mann JJ. Impulsivity, gender, and response to fenfluramine challenge in borderline personality disorder. Psychiatr Res. 2003 Jul 15;119(1-2):11-24. [ Links ]
14. Giesen-Bloo J, van Dyck R, Spinhoven P, van Tilburg W, Dirksen C, van Asselt T, et al. Outpatient psychotherapy for borderline personality disorder: randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry. 2006 Jun;63(6):649-58. [ Links ]
15. Dalgalarrondo P, Botega NJ, Banzato CE. Patients who benefit from psychiatric admission in the general hospital. Rev Saúde Pública. 2003 Oct;37(5):629-34. [ Links ]
16. Soloff PH, Fabio A, Kelly TM, Malone KM, Mann JJ. High-lethality status in patients with borderline personality disorder. J Pers Disord. 2005 Aug;19(4):386-99. [ Links ]
 Correspondence
Correspondence
Edilaine Cristina da Silva Gherardi-Donato
Universidade de São Paulo. Escola de Enfermagem de Ribeirão Preto
Departamento de Enfermagem Psiquiátrica e Ciências Humanas
Av. Bandeirantes, 3900
Bairro: Monte Alegre
CEP: 14040-902, Ribeirão Preto, SP, Brasil
E-mail: nane@eerp.usp.br
Received: Oct. 17th 2012
Accepted: Apr. 23rd 2013













