Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Journal of Human Growth and Development
versão impressa ISSN 0104-1282versão On-line ISSN 2175-3598
J. Hum. Growth Dev. vol.31 no.3 Santo André set,/dez. 2021
https://doi.org/10.36311/jhgd.v31.12604
ORIGINAL ARTICLE
DOI: 10.36311/jhgd.v31.12604
COVID-19 fear scale - translation and validation into Brazilian portuguese
Marcella Moreira AguiarI; Monalisa Nascimento dos Santos BarrosII; Antonio MacedoIII; Maria Inês Rosselli PucciaIV; Ana Telma PereiraV
IFederal University of Bahia (UFBA), Vitória da Conquista, Bahia. Student at the Master of Health Psychology at the Federal University of Bahia
IIState University of Southwest Bahia (UESB), Department of Natural Sciences - Vitória da Conquista, Bahia. University of Coimbra, Coimbra, Portugal. Postdoctoral student at the Institute of Medical Psychology of the University of Coimbra. Adjunct Professor of Medicine and Psychology at the State University of Southwest Bahia. PhD in Psychology
IIIUniversity of Coimbra, Portugal. Director of the Institute of Medical Psychology; Full Professor at the Faculty of Medicine of the University of Coimbra. Doctor of Medicine
IVFMABC University Center, Santo André, São Paulo. Assistant professor. PhD in Sciences
VUniversity of Coimbra, Portugal. Assistant Researcher at the Institute of Medical Psychology of the Faculty of Medicine of the University of Coimbra. PhD in Health Sciences
ABSTRACT
INTRODUCTION: fear is one of the main factors associated with psychopathological disorders evidenced in the context of the COVID-19 pandemic.
OBJECTIVE: translate and validate Fear of COVID-19 Scale (FCV-19S) into Portuguese Brazilian version, named Covid-19 Fear Scale (EMC-19).
METHODS: cross-sectional study with 364 individuals recruited through social networks, considering as inclusion criteria: being over 18 years old and fluent in Portuguese. After participant consentment an electronic form was completed, which included the preliminary Portuguese version and EMC-19, in addition to sociodemographic variables. Data processing was performed using the SPSS 26 version. For parametric measures, Pearson's coefficient and Student's T were used, and for non-parametric measures the U of Mann Whitney. The magnitude of the correlation coefficients was classified according to Cohen's criteria and the confirmatory factor analysis using AMOS 26.0. For internal consistency, Cronbach's alpha.
RESULTS: mean age of 33.11 years (±10,047), most of them female (n=332; 91,2%), with higher education (n=286; 78,6%), married (n=225, 61,8 %) and with children (n=300, 82,4%). Exploratory factorial analysis/EFA and confirmatory factor analysis/CFA made. Only one component emerged from the CFA, with an explained variance of 55,49%, resulting in a one-dimensional model with satisfactory adjustment indexes (X2/gl=2,135; RMSEA=0,061; CFI, TLI, GFI<0,095). Cronbach's alpha coefficient is 876.
CONCLUSIONS: the construct validity of the one-dimensional structure of the EMC-19 was demonstrated, as well as its good internal consistency.
Keywords: COVID-19, fear, psychometry, validation study.
Authors summary
Why was this study done?
It is essential to have a tool to measure the level at which fear of COVID-19 can affect individuals. The FCV-19S was developed at the beginning of the pandemic, precisely with this objective, having been translated into several languages and validated in several countries. This study aims to translate and validate the Portuguese version (from Brazil) of the FCV-19S, which is called the Covid-19 Fear Scale (EMC-19). After analyzing its main psychometric properties, such as validity and reliability, in addition to measuring, this scale can be used in clinical practice and in research, to better understand and intervene on the psychosocial repercussions of COVID-19. It will still be possible to carry out cross-cultural comparative studies between the different countries that have already translated and validated it. The knowledge produced in this way can help to promote health behaviors to prevent the impacts of COVID-19 on mental health, and to support public policies that are adequate to fight the pandemic.
What did the researchers do and find?
With the COVID Fear Scale validated for Brazil, it will be possible to carry out cross-cultural comparative studies between the different countries that have already translated and validated it. The knowledge produced in this way can help to promote health behaviors to prevent the impacts of COVID-19 on mental health, and to support public policies that are adequate to fight the pandemic.
What do these findings mean?
With the COVID Fear Scale validated for Brazil, it will be possible to carry out cross-cultural comparative studies between the different countries that have already translated and validated it. The knowledge produced in this way can help to promote health behaviors to prevent the impacts of COVID-19 on mental health, and to support public policies that are adequate to fight the pandemic.
INTRODUCTION
On March 11, 2020, the World Health Organization decreed the SARS-COV-2 virus pandemic, responsible for COVID-191. The first case in Brazil occurred on February 26, 2020, when the pandemic had already shown its expansion strength and lethality in China and in several countries in Asia and Europe.
In Brazil, although the pandemic arrived in late February, in mid March the inability of the federal government to manage epidemiological information was already evident, contributing to what has been called underreporting2.
After a year and a half of the pandemic, official information shows that Brazil accumulates more than 20 million notified cases of COVID-19 and surpassed the number of 570 thousand deaths from the disease, according to data from the Ministry of Health3. The country occupies fourth place in the world ranking of people affected by the pandemic4, still adding difficulties in implementing measures to contain the spread of the infection, in particular actions to immunize the population.
Despite all the sanitary measures adopted to control the dissemination of the coronavirus in the national territory, the psychosocial impact of the COVID-19 pandemic stands out, which, in its least relevant space among the adopted measures, represents a significant issue for the field of research and comprehensiveness of health care5.
According to Ornel et al.6, the repercussions of a global health crisis of this magnitude, from the perspective of mental health, can last for many years, even after the disease has been contained.
It is observed that, as the pandemic advances, several elements of significant importance for the installation of a crisis situation from the point of view of mental health were consolidated, considering both the individuals who were affected by COVID-19 , as for the general population7, 8.
Quarantine, physical distance, the risk of contamination, the increase in the number of deaths, including family members and close people, changes in the domestic and work routine, job loss, aggravated by loneliness, fear and grief, increase susceptibility to problems such as anxiety, posttraumatic stress disorder, panic syndrome, social isolation, among other disorders6, 8.
Crisis is understood, as defined by Slakieu, Mejía and López7, the state of disorganization produced by the impact of a life altering situation that exceeds people's usual capacity to face problems.
Efforts to respond to the crisis context require effective mental health resources to improve the quality of care, and reduce the global burden of mental disorders caused by missed opportunities for preventive actions and timely treatment, especially in developing countries9.
Discussing mental health in the face of COVID-19 and physical distancing, Galea, Merchant and Lurie10 warn that, as populations become physically and socially isolated, strategies must be used to plan the inevitability of loneliness and prevent its sequels.
The first systematic review and metaanalysis of the psychiatric consequences of coronavirus infection identified 72 independent studies, which provided data on acute psychiatric and neuropsychiatric characteristics and post coronavirus infection8.
Initially, the review suggests that most people do not suffer from any psychiatric disorder after coronavirus infection, and adds that to date, there is little to suggest that common neuropsychiatric complications, in addition to shortterm delirium, are a feature8. However, this review alerts physicians to the possibility of later development of depression, anxiety, fatigue, post-traumatic stress disorder and rarer neuropsychiatric syndromes8.
Thus, the increase in psychopathological disorders11,12 puts pressure on health systems to develop resources and rapid response strategies to deal with the COVID-19 pandemic. The imminent risk of successive "waves" of COVID-19, or the aggravation caused by the emergence of new variants of the coronavirus, further affect the mental health of individuals13.
In fact, in addition to the resurgence of the virus, in a few months, public health systems may have to face, simultaneously, the consequences of the pandemic on mental health14. Mental health problems (depression, stress, panic, anxiety, etc.) can, in more extreme situations, result in suicidal ideation, suicide attempts and actual occurrence of suicide15-16.
The most common repercussions for mental health, such as anxiety and depression, also tend to last longer, possibly six months after the end of the illness) and are associated with a higher prevalence of fear6, 17.
It should be noted that the dominant psychological aspect of the COVID-19 pandemic is fear. This constitutes a central emotional response to imminent threats, such as COVID-1918. Fear is defined gone as an unpleasant emotional state that is triggered by the perception of threatening stimuli19.
From an evolutionary perspective, this emotional response constitutes a basic component of the human experience, conceived as a shock emotion due to the perception of present and urgent danger that threatens the preservation of that individual; causing a series of physiological effects in the body, which make it capable of a defense reaction, such as escape20.
Thus, fear can be adaptive and determine the degree of protection and prevention to be adopted against the threat, as is the case with COVID-1919. On the other hand, when the intensity of fear is too intense or too weak, disproportionately to what the stimulus actually represents, maladaptive behaviors can be triggered, such as excessive exposure to the virus or paralysis in the face of the crisis, making access to resources difficult internal for coping19,20.
Increased fear can amplify the damage caused by the disease itself and can be directly associated with its transmission rate, as well as its morbidity and mortality18. The development of fear is not a strictly interindividual process, but the result of a complex interaction of biological, psychological and social factors, which can also lead to other psychosocial challenges, including stigmatization, discrimination and loss21.
With high levels of fear, individuals may not think clearly and rationally when reacting to COVID-19, resulting in irrational processing of information related to the pandemic22, which considerably increases suffering and psychosocial challenges21,23-25.
With regard to the motivating role of fear, there was a significant relationship between scores on the Fear of COVID-19 Scale (FCV-19S) and adherence to mitigation rules implemented in New Zealand26, namely compliance with the social distance of two meters and physical activity in outdoor places that can be easily accessed on foot. This finding is consistent with the results of Harper et al.26, who reported a positive correlation between FCV-19S scores and participants' perceptions of the degree to which various behaviors and practices were changed due to the pandemic (eg, hygiene, care of children and the elderly)26.
Effectively, it has been shown that high levels of fear, along with self efficacy, positively affect adaptive behavioral changes; low levels of fear and self efficacy were associated with the involvement of avoidant behaviors27.
Thus, it is essential to have a tool to measure the level at which fear of COVID-19 can affect individuals. The FCV-19S was developed at the beginning of the pandemic, precisely with this objective23, having been translated into several languages and validated in several countries, namely Italy28; New Zealand29; Russia and Belarus30; Turkey31; Peru32; Israel33; Arab Countries34; Spain35 and France36 always with positive results for their psychometric properties.
In this sense, this study aims to translate and validate the Portuguese version (from Brazil) of the FCV-19S23, which is called the COVID-19 Fear Scale (EMC-19). After analyzing its main psychometric properties, such as validity and reliability, in addition to measuring, this scale can be used in clinical practice and in research, to better understand and intervene on the psychosocial repercussions of COVID-19.
It will still be possible to carry out crosscultural comparative studies between the different countries that have already translated and validated it. The knowledge produced in this way can help to promote health behaviors to prevent the impacts of COVID-19 on mental health, and to support public policies that are adequate to fight the pandemic.
METHODS
The Fear of Covid-19 Scale (FCV19S)23 is a self-administered questionnaire consisting of seven items to be answered on a 5-point Liberte scale, from "Strongly Disagree" to "Strongly Agree". In the original psychometric study, a one dimensional scale was considered, with factor loadings ranging from 0.66 to 0.74. As for internal consistency, Cronbach's alpha of α= 0.82 was favorable, as well as the correlation coefficients between items and the corrected total, from 0.47 to 0.74. The test-retest stability of 0.72 was also acceptable. The FCV19S scores correlated significantly and positively with perceived vulnerability and anxiety and depression, assessed using the Likert scale23.
The process of translating the FCV19S into Brazilian Portuguese was as follows: first, the original scale in English (v1) was translated into Portuguese by two of the Brazilian researchers (v2). Then, the translated Portuguese version (v2) was translated back to English by a Google Translator (v3) translation software. Finally, the 2 Brazilian researchers compared the English version (v3) with the original version (v1), item by item, verifying the equivalence of meanings. Subsequently, a Portuguese researcher carried out a new review, so that the proposed version could be used in Brazil and Portugal. A total of 3 researchers participated in the process of translating the instrument in an interdependent manner, thus obtaining its final version in Portuguese (Brazil), called the COVID-19 Fear Scale (EMC-19).
Participants were recruited online, through social networks and invited to participate in the study, stating its objective and inclusion criteria, namely: being over 18 years of age and fluent in Portuguese. Participants who agreed to participate voluntarily gave their informed consent. They then filled out a form in Google Forms, which, in addition to the Portuguese version of the EMC19, asked about some sociodemographic variables, including: age in years, gender (male and female), education (elementary, graduation, master's doctorate, other) , race with which they identified (white, black, brown, indigenous or yellow), marital status (single, stable, married, divorced, other), in the case of women, if they were pregnant at the time of the research and the number of living children.
Statistical treatment was performed using the IBM SPSS Statistics program, version 26 for Windows. Data processing began by determining descriptive statistics, measures of central tendency and dispersion.
As the sample size is sufficient, and taking into account the central limit theorem, measures and parametric tests, such as Pearson's correlation coefficient and Student's T, were used to compare mean scores.
The magnitude of the correlation coefficients was classified according to Cohen's criteria: low if less than 0.19; moderate if between 0.20 and 0.49 and high if greater than 0.50.
In the Exploratory Factor Analysis (EFA), it was guided by the Kaiser Criteria (1958)37 and the scree test by Cattell38. Following Kline's39 suggestion, it is considered that "weights" (loadings) with values > 0.30 are associated with the factor and that "weights" > 0.60 are high.
Before proceeding with the factor analysis, the KMO test (Kaiser-Meyer-Olkin) and the Bartlett sphericity test were performed, which are two statistical procedures that allow to measure the quality of the correlations between the variables, in order to know if it is plausible perform the factor analysis40. To carry out this analysis safely, the first should approach one, being "good" if >0.80; the second should lead to rejecting the null hypothesis, which also happened with our data (p <0.001).
The AMOS 26.0 software was used for the confirmatory factor analysis (CFA). Violation of the normal distribution was verified with the skewness and kurtosis coefficients. The adjustment of the models was made from modification indices greater than 11, p < 0.001, produced by AMOS and based on theoretical considerations41. To assess the fit of the model, the following fit indices were used: X2/gl, Comparative Fit Index (CFI), Goodness of Fit Index (GFI), Tucker-Lewis Index (TLI), Root Mean Square Error of Approximation (RMSEA).
For the analysis of internal consistency, Cronbach's alpha coefficient was used. In order to determine the particular contribution of each item to the internal consistency of the dimension, Cronbach's alpha coefficients were determined excluding the respective items, and then compared with the global alpha of the dimension. To ascertain the discriminative power or internal validity of each item, the correlation coefficients were analyzed between each item and the total (excluding the item).
The study was approved by the National Research Ethics Committee of Brazil - CONEP, in accordance with the attributions defined in CNS Resolution No. 510 of 2016, in CNS Resolution No. 466 of 2012 and Operational Standard No. 001 of 2013 of the CNS, which manifested itself for the approval of the proposed research project with the CAAE number: 32934720.3.0000.5556, under the title: Perinatal Psychological Disorder in times of COVID. Data were treated with conditionality, equality and fairness. All procedures followed were in accordance with ethical standards. Informed consent was obtained from all participants included in the study. Case number: 4,179,143.
RESULTS
Sample characterization
During the period of data collection, between June 19th and July 23rd, 2020, 364 valid responses were obtained.
The mean age of participants was 33.11 years (±10.047), ranging from 18 to 67 years. The majority were female (n=332; 91.2%), with a degree of education or more (n=286; 78.6%); regarding marital status, most were married or in a stable relationship (n=225, 61.8%) and had children and/or were pregnant (n=300, 82.4%). Regarding the race with which they identified, the distribution was as follows: white, n=182 (50.0%); brown, n=119 (32.7%); black, n=52 (14.3%); indigenous, n=2 (5.0%) and yellow, n=9 (2.5%).
A little more than a quarter of the participants (n=95, 26.1%) were health professionals, and of these, 42 (11.5% of the total sample) are "frontline professionals", that is with direct contact with patients.
Construct validity
To establish the construct validity a random division of the sample into two sub-samples was performed; with one of them, EFA was performed (n=192; 52.7%) and, with the other, AFC (n=172; 43.3%). Mean age (33.29±10.41 vs. 32.91±9.68; t=0.311, p=0.756) and the proportions of females (91.3% vs. 90.4%; X2=0.002, p =0.557), of having children (55.5% vs. 45.0%; X2=3.474, p=0.073), of being a health professional (22.4% vs. 30.2%; X2=2.889, p =0.067) and being of black/brown race (91.3% vs. 90.4%; X2=0.002, p=0.557) did not vary significantly in these two subsamples, confirming their equivalence.
Preliminary to AFE it was verified that the KMO was equal to 0.860 and that the Bartlet test resulted in significant (p<0.001).
The exploration of the factor analysis, carried out without any rotation and without defining the number of factors (the only criterion was that components with latent roots greater than one were extracted), resulted in only one component, with an explained variance of 55.49%. The graph corresponding to the Scree plot of Catell is shown below (Figure 1).
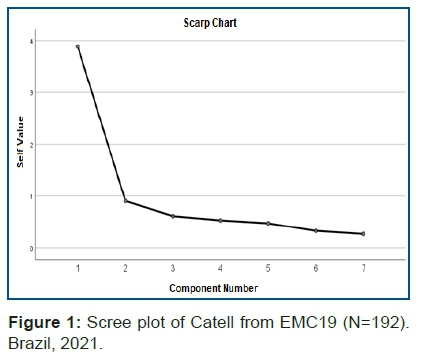
The observation of the scree plot also favors the option for a one-dimensional structure.
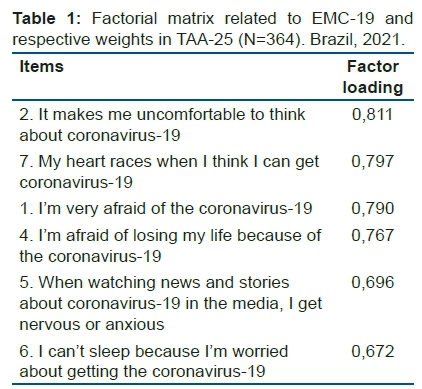
Table 1 corresponds to the factorial matrix obtained with the items arranged in de-scending order of their respective weight in the (single) factor. With this subsample, the alpha coefficient of internal consistency was a=0.865.
With the AFC, unsatisfactory adjustment indices were obtained from the initial one dimensional model with seven items (Table 2). After correlating fourth pairs of item errors (1 and 2, 1 and 7, 3 and 6 and 6 and 7) with modification indices greater than 1140, there was a very good overall fit (Table 2, Figure 2). Cronbach's alpha coefficient in this subsample (n=172) was a=0.898.
Cronbach's alpha coefficient in the total sample (N=364) was a=0.876.
The table 3 presents, in addition to the mean score and standard deviation of each item, the Cronbach's alpha if each item is excluded and the corrected item total correlation. It was found that all items in the scale contribute to internal consistency, as they presented corrected item total correlations greater than 0.40, ranging from 0.589 (item 6) to 0.709 (item 7) and that the exclusion of each one would cause the full scale Cronbach's alpha/ decreases slightly.
The mean total score on the EMC19 was 18.53 (±6.63), with a range from 7 to 35, that is, equivalent to the theoretical variation.
In Table 4, we present the values corresponding to the percentiles (and quartiles) of this sample.
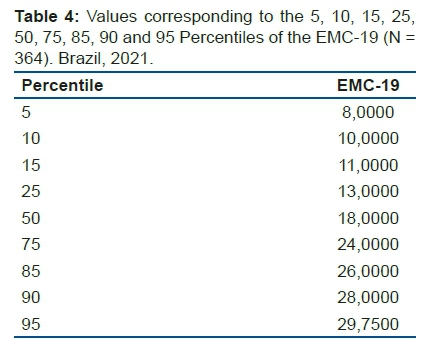
The mean total score was significantly higher in females (18.76±6.62) than in males (16.03±6.26) [t=2.243 (362), p=0.026)].
By age groups, organized into two categories, aged under 35 years (n = 192, 52.7%) vs. older than 36 years (n = 172, 47.2%), there was no significant difference in the mean total score on the EMC19 [ t = 2017 (362), p = 0.065)].
Having children, not having children or being pregnant also does not seem to influence fear of COVID19, measured by EMC19 [t= 1.200 (362), p=0.231)].
Race, categorized as white (n = 182, 50.0%) vs. others (n = 171, 47.0%) also did not result in previous scores beyond fear of COVID19 [t = -1386 (351), p = 0.167)].
When compared to other professional categories, it appears that health professionals did not present higher scores in the total CME19 [t= -0.524 (362), p=0.601)]. However, if only the "professionals at the top" are considered, it will be possible to notice that they have significantly lower scores for fear of COVID-19 (16.40±6.31) than the rest of the sample (18.80± 6.62) [t=-2.218 (362), p=0.027)].
DISCUSSION
The present study sought to ensure the validity and reliability of the COVID-19 Fear Scale, through its translated and validated version into Portuguese (Brazil), as a measure of the severity of fear of COVID-19 among a population of Brazilian adults, according to psychometric variables.
The results confirmed the construct validity of the one dimensional structure of the EMC-19, as well as its good internal consistency. In addition, normative values, means and percentiles are presented, which can be used to compare scores of individuals or groups, including across countries23.
The good psychometric properties of the scale offer confidence, rigor and objectivity in the assessment of this important component of the population's mental health during the pandemic, both in clinical practice and in research23,43.
No significant differences were found in scores when compared according to the sociodemographic variables selected in the study, with the exception of gender. Being a woman was also a variable that was associated with higher levels of fear of COVID-19, in the results obtained in other studies that used FCV-19S, as well as being married44,45,46. they also corroborate the findings in the literature regarding education that did not influence the perception of fear of the people in the sample23,44,47.
It is important to highlight that fear represents a stimulus strongly associated with triggering the stress response, which, in turn, interferes with the adaptive process in face of potentially life threatening situations48.
The ability to respond to stress is an individual characteristic. There are people who are robust to stress. That is, they are able to understand their experience, trigger effective emotional selfregulation strategies and adapt successfully48,50.
Others, in turn, present maladaptive coping that, in addition to denying or naturalizing stress, include behaviors and attitudes such as working too hard; hyperactivity; abusive use of legal and illegal substances; overeating; cultivate dysfunctional and depressive thoughts48,50.
It was found that the group of health professionals, particularly those who work in a different line, have lower levels of fear of COVID-19, which may be related to a phenomenon of desensitization or habituation, related to the reduction of fear and with cognitive changes49. That is, a set of coping strategies that some people end up developing in an attempt to maintain balance and deal with the pressures of life49,50.
On the other hand, these low levels of fear can be one of the signs of maladaptive coping that, in longerlasting situations, can lead to physical and mental illness49,50.
Furthermore, individuals with a low level of fear may not adhere to the sanitary measures recommended for the prevention of COVID-19, increasing their exposure to the risk of becoming ill18.
In addition to the personal risks involved in the provision of services, health professionals do not have, in the immediate future, a forecast about the end of this situation of pressure and psychoemotional overload.
Thus, it is essential to adopt preventive and care measures at an opportune time, considering that the context of the pandemic itself interferes with stress levels and can worsen the mental health of individuals already predisposed to psychoemotional disorders51.
Duan & Zhu (2020)52, propose that interventions aimed at mental health care should be broad and based on the careful assessment of risk factors, such as history of mental suffering, experience of mourning, selfinjury or violent behavior in relation to others people, panic, separation from the family and low family income.
The emotional experience of health professionals, as well as adaptive coping with stress, represent important questions for future studies, considering that coping styles and psychological growth are important for the maintenance of everyone's mental health42.
It is important to understand that the greater perception of fear can have repercussions as a motivational element in the adoption of preventive behavior, which constitutes a positive and functional response with regard to containing the advance of the pandemic26, 53. However, these individuals with higher levels of fear may adopt mistaken preventive measures that are not based on scientific evidence, making them more susceptible to infection18, as well as to the development of more severe mental disorders51.
These results overlap with those of other validation studies carried out in Iran, New Zealand, Paraguay, Russia, Saudi Arabia, Canada, France, Italy, Bangladesh, Israel28-36; among which, depression and/or anxiety scales were included to test the convergent validity, with positive, significant and moderate magnitude associations.
The availability of a valid and reliable instrument will support future correlational studies, already underway, in order to contribute to a better understanding of the correlates of fear of COVID-19. These correlational studies may also serve for additional validation of the instrument.
The findings of the present study must be considered in light of some limitations. First, this is not a population study and, therefore, the results apply only to the selected sample and do not allow generalizations. The sample was mostly represented by the female sex, which affects its representativeness. Although data collection through social networks facilitates the recruitment of volunteers for the research, it can lead to a selection bias, from the point of view of sociodemographic variables, such as education and socioeconomic level, and problems cannot be excluded. social and convenience factors may have influenced participants' responses to the questionnaire.
It is noteworthy that the temporal stability was not properly analyzed, considering that such analysis requires a longer term that allows for a valid instrument for this issue. In other words, it is considered that, given its urgency, it was not justified to wait two months for the retest.
Future studies should also assess whether individuals with underlying medical conditions associated with an increased risk of death from COVID-19 (eg, diabetes, hypertension, coronary heart disease, preexisting respiratory conditions) might have increased levels of fear from COVID-19.
It is important to collect a more representative sample of the Brazilian population to confirm the preliminary results provided by this study. However, the evidence that the total scores on the EMCV-19 do not differ significantly by age suggests that the EMC-19 can be used to assess fear of COVID-19 among Portuguese speaking individuals. The phrases used in each of the items are exactly the same in the Portuguese versions of Brazil and Portugal, in order to enable multicentric and crosscultural studies.
CONCLUSION
The Covid-19 Fear Scale (EMC-19) in its Portuguese (Brazil) version is a reliable and valid tool to assess the severity of fear of COVID-19 among Brazilian adults.
The EMC-19 validation process demonstrated the questionnaire's construct validity and internal consistency, characterized by the robustness of its psychometric qualities.
The EMC-19 is an instrument that is easy to apply by health teams, which will allow the assessment of behaviors in the face of the COVID-19 pandemic, in order to provide subsidies for mental health care, from planning to the implementation of preventive actions, educational and rehabilitation activities that aim to overcome fear and the impacts of psychoemotional disorders of COVID-19.
Author contributions
All authors contributed to the conception and design of the study. Material preparation, data collection and analysis were performed by Monalisa NS Barros, Ana Telma Pereira, Marcella Aguiar and António Macedo. The first draft of the manuscript was written by Monalisa N. S. Barros and Ana Telma Pereira. All authors commented on previous versions of the manuscript. Maria Inês Puccia made a final review of the article. All authors read and approved the manuscript.
Conflict of interest statement
The inexistence of a conflict of interest is declared, as so far, the existence of conflicts, whether financial or not, is not known.
REFERENCES
1.World Health Organization [Internet]. Copenhagen (DK): Mental health and COVID-19. c2020 [cited 2020 Mai 20]. Available from: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/novel-coronavirus-2019-ncov-technical-guidance/coronavirus-disease-covid-19-outbreak-technical-guidance-europe/mental-health-and-covid-19 [ Links ]
2.Basso M. [Internet]. Brasil: Subnotificação dificulta combate à COVID-19 no Brasil. c2020 [acesso 2020 abr 1]. Deutsche Welle. [about 1 screen]. Available form: https://www.dw.com/pt-br/subnotificação-dificulta-combate-à-covid-19-no-brasil/a-52919120 [ Links ]
3.Brasil. Ministério da Saúde [internet]. Brasilia (DF): COVID-19 - Painel Coronavírus. c2021 - [cited 2021 Aug 25]. Available from: https://covid.saude.gov.br/ [ Links ]
4.Coronavirus Resource Center [Internet]. Baltimore (MD): Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. c2021- [cited 2021 Aug 25]. Available from: http://coronavirus.jhu.edu/map.html [ Links ]
5.Reliefweb [Internet]. Conpenhagen (DK): Mental health and psychosocial considerations during COVID-19 outbreak; c Jun 14 2020 [cited 2020 Jul 28]. Office for the Coordination of Humanitarian Affairs (OCHA); [about 1 screen]. Available from: https://reliefweb.int/report/syrian-arab-republic/mental-health-and-psychosocial-response-during-covid-19-outbreak-une?gclid=CjwKCAjw4KyJBhAbEiwAaAQbE4bSTb-EEqrXv-LGA3rzH8Z2gl96dU1fXigYT2DxhB8_rWMTwuwHShoCXYgQAvD_BwE [ Links ]
6.Ornell F, Schuch JB, Sordi AO, Kessler FHP. "Pandemic fear" and COVID-19: mental health burden and strategies. Brazilian Journal of Psychiatry. 2020; 42(3): 232-235. [ Links ]
7.Slaikeu KA, Mejía MC, López MEG. Intervención en crisis: Manual para práctica e investigación. 2a ed. México: Manual Moderno; 1996. [ Links ]
8.Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. The Lancet Psychiatry. 2020; 7(7): 611-627. https://doi.org/10.1016/S2215-0366(20)30203-0 [ Links ]
9.Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The Lancet Commissions: The Lancet Commission on global mental health and sustainable development. The Lancet. 2018; 392(10157):1553-1598. https://doi.org/10.1016/S0140-6736(18)31612-X [ Links ]
10.Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Internal Medicine. 2020; 180 (6): 817-818. https://doi.org/10.1001/jamainternmed.2020.1562 [ Links ]
11.Mamun MA, Griffiths MD. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies. Asian Journal of Psychiatry. 2020; 51: 102073. https://doi.org/10.1016/j.ajp.2020.102073 [ Links ]
12.Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain, behavior, and immunity. 2020; 87: 34-39. https://doi.org/10.1016/j.bbi.2020.04.027 [ Links ]
13.World Health Organization [Internet]. Copenhagen (DK): Mental health and COVID-19. c2020 [cited 2020 Mai 20]. Available from: https://www.who.int/teams/mental-health-and-substance-use/covid-19 [ Links ]
14.Carbone, SR. Flattening the curve of mental ill-health: The importance of primary prevention in managing the mental health impacts of COVID-19. Mental Health & Prevention. 2020; 19:200185. https://doi.org/10.1016/j.mhp.2020.200185 [ Links ]
15.Goyal K, Chauhan P, Chhikara K, Gupta P, Singh, MP. Fear of COVID 2019: First suicidal case in India! Asian journal of psychiatry. 2020; 49:101989. https://doi.org/10.1016/j.ajp.2020.101989 [ Links ]
16.Griffiths MD, Mamun MA. COVID-19 suicidal behavior among couples and suicide pacts: Case study evidence from press reports. Psychiatry Research. 2020; 289: 113105. https://doi.org/10.1016/j.psychres.2020.113105 [ Links ]
17.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet Psychiatry. 2020; 395: 912-920. https://doi.org/10.1016/S0140-6736(20)30460-8 [ Links ]
18.Van Bavel JJ, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M et al. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour. 2020; 4: 460-471. https://doi.org/10.1038/s41562-020-0884-z [ Links ]
19.de Hoog N, Stroebe W, de Wit JB. The processing of fear-arousing communications: How biased processing leads to persuasion. Social Influence. 2008; 3(2): 84-113. https://doi.org/10.1080/15534510802185836 [ Links ]
20.Delumeau J. História do medo no ocidente: 1300-1800, uma cidade sitiada. São Paulo, Brasil: Companhia das Letras; 1989. [ Links ]
21.Pappas G, Kiriaze IJ, Giannakis P, Falagas ME. (2009). Psychosocial consequences of infectious diseases. Clinical Microbiology and Infection. 2009; 15(8), 743-747. https://doi.org/10.1111/j.1469-0691.2009.02947.x [ Links ]
22.Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N et al. Suicide risk and prevention during the COVID-19 pandemic. The Lancet Psychiatry. 2020; 7 (6), 468-471. https://doi.org/10.1016/S2215-0366(20)30171-1 [ Links ]
23.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 Scale: Development and initial validation. International Journal of Mental Health and Addiction. 2020; 1-9. https://doi.org/10.1007/s11469-020-00270-8 [ Links ]
24.Pakpour AH, Griffiths MD. The fear of COVID-19 and its role in preventive behaviors. Journal of Concurrent Disorders. 2020; 2(1): 58-63. [ Links ]
25.Xiang Y-T, Yang Y, Li W, Zhang L, Zhang Q, Cheung T et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry. 2020; 7(3): 228-229. https://doi.org/10.1016/S2215-0366(20)30046-8 [ Links ]
26.Harper CA, Satchell LP, Fido D, Latzman RD. Functional fear predicts public health compliance in the COVID-19 pandemic. International Journal of Mental Health and Addiction. 2020; 1-14. https://doi.org/10.1007/s11469-020-00281-5 [ Links ]
27.Witte K, Allen M. (2000). A meta-analysis of fear appeals: Implications for effective public health campaigns. Health Education & Behavior. 2020; 27(5): 591-615. [ Links ]
28.Soraci P, Ferrari A, Abbiati FA, Del Fante E, De Pace R, Urso A et al. Validation and psychometric evaluation of the Italian Version of the Fear of COVID-19 Scale. International Journal of Mental Health and Addiction. 2020; 1-10. https://doi.org/10.1007/s11469-020-00277-1 [ Links ]
29.Winter T, Riordan BC, Pakpour AH, Griffiths MD, Mason A, Poulgrain JW et al. Evaluation of the English Version of the Fear of COVID-19 Scale and Its Relationship with Behavior Change and Political Beliefs. International Journal of Mental Health Addiction. 2020; 1-11. https://doi.org/10.1007/s11469-020-00342-9 [ Links ]
30.Reznik A, Gritsenko V, Konstantinov V, Khamenka N, Isralowitz R. COVID-19 fear in Eastern Europe: validation of the Fear of COVID-19 Scale. International Journal of Mental Health and Addiction. 2020; 1-6. https://doi.org/10.1007/s11469-020-00283-3 [ Links ]
31.Satici B, Gocet-Tekin E, Deniz ME, Satici SA. Adaptation of the Fear of COVID-19 Scale: Its association with psychological distress and life satisfaction in Turkey. International Journal of Mental Health and Addiction. 2020. https://doi.org/10.1007/s11469-020-00294-0 [ Links ]
32.Huarcaya-Victoria J, Villarreal-Zegarra D, Podestà A, Luna-Cuadros MA. Psychometric properties of a Spanish version of the Fear of COVID-19 Scale in general population of Lima, Peru. International Journal of Mental Health and Addiction. 2020; 1-14. https://doi.org/10.1007/s11469-020-00354-5 [ Links ]
33.Bitan DT, Grossman-Giron A, Bloch Y, Mayer Y, Shiffman N, Mendlovic S. Fear of COVID19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Research. 2020; 289:113100. https://doi.org/10.1016/j.psychres.2020.113100 [ Links ]
34.Alyami M, Henning M, Krägeloh CU, Alyami H. Psychometric evaluation of the Arabic version of the Fear of COVID-19 Scale. International Journal of Mental Health and Addiction. 2020; 1-14. https://doi.org/10.1007/s11469-020-00316-x [ Links ]
35.Martínez-Lorca M, Martínez-Lorca A, Criado-Álvarez JJ, Armesilla MDC, Latorre JM. The Fear of COVID-19 Scale: Validation in Spanish university students. Psychiatry Research. 2020; 293: 113350. https://doi.org/10.1016/j.psychres.2020.113350 [ Links ]
36.Mailliez M, Griffiths MD, Carre A. Validation of the French Version of the Fear of COVID-19 Scale and its Associations with Depression, Anxiety and Differential Emotions. Research Square. 2020. DOI: 10.21203/rs.3.rs-46616/v1. [ Links ]
37.Kaiser HF. The varimax criteria for analytical rotation in factor analysis. Psychometrica. 1958: 23:141-5. [ Links ]
38.Cattel, RB. The scree test for the number of factors. Multivariate behavioral research. 1966; 1 (2): 245-276. [ Links ]
39.Kline P. The handbook of psychological testing. 2a ed. London and New York: Routledge; 2000. [ Links ]
40.Pestana MH, Gageiro JN. Análise de Dados para Ciências Sociais: A Complementaridade do SPSS. 6a ed. Lisboa: Edições Sílabo; 2014. [ Links ]
41.Marôco J. Análise Estatística com o SPSS Statistics. 7a ed. Pêro Pinheiro, Portugal: ReportNumber; 2018. [ Links ]
42.Sun N, Wei L, Shi S, Jiao D, Song R, Ma L et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. American Journal of Infection Control. 2020; 48(6): 592-598. https://doi.org/10.1016/j.ajic.2020.03.018 [ Links ]
43.Faro A, Bahiano MDA, Nakano TDC, Reis C, Silva BFPD, & Vitti LS. COVID-19 e saúde mental: A emergência do cuidado. Estudos de Psicologia (Campinas). 2020. 37: 1-14. https://doi.org/10.1590/1982-0275202037e200074 [ Links ]
44.Bakioğlu F, Korkmaz O, & Ercan H. Fear of COVID-19 and positivity: Mediating role of intolerance of uncertainty, depression, anxiety, and stress. International Journal of Mental Health and Addiction. (2020). https://doi.org/10.1007/s11469-020-00331-y [ Links ]
45.Doshi D, Karunakar P, Sukhabogi JR, Prasanna JS, & Mahajan SV. Assessing coronavirus fear in indian population using the Fear of COVID-19 Scale. International Journal of Mental Health and Addiction. 2020. https://doi.org/10.1007/s11469-020-00332-x [ Links ]
46.Tsipropoulou V, Nikopoulou VA, Holeva V, Nasika Z, Diakogiannis I, Sakka S, Parlapani E. Psychometric properties of the Greek Version of FCV-19S. International Journal of Mental Health and Addiction. 2020; 1-10. https://doi.org/10.1007/s11469-020-00319-8 [ Links ]
47.Sakib N, Bhuiyan AKMI, Hossain S, Al Mamun F, Hosen I, Abdullah AH, Mamun MA. Psychometric validation of the Bangla Fear of COVID-19 Scale: Confirmatory factor analysis and Rasch analysis. International Journal of Mental Health and Addiction. 2020. https://doi.org/10.1007/s11469-020-00289-x [ Links ]
48.Raio CM, & Phelps EA. The influence of acute stress on the regulation of conditioned fear. Neurobiology of Stress. 2015; 1: 134-146. https://doi.org/10.1016/j.ynstr.2014.11.004 [ Links ]
49.Benito KG, Walther M. Therapeutic process during exposure: Habituation model. Journal of Obsessive- Compulsive and Related Disorders. 2015; 6:147-57. [ Links ]
50.Kabat-Zinn, Jon. Viver a catástrofe total. 2ª.Ed. São Paulo: Palas Athena; 2019. [ Links ]
51.Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, & Benedek, DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry and Clinical Neurosciences. 2020; 74(4): 281. https://doi.org/10.1111/pcn.12988 [ Links ]
52.Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):300-302. http://dx.doi.org/10.1016/S2215-0366(20)30073-0 [ Links ]
53.Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard IM. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March. Journal of Anx-iety Disorders. 2020; 74:102258. [ Links ]
 Correspondence:
Correspondence:
marcellaguiar@gmail.com
Manuscript received: february 2021
Manuscript accepted: july 2021
Version of record online: november 2021














