Serviços Personalizados
artigo
Indicadores
Compartilhar
Journal of Human Growth and Development
versão impressa ISSN 0104-1282
Rev. bras. crescimento desenvolv. hum. vol.22 no.2 São Paulo 2012
ORIGINAL RESEARCH
Influence of overweight and obesity on posture, overall praxis and balance in schoolchildren
Andrezza Aparecida AleixoI; Elaine Leonezi GuimarãesII; Isabel Aparecida Porcatti de WalshII; Karina PereiraI, II
ICurso de Pós-Graduação em Educação Física. Universidade Federal do Triângulo Mineiro - Uberaba/MG
IIInstituto de Ciências da Saúde. Departamento de Fisioterapia Aplicada. Universidade Federal do Triângulo Mineiro - Uberaba/MG
ABSTRACT
This study aimed to evaluate overweight or obese school children aged 6-12 years on postural changes on the spine and lower limbs due to overload, balance and overall praxis. Study participants were 34 students (27 girls and seven boys) enrolled in a school of Uberaba / state of Minas Gerais, with a diagnosis of overweight or obesity according to the infant Body Mass Index (BMI). For praxis and global balance evaluation was used Fonseca psychomotor battery while posture was assessed through an evaluation form based on Kendall. Data analysis was based on descriptive statistics through the percentage method. The Kolmogorov-Smirnov parametric tests was used to verify the normality of the sample and the "t-Student" test to detect differences between groups, considering the significance level of 5% (p <0 , 05). The results showed postural changes in both groups, static balance without significant difference and a significant difference for the dynamic equilibrium there was significant difference characterizing the overweight group with hyperpraxic psychomotor profile, while the obese group was eupraxic. The overall praxis assessment showed significant difference between the groups in three sub-factors: eye-foot coordination (p = 0.022), dissociation of the upper limbs (p = 0.042) and the lower limbs (p = 0.045). The dissociation of lower and upper limbs was found in overweight subjects with eupraxic psychomotor profile while obese patients were dyspraxic. The eye-foot coordination analysis presented dyspraxia in both groups. The results indicatethat overweight and obesity in children may alter posture, balance and overall praxis.
Key words: children; obesity; posture; postural balance; overweight; physiotherapy.
INTRODUCTION
Obesity is a multifactorial disease that occurs through a combination of genetic, environmental and behavioral factors, and is currently found in epidemic levels at higher rates than malnutrition1,2.
Brazil is undergoing a nutrition transition with a reduction in malnutrition, which is characterized by low weight as well as short child and adult height. The same author also reports that in 1975, a little over 8% of Brazil's population was malnourished and about a half (4%) was obese. In recent years, those data have reversed, with 9% obesity and 3% malnutrition3.
During childhood, obesity can lead to difficulties in socialization, cardiorespiratory changes, high blood pressure, increased waist circumference, nonalcoholic fatty liver disease, polycystic ovary syndrome (PCOS), respiratory changes, orthopedic disorders, as well as alterations in normal motor development (NMD) compared to children with normal weight for their age 1,4-8.
Obese children featured several risk factors for the development of cardiovascular diseases and that metabolic syndrome is a reality for many of them, occurring in 17.3% of the obese children in their study. They also affirmed that this can lead to the earlier onset of diabetes mellitus type 2 and atherosclerotic diseases9.
Liver damage that accompanies childhood obesity is the result of the combination between the insulin resistance and oxidative stress. Damage usually starts with fatty infiltration of the liver, possibly progressing into steatohepatitis (20% of cases) and cirrhosis of the liver (2% of cases). In adolescents with polycystic ovary syndrome, the prevalence of obesity is between 55% and 73%. The risk of developing diabetes mellitus type 2 in patients with polycystic ovary syndrome is 3-7 times greater than in regular women, also due to insulin resistance1.
It was observed that many of the risk factors for cardiovascular diseases begin in childhood, including high blood pressure, which can lead to coronary atherosclerosis and left ventricular hypertrophy10. Other study confirmed that children with increased waist circumference characteristic of obesity or overweight were 2.8 times more likely to have higher blood pressure than children with adequate waist circumference for their weight and age11.
One of the respiratory problems resulting from obesity is Obesity Hypoventilation Syndrome (Pinckwickian Syndrome), causing air trapping and chronic alveolar hypoventilation. Patients become sleepy, are easily fatigued from effort and may present edemas in the lower limbs. These patients also present mood disorders and headaches in the evening or morning12.
Orthopedic disorders are frequent in obesity as well, due to joint overload, particularly in the knees. Slipped capital femoral epiphysis is also common13.
The excess body weight in obese or overweight children may result in reduced stability and the need to seek mechanisms of postural adaptation. This can cause changes to the habitual balance axis, resulting in increased lumbar lordosis, with abdominal protrusion and anterior tilting of the pelvis (anteversion). Over time, excessive shortening or lengthening may occur, which combined with anterior pelvic tilting lead to internal hip rotation and the onset of valgus knee and flat feet1,14.
Obese or overweight children find it difficult to take part in physical activities, either by the embarrassment of exposing their body or by the difficulty in performing the exercises. This leads them to choose activities with low energy expenditure, thus, reducing their level of physical activity5,15. Such a condition may in fact aggravate postural changes, dyspraxia and poor balance in those children.
Coordination or overall praxis is associated with conscious activity, planning, regulation and verification. It is linked to more anterior areas of the cortex, such as the premotor area, which its main role is to perform complex global movements that take place in a given period of time and require combined activity by various muscle groups. Its evaluation makes it possible to detect not only motor functioning but also the quality of sensory and psychomotor integration to evidence brain integrity, from the brainstem to the cerebral hemispheres. Any failure in that mechanism indicates dyspraxia16.
Dyspraxia means slow or inefficient planning of actions, regardless of normal intelligence or functional motricity. It can also mean an integrative sensory and psychomotor dysfunction16. Children with altered overall praxis are considered dyspraxic and have learning disabilities or slight brain dysfunctions16,17. Overall praxis is the simultaneous functioning of different muscle groups, in order to execute ample and voluntary movements, particularly involving the work of lower and upper limbs, and the torso16. D'Hondt et al.18 report that obesity and overweight have a negative impact on motor skill and postural balance, when both are activated simultaneously.
Lack of training and ample movement may also lead to delayed neuropsychomotor development (NPMD) compared to children at the ideal weight for their age. That occurs because motricity and intelligence develop as the result of the interaction of genetic, cultural and psychosocial factors, intrinsic and extrinsic, all of which influence child development4,17,19.
Considering the possibility that excess body mass influences balance and overall praxis while performing global motor activities, the objective of the present study was to evaluate balance and overall praxis activities on overweight and obesity schoolchildren.
METHODS
It is a prospective, cross-sectional and analytical study, approved by the Research Ethics Committee of the Universidade Federal do Triângulo Mineiro, under protocol 1492/2009, performed at a public school in the city of Uberaba-MG, between September and December 2009.
The first step was to assess the number of schoolchildren enrolled from the first to seventh grades at a local public school in the city of Uberaba-MG, totaling 432 students. A total of 268 students between 6 and 12 years old were evaluated. Among them, 74 were diagnosed as overweight (higher than the 85th and lower or equal to the 97th percentile) or with childhood obesity (higher than the 97th and lower or equal to the 99.9th percentile) (World Health Organization - WHO)20, with no other underlying condition. A total of 34 schoolchildren effectively took part in the study, and were evaluated for postural changes, balance and overall praxis using Fonseca's Psychomotor Battery (PMB)16. Postural evaluation was based on Kendall's study21.
To classify overweight and obesity, the body mass index (BMI) was used, which is the value obtained by dividing weight (kg) by height2 (m2), as well as body measurements (weight and height) and percentile analysis in the WHO age and gender curve20. Weight measurements were obtained in kilograms, using a Camry-brand BR9010 mechanical scale. Height was assessed using a measuring tape affixed on a wall, with children barefoot in standing position, arms alongside the body and feet together.
Anamnesis was first used to evaluate the schoolchildren, to identify: whether the child practiced any regular physical activity, its frequency and duration; whether there were other cases of obesity in the family; whether the child felt any pain when performing these physical activities, and the localization in the body; and what the child's favorite playing activity was. Vital signs such as blood pressure, heart rate and respiratory rate at rest were recorded.
Fonseca's Psychomotor Battery (PMB) was used to evaluate balance and overall praxis16 for the following aspects: eye-hand coordination, eye-foot coordination, dysmetria and dissociation. The following balance traits were evaluated: stillness, static and dynamic balance, graded on a scale from 1 to 4. A score of 1 evidenced an apraxic profile, imperfect, incomplete and uncoordinated performance (poor); 2 was dyspraxic, performed with control difficulties (satisfactory); 3 was eupraxic, with controlled and adequate performance (good); and 4 was hyperpraxic, with perfect, economical, harmonious and well-controlled performance (excellent).
For overall praxis, eye-hand coordination was measured by having the child throw a tennis ball four times into a paper box placed on a chair 2.5 m away; eye-foot coordination was assessed by having the child kick the tennis ball four times so that it passed through the legs of the chair 2.5 m away; dysmetria was evaluated by observing any lack of coordination when performing the two previous tasks; and dissociation was observed by asking the child to perform hand clapping and foot stomping, and then jump and clap hands simultaneously.
Balance was evaluated by observing the following factors: stillness, in which the child had to remain 60 seconds with feet together, standing up and with hand resting on the sides of the thighs; static balance, in which the child should remain still with eyes closed and hand on hips during 20 seconds, first with one foot in front of the other (tip-toe/heel), then on tip-toe, and next on one foot with the choice of best balance (dominant foot); and dynamic balance, in which the child should stand up, hand on hips, and walk a 3-meter straight line with one foot in front of the other (tip-toe/heel); hand on hips performing the following tasks: walk forward and backward, laterally to the right and left, skip on one foot for 3 meters with choice of foot, and jump for a total of 3 meters with eyes closed and feet together, first forward than backward.
Postural evaluation was based on Kendal21, observing the child standing with arms alongside the body, on anterior, lateral and posterior views, assessing: head protrusion and tilting, shoulder protrusion, dorsal kyphosis, knee hyperextension, asymmetry at popliteal fossae level, valgus or varus knee, flat feet, protruded abdomen and pelvic anteversion.
Data on age, gender, vital signs and body measurements were analyzed using simple descriptive statistics through the percentage method.
The quantitative variables of global praxis and balance were analyzed using GraphPad InStat software, and previously subjected to the Kolmogorov-Smirnov test to evaluate distribution. Once the normality of data was detected, the variables were compared between the overweight and obesity groups by Student's t-test, considering a 5% significance level.
RESULTS
The data show that among the 432 schoolchildren, 268 (62.03%) aged between 6 and 12 years old. Among them, 74 (27.61%) schoolchildren showed overweight or obesity. Among the 34 schoolchildren with abnormal MBI values, 11 (32.35%) were overweight and 23 (67%) were obese. Table 1 shows data on age and body measurements of the 34 schoolchildren.
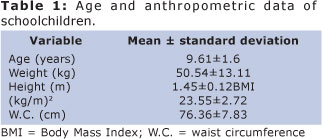
With regard to vital signs, mean respiratory rate was 19.85 (±2.93) cpm, heart rate was 82.17 (±10.65) bpm, and mean blood pressure was 80.61 (±9.69) mmHg.
According to the habit assessment questionnaire, none of the schoolchildren reported performing any physical activity in addition to that offered during physical education classes in school, and only 14.70% reported feeling pain or discomfort in the legs and back when doing physical exercises. The weekly frequency of physical activity ranged between twice (73.52% of schoolchildren) and three times a week (26.47% of schoolchildren), with a duration of 50 minutes. A total of 5.88% of the evaluated schoolchildren reported not enjoying doing those exercises.
The children were also asked whether other family members practiced physical activities, and which ones. The answer was yes for 32.35%, predominantly walking and gym work. 76.52% of schoolchildren reported having close family members with overweight or obesity.
When asked about their balance, 29.41% reported that they fall frequently, and 67.64% have poor balance or instability in the feet and ankles.
With regard to postural changes, Table 2 shows that 63.6% of overweight schoolchildren had protruded head position, 63.6% protruded shoulder, 72.7% had different shoulder heights, 54.5% lumbar hyperlordosis, and 54.5% had asymmetry at the popliteal fossae level. In the obesity group, 82.6% had different shoulder heights, 65.2% lumbar hyperlordosis, 47.8% hyperextended knees, 86.9% asymmetry at popliteal fossae level, 65.2% had valgus knees, 78.3% protruded abdomen, and 47.8% showed pelvic anteversion.
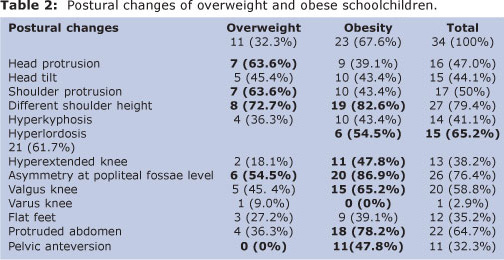
Table 3 reports the results regarding balance and overall praxis. No significant difference was found between obesity and overweight in sub-factor stillness and static balance. For dynamic balance, there was a significant difference in four sub-factors: shuttle walk test (p = 0.049), feet together forward (p = 0.009), feet together backward (p = 0.044) and feet together with eyes closed (p = 0.034). The overweight group showed a hyperpraxic psychomotor profile for the shuttle walk, feet together forward and feet together backward tests, whereas the obese group members were eupraxic. Both groups had eupraxic psychomotor profiles for sub-factor feet together with eyes closed.
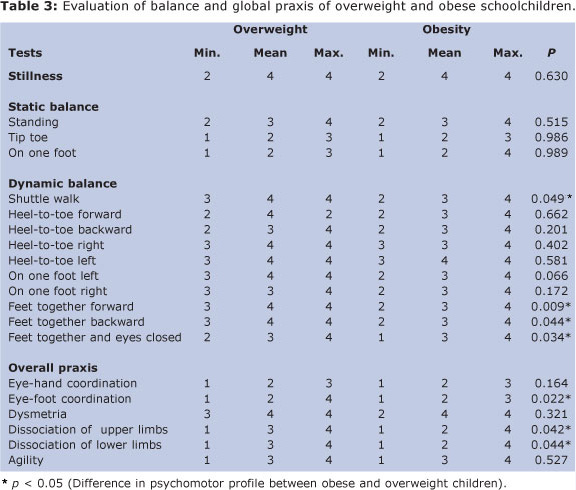
A significant difference was found in overall praxis between the two groups in three sub-factors: eye-foot coordination (p = 0.022); dissociation of upper limbs (p = 0.042) and dissociation of lower limbs (p = 0.0448). Sub-factors dissociation of lower and upper limbs in the overweight group showed a eupraxic psychomotor profile, whereas the obese group members were dyspraxic. Both groups were dyspraxic for eye-foot coordination.
DISCUSSION
The present study indicated that 74 of the 432 enrolled students (27.61%) were overweight or obese. The overweight rates in the Brazilian population have increased to the point of being considered an epidemic2,22. Along with a decline in child malnutrition, Brazil has seen a 16.7% increase in child overweight3. Pierine et al.23 observed a 33% prevalence of overweight and obese students, according to the BMI classification, similar for both genders. In contrast, Simon et al.24 observed a 35.4% rate of excess weight in a sample of 806 schoolchildren, showing no difference according to gender or age.
Postural changes were observed in both groups, with greater frequency for the spine and lower limbs, in which 14.7% reported pain or discomfort in the legs and back while performing physical activities. Previous studies showed that obesity creates an overload in the spinal column, altering its normal curvatures (mostly exacerbating them); postural changes in the lower limbs are quite frequent as well14. Obesity results in postural changes from the excess body mass, reduced stability and increased mechanical adaptations25. Wearing et al.26 observed that obese children undergo a variety of biomechanical changes in the lower extremities which may be linked to musculoskeletal pain in children and adolescents; however, those data are limited.
Among the 34 evaluated schoolchildren, 61.7% showed lumbar hyperlordosis, 64.7% had protruded abdomen and 32.3% pelvic anteversion, corroborating the findings of Fisberg2. That author observed a high number of postural changes, such as lumbar hyperlordosis, head protrusion, pelvic anteversion, medial hip rotation, valgus knee and flat feet, caused by excess body mass overloading the musculoskeletal system. Filippin et al.27 found similar results and affirmed that excess body mass in obese subjects contributes to reduced stability and leads to a need to seek posture adaptation mechanisms. Those authors also evidenced that obese children can present changes to their normal balance axis, resulting in increased lumbar lordosis, with abdominal protrusion and anterior tilting of the pelvis (anteversion).
The rates of valgus knee and flat feet were 58.8% and 35.2%, respectively. A previous study showed that over time, excessive shortening and lengthening take place, which combined with anterior pelvic tilt, lead to internal hip rotation and the onset of valgus knee and flat feet1.
Reports were found of frequent falls in 29.41% and poor balance in 67.64% of the evaluated schoolchildren. To Brun and Neto5, obese children have greater difficulty with balance, temporal organization and body scheme. Balance evaluation comprises postural control and reveals the level of integrity of important neurological areas and circuits, without which no activity could take place16.
In the evaluation of dynamic balance, a hyperpraxic psychomotor profile was observed in the overweight group, and eupraxic profile in obese children. Although both were within normality, the overweight group had better performance, corroborating the theory that children with excess body mass undergo balance changes5,28.
When analyzing the profile of overall praxis tasks, a significant difference was observed between the two groups for sub-factor dissociation of lower and upper limbs, with eupraxic psychomotor profile in the overweight group and dyspraxic profile in the obesity group. This confirms that overweight children have changes in overall dynamic coordination, as described by Hall29 and Bueno30, who observed that balance is responsible for awareness and distribution of weight in space, time and the gravity axis, and is the basis of all overall dynamic coordination.
As for physical activity, 5.88% of the evaluated schoolchildren declared not enjoying it. It may be related to the difficulties found in performing those activities, as reported by Pazin et al15, who, detected a greater deficit in temporal, spatial and balance organization in obese children, relating inactivity to obesity, difficulty in performing certain activities, choice of activities with low calorie expenditure, embarrassment in showing their bodies, as well as lifestyle traits.
With regard to the occurrence of obesity in the family, over 75% of the schoolchildren reported having obese family members (father, mother, grandparents, uncles/aunts or siblings), which suggests the presence of genetic factors and/or poor eating habits in the evaluated groups, given that physical activity was reported as constant 2 to 3 times a week for 50 minutes. Vitolo31 reports that when there are obese people in the family, the likelihood of the child developing obesity is much greater. If the father and mother are obese, the child presents an 80% chance of being obese.
All schoolchildren were within the normal range with regard to the vital signs assessed prior to the evaluations, as per Sarnento32 and Mion et al.33. Emphasis should be given to the collection of vital signs due to the close link between them and the different risk factors for the development of cardiovascular diseases in childhood and adult life34. A direct association between high blood pressure and obesity has been shown in several studies10,35, large waist circumference in children has also evidenced a high risk of developing coronary diseases11.
Although the study had a limiting factor - the absence of a control group - it was possible to observe differences between the groups of obese and overweight schoolchildren, suggesting that excess body mass can influence balance and overall praxis during global motor activities and daily life tasks.
Considering the obtained results, it may be concluded that overweight and obese schoolchildren are within normality parameters for the evaluation of global praxis and balance, although the overweight group showed better performance than the obese group during the evaluation: hyperpraxic profile for overweight schoolchildren and eupraxic for the obese group in dynamic balance, and eupraxic profile for overweight schoolchildren and dyspraxic profile for obese children in overall praxis.
REFERENCES
1. Sociedade Brasileira de Pediatria, Departamento de Nutrologia. Obesidade na infância e adolescência - manual de orientação. São Paulo; 2008. 120 p. [ Links ]
2. De Oliveira CL, Fisberg M. Obesidade na infância e adolescência: uma verdadeira epidemia. Arq Bras Endocrinol Metab. 2003;47(2):107-8. [ Links ]
3. Monteiro CA, Lenise M, Ana LMS, Barry MP. Da desnutrição para a obesidade: a transição nutricional no Brasil. In: Monteiro CA. Velhos e novos males da saúde no Brasil: evolução do país e as doenças. 2 ed. São Paulo: Hucitec; 2000. p. 247-255. [ Links ]
4. Soares D, Petroski EL. Prevalência, fatores etiológicos e tratamento da obesidade infantil. Rev Bras Cineantropom Desempenho Hum. 2003;5(1):63-74. [ Links ]
5. Brum KO, Neto FR. O perfil motor de escolares obesos. Rev Digital [Internet]. 2009 [citado 2009 Ago 28];14(134). Disponível em: http://www.efdeportes.com/. [ Links ]
6. Oliveira AM, Cerqueira EM, Souza JS, Oliveira, AC. Sobrepeso e obesidade infantil: influência de fatores biológicos e ambientais em Feira de Santana, BA. Arq Bras Endocrinol Metab. 2003;47:144-50. [ Links ]
7. Silva GA, Balaban G, Motta ME. Prevalence of overweight and obesity in children and adolescents of different socioeconomic conditions. Rev Bras Saúde Matern Infant. 2005;5:53-9. [ Links ]
8. Abrantes MM, Lamounier JA, Colosimo EA. Overweight and obesity prevalence among children and adolescents from Northeast and Southeast regions of Brazil. J Pediatr. 2002;78:335-40. [ Links ]
9. Ferreira AF, Oliveira CER, França NM. Síndrome metabólica em crianças obesas e fatores de risco para doenças cardiovasculares de acordo com a resistência à insulina (HOMA-IR). J Pediatr. 2007;83(5):21-6. [ Links ]
10. Salgado CM, Carvalhaes JTA. Hipertensão arterial na infância. J Pediatr. 2003; (79 Suppl 1):S115-124. [ Links ]
11. Constanzi CB, Halpern R, Rech RR, Bergmann LA, Alli LR, Mattos AP. Fatores associados a níveis pressóricos elevados em escolares de uma cidade de porte médio do sul do Brasil. J Pediatr. 2009;85(4):335-340. [ Links ]
12. SILVA GA. Síndrome Obesidade-Hipoventilação Alveolar. In: Simpósio Distúrbios Respiratórios do Sono- Cap. IV. (Medicina, Ribeirão Preto, v. 2, n. 39, p. 195-204, 2006). [ Links ]
13. Escrivão MAMS, Oliveira FLC, Taddei JAAC, Lopez FAA. Obesidade exógena na infância e na adolescência. J Pediatr. 2000;(76 Suppl 3): S305-310. [ Links ]
14. Bruschini S, Nery CAS. Aspectos Ortopédicos da Obesidade na Infância e Adolescência. In: Fisberg M. Obesidade na infância e adolescência. São Paulo: Byk; 1995. p. 105-125. [ Links ]
15. Pazin J, Frainer DESF, Moreira D. Crianças obesas têm atraso no desenvolvimento motor. Rev Digital [Internet]. 2006 [citado 2009 Ago 28];11(101). Disponível em: http://www.efdeportes.com/. [ Links ]
16. Fonseca V. Manual de observação psicomotora: significação psiconeurológica dos fatores psicomotores. Porto Alegre: Artes Médicas; 1995. 371 p. [ Links ]
17. Fonseca V. Abordagem Psicobiológica. In: Fonseca V. Psicomotricidade - Filogênese, Ontogênese e Retrogênese. Rio de Janeiro: Wak, 2009. p. 143-172. [ Links ]
18. D'Hondt E, Deforche B, Bour-deaudhuij ID, Lenoir M. Childhood obesity affects fine motor skill performance under different postural constraints. Neuroscience Letters. 2008; 440:72 - 75. [ Links ]
19. Nobre FSS, et al. Análise das oportunidades para o desenvolvimento motor (affordances) em ambientes domésticos no Ceará - Brasil. Rev Bras Crescimento Desenvolv Hum. 2009;19(1):9-18. [ Links ]
20. World Health Organization. WHO Child Growth Standards. 2007 [cited 2009 Set 25]. Disponível em: http://www.who.int/childgrowth/en/. [ Links ]
21. Kendall FP, Mccreary EK, Provance PG. Postura. In: Kendall FP, Mccreary EK, Provance PG. Músculos provas e funções. 5. ed. São Paulo: Manole; 2007. p. 49-117. [ Links ]
22. Kosti RI, Panagiotakos DB. The epidemic of obesity in children and adolescents in the world. Cent Eur J Public Health. 2006;14:151 - 9. [ Links ]
23. Pierine DT, Carrascosa APM, Forna-zari AC, et al. Composição, atividade física e consumo alimentar de alunos do ensino fundamental e médio. Rev Motriz. 2006;12(2): 113-124. [ Links ]
24. Simon VGN et al. Prevalência de sobrepeso e obesidade em crianças de dois a seis anos matriculadas em escolas particulares no município de São Paulo. Rev Bras Crescimento Desenvolv Hum. 2009;19(2):211-218. [ Links ]
25. Shumway-Cook A, Woollacott MH. Controle Postural. In: Shumway-Cook A, Woollacott MH Controle Motor- teoria aplicações práticas. São Paulo: Manole; 2003. p. 153-178 [ Links ]
26. Wearing SC, Hennig EM, Byrne NM, Steele JR, Hills AP. The impact of childhood obesity on musculoskeletal form. Obes Rev. 2006;7:209 - 18 [ Links ]
27. Philippin NT, Sacco ICN, Barbosa VLP, Lobo da Costa PHL. Estudo da distribuição das pressões plantares em crianças obesas: efeitos de um programa de intervenção. Rev Bras Educ Fís Esp. 2008;22(1):25-33. [ Links ]
28. McGraw B, McClenaghan BA, Williams HG, Dickerson J, Ward DS. Gait and postural stab ility in obese and nonobese prepubertal boys. Arch Phys Med Rehabil. 2000;81:484-9 [ Links ]
29. Brody LT, Dewane J. Deficiência de Equilíbrio. In Hall CM, Brody LT. Exercício terapêutico na busca da função. 2 ed. Rio de Janeiro: Guanabara Koogan; 2007. p.152-187. [ Links ]
30. BUENO JM. Desenvolvimento Neurológico. In: BUENO JM. Psicomotricidade, Teoria & Prática - Estimulação, Educação e Reeducação Psicomotora com Atividades Aquáticas. São Paulo: Lovise; 1998. p. 41-50. [ Links ]
31. Vitolo MR, Campagnolo PD. Fatores Determinantes para o Excesso de Peso em Crianças e Adolescentes. In: Vitolo MR. Nutrição da Gestação ao Envelhecimento. Rio de Janeiro: Rubio; 2008. p. 339-345. [ Links ]
32. Peixe AAF, Carvalho FA, Sarmento GJV. Avaliação de Fisioterapia Respiratória Pediátrica e Neonatal. In Sarmento GJV. Fisioterapia Respiratória em Pediatria e Neonatologia. São Paulo: Manole; 2007. p. 20-35. [ Links ]
33. Sociedade Brasileira de Cardiologia, Sociedade Brasileira de Hipertensão, Sociedade Brasileira de Nefrologia. V Diretrizes brasileiras de hipertensão arterial. São Paulo; 2006. Epidemiologia da hipertensão arterial; p. 5-13. [ Links ]
34. Ferreira AF, Oliveira CER, França NM. Síndrome metabólica em crianças obesas e fatores de risco para doenças cardiovasculares de acordo com a resistência à insulina (HOMA-IR). J Pediatr. 2007;83(5):21-6. [ Links ]
35. Silva MCP, Ramos CHB, Costa RF. Estado Nutricional e Níveis Pressóricos de Escolares Adolescentes da Cidade de Cubatão - SP, Brasil. Rev Bras Crescimento Desenvolv Hum. 2008;18(3): 288-297. [ Links ]
 Corresponding author:
Corresponding author:
andrezzaleixo@yahoo.com.br
Manuscript submitted Apr 10 2011
Accepted for publication Apr 16 2012











 texto em
texto em 

