Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Interamerican Journal of Psychology
versão impressa ISSN 0034-9690
Interam. j. psychol. v.42 n.2 Porto Alegre ago. 2008
Effectiveness of a Cognitive-Behavioral Intervention for Puerto Rican Children
La Efectividad de una Intervención Cognitiva-Conductual
José J. Cabiya1; Lymaries Padilla-Cotto; Karelyn González; Jovette Sanchez-Cestero; Alfonso Martínez-Taboas; Sean Sayers
Carlos Albizu University, San Juan Campus, Puerto Rico
ABSTRACT
This study evaluated the effectiveness of a cognitive-behavioral intervention for children with disruptive disorders and depressed mood. Four hundred thirty four boys and 174 girls, ages 8 to 13, attending public schools, were initially evaluated to determine the diagnosis of a disruptive disorder. Of those diagnosed with disruptive disorders, 278 were assigned to the two experimental groups. The Child Depression Inventory was administered to the children and the Bauermeister School Behavior Inventory was administered to the teachers at three different stages. At post-treatment, significant reductions were found in the treatment group vs. the control group in depressed mood and disruptive behaviors. Children in the treatment group showed further reductions at the follow-up in both areas.
Keywords: School age children, Aggressive behavior, Attention deficit hyperactivity disorder, Oppositional defiant disorder, Depression.
RESUMEN
Este estudio evaluó la efectividad de una intervención cognoscitiva/conductual para niños diagnosticados con trastornos disruptivos y depresión. Cuatrocientos treinta y cuatro niños y 174 niñas, entre 8 a 13 años y de escuelas públicas, fueron evaluados para determinar los diagnósticos de conductas disruptivas; sólo 278 fueron asignados a los grupos experimentales. El Inventario de Depresión de Kovacs fue administrado a los niños y el Inventario de Bauermeister de Conducta-Escuela fue administrado a maestros. Las medidas fueron administradas en tres momentos. Reducciones significativas en post-tratamiento fueron encontradas en el grupo del tratamiento vs. el grupo control en depresión y comportamientos disruptivos. Los niños en el tratamiento también mostraron reducciones significativas en el seguimiento de 6 meses en depresión y comportamientos disruptivos.
Palabras clave: Niños de edad escolar, Conducta agresiva, Desorden de déficit de atención con hiperactividad, Desorden oposicional desafiante, Depresión.
In recent years, studies have found high levels of psychiatric co-morbidity in children diagnosed with disruptive disorders (Pliszka, Carlson & Swanson, 1999). This high level of co-morbidity has been reported in culturally and regionally diverse epidemiological samples, as well as in clinical samples including samples from Spain (Cabanyes, García de Leon, Avila & Polaino- Lorente, 1994), México (Velázquez, Juárez, Caso-López & Cabrera, 2000) and Puerto Rico (Bauermeister et al., 2005). Findings from clinic-based samples indicate that children with Attention Deficit with Hyperactivity Disorder (ADHD) are more likely to meet diagnostic criteria for one or more mood disorders than are comparison children (Biederman, Faraone, Mick & Moore, 1996). Children with co-morbid ADHD and depressive symptoms also appear to be at higher risk for poor outcomes (e.g., suicidality) (Biederman et al.), aggressive behavior (Velázquez et al.) and drug abuse (Mirón, Serrano, Godás & Rodríguez, 1997). Moreover, in community samples, ADHD and other disruptive disorders have been associated with elevated levels of depressive symptoms (Bauermeister et al.; Treuting & Hinshaw, 2001).
Researchers (Brestan & Eyberg, 1998) have demonstrated recently that manual-based psychotherapies can successfully reduce disruptive behaviors in children diagnosed with disruptive disorders and depressed mood in this children, namely, ODD (Reid, Stratton & Hammond, 2003), ADHD (Miranda & Presentación, 2000), CD (Kazdin, 2003) and depressed children in children diagnosed with disruptive disorder (Kazdin). However, Roth and Fonagy (2005) concluded that empirically supported treatments of children who exhibit disruptive disorders have focused their attention only on “North American Caucasian samples” (p. 32). Moreover, Bernal and Scharron-del Río (2001) argue that no study have provided conclusive empirically-based support for any treatment with Latino children and youths living in the continental United States and even less to Puerto Ricans living in their native island.
Cognitive-behavioral interventions have been found to be particularly effective with non-minority children diagnosed with disruptive disorders and depression (Kazdin, 2003). Of particular interest to the present article is the cognitive-behavioral intervention developed by Lochman and Wells (2003). They proposed a cognitive-behavioral intervention for disruptive disorders which takes into consideration children’s social cognition in terms of how they perceive their social environment and how they respond to the perceived problems in that environment. The five stages of the model included: (a) encoding social cues, (b) making accurate interpretations and attributions about a social event, (c) generating a variety of adaptive solutions to the problem they perceive, (d) deciding which of these solutions to enact based on the strategy consequences, and (e) skillfully enacting the chosen strategy. Recently, Lochman and Wells (2003) demonstrated the effectiveness of this cognitive-behavioral intervention in reducing aggressive behaviors as well as other disruptive behaviors in children diagnosed with disruptive disorders. This therapeutic approach is a well-manualized and structured program where the children review examples of social encounters and review problem-solving components where they identify problems, generate solutions, and evaluate those solutions using pro-social judgment criteria. Also, specific skills to manage anger are practiced, with anger control strategies.
In conclusion, cognitive-behavioral interventions have been shown to be effective with non-minority populations in reducing disruptive behavior and depressed mood but there is no research up to date that has demonstrated the effectiveness of these interventions with Puerto Rican children who exhibit this type symptomatology. Thus, the main goal of the present pilot study was to evaluate transportability and efficacy of a cognitive-behavioral intervention administered in a group manner to Puerto Rican children who present significant symptomatology of both disruptive and depressive disorders.
Method
Participants
Six-hundred and eight students (434 boys and 174 girls) from ages 8 to 13 attending public schools of the San Juan (capital of Puerto Rico) metropolitan area, who were referred by their teacher for aggressive classroom behavior, were administered a symptoms checklist based on the DSM-IV-TR diagnostic criteria for disruptive disorders (American Psychiatric Association, 2000). A total of 355 children (249 boys and 106 girls) fulfilled the diagnostic criteria for one or more of the disruptive disorders, namely ADHD, ODD or CD. The children that fulfilled the inclusion criteria were then randomly assigned in equal numbers of both genders to the intervention or to a waiting list groups. No financial incentive was provided to the participants.
Informed consent to participate in the study was then requested from the parents of these children. The parents were explained that their participation was completely voluntary and that they were free to withdraw from the study at any time without penalty. They were explained the benefits and risks of their children’s participation in the study. Of those diagnosed with disruptive disorders, a total of 278 were finally assigned to the two experimental groups. The parents of 174 (124 boys and 50 girls) consented that their children participated in the intervention group while the parents of 104 children consented that their children participated in the waitlist group, but only 34 (22 boys and 12 girls) did complete the post-treatment evaluation.
The socioeconomic status of all of these children was low. Of the 174 children that started the intervention, 170 children (120 boys and 50 girls) completed the treatment and four dropped out. The outcome measures were administered to the two groups before the beginning of the intervention and a week after the 12 sessions were completed. Six months after the completion of treatment, 86 (51%) children in the treatment group were reassessed with all the outcome measures. The control group was not assessed at the follow-up. The two study groups were similar in age. The mean age of the intervention group was 10.58 (SD = 1.12) while the control group was 10.49 (SD = 1.11). Of the 170 children that receive the intervention, 86 children (57 boys and 29 girls) were evaluated again after 6 months for a follow-up. The mean age of this group was 10.13 (SD = 0.86).
Instruments
Bauermeister School Behavior Inventory (BSBI). This inventory, which is completed by teachers, consists of six scales for male children and five for female children. For this study, the Irritability/Hostility Subscale, High Activity/Impulsive and the Distractibility/ Low Motivation scales were studied as measures of disruptive behaviors. The Irritability/Hostility scale specifically was also used as a measure of aggressive behavior and is scored differently for boys and girls. This instrument was developed, validated and standardized for the Puerto Rican population (Bauermeister, 1994). Bauermeister found the test’s internal consistency fluctuated between .74 and .96 and that the test-re-test reliability (4 week period) fluctuated between .52 a .89.
Child Depression Inventory (CDI). The CDI is a selfreport scale consisting of 27 items related to depression. The scale was adapted for children and youths by Kovacs (1985). Scores of 0-11 are considered as absence of depression. Scores ranging between 12 and 18 are considered mild depression while scores 19 or higher are considered severe depression. The scale was translated and adapted for the Puerto Rican culture by Bernal, Rosselló, and Martínez (1997) and has shown an internal consistency of .82 and of .79 (Bernal et al.).
Procedure
Development of the culturally sensitive treatment manual. A treatment manual, written in Spanish, was developed based on the socio-cognitive model developed by Lochman and Wells (2003). The five steps of the model include: (a) encoding social cues, (b) making accurate interpretations and attributions about a social event, (c) generating a variety of adaptive solutions to the problem they perceive, (d) deciding which of these solutions to enact based on the strategy consequences, and (e) skillfully enacting the chosen strategy. The techniques described in the manual included role playing of different sketches where they were taught problems solving, self-control, conflict resolution and anger management techniques.
All the role playing sketches described in the manual were developed in a previous pilot study. In this pilot study, children, in conjunction with graduate research assistants, developed role-playing sketches, which were relevant and sensitive to their cultural milieu. The role playing sketches were determined to be culturally competent following Dana’s guidelines (Dana, 1998), namely, that they reflected typical events in their culture/ social class and that they be gender specific. The research team selected the final role-playing situations judged to satisfy these requirements, which then were included in the final version of the treatment manual used in the study.
Procedures to Guarantee Treatment Fidelity. Children who met the diagnostic criteria for inclusion in the study were assigned to treatment groups of eight children. Doctoral students in clinical psychology were trained by the project’s director, the first author of the present paper, on the implementation of his treatment manual. The project’s director conducted weekly meetings for the supervision of sessions according to the treatment manual. A plan to deal with ambiguities, which did arise, clearly defined “do’s” and “don’ts” in various situations, was developed and implemented to guarantee treatment fidelity. Specific situations that lead to deviations from the treatment plan were discussed in the supervision with the project’s director and specific steps were taken to guarantee that all aspects of the treatment manual were implemented.
Treatment Sessions
Treatment sessions were on average 50 minutes long with 10 minutes for social interaction. Treatment sessions were held in private rooms on school grounds. A general description of the sessions is presented next:
Sessions 1-2. The “Stop and Think” Technique for conflict resolution is presented. In this technique, participants are presented a series of culturally relevant vignettes in which they are taught how to (a) “stop” and define the problem, (b) “think” about possible alternatives to resolve the problem, and (c) concentrate and choose an alternative, which is appropriate to the situation. The participants practiced this technique by role-playing the appropriate responses in front of the group and all group members were encouraged to provide positive feedback to each other. The participating children were also taught how to set up a reinforcement program for which they decide which appropriate behaviors will be reinforced in the group, reinforcements that may be used as rewards (within the assigned budget), and the reinforcement schedule.
Sessions 3-5. The objectives of these sessions were to teach the following basic skills and techniques: (a) relaxation training, (b) anger management, (c) conflict resolution, and (d) self-regulation and self-control. Activities included role-playing of specific situations presented in a series of vignettes and group discussion of situations from their own lives. All group members were encouraged to provide positive feedback to each other and the reinforcement program was continued in these sessions.
Sessions 6-8. The objectives of these sessions were to teach skills directed at (a) appropriately interpreting social cues, (b) making socially acceptable interpretations and attributions about a social event, (c) generating a variety of socially acceptable solutions to the problematic situations, (d) deciding which of these solutions to enact based on the possible consequences of each alternative, and (e) demonstrating the appropriate behavior in a series of social vignettes which they roleplay in front of the group. All group members were encouraged to provide positive feedback to each other and the program of reinforcements was continued in these sessions.
Sessions 9-12. The main objectives of these sessions was to further develop and reinforce all the learned skills and techniques through further role playing of social vignettes, group discussions and teaching of more advanced techniques directed at developing more selfcontrol and appropriate attributions.
Procedures Directed at Guaranteeing the Cultural Sensitivity in the Administration of the Treatment. The treatment was administered following the recommendations described by Dana (1998). First, the acculturation of all participants was established. All were Spanish speaking Puerto Ricans living in a rural area of Puerto Rico. Second, a service delivery style was established by which all participants were treated with high frequencies of affiliate behaviors, respect, and in a very personal manner. Third, the counselors were all fluent Spanish speakers and much older than the participants.
Results
Pre-Treatment-Post-Treatment Comparisons with all Participants
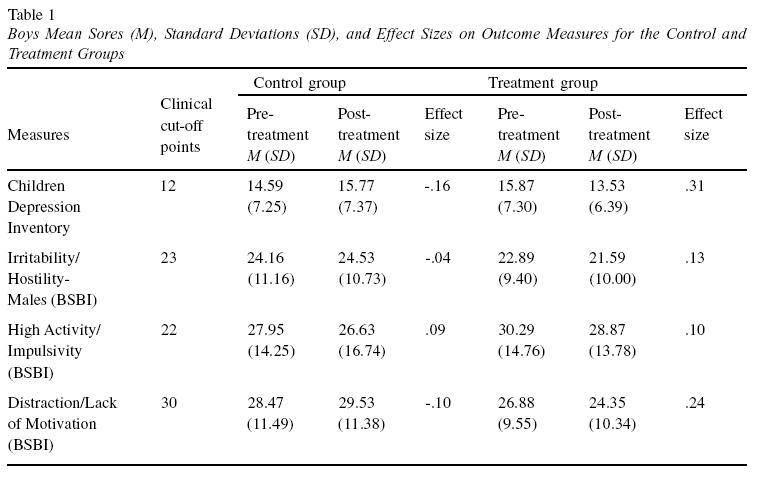
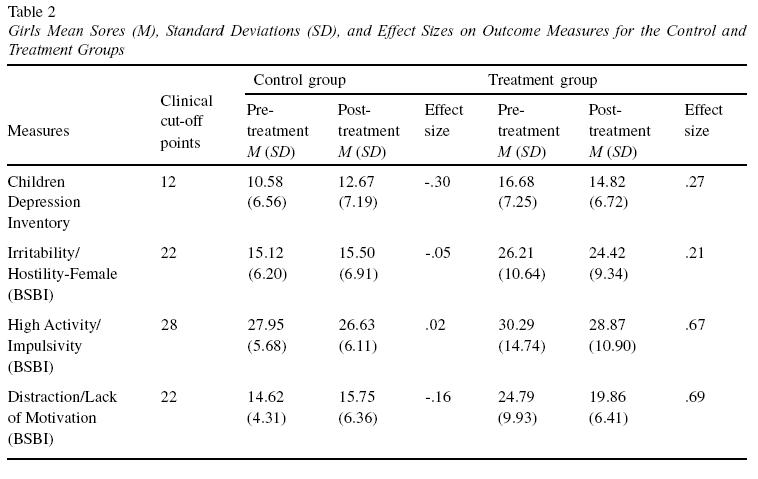
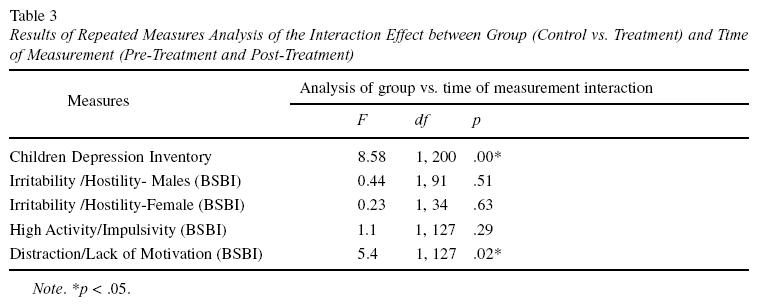
Repeated measures analyses of variance were performed with each measure, with type of group (control vs. treatment group) as the between subjects variable and the time of evaluation (pre- vs. post-treatment) as the within subjects variable. Gender was also enter as a between subject variable in the analyses of all measures except for the Irritability/Hostility subscale of the BSBI which was analyzed separately for males and females since they are gender specific. Effect sizes were calculated by subtracting the change score of the control group from the change score for the intervention group and dividing by the pooled standard deviation at baseline (Cohen, 1988). Effect sizes were calculated for two intervals, base line to post-treatment and baseline to follow-up. Results indicate that the Distractibility/Low Motivation subscale’s scores of the BSBI were significantly reduced in the treatment group at the posttreatment evaluation relative to the control group, F (1, 127) = 5.426, p = .021. In addition, results also show a significant reduction at the post-treatment evaluation from the pre-treatment levels in the CDI scores in the treatment group, but not in the control group, F (1, 200) = 8.576, p = .004. No gender by time of evaluation interaction effects was found to be significant. Tables 1, 2 and 3 present the results of these analyses.
Pre-Treatment-Follow-Up Comparisons
Repeated measures analyses were then performed to compare the pre-treatment and follow-up scores on the BSBI and the CDI subscales of the same set of the participants that completed the follow-up. Significant reductions were obtained for the Activity/ Impulsivity subscale (p<.001), the Distractibility/Low Motivation subscale (p<.001), and the CDI (p<.02) for both genders. In addition, significant reductions were found in the Irritability/Hostility subscale in males (p<.02), and females (p<.003) as shown in Table 4 and 5.
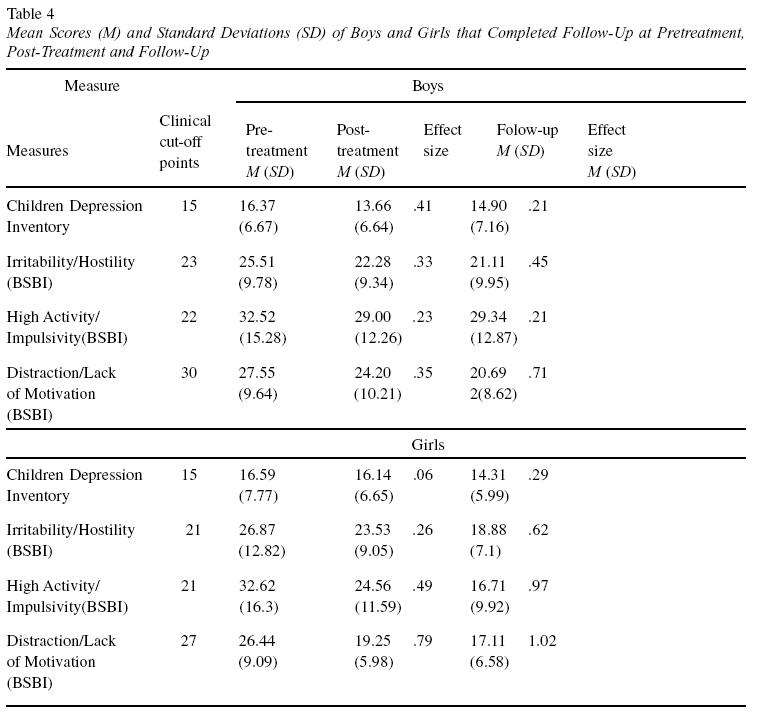
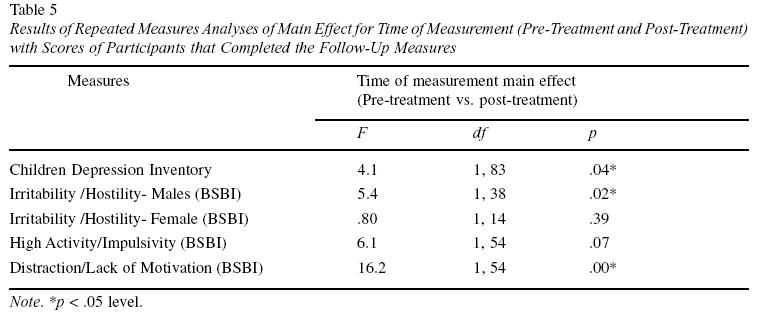
The reported effect sizes were moderate (<.40) for most initial comparisons. However, the results show that the effect sizes were higher when the pre-treatment and follow-up scores of the treatment group were compared as can be seen in Table 4. One can observe that at the follow-up measure, the effect sizes ranged from .21 to 1.02. In particular, the effect sizes obtained with the Distraction/Low Motivation, Activity Impulsivity and the medium subscales of the BSBI were 1.02, .97, and .62 respectively, which represents large effect sizes. Also, the results presented in Table 4 reveal that girls tended to exhibit larger effect sizes than boys on some measures.
Discussion
The goal of the present pilot study was to evaluate the transportability of a cognitive-behavioral intervention with Puerto Rican children in reducing disruptive behaviors and depressed mood. Results indicate that the cognitive-behavioral intervention was effective in reducing self-reports of depressed mood as measured in the CDI from pre-treatment to posttreatment. The results also showed significant reductions in the levels of distractibility and low motivation at posttreatment relative to the pre-treatment measures as reported by the teachers in the BSBI.
The results also showed that these differences were maintained and even enhanced in most cases in the 6 months follow-up. Both boys and girls in the treatment group showed significant reductions from the pretreatment to the follow up in their scores in all measures of disruptive disorders and depressed mood. Effect sizes at follow-up ranged form medium to large in size, indicating that, as a rule, children assigned to treatment are much better off than at pre-treatment. It is important to note that seldom these effect sizes are reported in this type of research (Siddle, Jones & Awenat, 2003).
Even more, the results show that the reduction in disruptive disorders and depressed mood were not only statistically significant, but also clinically significant. Moreover, in Table 1, if the means scores of both boys and girls of the control and treatment groups at pretreatment are observed more closely, one can see that most of these mean scores were above the clinical cutoffs for each scale. Furthermore, as one can see in Table 4, the mean scores in most scales of the treatment group are below the clinical cutoff points at the follow-up evaluation.
These results are consistent with research with Anglo-Americans boys with similar symptomatology who were also intervened with a social-cognitive model (Lochman & Wells, 2003). Outcome studies have evaluated the effects of interventions and found it more effective in reducing disruptive and aggression behavior in the classroom than either a no-treatment or a goal setting alone comparison condition.
This study provides evidence that a manualized treatment can be successful implemented and transported to Puerto Rican children with high levels of co-morbidity, and applied in day-to-day clinical practice. Thus, the present study contributes preliminary evidence of the impact of a socialcognitive intervention in a non-research and naturalistic setting (for a recent review see Roth & Fonagy, 2005).
Although we intended to assess the effectiveness of the intervention in reducing depressed mood we did not screened participants for depression due to the fact that we conceptualized depressed mood as a secondary symptom or byproduct of disruptive disorders. As discussed in the literature review above, several researchers have pointed out to the high co-morbidity between disruptive disorders and depressed mood (Biederman et al., 1996; Treuting & Hinshaw, 2001). If we had screened for depression, we could have easily ended up with a much more heterogeneous group of children where in some disruptive disorders was the primary disorders while in others depression might have been the primary while disruptive disorders the secondary disorder.
The present study has several limitations. First, the attrition rate at the 6 months follow-up was very high (46%), which limits the generalizability of these findings. The high attrition rate was the results in large part to the difficulty following-up children of low-income families in Puerto Rico since the school system does not provide any form of tracking them when they move from an elementary school to another intermediate school. However, although the groups might still differ in unknown factors affecting outcomes, participants lost to follow-up did not differ significantly in baseline measures from those assessed at 6 months, suggesting that those that remained were comparable in symptom severity at the outset of the study to those who dropped out. In fact, when we compare the change in pre intervention and one-week post intervention scores for those that remained and those lost to follow up we do not find significant differences by retention status.
Finally, the wait-list group was significantly smaller that the treatment group and there were no waitlist participants in the follow-up. This was due to the problems that we faced getting the parents to consent to participate in the wait-list group. Only the parents of the 57 children in the wait-list group consented to participate in the pre-treatment and post-treatment phases for a rate of engagement of 33%, which is lower than the rate of involvement of 42% reported by Coatsworth, Santisteban, McBride and Szapocznik (2001) for similar control conditions. As discussed above, 34 completed the post-treatment evaluation for an attrition rate of 46%, which is close to the 40% attrition rate reported by Santisteban et al. (1996). Possible cultural biases against research as suggested by different authors might have contributed to the low participation in this group (Marlow, 2004; Muir, Schwartz & Szapocznik, 2004; Santisteban et al., 1996). Marlow suggests that cultural responsiveness is central to clinical research assessing the effectiveness of any intervention. She argues that one aspect of cultural responsiveness is the extent to which research methods themselves are culturally responsive.
Thus, one possible recommendation for future clinical research, which evaluates the transportability of an intervention to another culture, is to develop specific strategies to engage Puerto Ricans in order for them to participate in the phases of research with little immediate benefits like wait-list groups that required repeated evaluations over an extended period before getting any intervention. These strategies could include providing monetary incentives. Another strategy is to train the research assistants on specific ways of engaging the parents in a culturally sensitive manner like appealing to “familism” which Muir et al. (2004) have found to be essential in engaging Latinos in general including Puerto Ricans in research. Nevertheless, engagement of Latinos including Puerto Ricans in research appears to be a significant challenge and future research needs to address this area by itself in a systematic and comprehensive manner.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: Author. [ Links ]
Bauermeister, J. (1994). Desarrollo y utilización del Inventario de Comportamiento Escuela (IDC-E) en la evaluación de niños puertorriqueños [Development and use of the Bauermeister School Behavior Inventory (BSBI) in assessing Latino children]. San Juan, PR: Author. [ Links ]
Bauermeister, J., Matos, M., Reina, G., Salas, C., Martínez, J., Cumba, E., & Barkley, R. (2005). Comparison of the DSM-IV combined and inattentive types of ADHD in a school-based simple of Latino/ Hispanic children. Journal of Child Psychology and Psychiatry, 46(2) 166-179. [ Links ]
Bernal, G., Rosselló, J., & Martínez, A. (1997). El Inventario de Depresión para niños y niñas: propiedades psicométricas en dos muestras puertorriqueñas [The Child Depression Inventory: Psychometric properties using two Latino samples]. Revista Psicológica Contemporánea, 4, 12-23. [ Links ]
Bernal, G., & Scharron-Del-Río, M. (2001). Are empirically supported treatments valid for ethnic minorities? Toward an alternative approach for treatment research. Cultural Diversity and Ethnic Minority Psychology, 7, 328-342. [ Links ]
Biederman, J., Faraone, S., Mick, E., & Moore, P. (1996). Child Behavior Checklist findings support comorbidity between ADHD and Major Depression in a referred sample. Journal of the American Academy of Child & Adolescent Psychiatry, 35(6), 734-742. [ Links ]
Brestan E., & Eyberg, S. (1998). Effective psychosocial treatments of conduct-disordered children and adolescents: Twenty nine years, 82 studies & 5, 272 kids. Journal of Clinical Child Psychology, 27(2), 180-189. [ Links ]
Coatsworth, J. D., Santisteban, D., McBride, C., & Szapocznik, J. (2001). Brief strategic family therapy versus community control: Engagement, retention, and an exploration of the moderating role of adolescent symptom severity. Family Process, 40(3), 313-332. [ Links ]
Cabanyes, J., García de León, M., Ávila, C., & Polaina-Lorente, A. (1994). Hiperactividad infantil y depresión: evaluación mediante cartografía cerebral [Brain cartography: Assessment of child’s hypercativity and depression]. Revista de Psiquiatría Infanto-Juvenil, 1, 16-21.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum. [ Links ]
Dana, R. (1998). Understanding cultural identity in therapy and assessment. Thousand Oaks, CA: Sage. [ Links ]
Kazdin, A. E. (2003). Problem-solving skills training and parent management training for conduct disorder. In A. E. Kazdin & J. R. Weisz (Eds.), Evidence-based psychotherapies for children and adolescents (pp. 241-26). New York: Guilford Press. [ Links ]
Kovacs, M. (1985). The Children’s Depression Inventory (CDI). Psychopharmacology Bulletin, 21, 995-998.
Lochman, J., & Wells, K. (2003). Effectiveness of the Coping Power Program and of classroom Intervention with aggressive children: Outcomes at a 1-year follow-up. Behavior Therapy, 34, 493-515. [ Links ]
Marlow, C. (2004). The evidence-based practitioner: Assessing the cultural responsiveness of research. In H. E. Briggs & T. L. Rzepnicki (Eds.), Using evidence in social work practice (pp. 257-272). Chicago, IL: Lyceum Books. [ Links ]
Miranda, A., & Presentación, M. J. (2000). Efficacy of cognitive-behavioral therapy in the treatment of children with ADHD, with and without aggressiveness. Psychology in the Schools, 37(2), 169-182. [ Links ]
Mirón, L., Serrano, G., Godás, A., & Rodríguez, D. (1997). Conducta antisocial y consumo de drogas en adolescentes españoles [Antisocial behavior and drug use in Spanish adolescents]. Análisis y Modificación de Conducta, 23(88), 255-283. [ Links ]
Muir, J. A., Schwartz, S. J., & Szapocznik, J. (2004). A program of research with Hispanic and African American families: Three decades of intervention development and testing influenced by the changing cultural context of Miami. Journal of Marital & Family Therapy, 30(3), 285-303. [ Links ]
Pliszka, S., Carlson, C., & Swanson, J. (1999). ADHD with comorbid disorders: Clinical assessment and management. New York: Guilford Press. [ Links ]
Reid, J., Webster-Stratton, C., & Hammond, M. (2003). Follow-up of children who received the incredible years intervention for Oppositional- Defiant Disorder: Maintenance and prediction of 2-year outcome. Behavior Therapy, 34(4), 471-491. [ Links ]
Roth, D., & Fonagy, P. (2005). What works for whom? New York: Guilford Press. [ Links ]
Santisteban, D., Szapocznik, J., Pérez-Vidal, A., Kurtines, W. M., Murray, E. J., & LaPerriere, A. (1996). Efficacy of intervention for engaging youth and families into treatment and some variables that may contribute to differential effectiveness. Journal of Family Psychology, 10(1), 35-44. [ Links ]
Siddle, R., Jones, F., & Awenat, F. (2003). Group cognitive behavior therapy for anger: A pilot study. Behavioral and Cognitive Psychotherapy, 31, 69-83. [ Links ]
Treuting, J., & Hinshaw, S. (2001). Depression and self-esteem in boys with Attention Deficit/ Hyperactive disorder: Associations with comorbid aggression and explanatory attributional mechanism. Journal of Abnormal Child Psychology, 29(1), 23-39. [ Links ]
Velázquez, H., Juárez, M., Caso-López, A., & Cabrera, F. (2000). Resultados preliminares del proyecto estudio longitudinal del desarrollo de la conducta agresiva en niños y su relación con el establecimiento de conducta antisocial en la adolescencia [Inicial results of a longitudinal study on the development of aggressive behavior in children and its relation with antisocial behavior in adolescents]. Revista Mexicana de Análisis de la Conducta, 26(1), 65-89. [ Links ]
Received 25/07/2007
Accepted 17/11/2007
José J. Cabiya. Professor, Carlos Albizu University, San Juan Campus, Puerto Rico.
Lymaries Padilla-Cotto. Professor, Carlos Albizu University, San Juan Campus, Puerto Rico.
Karelyn González. Professor, Carlos Albizu University, San Juan Campus, Puerto Rico.
Jovette Sanchez-Cestero. Professor, Carlos Albizu University, San Juan Campus, Puerto Rico.
Alfonso Martínez-Taboas. Professor, Carlos Albizu University, San Juan Campus, Puerto Rico.
Sean Sayers. Professor, Carlos Albizu University, San Juan Campus, Puerto Rico.
1 Dirección: PO Box 9023711, San Juan, Puerto Rico, 00902-3711.
Email: jcabiya@sju.albizu.edu













