Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Journal of Human Growth and Development
versão impressa ISSN 0104-1282
Rev. bras. crescimento desenvolv. hum. vol.23 no.1 São Paulo 2013
ORIGINAL RESEARCH
The impact of birthweight on adult minor illness: a study on a sub-clinical population
Denise A. Bellingham-YoungI; Elvidina N. Adamson-MacedoII
ICPsychol, FRSPH, FHEA. Lecturer in Public Health School of Health and Wellbeing University of Wolverhampton MH 218 Mary Seacole Building City Campus - North
IIEmeritus Professor of Maternal-Infant Mental Health University of Wolverhampton School of Health and Wellbeing Wolverhampton, UK
ABSTRACT
Official classification for low birth weight is 2500 gram or below. Whilst there is no consensus of what constitutes normal birth weight, it has been suggested that the optimal birthweight for long term health is 3500 - 4500 gram; hence those with birth weight between 2500 and 3490 gram could be deemed to be a sub clinical population. The objective was to investigate the relationship between disease and birthweight and to compare vulnerability of those with suboptimal and optimal birthweight in adulthood. This is a cohort study; with cross sectional retrospective design involving 258 adults aged 18-62 who knew their birth weight. Participants completed a minor illness checklist, using a median split, participants were categorised as high or low minor illness group. Results indicate a negative correlation between birthweight and minor illness score (r = -.155, p = .013). Those born with sub optimal birthweight are more likely to report minor illness symptoms above the media score of 16 (OR 1.70 CI 95% 1.04-2.79).It is concluded that there is a relationship between birthweight and level of minor illness in adulthood. Those born with birthweight 2500 - 3490 gram appear to be more vulnerable to minor illness. Thus, working with Foetal Origins theory, it may be possible that this group experienced a degree of foetal compensation, the consequence being that the immune system is compromised. Application of a three dimensional equilibrium model is suggested in designing interventions that improve foetal environment and subsequent health chances.
Key words: birthweight; minor illness; developmental origin of disease; equilibrium model.
INTRODUCTION
Risk of infection with communicable disease continues to be a public health issue in both the developed and developing world. Whilst risk of mortality from communicable disease may be greater in the developing world, morbidity and impact on wellbeing is universal.
There is a great deal of concern over the levels of minor illness. Under the umbrella classification of "minor illnesses", colds, flu, stomach upset and headache were identified as the highest cause of short term absence for both manual and non-manual workers1. According to Yardley2 over half the population in the United Kingdom consult their doctor each year for a minor symptom, with respiratory symptoms such as cough and sore throat being the most common reason for consultation. In addition to the cost to industry, minor illnesses contribute to huge levels of low grade morbidity and lack of wellbeing in populations.
Many minor illnesses go unreported, and traditional surveillance and sentinel methods underestimate the incidence and prevalence of such illnesses. During the 2009 A/H1N1flu pandemic, telephone interviews in ten states of America indicated that 13.5% of under 18s and 4.7% over 18's had flu like symptoms3. Based on a microneutralisation assay, McLeish et al.,4 estimate that 44% of the adult population of Scotland were sero-positive for A/H1N1 influenza by 1 March 2010 with the majority of these being a result of natural infections as opposed to vaccine. Further, Baguelin et al.,5 report that during this same period, 52% of 5 - 14 year olds in England had confirmed infections, which was up to 40 times higher than estimated from clinical surveillance.
A number of underlying causes of interest to public health practitioners explain the incidence and prevalence of minor and major infections.
Many studies investigating foetal origins theory exclude low and premature births and focus on those who were normal birthweight. Currently however there is no consensus on what normal birthweight is. Many studies investigating normal birthweight utilise the official classification of 2500 gram and above as normal, others analyse birthweight in 500 gram clusters. However, Spencer6 argues that the optimal birthweight for infant and adult long term health is 3500 - 4500 gram. There is therefore a portion of the population with neither clinically low nor optimally normal birthweight; a sub-clinical population about which very little is known.
As far as we are aware this population has not been hitherto specifically investigated in terms of determining their health risk compared to the optimal birthweight population, and not when the focus of that investigation was minor illness. Therefore, the objective of this study was to investigate the relationship between disease and birthweight and to compare vulnerability to disease between those with suboptimal and optimal birthweight in adulthood.
METHODS
This is a cohort study, with cross sectional retrospective design. A questionnaire was distributed to participants with the instruction that all questions referred to the previous month.
Measures
The Minor Illness Checklist7 measures symptoms from a range of common minor illnesses such as cold, cough, sore throat and upset stomach, was completed. Birthweight was self-reported and if stated in pounds and ounces was converted to grams. Self-reported birthweight is considered to be reliable and has been discussed elsewhere8.
Participants
Undergraduate and post graduate students, student midwives and members of the public were invited to take part in the study. Participants were recruited on the basis that they knew their birthweight and if they were full term or preterm. There were 258 full term participants, 219 female, 39 male. Age ranged18 to 62, birthweight ranged from 2540 to 4490 gram. Minor illness scores ranged from 0 to 49. Table 1 shows the mean and standard deviation for these.
Females and males had similar mean age and birthweight, whilst males had lower illness scores than females.
Data Analysis
The purpose of this study was twofold, first to investigate the link between birthweight and minor illness thus Pearsons Correlations were calculated: secondly to ascertain whether those with sub-optimal birthweights were more susceptible to incidence of minor illness. Chi-Square was carried out using the cross tabs function in SPSS; logistic regression analysis investigated predictors of levels of minor illness.
Participants were allocated to the sub-optimal birthweight group (2540 gram - 3490 gram) or the optimal birthweight group (3500 gram - 4500 gram). Between group t test was carried out to test differences between the mean illness score. Following previous studies9,10 scores above or below the median minor illness score of 16 were used to allocate participants to high and low minor illness group.
It is expected that a relationship will be seen between birthweight and minor illness. It is also expected that those with sub-optimal birthweight will be more likely to experience more minor illness than their optimal birthweight counterparts.
RESULTS
Scores in the minor illness scale ranged 0 - 49, mean18.269, median 16. Using a median split, 128 participants were allocated to the low minor illness group, 130 were allocated to the high minor illness group. There were 122 participants in the optimal birthweight group (3500 - 4500 gram) and 136 in the sub optimal birthweight group (2540 - 3490 gram).
Minor illness scores were significantly lower (t 2.39, p 0.018) for those in the optimal birthweight group (mean 16.40 std 10.62) than those in sub optimal group (mean 19.86, std 12.41). A significant negative correlation was observed between birthweight and minor illness score (r = -.55, p = .013); those with a lower birthweight were more likely to suffer more minor illness.
Frequency of membership to low or high minor illness group can be seen in figure 1 below. Chi-square indicates that those in the sub-optimal birthweight group are more likely to be in the high illness group whereas those in the optimal birthweight group are more likely to be in the low illness group (X2 = 4.46, df 1, p = .035).
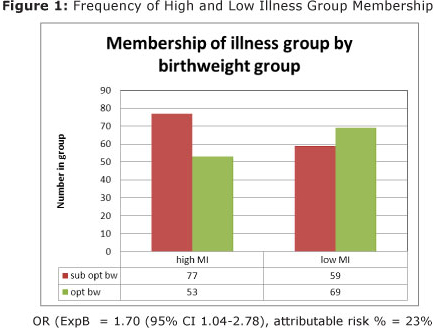
Logistic regression indicates that birthweight group will predict membership of minor illness group (X2 4.478, p = 0.034). Those in the sub-optimal birthweight group are 1.70 times more likely to suffer minor illnesses above the median (ExpB 1.70 CI 95% 1.04 - 2.78) than those in the optimal birthweight group. Attributable risk suggests that 23% of minor illnesses in adulthood can be attributed to being born in the sub-optimal group.
DISCUSSION
Results presented here reflect those of earlier studies with fewer participants11,12. There is a negative linear relationship between birthweight and levels of minor illness. Participants with lower birthweight report more minor illness. Additionally, those in the sub optimal birthweight group had a higher mean minor illness score and were more frequently in the group whose illness scores were above the median.
Birthweight predicts membership of the high or low minor illness group, with those with suboptimal birthweight between 2500 and 3490 gram being 1.70 times more likely to report minor illness symptoms above the median. Furthermore, twenty three per cent of minor illness can be attributable to being born with sub optimal birthweight.
These results provide further evidence of the link between birthweight and vulnerability to minor infectious disease. Indications are that there is a greater vulnerability to minor illness and morbidity in those with suboptimal 2500 -3490 gram birthweight compared to those with optimal birthweight 3500 - 4500 gram.
Theoretical explanation for these results can be found in a growing body of literature which suggests that the long term health chances of an individual are associated with size and shape at birth. For example, in a systematic review and meta-analysis, Risnes et al.,13 reports that lower birthweight has been associated with mortality from all causes. The association between lower birthweight and major non-communicable diseases has been known for some time with the association between birthweight and cardiovascular disease14,15, stroke16, and type II diabetes17,18 being well established.
Foetal origins of disease theory19 suggests that in a suboptimal foetal environment where oxygen and/or nutrient supply is restricted, the foetus will compensate by diverting nutrients in an effort to protect brain development, thereby programming functioning of cardiovascular, endocrine systems and metabolism. The result of such foetal compensation can be a vulnerability to disease in a range of physiological systems20,21. It is now emerging that foetal compensation also impairs immune function22 resulting in increased risk of communicable disease. Indications are that poor foetal nutrition is associated with impaired development of the immune system23 and decreased cell mediated immunity24.
Evidence indicates that lower birthweight has been associated with increased number of hospital admissions for infectious diseases in children25. These authors reported the results of a large Danish study following children from birth to 14 years. Across a range of birthweight from 1500gram to 5000 gram and above risk of hospitalisation for infectious disease increased 9% for each 500 gram reduction in birth weight. Results were consistent when low birthweight (< 2500 gram) participants were excluded from analysis and confounders such as mode of delivery and maternal smoking were controlled.
In a study conducted in Pakistan, a reduced antibody response to typhoid vaccination in participants with lower birthweight was reported26. The study population consisted of 257 adults with 86% being born 2500 gram or above. A significant negative association was reported between birthweight and antibody response to typhoid vaccine possibly rendering the vaccination less effective. Again these results remained when confounding factors were controlled for.
It has been postulated that poor foetal nutrition is a causal factor in lower birthweight and the resultant impaired immunity. Young men born in the hungry season in Gambia are more likely to suffer nutritionally mediated intrauterine growth retardation and to die from infectious conditions than those born in the harvest season23. Further work by these authors presents evidence of nutritionally mediated reduction in immune function27.
Incidence of TB is reported in a Swedish study involving twins to be related to lower birthweight. Tuberculosis risk was 11% lower for every 500 g of additional birthweight28. These authors also suggested that foetal growth may play a causal role in susceptibility to tuberculosis, possibly through early programming of immunity.
It can therefore be seen that evidence exists in literature of the association between birthweight and major infectious disease in both adults and children. Presented here is evidence of an association between birthweight and minor illness, indicating that those with lower birthweight have increased vulnerability to both major and minor infectious diseases.
Underlying causes of lower birthweight and foetal under nutrition are numerous with geographical variations. Issues such as maternal health, exposure to social, biological and psychological hazards can interact to impact the developing foetus and influence birth outcomes6. Following a number of rigorous experiments and empirical exploration, Gottlieb proposed the theory of probabilistic epigenesis29,30 and the concept of horizontal and vertical coactions to explain the impact of internal and external influences on biological development. Horizontal coactions refer to interactions within systems for example within biological systems cell to cell. Vertical coactions refer to interactions between systems for example between environmental, social or psychological systems and biological systems.
Gottlieb's theories provide a framework to explain the mechanisms of foetal compensation suggested by Barker. Thus a series of horizontal and vertical coactions provide explanation for the impact of exposures such as nutritional deprivation, environmental pollution or psychological stress. These maternal exposures impact the quality of the foetal environment which in turn has implications for the developing foetus.
Protecting the foetal environment is becoming a public health priority. Recent reports 31, 32 note the importance of promoting the health of girls and women of child bearing age in order to reduce adverse birth outcomes and infant mortality and improve infant and adult health. In line with previous studies cited earlier, it is possible to suggest that those in the suboptimal birthweight group developed in a suboptimal foetal environment and experienced a degree of foetal compensation, the consequence of which is compromised immune function.
Foetal origins of disease19 and Gottlieb's23,24 framework of horizontal and vertical coactions can be applied to provide further explanation for the results and recommendations for future research and practice. As nothing is known about the circumstance of our participant's mothers, it is difficult to fully explain the coactions that may have occurred. It is however possible to extrapolate from other studies23,27 and suggest a series of horizontal and vertical coactions that may have occurred.
It is hypothesised that negative maternal exposures such as nutritional deprivation, behaviour, social deprivation or physical illness resulted in a suboptimal foetal environment and subsequent foetal nutritional disruption. These negative external exposures trigger foetal compensation as evidenced by lower birthweight with the consequence of impaired immunity and greater susceptibility to acquiring minor illness when exposed to infectious agents. The vertical coactions occurring here are between systems; for example external exposures to internal foetal environment to biological development of foetus. Horizontal coactions are those which occur within systems such as the biological development of foetus. An example of a horizontal coaction is foetal compensation which occurs when nutrients are diverted from one physiological function such as cardiovascular and immune function to protect development of other physiological function such as the brain. As Nathanielsz21 argues even minor nutritional disruptions can lead to foetal compensations evidenced by minor reductions in birthweight that have long term health consequences.
Many public health policies and interventions focus upon combating major health issues. However, whilst not as serious as major communicable and non-communicable diseases, minor illnesses are common to the human condition2-5. They add to the burden of morbidity and for those who are economically active minor illness reduces their effectiveness or removes them temporarily from the workforce1. Thus the impact of minor illness goes beyond individual health, wellbeing and financial stability, but also impacts negatively on industry and commerce. We therefore argue that minor illness is an important public health issue and worthy of investigation.
In this article we make suggestions for simple policy and practice changes for the monitoring and support of individuals in this hitherto unrecognised risk group. Additionally, given evidence that the underlying causes of minor illness is in foetal life, we suggest a research and practice model to identify distal interventions that improve health prior to and during pregnancy thus protecting the foetal environment.
The importance of prioritising the health of women of childbearing age, expectant mothers and young children is already known31, 32. However, based on results reported here, it is suggested public health policy also gives particular attention to the health prospects of those born in the suboptimal birthweight group regardless of their sex or age. Currently however, this group is not easily identified. In the UK for example birth details such as weight, size, and gestational age are held with mother's medical records only
The report "Born Too Soon"31 called for improved monitoring of premature delivery. This will give a more accurate view of the incidence of premature delivery, but could also serve a longer term purpose. We suggest that birth details such as weight, size and gestation age, are routinely kept not just with mothers medical record, but also transferred to the infants own medical record as top level identifiers. Thus individuals at increased risk can be more readily identified allowing targeted interventions. For example, currently 'flu vaccine is available on request free of charge to NHS patients in UK. However it is only elderly or those with pre-existing conditions which increases risk of 'flu or complications from 'flu that are routinely called for vaccination. An ability to easily identify those born with sub optimal birthweight who may be at increased risk of 'flu, would facilitate the inclusion of this group in routine invitation for vaccination.
Further as those with lower birthweight have been shown to be less responsive to immunisation 26, a process of follow up for those with sub optimal birthweight to monitor antibody levels following immunisation could be beneficial. This may be particularly pertinent for specific programmes such as BCG vaccination for TB as well as general childhood and adult immunisation programmes. Research investigating links between birthweight and specific vaccination programmes along with the efficacy of such follow up is suggested.
In addition to the proximate interventions protecting the health of individual with suboptimal birthweight who may be at increased risk of disease, we suggest that distal interventions are essential in tackling the underlying causes. March of Dimes et al31 calls for a global strategy to combat premature delivery; the outcome of these strategies will naturally result in a reduction of low birthweight, sub optimal birthweight and small for gestation age. However given global variation of underlying causes, exposures to risk, availability of resources and community facilities, any strategy requires local context. We suggest that the application of an Equilibrium Model12 may assist public health practitioners in identifying and prioritising local implementation of global strategy.
Bellingham-Young and Adamson-Macedo12 suggested an equilibrium model based on Gottlieb's concept of horizontal and vertical coactions. This multi-dimensional model was originally developed to explain and depict incidence of and differences in minor illness levels and associations with birthweight and psychological states (for discussion of the model see previous work cited by these authors12). One axis represents the outcome (in this case minor illness); the other two represent a variable or cluster of variables that has influence upon the outcome. Equilibrium is a state of perfect health and wellbeing. Changes on one dimension will coact to trigger a change in the other dimension bringing an individual closer to or further from equilibrium with the resultant decrease or increase in the outcome.
The position of the co-ordinates along the axis determines the shape and size of the parallelepiped, thus providing a pictorial representation of the impact of each variable. Conceptually, movement on one axis coacts to trigger change on the other two axes. In the application of the model seen in figure 2, the dotted line MI1 represents an individual with total illness score of 42(Y axis) and below optimal birthweight of 2720 gram (Z axis). The solid line MI2 represents an individual with minor illness score of 9 and optimal birthweight of 3630 gram. The X axis in the original model is a psychological construct beyond the scope of this article, however we are suggesting that this axis could represent environmental or personal variables that impact birthweight. Importantly it is the combined effect of the coactions that brings the individual closer to or further from equilibrium as demonstrated by the flatter shape of the parallelepiped MI2.
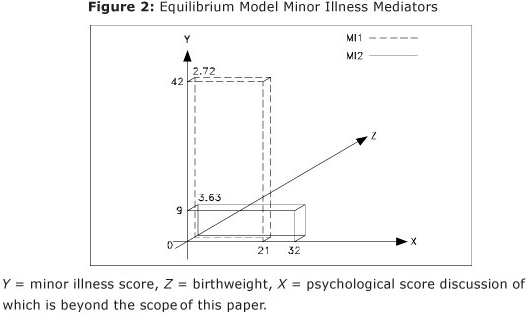
The Equilibrium Model provides a framework for identifying and quantifying multiple positive and negative exposures that impact upon an outcome, for example the desirable goal of optimal birthweight. Once a baseline model is established public health practitioners can hypothetically manipulate values on the axes to predict the impact of change in a given dimension thereby predicting the impact of bespoke interventions. It is thus cautiously suggested that there is potential to develop the model as a diagnostic and predictive tool providing public health practitioners insight into where to focus interventions and what their impact may be. Research investigating the combinations of variable clusters and application of these to the equilibrium model is suggested in order to facilitate prioritisation and design multi-disciplinary local interventions informed by global strategy.
One of the limitations of this study is that birthweight and term was self-reported, however self-reported birthweight is considered reliable 30. All participants reported that they were full term, however as gestational age is not known, it is not possible to identify those small for gestational age. A further limitation is that environmental exposures of participants mothers during pregnancy whether positive or negative are unknown. Access to birthweight and gestational age from official record would strengthen the generalizability of findings from future research.
This study has provided further evidence of the link between an individual's birthweight and vulnerability to disease in adulthood with a particular focus upon minor illness. The risk of minor illness is greater in adults born with sub optimal birthweight compared to those born with optimal birthweight. Suggestions for minor changes in policy to support this hitherto unrecognised risk group are made. Interventions that address underlying causes of sub optimal foetal environment should have a positive impact upon birth outcomes and subsequent health and life chances of future generations. Therefore, application of the Equilibrium Model is suggested to facilitate distal interventions that address underlying causes of suboptimal birthweight.
REFERENCES
1. Paton N. CIPD absence survey 2009. Occup Health 2009;61(9):8. [ Links ]
2. Yardley L, Joseph J, Michie S, Weal M, Wills G, Little P. Evaluation of a web-based intervention providing tailored advice for self-management of minor respiratory symptoms: Exploratory randomized controlled trial. Journal of Medical Internet Research 2010;12(4):e66. [ Links ]
3. Reed C, Angulo FJ, Biggerstaff M, Swerdlow D, Finelli L. Influenza-like illness in the community during the emergence of 2009 pandemic influenza A(H1N1) - survey of 10 states, April 2009. Clinical Infectious Diseases 2011 January 01;52(suppl 1):S90-3. [ Links ]
4. McLeish NJ, Simmonds P, Robertson C, Handel I, McGilchrist M, Singh BK, et al. Sero-prevalence and incidence of A/H1N1 2009 influenza infection in Scotland in winter 2009 - 2010. PLoS ONE 6(6): E20358. Doi:10.1371/journal.Pone.0020358 2011. [ Links ]
5. Baguelin M, Hoschler K, Stanford E, Waight P, Hardelid P, Andrews N, et al. Age-specific incidence of A/H1N1 2009 influenza infection in England from sequential antibody prevalence data using likelihood-based estimation. PLoS ONE 6(2): E17074. Doi:10.1371/journal.Pone.0017074 2011. [ Links ]
6. Spencer N. Weighing the evidence, how is birthweight determined. Radcliffe Medical Press; 2003. [ Links ] .
7. Bellingham-Young DA, Adamson-Macedo EN. Birthweight - is it linked to minor illness in adulthood? Neuroendocrinology Letters 2000;21:469-74. [ Links ]
8. Sandhu MS, Luben R, Day NE, Khaw KT. Self-reported birth weight and subsequent risk of colorectal cancer. Cancer Epidemiology Biomarkers & Prevention 2002 Sep; 11(9): 935-8. [ Links ]
9. Evans PD, Doyle A, Hucklbridge F, Clow A. Positive but not negative life-events predict vulnerability to upper respiratory illness. British Journal of Health Psychology 1996; 1(4): 339-48. [ Links ]
10. Steptoe A, Lipsey Z, Wardle J. Stress, hassles and variations in alcohol consumption, food choice and physical exercise: A diary study. British Journal of Health Psychology 1998; 3(1): 51-63. [ Links ]
11. Bellingham-Young DA, Adamson-Macedo EN. Prematurity and adult minor illness. Neuroendocrinology Letters 2004; 25 Suppl 1: 117-25. [ Links ]
12. Bellingham-Young DA, Adamson-Macedo EN. Early prediction and psycho-immunologic mediation of minor illness in adulthood. Neuroendocrinology Letters 2002 Jun; 23(3): 219-25. [ Links ]
13. Risnes KR, Vatten LJ, Baker JL, Jameson K, Sovio U, Kajantie E, et al. Birthweight and mortality in adulthood: A systematic review and meta-analysis. International Journal of Epidemiology 2011 June 1, 2011; 40(3): 647-61. [ Links ]
14. Barker DJP. Fetal origins of cardiovascular and lung disease. USA: Marcel Dekker; 2001. [ Links ] .
15. Rich-Edwards J,W., Kleinman K, Michels K,B., Stampfer M,J., Manson J,E., Rexrode K,M.,et al. Longitudinal study of birth weight and adult body mass index in predicting risk of coronary heart disease and stroke in women. BMJ 2005 2005-05-12 00:00:00; 330(7500): 1115. [ Links ]
16. Osmond C, Kajantie E, Forsen TJ, Eriksson JG, Barker DJP. Infant growth and stroke in adult life: The Helsinki birth cohort study. Stroke 2007 February 1, 2007; 38(2): 264-70. [ Links ]
17. Whincup PH, Kaye SJ, Owen CG, Huxley R, Cook DG, Anazawa S, et al. Birth weight and risk of type 2 diabetes: A systematic review. JAMA 2008 December 24, 2008;300(24):2886-97. [ Links ]
18. Barker DJP. Type 2 diabetes: The thrifty phenotype. England: Oxford University Press; 2001. [ Links ]
19. Barker DJP. The origins of the developmental origins theory. Journal of Internal Medicine 2007;261(5):412-7. [ Links ]
20. Gupta D. Humors and hormones in pregnancy: Determinants of personality development in the child. International Journal of Prenatal and Perinatal Studies 1992;4(1/2):1-15. [ Links ]
21. Nathanielsz PW. Life in the womb, the origin of health and disease. Ithaca New York: Promethean Press; 1999. [ Links ] .
22. Heppolette CA, Palmer D, Ozanne SE. Experimental models of low birth weight - insight into the development programming of metabolic health, aging and immune function. In: A. Plagemann, editor. Perinatal programming. Berlin: Walter de Gruyter GmbH & Co; 2012. [ Links ] .
23. Moore SE, Cole TJ, Collinson AC, Poskitt EM, McGregor IA, Prentice AM. Prenatal or early postnatal events predict infectious deaths in young adulthood in rural africa. International Journal of Epidemiology 1999 December 1, 1999; 28(6): 1088-95. [ Links ]
24. Chandra RK. Nutrition and the immune system. Proceedings of the Nutrition Society 1993 Feb;52(1):77-84. [ Links ]
25. Hviid A, Melbye M. The impact of birth weight on infectious disease hospitalization in childhood. American Journal of Epidemiology 2007 April 1, 2007;165(7):756-61. [ Links ]
26. Moore SE, Jalil F, Ashraf R, Chen Szu S, Prentice AM, Hanson LÃ. Birth weight predicts response to vaccination in adults born in an urban slum in Lahore, Pakistan. The American Journal of Clinical Nutrition 2004 August 1, 2004; 80(2): 453-9. [ Links ]
27. Prentice AM, Moore SE. Early programming of adult diseases in resource poor countries. Archives of Disease in Childhood 2005 April 1, 2005; 90(4): 429-32. [ Links ]
28. Villamor E, Iliadou A, Cnattingius S. Evidence for an effect of fetal growth on the risk of tuberculosis. Journal of Infectious Diseases 2010 February 1, 2010; 201(3): 409-13. [ Links ]
29. Lickliter R, Logan C. Developmental psychobiology special issue: ''Gilbert Gottlieb's legacy: Probabilistic epigenesis and the development of individuals and species''. Developmental Psychobiology 2007; 49: 747-748. [ Links ]
30. Gottlieb G. Environmental and behavioural influences on gene activity. Current Directions in Psychological Science 2000;9:93-7. [ Links ]
31. March of Dimes , PMNCH , Save the Children , WHO . Born too soon: The global action report on preterm birth. eds CPHowson, MV kinney, JE lawn. Geneva: World Health Organization; 2012. [ Links ]
32. The Marmot Review. Fair society healthy lives: Strategic review of health inequalities in England post 2010. The Marmot Review; 2010. [ Links ]
 Correspondence to:
Correspondence to:
d.bellingham-young@wlv.ac.uk
Manuscript submitted Aug 01 2012
Accepted for publication Dec 28. 2012.
This article is based on work from PhD thesis "Birthweight and Minor Illness" awarded by University of Wolverhampton 2004.













