Servicios Personalizados
Articulo
Indicadores
Compartir
Journal of Human Growth and Development
versión impresa ISSN 0104-1282versión On-line ISSN 2175-3598
J. Hum. Growth Dev. vol.31 no.2 Santo André mayo/ago 2021
http://dx.doi.org/10.36311/jhgd.v31.12225
ORIGINAL ARTICLE
Motor performance evaluation of newborns with gastroschisis after surgical correction
Gislaine Aparecida de Oliveira MotaI; Glaucia Yuri ShimizuII; Ana Lucia Capelari LahozII; Carla Marques NicolauII; Lucia Cândida Soares de PaulaII; Maristela Trevisan CunhaII; Clarice TanakaIII
IFisioterapeuta do Programa de Residência Multiprofissional em Neonatologia do Instituto da Criança e do Adolescente do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo - São Paulo (SP), Brasil
IIFisioterapeuta do Instituto da Criança e do Adolescente do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo - São Paulo (SP), Brasil
IIIProfessora Titular Departamento de Fisioterapia, Fonoaudiologia e Terapia Ocupacional da Faculdade de Medicina da Universidade de São Paulo - São Paulo (SP), Brasil
ABSTRACT
INTRODUCTION: Gastroschisis is a congenital malformation that has risk factors for delayed neuropsychomotor development. That is why it is important to recognize early developmental changes in these newborns during hospitalization in the Neonatal Intensive Care Unit
OBJECTIVE: To evaluate the motor performance of newborns with gastroschisis after surgical correction
METHODS: An observational and retrospective study was carried out with newborns with gastroschisis, assessed by the Test of Infant Motor Performance at the Neonatal Intensive Care Center 2 of the Instituto da Criança e do Adolescente. The test allows the classification of the risk for developmental delay in 4 categories: within the average for age, low average, below average, and well below average. Maternal, neonatal, surgical, and motor assessment data were collected through electronic medical records
RESULTS: Motor assessment was performed on 17 newborns, where 88.23% were classified as "below average" for age. The mean maternal age was 20 years, and the average gestational age and birth weight were 36.38 weeks and 2343.9 grams, respectively, with the majority being female. Simple gastroschisis accounted for 64.71%, and primary closure was possible in 82.35%. The average hospital stay of 53.24 days, and sepsis was the most frequent complication (64.71%
CONCLUSION: Newborns with gastroschisis remain hospitalized for a long time and are susceptible to complications. It was possible to identify the delay in the development of these newborns early during hospitalization, which allows intervention by physiotherapy before the delay worsens
Keywords: gastroschisis, psychomotor performance, surgical procedures, risk factor, neonatal intensive care
Authors summary
Why was this study done?
The study was carried out to assess the motor performance of newborns with gastroschisis because it is a congenital malformation that has risk factors for delayed neuropsychomotor development. Early identification of developmental changes is important and necessary so that interventions can be performed even during the hospitalization period and before they become worse.
What did the researchers do and find?
Seventeen newborns were evaluated in the postoperative period of gastroschisis correction using the Test of Infant Motor Performance (TIMP). Developmental changes were found in more than 80% of the sample, classified as "below average" for age according to the normative test table.
What do these findings mean?
This study shows that newborns with gastroschisis have developmental changes in the neonatal period, and multidisciplinary monitoring is important. These discoveries enable physical therapy intervention even in the hospital environment in order to prevent changes in development from setting in or getting worse.
INTRODUCTION
The advancement of care in the neonatal intensive care unit (NICU) and surgical techniques not only increased the survival of newborns (NBs) with various malformations but also raised concerns about morbidities resulting from hospitalization, such as changes in neuropsychomotor development (DNPM). Approximately 2% to 3% of all newborns have congenital anomalies that require some surgical procedure1,2.
DNPM alteration is multifactorial, and conditions such as low birth weight, congenital malformations, need for surgical procedures, prolonged hospitalization, mechanical ventilation, use of supplemental oxygen1, pain, sedation, analgesia3, sepsis, and maternal characteristics4,5 can influence neurological development. In this context, gastroschisis is one of the most common malformations of the abdominal wall that requires intensive care and has risk factors for changes in the DNPM1,6.
Gastroschisis is a congenital defect usually located in the right paraumbilical region, characterized by protrusion of abdominal organs during fetal development, exposing the viscera to amniotic fluid. Its prevalence is approximately 2.98 per 10,000 live births and can be classified as simple when only the exteriorization of Organs abdominal organs occurs without the association of other changes and complex when there is the presence of intestinal atresia, perforation, necrotic segments, or intestinal volvulus7.
This defect is considered a surgical emergency, and it is possible to perform the primary correction when there is no disproportion between the size of the abdominal cavity and the number of externalized viscera, or it is opted to perform the staged reduction through the use of silo with late closure when not primary closure is possible4.
The incidence of delayed motor development in children with congenital heart disease is well reported, but there are few studies conducted with newborns who required surgery to correct non-cardiac abnormalities1,8,9. That is why it is important to monitor these children and early identify risk factors and changes in development through their own assessment tools5.
According to the American Academy of Pediatrics, instruments for assessing and monitoring development help to identify children at risk and to carry out intervention measures with the intention of reducing the risk of developmental delay5. The Test of Infant Motor Performance (TIMP) is a translated and recently validated instrument for the Brazilian population, developed to assess postural motor control and motor performance of newborns at risk for functional activities and can be applied from 34 weeks up to 4 months of corrected gestational age, allowing its use in the NICU10,11.
The early recognition of changes in the DNPM even during hospitalization allows physiotherapy to perform interventions before the delay worsens, avoiding abnormal postural patterns and impairing coordination and functionality. The investigation of the motor performance of surgical NBs is scarce, as well as the use of TIMP in this population.
Due to the fact that it is a reference center in the correction of congenital abdominal malformations, the aim of the study is to analyze the motor performance of newborns with gastroschisis after surgical correction.
METHODS
An observational and retrospective study was carried out, comprising 17 newborns diagnosed with gastroschisis, who were evaluated by TIMP at the Centro de Tratamento Intensivo Neonatal do Instituto da Criança e do Adolescente do Hospital das Clínicas de São Paulo (Neonatal Intensive Care Center of the Institute of Children and Adolescents of the Hospital das Clínicas de São Paulo/HC-FMUSP), between January 2017 to August 2018.
Maternal, neonatal, surgical data, duration of ventilatory support, length of stay, main complications and morbidities, motor assessment data by TIMP, and patient outcome through electronic medical records were collected, creating a database in the Microsoft program® Excel (2013) for data tabulation.
To assess motor performance, TIMP was performed by a trained physiotherapist after surgical correction and clinical stabilization of the newborn. According to the TIMP normative table, newborns were classified as "within average", "low average", "below average," or "far below average" for the corrected age after obtaining the Z score.
Inclusion criteria: Premature newborns (PTNB) and terms, with corrected gestational age from 34 weeks to 4 months, diagnosed with gastroschisis after surgical correction, who were clinically stable on spontaneous breathing in room air or a low nasal flow (oxygen flow up to 1 L/min) catheter were included.
Exclusion criteria: NBs who were not submitted to TIMP evaluation due to hospital discharge, who had genetic syndromes, or who died.
Descriptive analysis was presented as mean, standard deviation and median. Nominal data were described in terms of percentages and proportions.
This research was approved by the Research Ethics Committee with Human Beings of the Faculty of Medicine of the University of São Paulo - FMUSP, with opinion number 2,780,324 in 2018.
RESULTS
During the study period, from January 2017 to August 2018, 25 newborns diagnosed with gastroschisis were admitted. Of the 25, five were excluded due to death, one with Moebius syndrome and two due to discharge before the test was applied. The TIMP motor assessment was performed in 17 newborns.
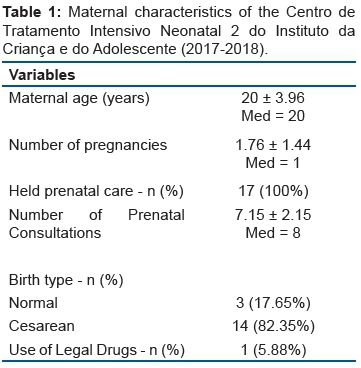
The mean maternal age was 20 ± 3.96 years, and all of them underwent prenatal care, with a predominance of cesarean delivery representing 82.35%. Regarding maternal education, only one completed higher education, with 41.18% of those having completed high school, as shown in table 1.
The mean gestational age and birth weight were 36.38 ± 2.13 weeks and 2343.9 ± 501.89 grams, respectively, with the majority of females, corresponding to 64.71% (table 2).
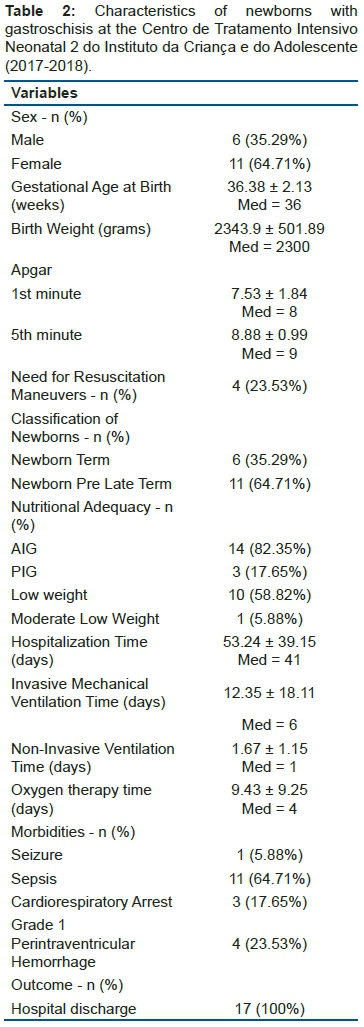
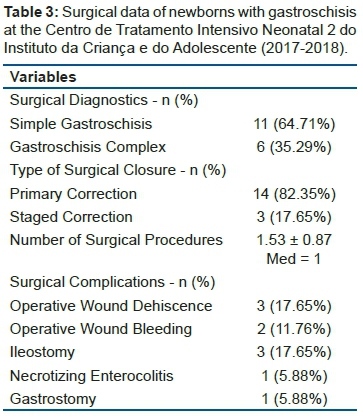
Of the 17 newborns evaluated, 64.71% had simple gastroschisis, and primary closure was possible in 82.35% of the newborns (table 3).
All NBs were intubated for the procedure, and the average duration of invasive mechanical ventilation was 12.35 ± 18.11 days, the average oxygen therapy time was 9.43 ± 9.25 days, and the average hospital stay was 53.24 ± 39.15 days. As for neonatal morbidities, 64.71% NB developed sepsis, and 23.53% had grade 1 perintraventricular hemorrhage (table 2).
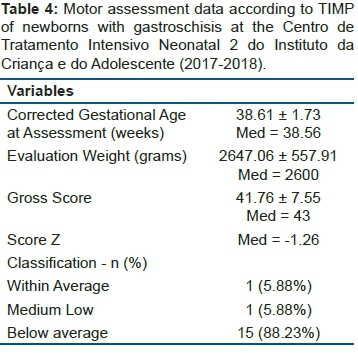
Regarding motor performance, the mean corrected gestational age in the evaluation was 38.61 ± 1.73 weeks, and 88.23% of the newborns were classified according to TIMP as "below average" according to table 4.
DISCUSSION
The characterization of newborns admitted to the NICU who need surgical procedures to correct gastroschisis is necessary for physiotherapists and other health professionals to recognize the main risk factors for changes in the DNPM and to intervene early in this population, in order to prevent the changes settle and get worse.
The assessment and monitoring of the DNPM of newborns with gastroschisis become a concern as its prevalence increases, although the cause is not fully understood. Some authors associate the increased incidence of the disease with maternal age below 20 years, smoking, use of illicit drugs during pregnancy, placental insufficiency, genetic, dietary factors, and exposure to chemicals12. Calderon et al. demonstrated in their recent population study carried out in the state of São Paulo-Brazil between the periods from 2005 to 2016 that the annual prevalence of gastroschisis increased by 2.6%13.
NB with gastroschisis are predisposed to late preterm delivery and low birth weight, as demonstrated in the retrospective multicenter observational study by Raymond et al., involving 566 NBs with gastroschisis, in accordance with the results obtained in our study14. Late PTNBs present changes in motor performance that are evident in the long term15.
In 2015 Trivedi et al. evaluated the impact of non-cardiac surgeries on the development of late preterm NBs, composed mostly of NBs with gastroschisis, and found that this population represents a risk for delay in the DNPM, suggesting that they are accompanied by a multidisciplinary team6.
The association of gastroschisis with other complications, such as atresia, perforation, necrosis, and intestinal volvulus, increases its complexity and can prolong the hospital stay and favor the occurrence of complications12. In surgical patients, infections are frequent complications and, therefore, a reason of concern16.
Even with the improvement in neonatal intensive care, sepsis is still among the main causes of neonatal morbidity and mortality, associated with longer hospital stays and hospital costs12,16-18. Neonatal sepsis, in addition to being a risk for delayed motor development, is associated with the incidence of cerebral palsy and high mortality16,18. In our study, sepsis was also the complication with the highest incidence.
NB undergoing surgical procedures present several risks. In addition to sepsis, they are exposed to other situations that may influence neurological development, such as the need for mechanical lung ventilation, use of sedatives and anesthetics, difficulty in controlling pain, difficulty in progressing the diet with the use of prolonged parenteral nutrition, and frequently changes in DNPM will be evident in the long run12,19,20.
Few studies analyze the possible alterations in the neurological development of children with gastroschisis, and, when performed, most are with children in school. In this period, deficits are more evident since greater cognitive demands are necessary20.
In 2017 Lap et al.21 found that school-age children who underwent gastroschisis correction in the neonatal period were associated with poor linguistic and verbal intelligence, with an increased risk for poor performance in different aspects of attention, inhibitory behavior, and fine motor skills when compared to their controls21. In this sense, it can be beneficial to monitor the DNPM of children with gastroschisis before school so that future academic performance is possible22.
In short to medium term, the congenital defect and the need for abdominal surgery can interfere with the performance of the abdominal muscles and postural control, and generate losses in the gross motor function in the first year of life, with difficulties in the acquisition of skills dependent on the activity of this musculature, such as the prone position, in rolling, crawling and sitting. Muscle tone changes were observed in the study by So et al.23, which demonstrated a reduction in muscle tone and impact on the acquisition of motor skills of these children. Abnormal general movements and poor performance were also observed, mainly in the assessment of gross motor function, associated with motor and cognitive delays in 88% of infants with gastroschisis23.
In our study, we showed that newborns assessed during hospitalization, with a mean corrected gestational age of 38.6 weeks, were found to have changes in motor performance and were classified as "below average" for their age, according to TIMP. TIMP is a tool developed for the evaluation of newborns and infants at risk for delay and is suitable for use by professionals trained and familiar with child development, in a hospital environment, in nurseries, and intensive care units24.
The early identification of developmental changes allows these newborns to be followed both in the hospital environment and after discharge and referred to multi-professional services, enabling the appropriate treatment since they are vulnerable to changes in the DNPM, which may be noticed in the future19.
It is important to highlight some limitations of the study. As this is an observational and retrospective study with the data collected through medical records, we are sometimes faced with a lack of information. The comparison of our findings, especially with regard to motor assessment, was not possible due to methodological differences.
No studies have been found to assess the motor performance of newborns with gastroschisis through TIMP while still in the NICU since most of the studies on the assessment of the DNPM of these children are for follow-up. The evaluation carried out in different periods of the DNPM, with children of different ages, makes it impossible to use the same tool between studies and consequently the comparison. This was a retrospective characterization study, and we believe it is important to conduct prospective studies with a control group for a more reliable assessment of the impact of the malformation on newborns.
NB with gastroschisis remain hospitalized for a long time in neonatal intensive care units and are susceptible to complications and delay in the DNPM. Therefore they need evaluation, early intervention, and follow-up by physiotherapy and the multidisciplinary team. It was possible to early identify the delay in the development of newborns with gastroschisis during hospitalization, using a validated scale for evaluation in premature newborns up to 4-month-old infants, which allows intervention by physical therapy before the delay gets worse.
There are no studies in the literature that assess the motor performance of newborns in the postoperative period of gastroschisis correction during hospitalization in the NICU. This study shows that these newborns have developmental changes in the neonatal period, and multidisciplinary monitoring is important. These discoveries enable physical therapy intervention even in the hospital environment in order to prevent changes in development from setting in or getting worse.
Abbreviations
NICU: Neonatal Intensive Care Unit
NB: Newborns
DNPM: Neuropsychomotor Development
TIMP: Test of Infant Motor Performance
HC-FMUSP: Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo
PTNB: Premature newborns
Orcid authors
Gislaine Aparecida de Oliveira Mota https://orcid.org/0000-0003-1271-7722
Glaucia Yuri Shimizu https://orcid.org/0000-0002-8440-7961
Ana Lucia Capelari Lahoz https://orcid.org/0000-0003-0220-6574
Carla Marques Nicolau https://orcid.org/0000-0001-5627-3751
Lucia Cândida Soares de Paula https://orcid.org/0000-0003-4460-3551
Maristela Trevisan Cunha https://orcid.org/0000-0001-8169-8778
Clarice Tanaka https://orcid.org/0000-0003-3900-5944
REFERENCES
1.Stolwijk LJ, Lemmers PM, Harmsen M, Groenendaal F, Vries LS de, Zee DC van der, et al. Neurodevelopmental outcomes after neonatal surgery for major noncardiac anomalies. Pediatrics [Internet]. 1o de fevereiro de 2016 [citado 27 de maio de 2021]; 137 (2). Disponível em: https://pediatrics.aappublications.org/content/137/2/e20151728 [ Links ]
2.Minutillo C, Rao SC, Pirie S, McMichael J, Dickinson JE. Growth and developmental outcomes of infants with gastroschisis at one year of age: A retrospective study. Journal of Pediatric Surgery. agosto de 2013; 48 (8): 1688-96. [ Links ]
3.McPherson C, Grunau RE. Neonatal pain control and neurologic effects of anesthetics and sedatives in preterm infants. Clinics in Perinatology. março de 2014; 41 (1): 209-27. [ Links ]
4.van Manen M, Hendson L, Wiley M, Evans M, Taghaddos S, Dinu I. Early childhood outcomes of infants born with gastroschisis. Journal of Pediatric Surgery. agosto de 2013; 48 (8): 1682-7. [ Links ]
5.de Moura DR, Costa JC, Santos IS, Barros AJD, Matijasevich A, Halpern R, et al. Risk factors for suspected developmental delay at age 2 years in a Brazilian birth cohort. Paediatric and Perinatal Epidemiology. maio de 2010; 24 (3): 211-21. [ Links ]
6.Trivedi A, Walker K, Loughran-Fowlds A, Halliday R, J. A. Holland A, Badawi N. The impact of surgery on the developmental status of late preterm infants - a cohort study. J Neonatal Surg [Internet]. 10 de janeiro de 2015 [citado 27 de maio de 2021]; 4 (1). Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4420401/ [ Links ]
7.Bergholz R, Boettcher M, Reinshagen K, Wenke K. Complex gastroschisis is a different entity to simple gastroschisis affecting morbidity and mortality-A systematic review and meta-analysis. Journal of Pediatric Surgery. outubro de 2014; 49 (10): 1527-32. [ Links ]
8.Gischler SJ, Mazer P, Duivenvoorden HJ, van Dijk M, Bax NMA, Hazebroek FWJ, et al. Interdisciplinary structural follow-up of surgical newborns: a prospective evaluation. Journal of Pediatric Surgery. julho de 2009; 44 (7): 1382-9. [ Links ]
9.Laing S, Walker K, Ungerer J, Badawi N, Spence K. Early development of children with major birth defects requiring newborn surgery: Development of children with birth defects. Journal of Paediatrics and Child Health. março de 2011; 47 (3): 140-7. [ Links ]
10.Campbell SK, Zawacki L, Rankin KM, Yoder JC, Shapiro N, Li Z, et al. Concurrent validity of the TIMP and the Bayley III scales at 6 weeks corrected age. Pediatr Phys Ther. 2013; 25 (4): 395-401. [ Links ]
11.Chiquetti EMDS, Valentini NC, Saccani R. Validation and reliability of the test of infant motor performance for brazilian infants. Phys Occup Ther Pediatr. 2020; 40 (4): 470-85. [ Links ]
12.Redondo AC, Feferbaum R, Vieira RA, Moreira D de AR, Tannuri U, Carvalho WB de, et al. Characteristics of the clinical development of a newborn with gastroschisis in an intensive care unit in latin america. J Hum Growth Dev. 29 de agosto de 2016; 26 (2): 190-8. [ Links ]
13.Calderon MG, Santos EF de S, Abreu LC de, Raimundo RD. Increasing prevalence, time trend and seasonality of gastroschisis in São Paulo state, Brazil, 2005-2016. Scientific Reports. 10 de outubro de 2019; 9 (1): 14491. [ Links ]
14.Raymond SL, Hawkins RB, St Peter SD, Downard CD, Qureshi FG, Renaud E, et al. Predicting morbidity and mortality in neonates born with gastroschisis. J Surg Res. janeiro de 2020; 245: 217-24. [ Links ]
15.The long-term neurodevelopmental and psychological outcomes of gastroschisis: A cohort study. Journal of Pediatric Surgery. 1o de abril de 2016; 51 (4): 549-53. [ Links ]
16.Ferreira RC, Mello RR, Silva KS. Neonatal sepsis as a risk factor for neurodevelopmental changes in preterm infants with very low birth weight. J Pediatr (Rio J). junho de 2014; 90 (3): 293-9. [ Links ]
17.Uribe-Leitz M, McCracken CE, Heiss KF, Wulkan ML, Raval MV. The influence of infectious complications in gastroschisis on costs and length of stay. American journal of perinatology. 1o de janeiro de 2017; 34 (1): 62-9. [ Links ]
18.Carvalho NS, Helfer TM, Serni P de O, Terasaka OA, Boute T, Araujo Junior E, et al. Postnatal outcomes of infants with gastroschisis: a 5-year follow-up in a tertiary referral center in Brazil. Journal Of Maternal-Fetal & Neonatal Medicine [Internet]. 2016 [citado 27 de maio de 2021]; Disponível em: https://repositorio.unifesp.br/handle/11600/58532 [ Links ]
19.Burnett AC, Gunn JK, Hutchinson EA, Moran MM, Kelly LM, Sevil UC, et al. Cognition and behaviour in children with congenital abdominal wall defects. Early Hum Dev. janeiro de 2018; 116: 47-52. [ Links ]
20.Giúdici L, Bokser VS, Maricic MA, Golombek SG, Ferrario CC. Babies born with gastroschisis and followed up to the age of six years faced long-term morbidity and impairments. Acta Paediatrica. 2016; 105 (6): e275-80. [ Links ]
21.Functional outcome at school age of children born with gastroschisis. Early Human Development. 1o de março de 2017; 106-107: 47-52. [ Links ]
22.Suominen J, Rintala R. Medium and long-term outcomes of gastroschisis. Seminars in Pediatric Surgery. outubro de 2018; 27 (5): 327-9. [ Links ]
23.Early neurodevelopmental outcomes of infants with intestinal failure. Early Human Development. 1o de outubro de 2016; 101: 11-6. [ Links ]
24.Herrero D, Gonçalves H, Siqueira AAF de, Abreu LC de. Escalas de desenvolvimento motor em lactentes:test of infant motor performance e aalberta infant motor scale. J Hum Growth Dev. 1o de abril de 2011; 21 (1): 122-32. [ Links ]
 Correspondence:
Correspondence:
Gislaine Aparecida de Oliveira Mota
gislaine_olivermota@hotmail.com
Manuscript received: March 2021
Manuscript accepted: May 2021
Version of record online: July 2021











 texto en
texto en 


