Serviços Personalizados
artigo
Indicadores
Compartilhar
Journal of Human Growth and Development
versão impressa ISSN 0104-1282
Rev. bras. crescimento desenvolv. hum. vol.21 no.3 São Paulo 2011
ORIGINAL RESEARCH
Lipid profile in overweight children and adolescents
Alessandra Teixeira RamosI; Danielle Franklin de CarvalhoI, II; Nathalia Costa GonzagaI; Anajás da Silva CardosoI; Juliana Andreia Fernandes NoronhaI; Maria Aparecida Alves CardosoI
INúcleo
de Estudos e Pesquisas Epidemiológicas (NEPE) – Universidade Estadual
da Paraíba (UEPB) - Endereço: Avenida das Baraúnas, 351
- Cidade Universitária - Prédio dos Mestrados - 2º andar
- Campina Grande-PB, CEP: 58429-500, Fone/Fax: (83) 3315-3300
IIUniversidade Federal de Pernambuco – Endereço: Av.
Prof. Moraes Rego, 1235 - Cidade Universitária, Recife - PE - CEP: 50670-901.
Fone PABX: (81) 2126.8000
ABSTRACT
OBJECTIVE:
to assess the lipid profile and associated factors in obese or overweight children
and adolescents.
METHODS: cross-sectional study developed from April to November 2009
including 217 overweight children and adolescents aged from two to 18 years
from the public health system of Campina Grande-PB. Nutritional status was classified
according to percentile as: overweight (85 < BMI < 95), obesity (95 <
BMI < 97) and severe obesity (BMI < 97). The following values were considered
abnormal: LDL-c < 130 mg/dL, HDL-c < 45 mg/dL and TG 130 mg/dL. Statistical
analysis included analysis of variance and chi-square tests adopting a confidence
interval of 95%. The SPSS 17.0 program was used.
RESULTS: most children and adolescents showed severe obesity (68.2%),
which was associated to sex (PR = 3.7) and to age group from two to nine years
(PR = 3.2). Dyslipidemia was observed in 85.3% of the study population, which
was prevalent (88.9%) in children from two to five years of age. Low HDL-c was
the most frequent alteration (80.6%), and the value was significantly lower
among those with severe obesity (p < 0.005).
CONCLUSIONS: The high prevalence of dyslipidemia observed since the preschool
age reinforces the need to control the lipid profile in the presence of obesity
or overweight, regardless of age.
Key words: obesity; overweight; dyslipidemias; cardiovascular disease.
INTRODUCTION
Atherosclerotic disease is currently a major cause of morbidity and mortality in Brazil and worldwide. It is multifactorial disorder that may have a silent begin in childhood, with progression during adolescence and adulthood1.
Recently, it has been recognized that changes in the serum lipid levels in childhood may be predictive of the occurrence of cardiovascular disease in adults. This is based on the tracking phenomenon, in which there is a strong tendency of children to maintain the same cholesterol percentiles until the adult life2. Moreover, the persistence of an unfavorable lipid profile increases the risk of coronary events, which explains the importance of adopting preventive measures early in childhood2,3.
The Pathobiological Determinants of Atherosclerosis in Youth (PDAY) and Bogalusa Heart Study emphasize the concept of atherosclerosis as a pediatric problem4, and according to the study of Stary5 on the presence of atherosclerotic lesions in the first four decades of life, injuries considered initial, types I and II (early lesions) can be found in indivi-duals with less than one year of age.
The increased overweight among children, in epidemic levels, appears to be responsible for negative changes in lipid profile, early indicated by the high levels of total cholesterol (TC), triglycerides (TG), low density cholesterol (LDL-c) and low levels of high density cholesterol (HDL-c)6.
There is evidence that the process of westernization of the lifestyle is associated with a growing trend in the prevalence of dyslipidemia. On the other hand, a decrease is observed in countries where prevention programs have already been implemented 2.
There are several studies on the prevalence of dyslipidemia in childhood; however, in Brazil, only two studies were focused on the population of overweight children and adolescents, one conducted in the state of Rio Grande do Norte 7 and the other in São Paulo8; in the latter, abnormal HDL values were observed in 68.75% of the participants, abnormal triglycerides in 35% and VLDL values in 37%. None of these studies included preschool children8.
In 2005, the Brazilian Society of Cardiology published the I Guidelines for the Prevention of Atherosclerosis in Children and Adolescents9, recommending changes in the desirable values of lipids, with reductions in the total cholesterol and LDL-C values and increase in the HDL-C values. So far, no research has been performed in this population using this new criterion.
Therefore, this study is aimed at contributing to this aspect and verifying the occurrence of changes in the lipid profile since preschool age, as well as associated factors in overweight children and adolescents. The identification of children with risk factors for atherosclerosis may allow early intervention, reducing the atherosclerotic process and thus preventing or delaying the occurrence of cardiovascular diseases.
METHODS
This was a cross-sectional study conducted from April to November 2009 as part of a larger project entitled "Prevalence of cardiometabolic risk factors among obese or overweight children and adolescents''.
Overweight children and adolescents aged 2 - 18 years users of the Unified Health System (SUS), in Campina Grande-PB, who had not undergone any treatment for weight reduction, were included in this study. The sampling was performed through the disclosure of the research in Basic Health Units, with support from the Municipal Department of Health. Individuals were referred by the health staff to the Centre for Childhood Obesity (CCO), created at the "Elpídeo de Almeida" Health Institute, in Campina Grande-PB, specifically designed to meet the demand of this study. The CCO is composed of researchers and multidisciplinary team composed of endocrinologist, nutritionist, psychologist, nurse, pharmacist, social worker and physical trainer.
At the first meeting, a screening was held to assess whether individuals met the inclusion criteria. Of 246 cases, those who, at the time of data collection, showed some condition that would harm the performance of physical activities, diabetes or other diseases, those making use of medications that interfere in the glucose or lipid metabolism were excluded. Twenty-seven losses were recorded for not attending the blood collection and two other were excluded for making use of corticosteroids, totaling 217 subjects.
Parents and / or guardians were informed about the objectives and procedures of the study, and if interested in participating, they signed the Free and Informed Consent Form (FICF). On this occasion, the first questionnaire was applied, which addressed socioeconomic, personal and family history issues; anthropometric measurements were assessed and laboratory tests were scheduled to determine the lipid profile, which were performed within 15 days after this interview.
Anthropometric data (weight and height) were collected in duplicate, so that the mean value of two measurements was considered. To obtain the weight, a platform-type digital scale was used (WelmyTM) with capacity of 200 kg and accuracy of 0.1 kg. Height was measured using a stadiometer (TonelliTM), with accuracy of 0.1 cm. During the measurement, the individuals were wearing light clothes, and followed the procedures recommended by the WHO10.
For the nutritional status classification, the body mass index (BMI) was calculated, and according to recommendation from the Centers for Disease Control and Prevention (CDC) (2002)11, and according to the percentiles, the following categories were found: overweight (85 > BMI < 95), obesity (95 > BMI < 97) and severe obesity (BMI > 97)10.
Total cholesterol, HDL-c and triglycerides were assessed using the enzymatic colorimetric method in automatic equipment (BioSystems Model 310), according to the LabtestTM kit manufacturer's recommendations. Blood collection was performed after a fasting period of 10 to 12 hours at the Laboratory of Clinical Analysis of the State University of Paraiba (LAC / UEPB). To calculate the LDL-c, the Friedewald formula was used: LDL-c = CT - HDL-c - TG/5, which is valid for TG values less than 400mg/dl.
Prevalence of dyslipidemia was presented in accordance with I Guidelines for the Prevention of Atherosclerosis in Children and Adolescents9, which establishes the following cutoffs for desirable values: TC <150 mg/dL, LDL-c <100 mg / dL, HDL-c e" 45 mg / dL and TG <100 mg/dL; for borderline values: TC 150-169 mg/dL, LDL-c 100-129 mg/dL and TG 100-129 mg/dL, and abnormal values: TC e" 170 mg/dL, LDL-c e" 130 mg/dL , TG e" 130 mg/dL and HDL-c < 45 mg/dL. Dyslipidemia cases were considered as those who had abnormal values of at least one of the following components: HDL-c, LDL-c and triglycerides, according to the IV Brazilian Guidelines on Dyslipidemia and Atherosclerosis Prevention12.
Statistical analysis was carried out using the SPSS software, version 17.0, with confidence interval of 95%. In the descriptive analysis, nutritional status and age groups described above were used. To conduct the hypotheses tests, they were regrouped for the application of the analysis of variance and chi-square test.
The study was approved by the Ethics Committee of the State University of Paraiba, process Nº 0040.0.133.000-08.
RESULTS
Of the 217 children and adolescents, 64.1% were female. The age distribution indicated that 12.4% had between two and five years, 26.3% between six and nine and 61.3% between 10 and 18 years of age. In relation to socioeconomic status, 19.9% had family income equal to at least one minimum wage; 38.9% had between one and two, and 41.2%, more than two. Regarding maternal education, 37.3% had only high school and 14.3% had higher education.
Most individuals (68.2%) had BMI > 97th percentile, characterizing as severe obesity, 18.9% were between 95th and 97th percentiles, and 12.9% were in the range of 85 > BMI < 95. Severe obesity was associated with males (RP = 3.7 - CI95% [1.7-6.7]) and to age group between two and nine years (RP = 3.2 - CI95% [1.7-6.1]).
Dyslipidemia was observed in 85.3% of the population: without association, 43.8% had only low HDL-c, 1.8% had high LDL-c and 0.5% abnormal TG. When examining the interactions between different lipids, it was found 24.9% of low HDL-c in association with increased triglycerides, 9.2% of associated alterations between HDL-c, TG and LDL-c, 4.6 % with two cholesterol fractions simultaneously abnormal and, finally, 0.5% of LDL-c and increased TG.
The lipid profile distribution is shown in figure 1. Low HDL-c was the most frequent alteration (80.6%), while prevalence of abnormal LDL-C was lower (14.7%). The mean values of lipids, except for LDL-c, are outside values recommended in the I Guideline for the Prevention of Atherosclerosis in childhood 9. It was also observed that the HDL-c value was significantly lower among severely obese patients (Table 1).
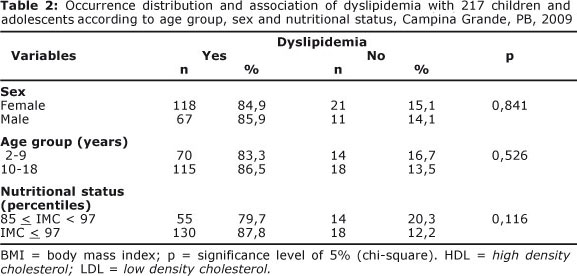
The age group distribution shows that abnormal TC was more frequent in the age group between six and nine years, LDL-c and TG between 10 and 18 years and HDL-c between two and five years (Figure 2). There were no statistically significant differences between these abnormal values (total cholesterol, HDL-c, LDL-c and TG) for the different age groups, as well as the association of dyslipidemia with nutritional status, sex or age group (Table 2).
DISCUSSION
The high prevalence of dyslipidemia found in the study group, mainly in the age group from two to five years, reflects the importance of overweight as risk factor for atherosclerosis.
Studies conducted worldwide have shown that high cholesterol levels in children is directly associated to the prevalence of coronary diseases in adults 13-16. This reinforces the importance of reducing the average cholesterol levels of the population since childhood in order to decrease the frequency of complications of atherosclerosis.
The increasing prevalence of childhood obesity and its importance as risk factor for dyslipidemia is a seriously aggravating factor for cardiovascular diseases. Studies with adolescents have shown that obesity is related to adverse levels of lipids and with atherosclerotic lesions in coronary arteries and aorta, in different degrees, as well as with blood pressure alterations 14, 17,1.
The present study found prevalence of dyslipidemia (85.3%) higher than that described in literature for Brazilian children and adolescents, which ranges from 30.0% in the general population to 68.7% in obese children15,8. A previous study, developed in the same municipality but with adolescents aged 14 to 18 years, reported no cases of obesity and the prevalence of overweight was 14.4%. In relation to dyslipidemia, a high prevalence was observed (66.7%) and low HDL-c was the most frequent alteration (56.7%)18. It is important to emphasize that the study mentioned above used a cutoff point for the desirable value (< 35mg/dL) lower than that adopted in this study.
The results of this study showed the high prevalence of severe obesity (68.2%) and that dyslipidemia was found in all age groups, being most frequently between two and five years of age (88.9%), followed by the age group from 10 to 18 years (86.5%). Ribas et al 16 studied a population from 6 to 19 years of age and found similar results, and the highest prevalence of dyslipidemia was found in the age group from 10 to 15 years.
Freedman et al.13 found that the risk of hypertriglyceridemia appears to be higher in younger children, while the risk of hypercholesterolemia is higher among adolescents. These findings may be the result of changes in the levels of serum lipids and lipoproteins during growth and development, when two phases of significant increase are observed: up to the 2nd year of life and during sexual maturation 3.
A study conducted in São Paulo involving children with family history of premature coronary disease showed that 38.5% had dyslipidemia, a value that rose to 57.1% in those with obesity or overweight. This lower prevalence, compared to our study, could be attributed to the lower reference values adopted for the cutoff of abnormal HDL-c used by the authors19.
The association between body mass and lipid profile can be explained by the activation of the AMP-dependent protein kinase induced by increased insulin and leptin levels, as well as by the reduced activation of adiponectin, which leads to increased fatty acid oxidation. Adiponectin is positively associated with increased insulin sensitivity and HDL-c values and negatively associated with triglycerides6. This has been evidenced by studies that showed, as the main cause of obesity-associated dyslipidemia, mild to moderate increases in TG and decreases in HDL-c20,8.
Prevalence of dyslipidemia of about 50% have been described for children with BMI above the 99th percentile for the age 6 and adolescents showed a positive linear association between BMI and total cholesterol and LDL-c18. In this study, BMI equal to or above the 97th percentile was found to be predominantly associated with abnormal values of HDL-c, instead of LDL-c.
HDL-c is a lipoprotein that acts as a protective factor against cardiovascular disease and was the most prevalent lipid abnormality found in this study (80.6%). This finding was observed, although in smaller proportions, by other authors, ranging from 29.5% to 68.7%7,3. Importantly, the authors studied the general populations of children and adolescents, regardless of nutritional status, and with different cutoff points.
Increased HDL-c levels decrease the relative risk for CVD due to the ability of HDL-c in performing the reverse cholesterol transport. Although some studies consider increased total cholesterol as a cardiovascular risk factor, LDL-c is the main predictor of CVD and is the main target of medical intervention3. In this sense, it is worth mentioning the result of a recently published study, in which increased total cholesterol in childhood was not associated with increased risk for premature endogenous death21, 22.
The high prevalence of TC was found in 37.8% of the study population, whose values are within the range observed in literature. In Brazil, the prevalence of hypercholesterolemia in school children and adolescents is around 35.0%, when the criterion adopted is TC above 170 mg/dL23, a cutoff similar to that used in this study.
Pereira et al21 evaluated children and adolescents from Itapetininga - SP classified by nutritional status and concluded that childhood obesity led to a greater incidence of high total cholesterol, LDL-c and triglycerides, when compared with normal children, which was not observed for HDL-c.
Hypertriglyceridemia was present in 35% of individuals, and this prevalence is similar to that reported by Lima et al 7 and lower than that reported by Valverde et al8 (67.6%). Although TG is not considered an independent risk factor for coronary heart disease, high TG levels can lead to the formation of small and dense LDL-c particles and / or to decreased HDL-c levels 20, a fact also observed in this study, in which abnormal TG associated with HDL-c was present in 24.9% of cases. When not associated, alteration was only found in 0.5% of individuals, which is similar to results of Romaldini et al.19, who found a frequency of 0.9% in children and adolescents with family history of premature coronary disease.
LDL-c was the less frequent lipid abnormality (14.7%); however, it is important to emphasize that obese children appear to have a higher percentage of pattern B LDL-C, with smaller and more atherogenic particles, than children with normal weight for height, which is an aspect not evaluated in this study9.
The prevalence of abnormal LDL-c was higher than those found in studies conducted in schools in the state of Pernambuco20 (10.0%) and Florianópolis 23 (6.0%), but lower than that found by Lima et al7 in obese boys (50%).
In this study, the mean values of lipids, except for LDL-c, are not within the recommended values in the I Guideline for the Prevention of Atherosclerosis in Childhood. The mean total cholesterol (162 mg/dL) and LDL-c values (99 mg/dL) were close to the findings of studies involving school children and adolescents conducted by Giuliano et al23, with values of 162 mg/dL and 92 mg/dL, respectively, and by Moura et al.24, with TC of 160 mg/dl and LDL-C of 96 mg/dL. The mean values of TG (122 mg/dL) and HDL-c (39 mg/dL) were different from those found in these two studies, in the first, the average TG value was 93 mg/dL and HDL-c was 53 mg / dL and in the second, the values were 79 mg/dL and 49 mg/dL, respectively23,24. These findings corroborate observation that the main alterations in the lipid profile in overweight or obese children involve TG and HDL-c.
Some epidemiological studies have shown that lipid and lipoprotein levels are higher in females, regardless of age3,16. In our study, higher frequency of dyslipidemia, although not statistically significant, was observed in males. In this study, this can be explained by the association, in this population, of severe obesity with sex (RP = 3.7).
The literature also shows that the prevalence of dyslipidemia may vary according to the population studied, to the cutoff values adopted as desirable or normal values, as well as to educational, cultural and genetic factors 23. These findings lead us to a limitation of this study, which is the fact that the different criteria adopted, as well as the different populations studied, have made comparisons difficult. However, it is important to emphasize that there were no previous studies involving overweight children and adolescents including the number of cases and the wide age group as in this study.
Finally, although this is not a population-based study, the results found here reflect, to some extent, the profile of the population of obese children and adolescents attended at the Unified He
Thus, the high prevalence of dyslipidemia in the population studied since pre-school age contributes to collect evidence about the need to use overweight or obesity as a criterion to evaluate their lipid profile, regardless of age. Moreover, it is important to emphasize that dyslipidemia is only one of the complications associated with obesity that, in its severe form, was associated with the age group from two to five years.
The implementation of prevention programs, as well as the early detection and intervention of complications associated with obesity, in particular, dyslipidemia, will reduce the risk of cardiovascular diseases in this population, which composes a significant part of the general population. Thus, it will contribute to develop a new health model aimed at health protection and promotion and disease prevention.
ACKNOWLEDGMENTS
To the Foundation for Research Support of the State of Paraíba-FAPESQ for financial support through public notice 01/2008-FAPESQ/PB-MCT/CNPq (Approval No. 198/08)
REFERENCES
1. McMahan CA, Gidding SS, Malcon GT, Tracy RE, Strong JP, McGill HC Jr. Pathobiological determinants of atherosclerosis in youth risk scores are associated with early and advanced atherosclerosis. Pediatrics. 2006; 118: 1447-55. [ Links ]
2. Pereira JC, Barreto SM, Passos VMA. Perfil de risco cardiovascular e auto-avaliação da saúde no Brasil: estudo de base populacional. Rev Panam Salud Publica. 2009; 25(6): 491-8. [ Links ]
3. World Health Organization (WHO). Preventing Chronic Diseases - A Vital Investments. Geneva, 2005. 182 p. [ Links ]
4. Bridger T. Childhood obesity and cardiovascular disease. Paediatr Child Health. 2009; 14(3): 177-182. [ Links ]
5. Rabelo LM. Fatores de risco para doença aterosclerótica na adolescência. J Pediatr (Rio J). 2001; 77(2): s153-s64. [ Links ]
6. Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW et al.. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004; 350(23): 2362-74. [ Links ]
7. Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S et al.. Overweight in Children and Adolescents: Pathophysiology, Consequences, Prevention, and Treatment. Circulation. 2005; 111: 1999-2012. [ Links ]
8 Centers of Disease Control and Prevention (CDC). Prevalence of abnormal lipid levels among youths - United States, 1999-2006. MMWR. 2010; 59(2): 29-33. [ Links ]
9. Carneiro JRI, Kushnir MC, Clemente ELS, Brandão MG, Gomes MB. Obesidade na adolescência: fator de risco para complicações clínico-metabólicas. Arq Bras Endocrinol Metab. 2000; 44(5): 390-6. [ Links ]
10. Lima SC, Arrais RF, Almeida MG, Souza ZM, Pedrosa LF. Perfil lipídico e peroxidação de lipídeos no plasma em crianças e adolescentes com sobrepeso e obesidade. J Pediatr (Rio J). 2004; 80(1): 23-8. [ Links ]
11. Romaldini CC, Issler H, Cardoso AL, Diament J, Forti N. Fatores de risco para aterosclerose em crianças e adolescentes com história familiar de doença arterial coronariana prematura. J Pediatr (Rio J). 2004; 80(2): 135-40. [ Links ]
12. Valverde MA, Vitolo MR, Patin RV, Escrivão MAMS, Oliveira FLC, Ancona-Lopez F. Investigação de alterações do perfil lipídico de crianças e adolescentes obesos. Arch Latinoam Nutr. 1999; 49: 338-43. [ Links ]
13. Giuliano ICB, Caramelli B, Pellanda L, Duncan B, Mattos S, Fonseca FAH et al.. I Diretriz de Prevenção da Aterosclerose na Infância e na Adolescência. Arq. Bras. Cardiol. [online]. 2005, 85(6): 3-36. [ Links ]
14. World Health Organization - WHO. Physical Status: the study and interpretation of anthropometry. WHO Technical Report Series n. 854. Geneva: WHO, 1995. [ Links ]
15. Centers of Disease Control and Prevention (CDC) table for calculated body mass index values for selected highs and weights for ages 2 to 20 years. Developed by the National Center for Health Statistc in collaboration with the National Center for Chronic Disease Prevention and Health Promotion, 2000. Publicado em maio de 2002, modificado 20/04/2001. Disponível em: htpp://www.cdc.gov/growthcharts. [ Links ]
16. Sposito AV, Caramelli B, Fonseca FAH, Bertolami MC, Afiune NA, Souza AD et al.. IV Diretriz Brasileira sobre Dislipidemias e Prevenção da Aterosclerose do Departamento de Aterosclerose da Sociedade Brasileira de Cardiologia. Arq Bras Cardiol. 2007; 88(1): 1-19. [ Links ]
17. Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001; 108(3): 712-8. [ Links ]
18. Hong MY. Atherosclerotic Cardiovascular Disease Beginning in Childhood. Korean Circ J. 2010; 40: 1-9. [ Links ]
19. França E, Alves JGB. Dislipidemia entre crianças e adolescentes de Pernambuco. Arq Bras Cardiol. 2006; 87(6): 722-7. [ Links ]
20. Ribas AS, SILVA LCS. Dislipidemia em escolares na rede privada de Belém. Arq. Bras. Cardiol. 2009; 92(6): 446-51. [ Links ]
21. Carvalho DF, Paiva AA, Melo ASO, Ramos AT, Medeiros JS, Medeiros CCM et al.. Perfil lipídico e estado nutricional de adolescentes. Rev. bras. Epidemiol. 2007; 10(4): 491-8. [ Links ]
22. Pereira A, Guedes AD, Verreschi ITN, Santos RD, Martinez TLR. A Obesidade e sua Associação com os Demais Fatores de Risco Cardiovascular em Escolares de Itapetininga, Brasil. Arq Bras Cardiol. 2009; 93(3): 253-60. [ Links ]
23. Franks PW, Hanson R L, Knowler WC, Sievers, ML, Bennett PH, Looker HC, MB. Childhood Obesity, Other Cardiovascular Risk Factors, and Premature Death. N Engl J Med. 2010; 362: 485-93. [ Links ]
24. Giuliano IC, Coutinho MS, Freitas SF, Pires MM, Zunino JN, Ribeiro RQ. Lípides séricos em crianças e adolescentes da rede escolar de Floria-nópolis - Estudo Floripa Saudável 2040. Arq Bras Cardiol. 2005; 85(2): 85-91. [ Links ]
25. Moura EC, de Castro CM, Mellin AS, de Figueiredo DB. Perfil lipídico em escolares de Campinas, SP, Brasil. Rev Saúde Pública. 2000; 34(5): 499-505. [ Links ]
Manuscript submitted
Dec 06 2010, accepted for publication Aug 10 2011. Realização
do trabalho: Núcleo de Estudos e Pesquisas Epidemiológicas (NEPE)
– Universidade Estadual da Paraíba(UEPB) - Endereço: Avenida
das Baraúnas, 351 - Cidade Universitária – Prédio
dos Mestrados – 2º andar - CampinaGrande-PB, CEP: 58429-500, Fone/Fax:
(83) 3315-3300 Correspondence to:
Correspondence to:
carlacamposmunizmedeiros@gmail.com
Pesquisa financiada pela Fundação de Apoio à Pesquisa do
Estado da Paraíba-FAPESQ, através do edital 01/2008-FAPESQ/PB-MCT/CNPq
(Termo de Concessão nº 198/08).











 texto em
texto em 


