Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Journal of Human Growth and Development
versão impressa ISSN 0104-1282versão On-line ISSN 2175-3598
J. Hum. Growth Dev. vol.31 no.3 Santo André set,/dez. 2021
https://doi.org/10.36311/jhgd.v31.12792
ORIGINAL ARTICLE
DOI: 10.36311/jhgd.v31.12792
Trends in COVID-19 mortality and case-fatality rate in the State of Paraná, South Brazil: spatiotemporal analysis over one year of the Pandemic
Djalma de Siqueira JuniorI; Tassiane Cristina MoraisII, III; Isabella PortugalIV; Matheus Paiva Emidio CavalcantiI; Blanca Elena Guerrero DaboinI; Rodrigo Daminello RaimundoV; Lucas Cauê JacinthoVI; Jorge de Oliveira EcheimbergV; Khalifa ElmusharafI; Carlos Eduardo SiqueiraI, VII
IMaster of Public Health Program, School of Medicine, University of Limerick, V94 T9PX, Limerick, Ireland
IIEscola Superior de Ciências da Santa Casa de Misericórdia (EMESCAM), 29045-402 Vitória, ES, Brazil
IIIDepartamento de Educação Integrada em Saúde, Universidade Federal do Espírito Santo, 29075-910 Vitória, ES, Brazil
IVDepartamento de Clínica Médica, Faculdade de Medicina da Universidade de São Paulo, 05403-000 São Paulo, SP, Brazil
VLaboratório de Delineamento de Estudos e Escrita Científica, Centro Universitário FMABC, 09060-870 Santo André, SP, Brazil
VIDivisão de Imunologia e Alergia Clínica, Departamento de Medicina, Faculdade de Medicina da Universidade de São Paulo, 05403-000 São Paulo, SP, Brazil
VIIDepartment of Urban Planning and Community Development, School for the Environment, University of Massachusetts Boston, 100 Morrissey Boulevard, Boston, MA 02125
ABSTRACT
INTRODUCTION: By late 2019, China notified a new disease rising, and with the agent's identification, it was called COVID-19. Despite the efforts of the World Health Organization (WHO) and worldwide countries, the disease spread out of control; on March 11, WHO declared the pandemic state. Brazil is the biggest country in South America, demarcated into 26 states with different economic, cultural, and social aspects. Paraná is one of the Brazilian federative units, it is the sixth more economically important and ranks second in Education. Its first COVID-19 case was confirmed on March 12, 2020, and the first death was on March 27, two weeks after the first death in Brazil.
OBJECTIVE: This study objective is to determine the mortality and case-fatality rates of COVID-19 in the State of Paraná, Brazil, from March 1, 2020, to March 31, 2021.
METHODS: It is an ecological time-series study, using all cases (854,326) and deaths (17,229 deaths) of COVID-19 reported in public and official database of the State of Paraná Health Department. Case fatality and mortality rates were stratified by sex and age. For trend analysis, the period was divided into a first "wave" (March to November 2020) and a second "wave" (December 2020 to March 2021). The Prais-Winsten regression model for population mortality and case-fatality rates allowed classifying whether it increased, decreased, or was flat.
RESULTS: Women were more affected by the number of cases, with 454,056 cases (53.15%) confirmed and 7,257 fatalities (42.12%). A total of 400,270 men (46.85%) were infected and 9,972(57.87%) died. For the first year of COVID-19, in the State of Paraná, the incidence was calculated as 7404.12/100,000 inhabitants, the mortality was 149.32/100,000 inhabitants, and the case-fatality rate was 2.02%. We saw a tendency for decreasing the case-fatality rate (DPC = -0,18; p<0,001). The mortality and incidence showed an increasing trend (DPC=1,13, p<0,001; DPC=1,58, p<0,001, respectively.
CONCLUSION: The level and variability of transmission during this first year of pandemic suggest that the disease in the State of Paraná was never under control.
Keywords: COVID-19, mortality, case-fatality, SARS-CoV-2, Epidemiology.
Authors summary
Why was this study done?
This study was carried out in response to the critical state of the country's health system in the fight against the COVID-19 pandemic. The lack of epidemiological data to strategically deal with the situation, especially in the state of Paraná, increases the risk of uncontrolled pandemics and consequently, increases the number of deaths.
What did the researchers do and find?
This study aims to determine the mortality and case-fatality rates of COVID-19 in the State of Paraná, Brazil, from March 1, 2020, to March 31, 2021. It is an ecological time-series study, using all the cases and deaths of COVID-19 reported in public and official database of the State of Paraná Health Department, Brazil. The effective reproduction number (Rt), the incidence, mortality, and lethality were estimated, then the trend analysis according to the wave period was classified as increased, decreased, or flat/stationary. We found that from May to August, the Rt was always above 1,0, after that period from August to mid-October, a number below 1,0.
What do these findings mean?
This study was essential to elucidate the status of the high mortality rate and confirm the lack of pandemic control in addition to the emerging need of the population of the state of Paraná to adhere to non-pharmacological measures as well as the advance of vaccination to control the COVID-19 pandemic.
INTRODUCTION
At the end of 2019, Chinese public health authorities reported a new viral respiratory disease surge to the world. On January 10, 2020, the country identified the etiological agent causing the severe acute respiratory syndrome (SARS), the coronavirus named SARS-CoV-2. Lately, the World Health Organization (WHO) announced the new coronavirus disease 2019 (COVID-19) and declared the pandemic state on March 11, 2020, despite the global efforts to contain the spread of the disease1.
In Brazil, the first COVID-19 case was confirmed on February 26, 2020. A 61 years old man who had traveled to Italy and returned to his home in São Paulo. The first death was a 57 years old woman from São Paulo, which occurred on March 11, 2020. Since then, COVID-19 has uncontrollably disseminated through all sociodemographic regions of the country, leading to an unprecedented socioeconomic crisis and health system collapse. By July 13, 2021, Brazil had 19.151.993 accumulated cases and 535.838 deaths, with an incidence of 9113.6 new cases by 100,000 inhabitants, mortality of 255.0 deaths by 100,000 inhabitants, and lethality of 2.8%2 being ranked as the second nation in the global death toll due to COVID-193.
Brazil is the largest country in South America, with an estimated population of 210,147,125 inhabitants and an extensive territory (8,510,345,538 km2) divided into 26 states and 1 Federal District. According to economic, cultural, and social aspects, the national territory is demarcated into five geographic regions (North, Northeast, Central-West, Southeast, and South), indicating a situation of disparities and inequalities permanently confronted by consecutive governments4.
In 1988 Brazil approved a new Constitution, which included a basic definition for health as a universal right and a governmental responsibility. The new Constitution also implemented universal and decentralized health coverage by creating the Unified Health System (Sistema Único de Saúde or SUS), responsible for providing public health care services since 19905. During the past three decades, despite all issues and challenges to cover over 200 million people living in a vast territory and socially unequal country, the SUS is well-known to have a robust primary care provision through the Family Health Strategy (Estratégia de Saúde da Família or ESF) program. Remarkably, the SUS vaccination program is a worldwide example of success6. The COVID-19 pandemic overwhelmed this system, increasing the demand for Intensive Care Unit (ICU) beds and advanced health care services, which evidenced the frailty of the Brazilian preparedness plan in response to public health emergencies7.
Suppose this sociodemographic condition, by itself, could be a tremendous challenge for the country to fight against a pandemic. In that case, a political situation leaves the country without the federal government's central organization to struggle with the problem. As an example, Brazil changed the Minister of Health four times during the first year of the pandemic.
So, the States had to deal with the pandemic independently, managing their treatment protocols, diagnostic tests, the negotiation of mechanical ventilators, supplies such as personal protective equipment, the training of health workers, and hospital resources like ICU beds. Everything had to be done respecting each state's context. It potentially led to different outcomes and, using the words of WHO's General Director, Mr. Teodros Adhanom Ghebreyesus, "Equity is critical. It applies to information, innovation, essential medical equipment, and supplies, as well as medicines, vaccines, and diagnostic"8.
Paraná is one of the Brazilian federative units located in the South Region. Together with the Southeast, they are the two more prosperous and developed regions of the country. Paraná is the sixth most crucial Brazilian state in terms of Economy and ranks second in Education. The State shares borders with Paraguay, and the port of Paranaguá, on the coast, is an essential route for international business. The airport of Curitiba, the capital State, is a critical gateway to other countries9. The first COVID-19 case of Paraná was confirmed on March 12, 2020, and the first death on March 27, almost two weeks after the first death in Brazil. As a similarity, all patients aforementioned were linked to recent international travel10.
To understand the COVID-19 risks and severity to better determine health programs and interventions, it is critical to know indicators like the incidence, mortality, and case-fatality rates. It can also be used to compare the outcomes of different Brazilian States, how they have managed COVID-19, and give insights regarding the expected inequalities that could arise during the fight against the disease.
Under these circumstances, this study objective is to determine the mortality and case-fatality rates of COVID-19 in the State of Paraná, Brazil, from March 1, 2020, to March 31, 2021.
METHODS
Study Design
It is an ecological time-series study, using all the cases and deaths of COVID-19 reported in public and official database of the State of Paraná Health Department, Brazil, available on the website https://www.saude.pr.gov.br/Pagina/Coronavirus-COVID-19. This study is part of a population-based umbrella project, where each state of Brazil was analyzed separately, following a standard protocol for ecological time-series studies as described by Abreu, Elmusharaf and Siqueira11.
Study Location and Period
The database was updated on June 1, 2021, considering information about cases and deaths of COVID-19 in residents of the state of Paraná, southern Brazil, from March 2020 to March 2021.
Study Population and Eligibility Criteria
Were included in the study all the cases and deaths by COVID-19 that occurred in Paraná and were reported by the municipalities (854,326 cases and 17,229 deaths) from March 2020 to March 2021.
All notifications of cases and deaths referred to COVID-19 were considered, using the International Classification of Diseases, 10th edition (ICD-10) of "U07.1 COVID-19, "identified virus" or "U07.2 COVID-19, virus not identified"12, associated with the diagnosis of the disease, according to with clinical, laboratory or epidemiological confirmation of disease. Cases and deaths were classified according to the date of diagnosis and death, respectively.
Data Collection
Two researchers independently extracted the data to minimize collection bias and guarantee the quality and reliability of the data obtained. The collected data were organized into spreadsheet software Microsoft® Excel 2016.
Population data were obtained using the Projection of the Federation Units Population by gender and age groups for the year 202013.
Data from cases and deaths of COVID-19 were collected and stratified by sex (male and female) and age groups (0-19 years, 20-29 years, 30-39 years, 40-49 years, 50-59 years, 60-69 years, 70-79 years, 80 or more years). The variables analyzed were sex (male and female), age groups, date of data de diagnosis, date of death, municipality of residence of the patient, and the number of daily and monthly cases and deaths.
Data Analysis
The effective reproduction number (Rt) was estimated using R studio software EpiEstim package14, version 2.2.4, a previously time-varying reproduction number for epidemics model, developed by Thompson and colleagues15. Our model used a mean serial interval of 2.97 days with an average standard deviation of 3.29 days, as described in previous studies16,17.
The incidence (1) and mortality rates (2) by 100,000 inhabitants and the case-fatality (3) (%) were calculated according to the equations:
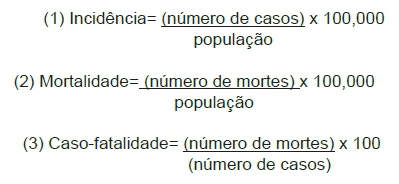
Mortality rates were also calculated and stratified by sex and age for the same period. According to the population projection of Federation Units for the year 2020, the State of Paraná had 11,538,518 inhabitants13.
For trend analysis, the period was divided into the first wave (1st Wave - March to October 2020) and second wave (2nd Wave - November 2020 to June 2021) to define the end of the first wave, the month with the lowest mortality rate was considered, which suggested the end of a first wave in the curve.
The trends were analyzed according to the methodological guidelines by Antunes and Cardoso18, the Prais-Winsten regression model for population mortality rates was used to build time series, series as well as to determine the incidence, case fatality, and mortality trends. Were estimated the probability (p), and Daily Percent Change (DPC), considering a 95% level significance, according to equations (1), (2), and (3):
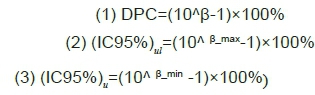
In these equations, we considered β as the angular coefficient from the linear regression, the indexes ul as the upper limit, and ll as the lower limit of the confidence level.
The case-fatality, mortality, and incidence trends were classified as increased, decreased, or flat. Flat trends were considered when the p-value was not significant (p<0.05).
Statistical analyses were performed using the STATA 14.0 software (College Station, TX, U.S. 2013).
Ethical and Legal Aspects of the Research
It is a secondary data analysis with no identification of the individuals in the database, and therefore no ethics committee approval was necessary.
RESULTS
The population of residents in the State of Paraná was taken from the projection of Federation Units for 202013, distributed by age and gender (table 1). Table 2 shows essential sociodemographic characteristics of the State of Paraná. The total population estimated for the State of Paraná in 2020 was 11,538,518 inhabitants.
According to the official database of the State of Paraná Health Department, from March 1, 2020, to March 31, 2021, there were 854,326 confirmed cases of COVID-19, and 17,229 people died from the disease. The distribution of cases and deaths by municipalities is illustrated in Figure 1.
For the first year of COVID-19 in the State of Paraná, the incidence was calculated as 7404,12/100,000 inhabitants, the mortality was 149,32/100,000 inhabitants, and the case-fatality rate was 2,02%.
Women were more affected by the number of cases, with 454,056 cases (53,15%) confirmed and 7,257 fatalities (42,12%). A total of 400,270 men (46,85%) were infected and 9,972 (57,87%) died. The highest number of confirmed cases was seen in 30-39 years women (99,952), and the deaths were higher in 70-79 years older men (2665) (Table 3).
The more economically active population, ranging from 20 to 59 years of age, was more infected than the older population (60 or more years) and the youngers (0-19 years), with an incidence of 5,607, 1,031, and 764 per 100,000 inhabitants, respectively. By the other side, mortality and case-fatality rate were higher in people older than 60, compared to the ranges of 20-59 and 0-19 years old (mortality = 110.97; 37.95; 0.40/100,000 inhabitants, and case-fatality = 10.76%; 0.67%; 0.05%, respectively). Figure 2 shows the proportions of cases (A), the proportion of deaths (B), the case-fatality (%) (C), and the mortality rate (per 100,000 inhabitants) of COVID-19 distributed by gender and age in the state of Paraná from March 2020 to March 2021.
According to new cases distributed by day, the effective reproductive number Rt was estimated from March 2020 to March 2021. In the beginning, there was a higher variability, with April having numbers as high as almost 1.7 and low below 0.8. After this, with a few days of variations, from May to August, the Rt was always above 1.0. Only from August to mid-October, a number below 1.0, with a decreasing trend in transmissibility rates, could be seen. After these two and a half months of hope, the levels arose again, with peaks of 1.27 at the beginning of November, 1.16 just after Christmas and New Year's Eve in January, and then 1.22 in the last days of February. Thus, the level and variability of transmission during this first year of pandemic suggest that the disease in the State of Paraná was never under control.
Figure 3 shows the distribution of new cases and the Rt during this period.
To define the periods for trend analysis or "waves," the end of each period must be the one with the lowest level of mortality happening after a peak and then constant dropping in numbers for more than two months. Looking at data, the bottom tier after the first peak descendent was October 2020, with mortality of 7.01/100,000 inhabitants. It gave us a division in the entire period of March 2020 to March 2021 in two waves. The first one was from March 2020 to October 2020, and the second wave was from November 2020 to March 2021 (Figure 4b). We could see mortality as high as 13.63/100,000 inhabitants in August 2020, the peak of the first wave, and much higher mortality, 40.50/100,000 inhabitants, in March 2021.
The case-fatality rate was high in April (4.96%), when there still was a lot of uncertainty about the best way to treat the disease and had the bottom level in November 2020 (1.05%). After this, in March, probably related to the appearance of new variants, the rate rose again to 3.22%.
Figure 4 shows the percentual case-fatality (A), the mortality rate (B), and the incidence rate (C) per 100,000 inhabitants of COVID-19 in the State of Paraná, according to the 1st (March to October 2020) and 2nd (November 2020 to March 2021) waves.
The Prais-Winsten regression model for population mortality and case-fatality rates were used to build time series, assessing whether it increased, decreased, or was flat. From March 2020 to March 2021 we saw a tendency for decreasing the case-fatality rate with a daily reduction rate of 0.18% (DPC = -0.18%; p<0.05), maybe because of the better knowledge about the disease and how to treat it. However, the mortality and incidence showed an increasing trend (p<0.001) (Table 4).
The first wave had a tendency of a decreasing case-fatality (DPC= -0.34; p<0.001), and an increasing mortality (DPC= 1.69; p<0.001) and incidence (DPC=2.57; p<0.001). The second wave, maybe influenced by the explosion of cases and deaths caused by the new variant P1, had an increasing trend of fatalities (DPC= 0.73; p<0.001) and mortality (DPC=1.02; p<0.001) (Table 4).
DISCUSSION
The first year of the COVID-19 pandemic in the State of Paraná, Brazil, had an incidence of 7404.12 new cases by 100,000 inhabitants, the mortality was 149.32 deaths by 100,000 inhabitants, and the case-fatality rate was 2.02%.
In our results, women are more affected by the disease than men, although men died more than women. The range of 30 to 39 years old had more confirmed cases, both in men and women. However, the number of deaths was higher in 70 to 79 years old, both in men and women. In a wide range of ages, the more economically active population, between 20 to 59 years, had the higher incidence of the disease. The more elderly, with 60 or more, had a higher case-fatality rate. These results could be explained by the more economically active population having to work to earn their money for the family. Even with the risk of being infected, they are more prominent not to follow public health advisory of social distancing or lockdowns. It is especially true in low-income countries. Regarding age, since the beginning of the pandemic and mainly when Italy was brutally hit by it, older adults (60> or older) were identified as a significant risk factor for COVID-19 severity, which may be related to their higher frequency of comorbidities compared to the general population.
COVID-19 transmissibility in Paraná, during the first year of the pandemic, looks out of control most of the time. The estimated Rt was higher than 1.0, with peaks in April, the second month of the pandemic in Brazil, and the months of November, early days of January, and the end of February, possibly related to the Christmas and New Year's Eve and the appearance, in the city of Manaus, of the P1 variant, more contagious and aggressive19. Except for some slight days variation, from mid-August to mid-October was the only period when the estimated Rt was below 1.0. It could be explained by the results of the measures taken by states and municipalities to control the transmission (social distancing measures, obligatory use of masks, borders control, closure of schools, bars, restaurants, and stores). Maybe, after this short period, without political support, the population, tired of being at home and needed to restart working, did not see more periods of the low transmission rate.
Following the periods defined for trend analysis or waves, the first wave (March to October 2020) showed a peak of incidence and mortality in August (589.13 and 13.63/100,000 inhabitants, respectively), and the end of the curve at the lowest level showed an incidence of 337.75/100,000 inhabitants and mortality of 7.01/100,000 inhabitants. Because of the reasons mentioned above, the case-fatality rate had a peak in April (4.96%) and the lowest level in November (1.05%). The second wave (October 2020 to March 2021) has not ended by the data collection date. We established our study's scope as the first year of the pandemic, so further studies are needed to know the curve's behavior. The incidence, mortality, and case-fatality were rising at the end of March (1256.94/100,000 inhabitants, 40.56/100,000 inhabitants, and 3.22%, respectively).
This was a critical period, the pandemic caused by the COVID-19 has battered the healthcare infrastructure all around the globe, reverberating in the health care workers' tiredness as a reason, and expect that mass vaccination reduces these numbers20. The vaccination program started in Brazil on January 202121.
The Prais-Winsten regression estimates showed a statistically significant tendency (p<0.001) of an overall increasing incidence and mortality, indicating that the pandemic was still out of control. The decreasing trend in the fatality-case rate during the first wave and during the entire period could be explained by better knowledge and treatment protocols, and the increasing tendency during the second wave could be influenced by the appearance of new variants, problems with supplies like oxygen and the tiredness of health workers. These factors must be better studied. The lack of diagnostics and underreporting can influence the results of the incidence in the second wave.
Looking at the results around the world, Brazil is still not going well7. Besides the fact that it is difficult to compare the effects of countries and regions with different sociodemographic characteristics, health systems capacities, and amount of diagnostic tests done, by July 27, 2021, the country was the second in the number of deaths (550,586) and the third in cumulative cases (19,707,662), only behind the USA (611,010) and the USA and India (34,536,402 and 31,440,951), respectively22. During the first year, the incidence of COVID-19 in Brazil was 5974,41/100,000 inhabitants, the mortality was 150.67/100,000 inhabitants, and the case-fatality rate was 2.52%.
The State of Paraná had a similar result. Nevertheless, compared to the other two states from South Region, Santa Catarina, and the Rio Grande do Sul, with very similar sociodemographic characteristics, Paraná had the worst indicators23. The study of Marinho et al., 24, using another source of database (COVID-19 Data Hub project - https://covid19datahub.io/) and looking for the rates of mortality and lethality in Brazil until October 2020, showed a slight variation in lethality (2.89%) but drew the attention to the fact that these indicators had potentially bias because the low number of reliable diagnostic tests. They also ranked among the ten worst Brazilian states according to the severity of the disease, although Paraná was not.
There are a lot of factors that are important to be accessed in a respiratory tract viral pandemic. The agent, the host, the environment, the health workforce, Primary Health Care (PHC) programs and hospital structures and supplies, the political situation, and leadership. In their review article, Lippi, Sanchis-Gomar, and Henry25 used the expression "the perfect storm" to define the Covid-19 pandemic. They pointed that SARS-CoV-2 structure and peculiar biology of infection, high risk of inter-human transmission, long incubation time combined with early and sustained viral load, the existence of asymptomatic or mildly-symptomatic carriers, viral shedding for days after symptom relief, unfavorable progression towards respiratory distress and death in up to 5-10% of patients thus causing dramatic healthcare challenges, as well as environmental contamination", were factors that contribute to the magnitude of the pandemic.
We found that more men died in Paraná, and the elderly are more at risk too. Analyzes of the mortality risk factors in Brazil, using the SIVEP-Gripe, Brazilian Ministry of Health database of 162,045 patients (March to August 2020), showed that elder age, male gender with comorbidities are at higher risk of death26. The same result was found in the first 500 patients hospitalized in a major tertiary hospital in São Paulo. Age (older than 60 years old, gender (male), pulmonary CT scan findings, and troponin are variables that influence the outcome of death27.
Sociodemographic aspects and their relationship with the incidence and mortality of COVID-19 were analyzed in a prospective geospatial study between February and July 2020. The authors suggested that the incidence was influenced by houses where two or more people sleep in the same room and cities where the index of social vulnerability (SVI) and the municipality human development index (MHDI) were low. Mortality was also affected by low numbers in both indexes28.
Paraná is the 6th most populated state in the country, and besides this higher demographic density (52.4 inhab./km2), it is ranked five in the Human Development Index (HDI)9. Paraná also has a good health infrastructure. In January 2020, the number of ICU beds was 6559 in the South region, representing an average of 2.2/10,000 inhabitants. The area with the best index is the Southeast with 2.7/10,000 inhabitants, and the worst is the North with 0.9/10,000 inhabitants. The recommended number by the Brazilian Ministry of Health and WHO is 1 to 3/10,000 inhabitants29. On March 31, 2021, there was a higher occupation of 95% of ICU beds10. Whether there were cases of patients who died waiting for a bed or without assistance requires further investigations.
Our study did not evaluate the transmissibility of the virus, influenced by environmental factors such as the weather or season30,31. Paraná is part of the South region of Brazil, with subtropical weather and temperatures with a mean approximate of 19oC. Curitiba is the coldest state capital of Brazil32. The estimated Rt found in our study, during the winter in Paraná, was the lowest of the entire period, and the mortality also was in a descending curve. According to another study made in Pará, a North region State, where the spread of the virus didn't give up even in a tropical climate and much higher temperatures33.
The transmissibility and, consequently, the incidence are also influenced by social isolation or distancing measures34. Chen and colleagues35 examined coronavirus transmission and associated factors in six countries (China, Korea, Japan, Italy, the USA, and Brazil). In a qualitative analysis, they compared mitigation measures like border control, isolation and lockdowns, tracking of contaminated patients and their contacts, and the disease severity, measured by the number of cases and deaths. They concluded that China and Korea had taken high mitigation measures and had low severity of the disease. The USA and Brazil had insufficient mitigation and high severity. Another analytic, comparative study tried to see the correlation between social isolation in the states of Paraná and Santa Catarina and mortality. The level of social isolation in Paraná was never above 54%, with a mean of 37%, and the author saw no correlation between this factor and the variability of cases and deaths36.
We still need to investigate more about the consequences of Brazilian political leaders' influence on the disease behavior in the country. According to Ortega and Orsini37 Paraná is governed by a federal government ally who has been criticized for defending the Economy at the expense of health. Denemark38 in his article covering the historical perspective of past pandemics like the Spanish Flu and the Black Death, pointed that the best way to control a pandemic is to attack the problem as a public health challenge, and more than the type of government, authoritarian or democratic, is the leader positioning taking rapid scientific, informed decisions that will have the trust of the citizens and reach the best results. He also emphasized the low number of deaths in 12 countries led by women and needs further investigation.
"This pandemic reminds us that we have a shared destiny.
None of us, our health systems, and our economies operate in a vacuum.
We are interdependent. We cannot win without solidarity.
As long as COVID-19 persists in one country, it is a threat to all of us."
Mr. Teodros Adhanom Ghebreyesus - WHO's General Director (WHO, 2020).
Limitations
The current study used a secondary database. Although the database is from an official government department and collected on a large scale, secondary data will always have the limitation of reliability of data. In this particular case, the underreporting of COVID-19 in Brazil is recognized as a significant problem. The number of tests is deficient in the country. It directly impacts the case-fatality rate since many non-fatal cases have not been tested.
Another limitation is that the pandemic has not ended in Paraná, Brazil. The study comprised only the first year period. Otherwise, the number of cases and deaths revealed a continuous increase by March 2021. So, it was not possible to analyze until the end of the second established wave. It will be necessary to continuously investigate the numbers after the pandemic ends to have the final mortality and case-fatality rate results in the state.
CONCLUSION
During the first year of the COVID-19 pandemic in Paraná, Brazil, there were 854,326 confirmed cases of COVID-19, and 17,229 people died from the disease.
Even more than a year after the start of the Pandemic, Paraná registered a high concentration of new cases and deaths from COVID-19, factors that contributed to the second wave representing a more alarming scenario, with increasing trends in lethality (DPC= - 0.73 %) and mortality (DPC = 1.02%).
Author Contributions
Conceptualization, D.S.J., T.C.M., IP, M.P.E.C; B.E.G.D. and L.C.A.; methodology, D.S.J., T.C.M., L.C.J., R.D.R., K.E., C.E.S., and L.C.A.; software, T.C.M. L.C.J.; validation, L.C.J.; T.C.M., C.E.S., and L.C.A.; data curation, D.S.J., T.C.M., L.C.A.; writing-review and editing, all the authors; visualization, all the authors; supervision, K.E., C.E.S.; project administration, C.E.S., and L.C.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
to the staff of the Laboratório de Delineamento em Estudos e Escrita Científica, Centro Universitário FMABC, especially Celia Guarnieri, for her support in designing the map, and Henrique Moraes Ramos Da Silva for his contribution to access the platforms of secondary data.
Conflicts of Interest
The author declares that there is no conflict of interests related to this study.
REFERENCES
1.WHO (2021). WHO's Timeline Covid-19 Response' [internet]. 2021a . Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline# [ Links ]
2.Brazil - Ministry of Health. Covid-19 no Brasil'[internet]. 2021. Available from: https://qsprod.saude.gov.br/extensions/covid-19_html/covid-19_html.html [ Links ]
3.WHO (2021). Who Coronavirus Covid-19 Dashboard [internet]. 2021. Available at: https://covid19.who.int/table [ Links ]
4.Brazil - IBGE (2021). Áreas Territoriais [internet]. 2021. Available from: https://www.ibge.gov.br/geociencias/organizacao-do-territorio/estrutura-territorial/15761-areas-dos-municipios.html?=&t [ Links ]
5.Castro MC, Massuda A, Almeida G, Menezes-Filho NA, Andrade MV, de Souza Noronha KVM, Rocha R, Macinko J, Hone T, Tasca R, Giovanella L, Malik AM, Werneck H, Fachini LA, Atun R. Brazil's unified health system: the first 30 years and prospects for the future. Lancet. 2019; 394(10195): 345-356. DOI: 10.1016/S0140-6736(19)31243-7 [ Links ]
6.Funcia FR. Subfinanciamento e orçamento federal do SUS: referências preliminares para a alocação adicional de recursos. Ciência & Saúde Coletiva. 2019; 24(12): 4405-4415. DOI: 10.1590/1413-812320182412.25892019 [ Links ]
7.Abreu LC de. The path of humanity in the pandemic of COVID-19: the choice of the realistic, optimist or pessimist scenario. J Hum Growth Dev. 2021; 31(1): 05-08. DOI: http://dx.doi.org/10.36311/jhgd.v31.11683. [ Links ]
8.WHO (2020).WHO Director-Generals remarks for G20 trade ministers' [internet]. 2020. Available from: https://www.who.int/director-general/speeches/detail/who-director-generals-remarks-for-g20-trade-ministers [ Links ]
9.IBGE. Paraná. [internet]. 2021. Available from: https://cidades.ibge.gov.br/brasil/pr/panorama [ Links ]
10.Paraná - Secretaria de Saúde do Estado do Paraná. Boletim - Informe Epidemiológico Coronavírus (Covid-19) - Arquivos PDF. [internet]. 2021. Available from: https://www.saude.pr.gov.br/Pagina/Coronavirus-COVID-19 [ Links ]
11.Abreu LC, Elmusharaf K, Siqueira CEG. A time-series ecological study protocol to analyze trends of incidence, mortality, lethality of COVID-19 in Brazil. J Hum Growth Dev. 2021; 31(3):491-495. DOI: 10.36311/jhgd.v31.12667 [ Links ]
12.Who, 2020. International Statistical Classification of Diseases and Related Health Problems 10th Revision. World Health Organization [internet]. 2020. Available from: https://icd.who.int/browse10/2019/en#/U04 [ Links ]
13.Datasus. Informações de Saúde - TABNET. Demográficas e Socioeconômica. População residente [Internet]. Available from: http://www2.datasus.gov.br/DATASUS/index.php?area=0206&id=6942. [ Links ]
14.Cori A, Ferguson NM, Fraser C, Cauchemez S. A new framework and software to estimate time-varying reproduction numbers during epidemics. Am J Epidemiol. 2013; 178(9): 1505-1512. doi: 10.1093/aje/ kwt133. [ Links ]
15.Prete CA, Buss L, Dighe A, Porto VB, da Silva Candido D, Ghilardi F, Pybus OG, de Oliveira WK, Croda JHR, Sabino EC, Faria NR, Donnelly CA, Nascimento VH. Serial interval distribution of SARS-CoV-2 infection in Brazil. J Travel Med. 2021 Feb 23; 28(2): taaa115. DOI: 10.1093/jtm/taaa115 [ Links ]
16.Ali ST, Yeung A, Shan S, Wang L, Gao H, Du Z, Xu XK, Wu P, Lau EHY, Cowling BJ. Serial intervals and case isolation delays for COVID-19: a systematic review and meta-analysis. Clin Infect Dis. 2021:ciab491. DOI: 10.1093/cid/ciab491 [ Links ]
17.Thompson RN, Stockwin JE, van Gaalen RD, Polonsky JA, Kamvar ZN, Demarsh PA, Dahlqwist E, Li S, Miguel E, Jombart T, Lessler J, Cauchemez S, Cori A. Improved inference of time-varying reproduction numbers during infectious disease outbreaks. Epidemics. 2019; 29: 100356. DOI: 10.1016/j. epidem.2019.100356. [ Links ]
18.Antunes JLF, Cardoso MRA. Uso da análise de séries temporais em estudos epidemiológicos. Epidemiol Serv Saúde 2015; 24(3): 565-576. DOI: 10.5123/S1679-49742015000300024 [ Links ]
19.Faria NR, Mellan TA, Whittaker C, Claro IM, Candido DDS, Mishra S, Crispim MAE et al. Genomics and epidemiology of the P.1 SARS-CoV-2 lineage in Manaus, Brazil. Science. 2021; 372(6544): 815-821. DOI: 10.1126/science.abh2644 [ Links ]
20.Rajhans PA, Godavarthy P. COVID-19 Combat Fatigue among the Healthcare Workers: The Time for Retrospection and Action. Indian J Crit Care Med. 2021; 25(1):3-5. DOI: 10.5005/jp-journals-10071-23699. [ Links ]
21.BRASIL 2021. Brasil Pátria Vacinada. Brasil, Ministério da Saúde [internet]. 2021. Available from: https://www.gov.br/saude/pt-br/vacinacao [ Links ]
22.Johns Hopkins University & Medicine 'Covid-19 Dashboard' [internet]. 2021. Available from: https://coronavirus.jhu.edu/map.html [ Links ]
23.Brazil - Ministry of Health 'Painel Coronavirus'[internet]. 2021. Available from: https://covid.saude.gov.br/ [ Links ]
24.Marinho PR, Cordeiro GM, Coelho HFC, Cabra PC. The COVID-19 Pandemic in Brazil: Some Aspects and Tools. Epidemiologia. 2021; 2(3): 243-255. DOI: https://doi.org/10.3390/epidemiologia2030018 [ Links ]
25.Lippi G, Sanchis-Gomar F, Henry BM. Coronavirus disease 2019 (COVID-19): the portrait of a perfect storm. Ann Transl Med. 2020; 8(7): 497. DOI: 10.21037/atm.2020.03.157 [ Links ]
26.de Souza FSH, Hojo-Souza NS, Batista BDO, da Silva CM, Guidoni DL. On the analysis of mortality risk factors for hospitalized COVID-19 patients: A data-driven study using the major Brazilian database. PLoS One. 2021; 16(3): e0248580. DOI: 10.1371/journal.pone.0248580 [ Links ]
27.Brandão Neto RA, Marchini JF, Marino LO, Alencar JCG, Lazar Neto F, Ribeiro S, Salvetti FV, Rahhal H, Gomez Gomez LM, Bueno CG, Faria CC, da Cunha VP, Padrão E, Velasco IT, de Souza HP; Emergencia USP Covid group. Mortality and other outcomes of patients with coronavirus disease pneumonia admitted to the emergency department: A prospective observational Brazilian study. PLoS One. 2021; 16(1): e0244532. DOI: 10.1371/journal.pone.0244532 [ Links ]
28.Castro RR, Santos RSC, Sousa GJB, Pinheiro YT, Martins RRIM, Pereira MLD, Silva RAR. Spatial dynamics of the COVID-19 pandemic in Brazil. Epidemiol Infect. 2021; 149: e60. DOI: 10.1017/S0950268821000479 [ Links ]
29.Associação de Medicina Intensiva Brasileira (AMIB) 'Dados atualizados sobre leitos de UTI no Brasil'[internet]. 2020. Available from: https://www.amib.org.br/fileadmin/user_upload/amib/2020/abril/28/dados_uti_amib.pdf [ Links ]
30.Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci Total Environ. 2020; 729: 138474. DOI: 10.1016/j.scitotenv.2020.138474 [ Links ]
31.Gardner EG, Kelton D, Poljak Z, Van Kerkhove M, von Dobschuetz S, Greer AL. A case-crossover analysis of the impact of weather on primary cases of Middle East respiratory syndrome. BMC Infect Dis. 2019; 19(1): 113. DOI: 10.1186/s12879-019-3729-5 [ Links ]
32.Krüger E; Rossi F. Quantificação da ilha de calor de curitiba considerando aspectos de estabilidade atmosférica. Rev Bras Meteorol. 2015; 30(4): 394-404. DOI: 10.1590/0102-778620130093 [ Links ]
33.da Silva FL, Pita JD, Gomes MDA, Lélis da Silva AP, da Silva GLP. Intraregional propagation of Covid-19 cases in Pará, Brazil: assessment of isolation regime to lockdown- CORRIGENDUM. Epidemiol Infect. 2021; 149: e93. DOI: 10.1017/S0950268821000765 [ Links ]
34.Costa de Assis SJ, Lopes JM, Guedes MBOG, Sanchis GJB, Araujo DN, Roncalli AG. Primary health care and social isolation against COVID-19 in Northeastern Brazil: Ecological time-series study. PLoS One. 2021; 16(5): e0250493. DOI: 10.1371/journal.pone.0250493 [ Links ]
35.Chen YT, Yen YF, Yu SH, Su EC. An Examination on the Transmission of COVID-19 and the Effect of Response Strategies: A Comparative Analysis. Int J Environ Res Public Health. 2020; 17(16): 5687. DOI: 10.3390/ijerph17165687 [ Links ]
36.Neves FS. Correlation of the rise and fall in COVID-19 cases with the social isolation index and early outpatient treatment with hydroxychloroquine and chloroquine in the state of Santa Catarina, southern Brazil: A retrospective analysis. Travel Med Infect Dis. 2021; 41: 102005. DOI: 10.1016/j.tmaid.2021.102005 [ Links ]
37.Ortega F, Orsini M. Governing COVID-19 without government in Brazil: Ignorance, neoliberal authoritarianism, and the collapse of public health leadership. Glob Public Health. 2020; 15(9): 1257-1277. DOI: 10.1080/17441692.2020.1795223 [ Links ]
38.Denemark RA. Pandemics in global and historical perspective (2020). Globalizations. 2021. DOI: 10.1080/14747731.2021.1944460 [ Links ]
 Correspondence:
Correspondence:
luizcarlos.deabreu@ul.ie
Manuscript received: september 2021
Manuscript accepted: october 2021
Version of record online: november 2021














