Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Journal of Human Growth and Development
versão impressa ISSN 0104-1282versão On-line ISSN 2175-3598
J. Hum. Growth Dev. vol.30 no.1 São Paulo jan./abr. 2020
https://doi.org/10.7322/jhgd.v30.9958
ORIGINAL ARTICLE
Ophidian envenomings in a region of Brazilian Western Amazon
Envenenamentos ofídicos em uma região da Amazônia Ocidental Brasileira
Ozianndeny Ferreira CâmaraI; Delcio Damasceno da SilvaI; Marlon Negreiros de HolandaI; Paulo Sérgio BernardeII; Ageane Mota da SilvaIII; Wuelton Marcelo MonteiroIV; Marcos Venicicus Malveira de LimaV; Adilson MonteiroVI; Rubens WajnsztejnI
ILaboratório de Delineamento de Estudos e Escrita Científica. Centro Universitário Saúde ABC, Santo André, São Paulo, Brazil
IILaboratório de Herpetologia, Campus Floresta, Universidade Federal do Acre, Cruzeiro do Sul, Acre, Brazil
IIIInstituto Federal do Acre, Campus de Cruzeiro do Sul, Acre, Brazil
IVInstituto de Pesquisa Clínica Carlos Borborema, Fundação de Medicina Tropical Dr. Heitor Vieira Dourado, Manaus, Amazonas, Brazil. Escola Superior de Ciências da Saúde, Universidade do Estado do Amazonas, Manaus, Amazonas, Brazil
VSecretaria de Estado de Saúde do Acre, Rio Branco, Acre, Brazil
VIUniversidade Federal do MAto Grosso - UFMT campus Rondonópolis. Brazil
ABSTRACT
INTRODUCTION: Snakebites are a public health problem and are considered clinical emergencies, what makes studies in high-incidence regions very important
OBJECTIVE: To describe the clinical and epidemiological aspects of patients suffering from snakebite accidents in a region of the Western Amazon, Brazil
METHODS: It is a cross-sectional, retrospective and documentary quantitative approach, from 2015 to 2016, held at the Regional Hospital of Juruá, located in the city of Cruzeiro do Sul, Acre, Brazil. Epidemiological data were obtained from the forms of the Notification Disease Information System (SINAN), in the Epidemiological Surveillance Sector of the hospital. The following variables were verified: month of occurrence, snake identification (type of accident), accident location (urban and rural), locality, municipality, victim data (age group, sex, anatomical region affected), symptoms and signs circumstances of the accident, time elapsed between accident and care, number of ampoules used, and type of serum
RESULTS: An average of 124 cases of snakebites were treated per year (76.71 cases per 100,000 inhabitants/year), most of them were botropic accidents and the patients were male adult and rural workers, bitten in the lower limbs. More than 30% of cases were treated six hours after poisoning and 24-hour care is a risk factor for complications, as seven of the eight patients who had complications were treated within one day of the accident
CONCLUSION: It was presented a constant increase in the cases, which generated a worrying point of reflection, which may be associated with two factors, where one turns to the improvement in the displacement of victims (improvements in branch roads and implementation of SAMU speedboat) facilitating plus transport and telephone coverage by improving communication, or the failure of public health policies to provide better conditions and guidance to the population
Keywords: venomous animals, snakebites, Amazonian ecosystem.
INTRODUCTION
Authors summary
Why was this study done?
Snakebites throughout the Western Amazon is a major public health problem due to its high incidence, so it is necessary to know the main species that cause more accidents in each region. In the Amazon, among the predominant work activities, are extraction, fishing and hunting, thus making this population more vulnerable to the occurrence of this disease and leaving them exposed to irreversible injuries or even death. And one of the main difficulties for the urgency of care is the difficult access to the reference unit for this care because it is concentrated in the urban perimeter and the places of occurrence of these ophidian poisonings are in regions where the access is by river or road in precarious conditions, not allowing vehicle access in the rainy season.
What did the researchers do and find?
In previous studies carried out in the state of Acre, many lachetic accidents were observed and the number of botropic accidents was underestimated. This fact does not corroborate with the report of the residents of this locality who affirm that the most common species is Surucucu or Jararaca being the main cause of botropic accidents. It was also demonstrated by this and other studies that the most common accident in this region is the botropic type and the number of lachetic and elapidic accidents are uncommon. This data is important so that a sufficient number of specific antivenom can be made available for each region, thus avoiding waste and lack of it.
What do these findings mean?
This problem is of great importance to public health because it is a compulsory notification and requires the monitoring of epidemiological surveillance so that it can determine educational actions, guide the population about the occurrence and need for georeferencing of the places that present the highest occurrence and species that affect this population. Thus, it brings an alert for the implementation of a public policy for snakebites, favoring rapid care, reduction of underreporting and adequate distribution of antifidic serum according to the species affected in the region.
In Brazil, approximately 29,000 cases of snakebite accidents are reported per year by the SINAN (Reporting Disease Information System) with an average of 129 reported deaths (0.44% lethality)1.
The epidemiological profile of the victims comprises in most cases male rural workers, aged between 15 and 49 years and the lower limbs are the most affected2-4. Although the National Reporting Disease System (SINAN) is the best tool to collect some epidemiological variables of ophidism in the country5, underreporting exists due to failures during the completion of forms by health professionals, which results in the loss of valuable information for a more global understanding of ophidism as a public health problem1.
In addition, there is the possibility of unreported cases occurring in places farther from hospital care, especially in locations that are more difficult to reach, such as in the interior of the Amazon5,6.
In the Brazilian Amazon there are the largest number of reports of snakebite accidents per year1,7 and also the highest percentage of cases reported among children and adolescents between 10 and 19 years old, corresponding to 23.2% of victims8. The less time elapses between the snakebite accident and the onset of serotherapy, the less likely it is that complications and sequelae will develop, as well as the evolution to death4,9.
One of the biggest problems regarding snakebite accidents in the Amazon is the time elapsed between the bite and the medical care, mainly due to the geographical conditions present in the region4,10.
In the Western Amazon, the municipality of Cruzeiro do Sul, located in the state of Acre in the region of Alto Juruá, is characterized by a high incidence of cases of snakebite accidents. This frequency of snakebite accidents may be associated with the activities (extractivism, fishing, hunting, flour production) of people living in forest areas (national park, state forests, extractive reserves and indigenous lands) who are more exposed to snakebite accidents11.
The most common venomous snake responsible for most snakebite accidents in this region is Bothrops atrox, known regionally as surucucu, jararaca, boca-podre ou surucucu-do-barranco11,12. Bothrops atrox is the most abundant venomous snake in the Amazon and this is largely due to its ease in adapting to altered environments (grasslands, crops and even urban areas) and feeding on various types of prey (rodents, amphibians), lizards, other snakes, birds, centipedes)13,14.
Epidemiological information on health problems is fundamental for the elaboration of proposals for educational actions, preventive measures and also can provide subsidies for planning in hospital management (eg, estimating the amount of serum ampoules needed throughout the year, availability of beds).
Thus, this study aims to describe the clinical and epidemiological aspects of patients suffering from snakebites at a referral hospital in the Western Amazon region, Brazil.
METHODS
This is a cross-sectional, retrospective and documentary study of quantitative approach, from 2015 to 2016, conducted at the Juruá Regional Hospital, a reference in the emergency care of the city of Cruzeiro do Sul, Acre, Brazil, located in the northwest of Brazil and the region known as the Western Amazon15.
Epidemiological data were obtained from SINAN records in the Epidemiological Surveillance Department of the Juruá Regional Hospital. The following variables were verified: month of occurrence, snake identification (type of accident), accident location (urban and rural), locality, municipality, victim data (age group, sex, anatomical region affected), symptoms and signs circumstances of the accident, time elapsed between accident and care, number of ampoules used, and type of serum.
The morbidity coefficient (cases/100,000 inhabitants) was calculated by dividing the number of people who suffered snakebite accidents by the number of inhabitants of the municipality during the study period16. Rainfall data were obtained from the Cruzeiro do Sul Meteorological Station of the National Institute of Meteorology (INMET). To verify a possible relationship between the number of monthly snakebite accidents with rainfall, the Spearman correlation test was used17.
The study complied with the ethical precepts involving research with human beings, obtaining approval from the Ethics Committee on Research with Human Beings of the Dr. Heitor Vieira Dourado Foundation for Tropical Medicine, under opinion No. 2.084.630.
RESULTS
From 2015 to 2016, 248 patients who were victims of snakebite were treated, with an average of 124 annual cases and a morbidity coefficient of 76.71 cases per 100,000 inhabitants for the Alto Juruá region.
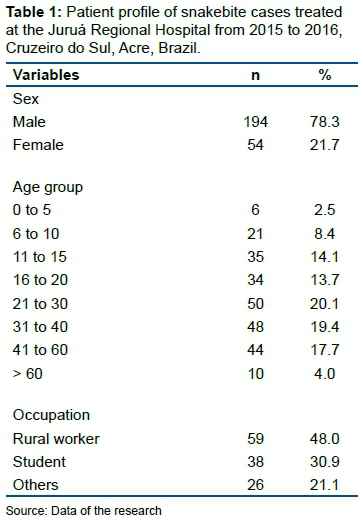
Most accidents occurred in males (78.3%) and aged between 21 and 60 years (57.2%). Children under 15 accounted for 25% of victims. Regarding occupation, the majority (48%) of the accidents occurred in rural workers (Table 1).
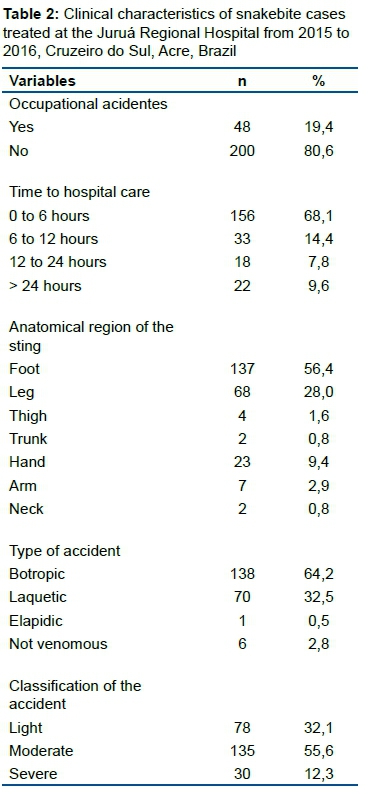
Forty-eight cases (19.4%) were considered occupational accidents. The main anatomical region in which the bite occurred was the foot (56.4% of cases), followed by the leg (28%). The time elapsed between the accident and hospital care was mostly (68.1% of cases) in less than six hours. Of the records where the causative snake was filled (215 cases; 87%), most accidents were considered botropic (64.2%), followed by laquetic (32.5%), non-venomous snakes (2.8%) and a case of elapid poisoning (Table 2).
The municipality with the highest number of cases attended was Cruzeiro do Sul (159 cases), followed by Rodrigues Alves (32), Mâncio Lima (19), Marechal Thaumaturgo (12), Tarauacá (11), Guajará (AM - 9), Porto Walter (4), Feijó (1) e Atalaia do Norte (AM - 1) (Figure 1). The municipalities of the state of Amazonas described here do not enter the study quantity, are only shown to have been referred for care at the Juruá Hospital in Cruzeiro do Sul - AC (Figure 1).
Regarding the area of occurrence, the majority (85%) occurred in the rural area. Regarding the data in relation to the place where the accident occurred, in 148 cases the information was obtained, and the accidents occurred mostly in trails, woods and meadows, according to Table 3.
There was a correlation between snakebite accidents and monthly rainfall (r=0.58444; p=0.00271; n=24) (Figure 2), and a larger number of cases (57.6%) were observed during the period of highest rainfall (1,854 mm) between November and April and a smaller number of cases during the three driest months (June to August).
Of the six cases attributed to non-venomous snakes during 2016, four occurred in urban areas, where the symptoms presented were pain (100%), edema (83.3%) and bleeding (16.6%). Three patients reported the accident-causing snake as surucucu and two as jararaca, regional popular names given to Bothrops atrox, and one to papagaia (B. bilineatus) (Figure 3 and Board 1).
The most frequent symptoms and signs in patients were pain (97.1%) and edema (92.7%), followed by hemorrhage (16.1%), vagal signs (8%), bruising (2.07%) and necrosis (1.6%) (Figure 4).
The Blood Coagulation Test (CT) was performed in 155 (62.5%) of the 248 patients, and the coagulation time changed in 57 (37.1%) of the cases.
In two patients (0.8%) there were complications of renal failure and in other five (2%), compartment syndrome, requiring fasciotomy. Secondary infection was reported for one patient (0.4%).
Seven of these eight patients who had complications were seen 24 hours after poisoning. One elderly patient treated four days after the accident died (0.4% lethality).
Patients with ophidian accidents remained in the hospital for 1 to 15 days, with an average of 4.5 days per patient.
DISCUSSION
The annual average of accidents treated at the Juruá Regional Hospital between 2015 and 2016 was higher than that reported by Bernarde and Gomes11 during the period from August 2007 to July 2009 at the same location. The morbidity coefficient of snakebite accidents recorded in this study for the Upper Juruá region was also higher than the period studied by Bernarde and Gomes11 (67.01 cases per 100,000 inhabitants/year) and for the state of Amazonas (52 8 cases per 100,000 inhabitants/year), where in some municipalities they exceed more than 150 cases per 100,000 inhabitants per year4.
The data evidenced in the study corroborate with the results of several studies found in the literature in countries such as Morocco, India and Kenya where they show the frequency of men, rural workers and young age group with an average age of 26 years18-20.
However, in a study conducted in the United States by Spyres et al.21, most accidents affected landscapers and mainly upper limb bites, differing from the reality of other regions of the world, such as Latin America and Asia, which are predominant of snakebite accidents on farmers who were bitten in the lower limbs22.
In other studies conducted in the Amazon2,4,23, most snakebite accidents also occurred in rural areas with adult male individuals and rural workers, biting in the lower limbs.
These findings can be explained by the exposure that the male and rural public presents more outdoor work activities, as well as agricultural work, especially in the Brazilian Amazon region, which has much agricultural work due to its immense forestry19.
Although there was a high number in farmers, it is worth mentioning the high percentage of accidents with students. Moreno et al.2 identified some vulnerability to snakebite accidents in this group, as many in rural areas travel long distances between their homes and schools, passing through areas that have snakes, such as trails, woods and streams.
Most of the occurrence of bites occurred in rural areas, with locations distributed in trails, woods and meadows, a result that is also widely highlighted and discussed in research20,24, especially in periods with high monthly rainfall.
The variety of places where the accidents occurred (woods, meadows, aquatic environments and backyards) denotes the diversity of habitats in which the main poisonous snake in the region occurs, the Bothrops atrox, which is the most abundant of venom, being present in forests, rural areas and even in urban areas11,25.
As observed by Bernarde and Gomes11, the correlation between snakebite accidents and high rainfall is probably due to the greater activity of snakes in this period14,25 and also the flooding of rivers, which makes snakes look for drier areas on dry land, and certain agricultural and extractive practices at this time2,4,10, that increases the likelihood of encounter between these animals and people.
In a study by Roriz et al.26 in the state of Rondônia, also located in the western Amazon region, the results are close to the present study, showing mainly the causes of snakebite snakebite accidents, as well as the bites in rural areas during periods of high rainfall from November to April.
Bernarde & Gomes11 observed that the majority of accidents (51%) were mistakenly recorded as laquetic which results were overestimated, including records of crotalic accidents, and the responsible gender (Crotalus) does not occur in the state of Acre.
In a recent study, the accidents recorded in the municipality of Tarauacá, composed by the majority (95.8%), followed by the laquetics (3.2%), were close to expected in the epidemiology of snakebite accidents in the state of Acre, where the Botropic envenoming is the most common, the laquetic is uncommon and the elapidic is rare27.
In this study, the majority of reported accidents were botropic (64.2%), while laquetic accounted for 32.5% of cases. Bernarde12 and Bernarde et al.28 show the importance of differentiation between species, but this does not happen, as few patients take the snake to the hospital, or make a photographic record of this species.
However, 17 patients took the snakes that had bitten them, and it was found that seven of them belonged to the species Bothrops atrox and ten to Helicops angulatus. Several authors affirm the importance of victims taking or photographing the snake that causes the accident, since it facilitates the diagnosis and therapy to be used11,28-30. Five patients bitten in the lower limbs (feet and legs) reported that the responsible snake had been Jararaca or Surucucu, popular names attributed to Bothrops atrox, the main poisoning species in Acre and the Brazilian Amazon, as well as in other Amazonian countries. And a patient bitten on the arm reported that the snake had been the Papagaia, a popular name given to Bothrops bilineatus, a tree species that is often found in some forests in this region.
Pain and edema are commonly the most frequent symptoms in snakebite accidents in general31 and also in the Amazon2,4,32, as shown in the study.
The predominance of these two symptoms may be associated with a higher classification of mild and moderate cases, as in these cases the expected signs and symptoms vary from stinging pain, edema, fever, malaise or minor rash. The patient receiving the anti-drug should undergo constant blood tests, as poison reactions can lead to multiple organ failure, even if they show few signs and symptoms33-35.
In more severe cases, the snakebite can lead to visual problems, major bleeding, intravascular coagulation, renal dysfunction, and various complications, depending on the species and location of the bite, and may lead to death if the dose of antifidic is not sufficient to combat the reaction31. In the study, the evolution of cases to necrosis, death, renal failure and compartment syndrome and altered coagulation time were few, however, observed in some studies in the Amazon region in Brazil, as well as in countries such as Colombia and Ecuador2,4,29,30,32. The Brazilian Ministry of Health recommends blood coagulation tests to aid diagnosis confirming snake envenoming and also to evaluate the success of venom neutralization by serotherapy1.
Also noteworthy is the time of treatment of the bite to the hospital, where patients who presented complications and death, the predominant majority were seen 24 hours after envenoming, showing that late care is a factor associated with the onset of complications and death9,23,36.
The study by Mitra et al.37 conducted in rural northern India reinforces this hypothesis, where it was found that mortality was significantly lower among those who were seen within five hours after the bite.
Although the average number of cases attended in less than six hours was similar to other studies conducted in the Amazon region2,26,36, there is a great divergence with the southern and southeastern regions of the country, where respectively 88% and 94% of the victims can be met in less than six hours. This fact may be associated with the urbanization of regions, where access to health services in the above regions is easier3,6,38,39.
In addition, the delay in care in the Brazilian Amazon region is the distance from victims to hospital care, which usually depend on river or dirt roads in conditions of great difficulty2,23,26,36.
The study has limitations mainly in case reporting, which is still impaired due to the difficulties of access of the population to health services that are usually located in urban areas. Although the research was conducted in the hospital's own surveillance sector, the poor availability of data and records precludes further analysis that allows for greater understanding of the site, species of snake and other factors that may be determinant.
It was presented a constant increase in the cases, which generated a worrying point of reflection, which may be associated with two factors, where one turns to the improvement in the displacement of victims (improvements in the extension roads and implementation of SAMU speedboat) facilitating plus transport and telephone coverage improving communication, or failure of public health policies to provide better conditions and guidance to the population.
Collaborators
O.F. Câmara participated in the data analysis and the final writing of the article. D. D. Dilva and M. N Holanda guided and revised the data analysis. P. S. Bernarde, M.V.M Lima, L.C. de Abreu, A. M. da Silva, W. M. Monteiro and R. Wajnszteijn contributed to the writing and critical review of the article.
Acknowledgements
The viability of the article is due to the Acre - Health Project in the Western Amazon (multinstitutional agreement process no. 007/2015 SESACRE-UFAC-FMABC).
REFERENCES
1.Bernarde PS. Serpentes peçonhentas e acidentes ofídicos no Brasil. São Paulo: Anolis Books, 2014; p.224. [ Links ]
2.Moreno E, Queiroz-Andrade M, Lira-da-Silva RM, Tavares-Neto J. Caracteristicas clinicoepidemiologicas dos acidentes ofidicos em Rio Branco, Acre. Rev Soc Bras Med Trop. 2005;38(1):15-21. DOI: http://dx.doi.org/10.1590/S0037-86822005000100004 [ Links ]
3.Oliveira RJ, Kirchner RM, Scherer ME, Santos ER, Eidelwein LPS. Perfil epidemiológico de acidentes ofídicos no estado do Rio Grande do Sul no período de 2007 a 2013. Enciclop Biosf. 2015;11(22):3074-83. DOI: http://dx.doi.org/10.18677/Enciclopedia_Biosfera_2015_024 [ Links ]
4.Feitosa EL, Sampaio VS, Salinas JL, Queiroz AM, Silva IM, Gomes AA, et al. Older age and time to medical assistance are associated with severity and mortality of snakebites in the Brazilian Amazon: A case-control study. PLoS One. 2015;10(7): e0132237. DOI: http://dx.doi.org/10.1371/journal.pone.0132237 [ Links ]
5.Pierini SV, Warrell DA, Paulo A, Theakston RDG. High incidence of bites and stings by snakes and other animals among rubber tappers and Amazonian Indians of the Jurua valley, acre state, Brazil. Toxicon. 1996;34(2):225-36. DOI: http://dx.doi.org/10.1016/0041-0101(95)00125-5 [ Links ]
6.Lima JS, Martelli Júnior H, Martelli DRB, Silva MS, Carvalho SFG, Canela JR, et al. Perfil dos acidentes ofídicos no norte do Estado de Minas Gerais, Brasil. Rev Soc Bras Med Trop. 2009;42(5):561-4. DOI: http://dx.doi.org/10.1590/S0037-86822009000500015 [ Links ]
7.Wen FH, Monteiro WM, Silva AMM, Tambourgi DV, Silva IM, Sampaio VS, et al. Snakebites and Scorpion Stings in the Brazilian Amazon: Identifying Research Priorities for a Largely Neglected Problem. PLoS Negl Trop Dis. 2015;9(5):e0003701. DOI: http://dx.doi.org/10.1371/journal.pntd.0003701 [ Links ]
8.Bochner R, Fiszon JT, Machado C. A Profile of Snake Bites in Brazil, 2001 to 2012. J Clin Toxicol. 2014;4(3):100-94. DOI: http://dx.doi.org/10.4172/2161-0495.1000194 [ Links ]
9.Ribeiro LA, Albuquerque MJ, Campos VAFP, Katz G, Takaoka NY, Lebrão ML, et al. Óbitos por serpentes peçonhentas no Estado de São Paulo: avaliação de 43 casos, 1988/93. Rev Assoc Médica Bras. 1998;44(4):312-8. DOI: http://dx.doi.org/10.1590/S0104-42301998000400010 [ Links ]
10.Waldez F, Vogt RC. Aspectos ecológicos e epidemiológicos de acidentes ofídicos em comunidades ribeirinhas do baixo rio Purus, Amazonas, Brasil. Acta Amaz. 2009;39(3):681-92. DOI: http://dx.doi.org/10.1590/S0044-59672009000300025 [ Links ]
11.Bernarde PS, Gomes JO. Serpentes peçonhentas e ofidismo em Cruzeiro do Sul, Alto Juruá, Estado do Acre, Brasil. Acta Amaz. 2012;42(1):65-72. DOI: http://dx.doi.org/10.1590/S0044-59672012000100008 [ Links ]
12.Bernarde PS. Serpentes peçonhentas e acidentes ofídicos no Acre. Curitiba: Anolis Books, 2012. [ Links ]
13.Campbell JA, Lamar WW. The venomous reptiles of the Western Hemisphere. Ithaca: Cornell University Press, 2004. [ Links ]
14.Oliveira ME, Martins M. When ans where to find a pitviper: activity patterns and habitat use of the lancehead, bothrops atrox, in central amazonia, Brazil. Herpetol Nat Hist. 2001;8(2):101-10. [ Links ]
15.Acre. Governo do Estado. Programa Estadual de Zoneamento Ecológico-Econômico do Estado do Acre. Zoneamento ecológico-econômico do Acre fase II: documento síntese. Rio Branco: Secretaria de Estado de Planejamento e Desenvolvimento Econômico Sustentável, 2006. [ Links ]
16.Intitutudo Brasileiro de Geodrafia e Estatística (IBGE). Censo demográfico. 2017 [ Links ]
17.SAS Institute. JMP. Version 10. (1989 - 2013). Cary, NC: 2013. [ Links ]
18.El hattimy F, Chafiq F, Hami H, Mokhtari A, Soulaymani A, Rachida SB. Geographical distribution of health indicators related to snake bites and envenomation in Morocco between 1999 and 2013. Epidemiol Health. 2018;40: e2018024. DOI: http://dx.doi.org/10.4178/epih.e2018024 [ Links ]
19.Kumar KS, Narayanan S, Udayabhaskaran V, Thulaseedharan NK. Clinical and epidemiologic profile and predictors of outcome of poisonous snake bites - an analysis of 1,500 cases from a tertiary care center in Malabar, North Kerala, India. Int J Gen Med. 2018;11:209-16. DOI: http://dx.doi.org/10.2147/IJGM.S136153 [ Links ]
20.Ochola FO, Okumu MO, Muchemi GM, Mbaria JM, Gikunju JK. Epidemiology of snake bites in selected areas of Kenya. Pan Afr Med J. 2018;29:217. DOI: http://dx.doi.org/10.11604/pamj.2018.29.217.15366 [ Links ]
21.Spyres MB, Ruha AM, Seifert S, Onisko N, Padilla-Jones A, Smith EA. Occupational Snake Bites: a Prospective Case Series of Patients Reported to the ToxIC North American Snakebite Registry. J Med Toxicol. 2016;12(4):365-9. DOI: http://dx.doi.org/10.1007/s13181-016-0555-7 [ Links ]
22.Bhalla G, Mhaskar D, Agarwal A. Clinical profile of snake bite at a tertiary care centre. Toxicol Int. 2014;21(2):203-8. DOI: http://dx.doi.org/10.4103/0971-6580.139811 [ Links ]
23.Borges CC, Sadahiro M, Santos MC. Aspectos epidemiológicos e clínicos dos acidentes ofídicos ocorridos nos municípios do Estado do Amazonas. Rev Soc Bras Med Trop. 2018;32(6):637-46. DOI: http://dx.doi.org/10.1590/S0037-86821999000600005 [ Links ]
24.Yañez-Arenas C, Yañez-Arenas A, Martínez-Ortíz D. Panorama epidemiológico de las mordeduras por serpiente venenosa en el estado de Yucatán, México (2003-2012). Gac Med Mex. 2016;152(4):568-74. [ Links ]
25.Turci LCB, Albuquerque S, Bernarde PS, Miranda DB. Uso do hábitat, atividade e comportamento de Bothriopsis bilineatus e de Bothrops atrox (Serpentes: Viperidae) na floresta do Rio Moa, Acre, Brasil. Biota Neotrop. 2009;9(3):197-206. DOI: http://dx.doi.org/10.1590/S1676-06032009000300020 [ Links ]
26.Roriz KRPS, Zaqueo KD, Setubal SS, Katsuragawa TH, Silva RR, Fernandes CFC, et al. Epidemiological study of snakebite cases in Brazilian western Amazonia. Rev Soc Bras Med Trop. 2018;51(3):338-46. DOI: http://dx.doi.org/10.1590/0037-8682-0489-2017 [ Links ]
27.Saboia CDO, Bernade PS. Snakebites in the Municipality of Tarauacá , Acre , West of the Brazilian Amazon. J Hum Growth Dev. 2019;29(1):290-7. DOI: http://dx.doi.org/10.7322/jhgd.157760 [ Links ]
28.Bernade PS, Mota-da-silva A, Abreu LC. Ofidismo no Estado do Acre - Brasil. J Amaz Heal Sci. 2015;1(2):44-63. [ Links ]
29.Otero R, Guti6rrez JM, Ntitiezl V, Robles A, Estrada R, Segura E, et al. A randomized double-blind clinical trial of two antivenoms in patients bitten by Bothrops atrox in Colombia and The Regional Group on Antivenom Therapy Research. Trans R Soc Trop Med Hyg. 1996;90(6):696-700. DOI: http://dx.doi.org/10.1016/s0035-9203(96)90442-3 [ Links ]
30.Smalligan R, Cole J, Brito N, Laing GD, Mertz BL, Manock S, et al. Crotaline snake bite in the Ecuadorian Amazon: randomised double blind comparative trial of three South American polyspecific antivenoms. BMJ. 2004;329(7475):1129. DOI: http://dx.doi.org/10.1136/bmj.329.7475.1129 [ Links ]
31.Hifumi T, Sakai A, Kondo Y, Yamamoto A, Morine N, Ato M, et al. Venomous snake bites: Clinical diagnosis and treatment. J Intensive Care. 2015;3(1):16. DOI: http://dx.doi.org/10.1186/s40560-015-0081-8 [ Links ]
32.Pardal PPO, Souza SM, Monteiro MR, Fan HW, Cardoso JL, França FO, et al. Clinical trial of two antivenoms for the treatment of Bothrops and Lachesis bites in the north eastern Amazon region of Brazil. Trans R Soc Trop Med Hyg. 2004;98(1):28-42. DOI: http://dx.doi.org/10.1016/s0035-9203(03)00005-1 [ Links ]
33.Lundquist AL, Chari RS, Wood JH, Miller GG, Schaefer HM, Raiford DS, et al. Serum sickness following rabbit antithymocyte-globulin induction in a liver transplant recipient: case report and literature review. Liver Transplant. 2007;13(5):647-50. DOI: http://dx.doi.org/10.1002/lt.21098 [ Links ]
34.Kanji S, Chant C. Allergic and hypersensitivity reactions in the intensive care unit. Crit Care Med. 2010;38(6 Suppl.):S162-8. DOI: http://dx.doi.org/10.1097/CCM.0b013e3181de0c99 [ Links ]
35.Boothpur R, Hardinger KL, Skelton RM, Lluka B, Koch MJ, Miller BW, et al. Serum sickness after treatment with rabbit antithymocyte globulin in a heart transplant recipient with previous rabbit exposure. Am J Kidney Dis. 2010;55(3):141-3. DOI: http://dx.doi.org/10.1053/j.ajkd.2009.06.017 [ Links ]
36.Feitosa ES, Sampaio V, Sachett J, Castro DB, Noronha MDN, Lozano JLL, et al. Snakebites as a largely neglected problem in the Brazilian Amazon: highlights of the epidemiological trends in the State of Amazonas. Rev Soc Bras Med Trop. 2015;48(Suppl I):34-41. DOI: http://dx.doi.org/10.1590/0037-8682-0105-2013 [ Links ]
37.Mitra S, Agarwal A, Shubhankar BU, Masih S, Krothapalli V, Lee BM, et al. Clinico-epidemiological profile of snake bites over 6-year period from a rural secondary care centre of Northern India: A descriptive study. Toxicol Int. 2015;22(1):77-82. DOI: http://dx.doi.org/10.4103/0971-6580.172263 [ Links ]
38.Ribeiro LA, Jorge MT, Iversson LB. Epidemiologia do acidente por serpentes peçonhentas: estudo de casos atendidos em 1988. Rev Saude Publica. 1995;29(5):380-8. DOI: http://dx.doi.org/10.1590/S0034-89101995000500007 [ Links ]
39.Machado C, Bochner R, Fiszon JT. Epidemiological profile of snakebites in Rio de Janeiro, Brazil, 2001-2006. J Venom Anim Toxins Incl Trop Dis. 2012;18(2):217-24. DOI: http://dx.doi.org/10.1590/S1678-91992012000200012 [ Links ]
 Correspondence:
Correspondence:
ozianndeny@hotmail.com
Manuscript received: August 2019
Manuscript accepted: February 2020
Version of record online: March 2020














