Services on Demand
article
Indicators
Share
Estudos de Psicologia (Natal)
Print version ISSN 1413-294XOn-line version ISSN 1678-4669
Estud. psicol. (Natal) vol.26 no.3 Natal July/Sept. 2021
http://dx.doi.org/10.22491/1678-4669.20210024
10.22491/1678-4669.20210024
SOCIAL WORK PSYCHOLOGY
Anxiety, depression, stress and burnout in health professionals during the COVID-19 pandemic
Ansiedade, depressão, estresse e burnout em profissionais de saúde durante a pandemia de COVID-19
Ansiedad, depresión, estrés y burnout en los profesionales de la salud durante la pandemia de COVID-19
Fernanda Lúcia Nascimento Freire CavalcanteI,II; Kamilla Sthefany Andrade de OliveiraIII; Carla Larissa Fernandes Pinheiro AraújoI; Pedro Obede Medeiros CostaIV; Eliane Pereira da SilvaV,I; Eulália Maria Chaves MaiaV
IHospital Universitário Onofre Lopes
IIHospital Giselda Trigueiro
IIISecretaria de Estado da Saúde Pública do Rio Grande do Norte
IVPsicólogo Clínico
VUniversidade Federal do Rio Grande do Norte
ABSTRACT
The objective of this study is to assess the prevalence of anxiety, depression, stress and burnout in the health staff of an Intensive Care Unit - ICU. This is a study with an exploratory, descriptive, and longitudinal design, with a quantitative approach. The sample consisted of 90 health professionals. The reduced version of the Depression, Anxiety and Stress Scale-21 (DASS-21) and the Oldenburg Burnout Inventory (OBLI) scale were used. In order to apply statistical tests, the free statistical software R, version 3.6.1, was used. The institution's professionals showed higher levels of stress and exhaustion regardless of the provision of adequate training and guaranteed access to personal protective equipment. Efforts must be made to reduce the burnout on professionals. It is hoped that the results of the study will contribute to the provision of evidence to assist in the construction of intervention strategies to mitigate adverse responses to the COVID-19 pandemic in health professionals.
Keywords: anxiety; depression; burnout, psychological; coronavirus; health professionals.
RESUMO
O objetivo deste estudo é avaliar a prevalência de ansiedade, depressão, estresse e burnout na equipe de saúde de uma Unidade de Terapia Intensiva-UTI. Trata-se de um estudo com delineamento exploratório, descritivo e longitudinal, de abordagem quantitativa. A amostra foi composta por 90 profissionais da saúde. Foram utilizadas a versão reduzida da Escala de Ansiedade Depressão e Estresse-21 (DASS-21) e a escala Oldenburg Burnout Inventory (OBLI). Para aplicação de testes estatísticos, utilizou-se o software estatístico livre R, versão 3.6.1. Os profissionais da instituição apresentaram maior nível de estresse e exaustão, independentemente da oferta de treinamento adequado e garantia de acesso a equipamento de proteção individual. Devem ser feitos esforços para redução do desgaste dos profissionais. Espera-se que os resultados do estudo contribuam com o fornecimento de evidências que auxiliem na construção de estratégias de intervenções para mitigar as respostas adversas da pandemia de COVID-19 nos profissionais de saúde.
Palavras-chave: ansiedade; depressão; esgotamento psicológico; coronavírus; pessoal de saúde.
RESUMEN
El objetivo de este estudio es evaluar la prevalencia de ansiedad, depresión, estrés y burnout en el equipo de salud de una Unidad de Cuidados Intensivos - UCI. Este es un estudio con un diseño exploratorio, descriptivo, longitudinal, con un enfoque cuantitativo. La muestra estuvo conformada por 90 profesionales de la salud. Se utilizó la versión abreviada de la Escala de Depresión, Ansiedad y Estrés-21 (DASS-21), y la escala del Inventario de Burnout de Oldenburg (OBLI). Para la aplicación de pruebas estadísticas, se utilizó el software estadístico gratuito R, versión 3.6.1. Los profesionales de la institución mostraron un nivel más alto sobre la dimensión de estrés y agotamiento, independientemente de la provisión de capacitación adecuada y acceso garantizado a Equipos de Protección Personal. Se deben hacer esfuerzos para reducir el desgaste de los profesionales. Se espera que los resultados del estudio contribuyan a proporcionar evidencia para ayudar en la construcción de estrategias de intervención para mitigar las respuestas adversas a la pandemia de covid-19 en profesionales de la salud.
Palabras clave: ansiedad, depresión, desgaste psicológico, coronavirus, profesionales de la salud.
The context of viral epidemics around the world was experienced several times and, in mid-December 2019, a new infectious outbreak started in China, when the first case was identified in the city of Wuhan (Chen, Liu, & Guo, 2020). The disease, then called covid-19 and caused by SARS-CoV-2, spread quickly. On January 30, 2020, the World Health Organization (WHO) made the outbreak of COVID-19 public, declaring a state of public health emergency (WHO, 2020) and, in March, elevated the status of contamination to the COVID-19 pandemic, due to the rapid geographic dissemination of the disease (Wang et al., 2020).
Exposure to disasters and pandemics imposes on individuals a range of reactions that arise soon after the traumatic experience, including: worry, fear, anguish, somatic complaints and sleep disturbance (Bao, Sun, Meng, Shi, & Lu, 2020). Some occupational groups showed greater vulnerability to adverse mental health responses (Brooks, Dunn, Amlôt, Greenberg, & Rubin, 2016).
A review, based on 59 articles, identified that there were high levels of stress and psychological distress in health professionals who worked during the outbreaks of SARS, MERS, H1N1 influenza, H7N9 influenza, Ebola and COVID-19, and that the effects could be noticed both during and after the event and lasted up to three years (Kisely et al., 2020). Surveys carried out among health professionals at the beginning of the COVID-19 pandemic observed that 70% reported psychological distress, with 50.4% being symptoms of depression, 44.6% of anxiety and 34.0% of insomnia (Lai et al., 2020). In India, depression was present in 34.9% of physicians treating patients with COVID-19, anxiety in 39.5% and stress in 32.9% (Chatterjee et al., 2020). Other evidence found a combined prevalence of 24.3% for depression, 25.8% for anxiety and 45% for stress among the health staff (Salari et al., 2020).
Working in the health area and being on the front line of the care of patients with COVID-19 is a risk factor for mental health impacts. According to Sanghera et al. (2020), the main outcomes found among health professionals based on the International Classification of Diseases (ICD-10) are: anxiety, depression, acute stress, PTSD, insomnia and burnout.
In usual work situations, in a hospital environment, adverse mental health responses are already well documented, including the risk of suicide (Dutheil et al., 2019), and these results can worsen the distress of professionals in an unprecedented context such as that experienced after COVID-19 (Sirois & Owens, 2021).
Among the main factors associated with adverse mental health responses during a pandemic period, one can mention: long working hours, risk of infection, shortage of personal protective equipment-PPE (Trevisan et al., 2020), loneliness and separation from relatives (Kang et al., 2020). These responses add up to a climate of increased stress, increased occupational responsibilities, strict safety measures and reduced self-care (WHO, 2020). Other evidence indicates that being female, being a nurse, experiencing situations of discrimination and low coping resources are predisposing factors to psychological impacts (Sirois & Owens, 2021).
Accordingly, it is observed that the attention to the mental health of health professionals cannot be neglected to the detriment of the management of the infection. There is evidence that the number of people who have some type of mental illness after outbreaks of infectious diseases is greater than the number of people who became ill (Allsopp et al., 2019).
Interest in the topic of mental health during COVID-19 has been increasing, but most of the evidence and empirical studies are primarily international publications, i.e., little research has explored the context of the health professional in Brazil (Civantos et al, 2020; Dal' Bosco et al., 2020; Santos et al., 2021). Therefore, the need to assess the mental health impacts of the pandemic among Brazilian health professionals in an attempt to mobilize efforts to minimize them.
Some hypotheses were raised: Does Brazil keep pace with the internationally described mental health results? Is it possible to observe differences between sociodemographic characteristics and the occurrence of depression, anxiety, stress and burnout? Are professional aspects related to COVID-19 significantly associated with the occurrence of depression, anxiety, stress and burnout?
In light of the foregoing, and emphasizing the need to monitor the mental health responses of health professionals and to provide evidence to assist in the construction of intervention strategies, this study has the objective of assessing the prevalence of anxiety, depression, stress and burnout in the health staff of an ICU.
Methodology
Ethical Aspects
The study was approved by the Research Ethics Committee of the Federal University of Rio Grande do Norte – UFRN and the National Research Ethics Committee – CONEP under Opinion nº 4.021.442.
Design, Period and Place of Study
This is an exploratory, descriptive, longitudinal study, with a quantitative approach, carried out in an ICU of a university hospital in the northeast region of Brazil. This institution has 197 nursing beds, 19 adult ICU beds and 5 pediatric ICU beds regulated for the Brazilian Unified Health System – SUS (HUOL, 2021). Data collection took place from May 13 to 24, 2020. During this period, the institution did not have regulated beds for the care of patients with COVID-19.
Participants
The sample of study participants was obtained in a non-probabilistic and intentional way. A total of 90 health professionals participated in it. The inclusion criteria for the participants were: being a physician, nurse, nursing technician or physical therapist, working in the ICU during the COVID-19 pandemic period and with internet access. Psychology, social service, pharmacy and nutrition professionals, administrative employees, professionals performing temporary functions, medical and multiprofessional residents, in addition to workers on leave or in remote work, were excluded from the sample.
The professionals were invited, during the shift, to participate in the research. After consent, through the signature of FICF, the questionnaires and scales with mandatory response items were created in Google Forms, which guarantees the confidentiality and protection of the participants' data, and sent via the WhatsApp application.
Study Protocol
The study was divided into two stages. The first, described here, took place from May 13 to 24, 2020. The second stage took place from September 22 to November 28, 2020 and will be reported on another occasion. In both stages, data were collected using structured questionnaires on sociodemographic characteristics and on professional aspects related to COVID-19, as well as through the Depression, Anxiety and Stress Scale (DASS-21) and the Oldenburg Burnout Inventory (OBLI).
The questionnaire on sociodemographic characteristics investigated data such as age, gender, education, function, length of service in the position, marital status, income, family nucleus, practice of some religion, history of psychiatric disorder and previous follow-up. The questionnaire on professional aspects related to COVID-19 investigated access to personal protective equipment, information about the disease and training aimed at the scenario of the COVID-19 pandemic. This is in addition to the question about the professional's fear of becoming ill, the belief that he/ she will be asked to work during the pandemic, perception of professionalism and preparedness to provide care to patients.
In order to assess depression, anxiety and stress, the DASS-21 scale was used, which was translated and adapted for Brazil, and then revealed properties that attest to its quality in terms of assessing emotional states (Vignola & Tucci, 2014). The scale is a self-report measure, typified as Likert, composed of 21 items that are easy and quick to administer (Szabó & Lovibond, 2006).
In turn, in order to assess burnout, the OBLI scale was used, already validated and cross-culturally adapted to the Portuguese language. The OLBI consists of 16 items in two subdomains: emotional exhaustion and work disengagement. Each item is responded to on a 5-point scale. In order to limit the study to the burnout related to COVID-19, the phrase "caused by COVID-19" was added to each item (Sinval, Queirós, Passian, & Marôco, 2019).
Data Analysis
The identified variables were coded and stored in a database. In order to design the descriptive tables and to carry out the application of statistical tests, the free statistical software R, version 4.0.2, was used. In the qualitative variables, a descriptive analysis was performed by means of absolute and relative frequency distributions. In turn, in the quantitative variables, descriptive statistics were analyzed for measures of central tendency and data dispersion.
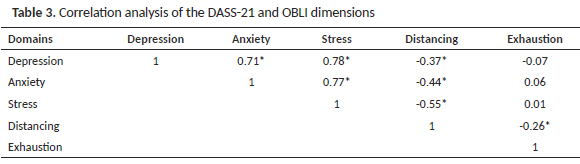
The occurrence of anxiety, depression, stress and burnout was considered as a dependent variable, while sociodemographic characteristics and professional aspects related to COVID-19 were taken as independent variables. When comparing the sociodemographic profile with the DASS-21 and OBLI dimensions, additional Student's t, Chi-square and Fisher's Exact tests were applied. In the analysis of correlation among the constructs, Pearson's test was used. It should be underlined that, for all statistical tests used, the significance level was 5%.
Results
This study was intended to assess the prevalence of anxiety, depression, stress and burnout in the health staff of an Intensive Care Unit-ICU of a hospital in the northeast region during the COVID-19 pandemic. The professional staff of the ICU contains 137 employees, among them: physicians, nurses, nursing technicians and physical therapists. During the collection period, 21 professionals were away or working remotely, another 25 did not respond to the instrument within the stipulated time for data collection or did not respond to the informed consent and 1 refused to participate in the research. Therefore, the final sample consisted of 90 professionals.
Sociodemographic Characteristics
In the study, among the 90 health professionals, 53 (58.89%) were nursing technicians, 17 (18.89%) were nurses, 12 (13.33%) were physicians and 8 (8.89%) were physical therapists. In the sample, female participants (61.11%), aged between 18 and 39 years old (56.66%) and married (54.44%) were prevalent. In general, participants live with a spouse (64.44%) and/or children (44.44%), but a portion of them live alone (20%). As for income, just under half of the sample survives with up to 2 to 4 minimum wages.
Just over half of the sample, that is 51.11%, have graduate studies and 56.67% have worked for up to 10 years. Around 78.89% practice some type of religion. In addition, 3.33% have some type of psychological disorder and 7.78% undergo psychological follow-up.
Professional Aspects Related to COVID-19
Regarding the professional aspects related to COVID-19, the vast majority (98.89%) reported having access to Personal Protective Equipment - PPE in the workplace, in addition to the fact that 97.78% declared to participate in training on how to behave in the face of the new coronavirus pandemic scenario. Moreover, 84.44% receive information about the disease every day at work.
All professionals reported the knowledge that their work is essential during the pandemic crisis, where 90.00% believe they will be summoned to act in the crisis; however, 84.44% indicated they were afraid of contracting the disease. Despite this, only 20% say they are prepared to work and provide care to patients with COVID-19, while 30% rate their professionalism as moderate.
Prevalence of Depression, Anxiety and Stress
The following levels of depression were noted: 26.67% mild, 14.44% moderate and 6.67% severe. Regarding the variable related to anxiety, the results indicate: 20% mild, 14.44% moderate and 4.44% severe. As for stress: 33.33% mild, 27.78% moderate and 8.89% severe.
Association of Depression, Anxiety and Stress with Sociodemographic Characteristics and Professional Aspects
Using Student's t test, it was observed that professionals who reported being under psychological care before the pandemic had higher averages in all assessed constructs, but it was observed a statistically significant difference only for depression and stress. In turn, moderate professional self-assessment showed a statistically significant difference for depression and anxiety. It was also noted that the feeling of not being prepared to act in the pandemic showed a statistical difference for anxiety, as displayed in Table 1. The other variables did not show significant statistical differences.
Through Chi-square test (X²) with a significance level of 5%, it was noted that, in those professionals who declare moderate professional self-assessment, depression levels can increase by 74%, compared to professionals with high professional self-assessment (p = 0.05, 95% CI=0.26 [0.10; 0.68]).
Regarding anxiety, it was observed that those professionals who reported being under psychological follow-up were 98% more likely to have anxiety (p = 0.013, 95% CI=11.17 [1.28; 97.32]). Similarly, it was observed that the greater the feeling of preparedness to deal with COVID-19, the greater the chance of not having symptoms of anxiety (p = 0.007).
There was a statistical association among the stress felt, the position held, the level of education and the fear of contracting COVID-19. Professionals with higher education positions (p = 0.038) and with graduate studies (p = 0.040) showed greater stress. Similarly, professionals who reported fear of contracting the disease may have a change in stress level 4 times greater than those who are not afraid of contracting the respective disease (p = 0.025, 95% CI=4 [1.23; 13.00]).
Prevalence of Emotional Exhaustion and Work Disengagement
In the assessment of the prevalence of Burnout, it was identified that 93.33% of participants showed emotional exhaustion and 36.67% work disengagement.
Association of Exhaustion and Work Disengagement with Sociodemographic Characteristics and Professional Aspects
Using Student's t test, it was observed that the only variable that showed a statistically significant difference among the averages for exhaustion was the psychological follow-up prior to the pandemic. Thus, those professionals who declare they are undergoing psychological follow-up had a higher rate of exhaustion. As for the dimension related to work disengagement, only the variable on gender showed a statistically significant difference. Accordingly, male professionals had a higher rate of work disengagement, as displayed in Table 2.
Through Fisher's Exact test with a significance level of 5%, it was found that the professional who declares fear of contracting COVID-19 may have a 14.80 times greater change in exhaustion compared to those who declared not to be afraid of contracting the disease (p = 0.005, 95% CI=14.80 [2.39; 91.46]). Professionals who are married or in a stable relationship also show a change in exhaustion, which can be 10.56 times higher compared to single or divorced professionals (p= 0.020, 95% CI=10.56 [1.17; 94.82]).
In the dimension related to work disengagement, the variables on gender and position showed a statistically significant association, according to the Chi-square test (X²). Thus, male professionals showed 2.82 times greater work disengagement when compared to female professionals (p = 0.020, 95% CI=2.82 [1.16; 6.87]). Regarding the positions, physical therapists and physicians were notably more likely to manifest behaviors related to disengagement compared to nurses and nursing technicians (p = 0.014). The summary of the comparison of the OBLI dimension with the general characteristics of the professionals is described in Table 2.
Correlation among Depression, Anxiety, Stress and Burnout
Through Pearson's correlation analysis, the DASS-21 and OBLI dimensions were compared, and it was found evidence of a strongly positive and statistically significant correlation between anxiety and stress, showing that as anxiety increases, stress also increases. The opposite is also true. There was also a strong positive correlation between depression and anxiety, as well as between depression and stress. Thus, as the score of one of these domains increases, the other domain also tends to increase. There is also a moderate negative correlation among disengagement, depression, anxiety and stress. Thus, as the distance score increases, depression, anxiety and stress tend to decrease, as displayed in Table 3.
Discussion
This research involved 90 health professionals working in a university hospital in the northeast region of Brazil and identified a high prevalence of mental disorders. In general, it was found that 70% of professionals had stress, 47.78% depression and 38.88% anxiety. Exhaustion was found in 93.33% of the surveyed participants and work disengagement was observed in 36.67%.
Regarding depression and anxiety, the results shown are compatible with what is pointed out by Lai et al. (2020) and by Pappa et al. (2020), where there is a high proportion of health professionals who experience significant levels of anxiety and depression during the pandemic and that, in most cases, the symptoms manifested themselves in a mild form.
The levels of moderate to severe depression and anxiety in our survey reached 21.11% and 18.88%, respectively. Similar to the study by Kang et al. (2020), which involved 994 health professionals and identified that mild disorders had a higher percentage than the sum of moderate and severe cases.
In turn, the data on stress from this study differ from the findings in previous studies, since the maximum prevalence of stress found in a review was 32.9% (Sanghera et al., 2020). According to Kang et al. (2020), the main reasons for adverse responses include long working hours, risk of infection and physical fatigue. Stress is an important factor to be considered in health workers and, according to Cattaneo et al. (2016), it is the main environmental risk factor for psychiatric diseases. Thus, prevention should be based on actions that minimize the time of exposure to stressful situations (Anjos &Santos, 2020).
Regarding exhaustion, one of the symptoms manifested in the burnout syndrome, our results surpassed the prevalence indicated by Rotenstein et al. (2018) in a review that included 184 studies and found a prevalence of up to 89% of emotional exhaustion. Another Brazilian study carried out by Tironi et al. (2016) in intensive care physicians found a prevalence of 50.6%. It is a fact that the pandemic brings an emotional impact to health workers and generates an additional aggravating factor for the occupational stress that is already constant in health care practices.
Burnout syndrome is one of the major psychosocial problems that affect the quality of life of professionals (Silva, et al., 2015). High levels of burnout are associated with poor care in relation to patient safety and the occurrence of adverse events (L. H. Hall, Jijnson, Watt, Tspi, & O'Connor, 2016). Moreover, high levels of emotional exhaustion among nurses causes a decrease in professional performance, can lead to greater absenteeism and implies greater patient dissatisfaction (Dyrbye et al., 2019).
According to Sirois and Owens (2021), there are factors that may contribute to the risk of adverse mental health responses or resilience. Therefore, the psychic implications for health professionals may vary according to the sociodemographic, occupational, social and psychological data of the individuals. Among sociodemographic factors, our study found that being male was associated with work disengagement. Another research carried out by Song et al. (2020), which involved 14,825 physicians and nurses in China, also found that men were more prone to depression than women. Nevertheless, this fact runs counter to most evidence assessing the association between gender and psychological distress, which indicates women as more prone to mental health symptoms (Sirois & Owen, 2021). Among other factors, these results may reflect the dilemma of work and family care, or even hormonal factors (Li & Graham, 2017) and employment inequalities (Li & Graham, 2020).
Regarding the position, it was observed that physical therapists and physicians were more prone to work disengagement and stress responses. Conversely, the literature attributes the higher prevalence of psychological distress to the nursing position, when compared to other health professionals (Luo, Guo, Yu, Jiang, & Wang, 2020; Pappa et al, 2020; Sanghera et al., 2020). Lai et al. (2020) also proposes that nursing professionals are affected with the most severe levels of all measurements of mental disorders.
In our study, education was a risk factor for stress responses, specifically the graduate level. Some investigations corroborate this finding and observed that having higher education and working in the health area are considered greater risk factors for impacts on mental health, especially the feeling of anguish, due to self-awareness of the risks entailed by working in a pandemic health context (Kisely et al., 2020; Lai et al., 2020; Qiu et al., 2020).
Social support is a protective factor that helps people deal with stressful situations more effectively (Brooks, et al., 2016; Kisely et al., 2020). Nonetheless, our results highlighted that professionals who are married or in a stable union show alterations in exhaustion, which may signalize that the level of social support may not be adequate to the needs of these professionals. In the research carried out by Sirois and Ower (2021), four studies found a similar result and two of them indicated that having a child generated greater stress. In addition to family support, institutional or peer support is also important. With regard to organizational support, D'Ettorre et al. (2021) indicated that low social support at work, high pressure, an unsafe environment coupled with the risk of becoming ill, and the low supply of PPE are risk factors for the mental health of workers.
In a period of viral outbreaks, psychological distress is also associated with the fear of contracting the disease, given the possibility of transmission among health professionals and their own families. In general, fear can take place due to reports of asymptomatic transmission of COVID-19 (Brooks et al., 2020). R. C. Hall, Hall, and Chapman (2008) add that the factors that negatively influence well-being are the testimony of illness and death of colleagues.
The fear of becoming ill was reported by 84.44% of the surveyed professionals and was an influencing factor for stress and exhaustion. When comparing our results with those of other studies carried out during the outbreak of Ebola, for example, it was observed that fear has an epidemiological impact, individually and collectively, increasing rates of psychiatric distress and symptoms (Ornell, Schuch, Sordi, & Kessler, 2020). Banerjee (2020) suggests that mental health be a focus of attention and also that psychiatrists and mental health professionals join health services to mitigate adverse outcomes.
Our study showed that individuals who reported a moderate assessment of professionalism had an increased chance of developing depression. According to R. C. Hall et al. (2008), it is possible to identify, among health professionals, the feeling of being underestimated. Du et al. (2020) observed that those professionals who considered themselves less psychologically prepared and with a low perception of self-efficacy to perform patient care were more affected by symptoms of depression and anxiety. In the same vein, it was identified an association between high ratings of professionalism and lower risk of depression. In addition, insufficient knowledge was described by Sanghera et al. (2020) as a predictor for anxiety.
A history of psychological distress and pre-existing mental health disorders cause worse mental health outcomes in disaster situations (Brooks et al., 2016) or in situations involving disease outbreaks such as SARS, MERS, H1N1, H7N9, Ebola virus disease and COVID-19 (Kisely et al., 2020). The data found in this study corroborate this perspective, as it was found great chances that a professional under psychological follow-up will manifest altered anxiety.
Finally, it is important to underline that, at the time of collection of this study, the hospital that participated in the research did not have beds regulated for SUS; even so, the results indicated a high prevalence of stress and exhaustion. However, according to the literature, adverse responses are more present in professionals on the front line of care related to COVID-19 compared to other health professionals. In addition, it was found that almost 100% of professionals claimed to have access to PPE and adequate training, a fact that did not imply significant results, and both initiatives have been pointed out in recent studies as protective factors for the mental health of health professionals and the reduction of burnout (Brooks et al., 2016; Kisely et al., 2020). Therefore, the mental health burden is extensive, thus raising the need for efforts to reduce burnout, so that work stress is managed and resolved and that protective measures can minimize impacts.
Conclusion
It was identified a high level of stress among professionals working in the ICU environment in the period of the COVID-19 pandemic, regardless of the provision of adequate training and guarantee of access to PPE. There was also a high level of burnout, mainly signalized by the change in the exhaustion of professionals.
Among the strengths of the study, one can cite the fast survey of the panorama of the psychological manifestations of health professionals who work in the ICU environment during the initial phase of the outbreak of COVID-19 and the opportunity for longitudinal follow-up that will allow a greater assessment of the impacts on a long-term basis. Allied to this, the survey was disseminated to the entire staff and had a high response rate. On the other hand, it is a fact that this is a specific context and an institution that, at the time of data collection, was not a reference in the care of patients with COVID-19, but that occupies a prominent place in the provision of health services to the population and in terms of health education.
Other limitations deserve consideration. Data were collected from a non-probabilistic sample, where the employed instruments reflect a subjective prevalence, since it did not include a standardized clinical interview. Additionally, the research took place during the outbreak, a fact that may impose greater awareness among professionals.
It is expected that the results of the study will contribute to the provision of evidence that will help in the construction of intervention strategies to mitigate adverse responses in health professionals. Likewise, there is a need for more empirical studies with prospective cohorts that may expand the understanding of the variables on stress, anxiety, depression and burnout in coping with the pandemic situation and in providing safe care to patients. In addition, research is suggested to measure the impacts related to the implementation of group interventions, psychoeducational actions in the face-to-face format or using the internet.
References
Allsopp, K., Brewin, C. R., Barrett, A., Williams, R., Hind, D., Chitsabesan, P., & French, P. (2019). Responding to mental health needs after terror attacks. BMJ (Clinical research ed.), 366, l4828. doi: 10.1136/bmj.l4828 [ Links ]
Anjos, K. F., & Santos, V. C. (2020). Transtorno de Estresse Pós-Traumático no contexto da COVID-19. Revista Brasileira de Saúde Funcional, 11(1), 6. Retrived from https://seer-adventista.com.br/ojs3/index.php/RBSF/article/view/1303 [ Links ]
Banerjee, D. (2020). The COVID-19 outbreak: Crucial role the psychiatrists can play. Asian Journal of Psychiatry, 50, 102014. doi: 10.1016/j.ajp.2020.102014 [ Links ]
Bao, Y., Sun, Y., Meng, S., Shi, J., & Lu, L. (2020). 2019-nCoV epidemic: Address mental health care to empower society. The Lancet, 395(10224), e37-e38. doi: 10.1016/S0140-6736(20)30309-3 [ Links ]
Brooks, S. K., Dunn, R., Amlôt, R., Greenberg, N., & Rubin, G. J. (2016). Social and occupational factors associated with psychological distress and disorder among disaster responders: a systematic review. BMC Psychology, 4(18). doi: 10.1186/s40359-016-0120-9 [ Links ]
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, J. G. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evi-dence. The Lancet, 395(10227), 912-920. doi: 10.1016/ S0140-6736(20)30460-8 [ Links ]
Cattaneo. A., & Riva, M. A. (2016). Stress-induced mechanisms in mental illness: A role for glucocorticoid signalling. The Journal of Steroid Biochemistry and Molecular Biology, 160, 169-74. doi: 10.1016/j. jsbmb.2015.07.021 [ Links ]
Chatterjee, S. S., Bhattacharyya, R., Bhattacharyya, S., Gupta, S., Das, S., & Banerjee, B. B. (2020). Attitude, practice, behavior, and mental health impact of COVID-19 on doctors. Indian Journal of Psychiatry, 62(3), 257-265. doi: 10.4103/psychiatry.IndianJPsychiatry_333_20 [ Links ]
Chen, Y., Liu, Q., & Guo, D. (2020). Emerging coronaviruses: Genome structure, replication, and pathogenesis. Journal of Medical Virology, 92(10), 2249. doi: 10.1002/jmv.26234 [ Links ]
Civantos, A. M., Bertelli, A., Gonçalves, A., Getzen, E., Chang, C., Long, Q., & Rajasekaran, K. (2020). Mental health among head and neck surgeons in Brazil during the COVID-19 pandemic: A national study. American Journal of Otolaryngology, 41(6), 102694. doi: 10.1016/j. amjoto.2020.102694 [ Links ]
DalâºBosco, E. B., Floriano, L. S. M., Skupien, S. V., Arcaro, G., Martins, A. R., & Anselmo, A. C. C. (2020). Mental health of nursing in coping with COVID-19 at a regional university hospital. Revista Brasileira de Enfermagem, 73(Suppl. 2), e20200434. doi: 10.1590/0034-7167-2020-0434 [ Links ]
DâºEttorre, G., Ceccarelli, G., Santinelli, L., Vassalini, P., Innocenti, G. P., Alessandri, F., ... Tarsitani, L. (2021). Post-Traumatic Stress symptoms in healthcare workers dealing with the COVID-19 pandemic: A systematic review. International Journal of Environmental Research and Public Health, 18(2), 601. doi: 10.3390/ijerph18020601 [ Links ]
Du, J., Dong, L., Wang, T., Yuan, C., Fu, R., & Zhang, L. (2020). Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. General Hospital Psychiatry, 67, 144-145. doi: 10.1016/j.genhosppsych.2020.03.011 [ Links ]
Dutheil, F., Aubert, C., Pereira, B., Dambrun, M., Moustafa, F., Mermillod, M., Baker, J. S., Trousselard, M., Lesage, F.-X., & Navel, V. (2019). Suicide among physicians and health-care workers: A systematic review and meta-analysis. PLoS ONE, 14(12): e0226361. doi: 10.1371/journal.pone.0226361 [ Links ]
Dyrbye, L. N., West, C. P., Johnson, P. O., Cipriano, P. F., Beatty, D. E., Peterson, C., ... Shanafelt, T. (2019). Burnout and satisfaction with work-life integration among nurses. Journal of Occupational and Environmental Medicine, 61(8), 689-698. doi: 10.1097/JOM.0000000000001637 [ Links ]
Hall, L. H., Jijnson, J.; Watt, I.; Tspi, A.; & O'Connor, D. (2016). Healthcare Staff Wellbeing, burnout, and patient safety: A systematic review. PLoS ONE, 11(7): e0159015. doi: 10.1371/journal.pone.0159015 [ Links ]
Hall, R. C., Hall, R. C., & Chapman, M. J. (2008). The 1995 Kikwit Ebola outbreak: Lessons hospitals and physicians can apply to future viral epidemics. General Hospital Psychiatry, 30(5), 446-452. doi: 10.1016/j.genhosppsych.2008.05.003 [ Links ]
Hospital Universitário Onofre Lopes. (2021). Núcleo Interno de Regulação de Leitos. Natal Retrieved from www.gov.br/ebserh/pt-br/hospitais-universitarios/regiao-nordeste/huol-ufrn/acesso-a-informacao/institucional [ Links ]
Kang, L., Li, Y., Hu, S., Chen, M., Yang, C., Yang, B. X., ... Liu, Z. (2020). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry, 7(3), e14. doi: 10.1016/s2215-0366(20)30047-x [ Links ]
Kisely, S., Warren, N., McMahon, L., Dalais, C., Henry, I., & Siskind, D. (2020). Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ, 369:m1642. doi: 10.1136/bmj. m1642 [ Links ]
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., ... Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA, 3(3), e203976. doi: 10.1001/jamanetworkopen.2020.3976 [ Links ]
Li, S. H., & Graham, B. M. (2017). Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet Psychiatry, 4(1), 73-82. doi: 10.1016/ S2215-0366(16)30358-3 [ Links ]
Luo, M., Guo, L., Yu, M., Jiang, W., & Wang, H. (2020). The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - A systematic review and meta-analysis. Psychiatry Research, 291, 113190. doi: 10.1016/j.psychres.2020.113190 [ Links ]
Ornell, F., Schuch, J. B., Sordi, A. O., & Kessler, F. H. P. (2020). "Pandemic fear" and COVID-19: Mental health burden and strategies. Brazilian Journal of Psychiatry, 42(3), 232-235. doi: 10.1590/1516-4446-2020-0008 [ Links ]
Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G, Papoutsi, E., & Katsaounou, P. (2020). Prevalência de depressão, ansiedade e insônia entre os profissionais de saúde durante a pandemia de COVID-19: uma revisão sistemática e metanálise. Brain, Behavior, and Immunity, 88, 901-907. doi: 10.1016/j.bbi.2020.05.026 [ Links ]
Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B., & Xu, Y.(2020). A nation-wide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry, 33(2), e100213. 2020. doi: 10.1136/gpsych-2020-100213 [ Links ]
Rotenstein, L. S., Torre, M., Ramos, M. A., Rosales, R. C., Guille, C., Sen, S., & Mata, D. A. (2018). Prevalence of burnout among physicians: A systematic review. JAMA, 320(11), 1131-1150. doi: 10.1001/jama.2018.12777 [ Links ]
Salari, N., Khazaie, H., Amim, H.-F., Kazeminia, M., Mohammadi, M., Daneshkhan, A., & Eskandari, S. (2020). The prevalence of stress, anxiety and depression within front-line heathcare workers caring for COVID-19 patients: A systematic review and meta-regression. Human Resources for Health, 18, 100. doi: 10.1186/s12960-020-00544-1 [ Links ]
Sanghera, J., Pattani, N., Hashmi, Y., Varley, K. F., Cheruvu, M. S., Bradley, A., & Burke, J. R. (2020). The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting-A Systematic Review. Journal of Occupational Health, 62(1), e12175. doi: 10.1002/1348-9585.12175 [ Links ]
Santos, K. M. R., Galvão, M. H. R., Gomes, S. M., Souza, T. A., Medeiros, A. A., & Barbosa, I. R. (2021). Depressão e ansiedade em profissionais de enfermagem. Escola Anna Nery Revista de Enfermagem, 25(spe), e20200370. doi: 10.1590/2177-9465-EAN-2020-0370 [ Links ]
Silva, S. C. P. S., Nunes, M. A. P., Santana, V. R., Reis, F. P., Machado Neto, J., & Lima, S. O. (2015). A síndrome de burnout em profissionais da Rede de Atenção Primária à Saúde de Aracaju, Brasil. Ciência & Saúde Coletiva, 20(10), 3011-3020. doi: 10.1590/1413-812320152010.19912014 [ Links ]
Sinval, J., Queirós, C., Passian, S., & Marôco, J. (2019). Transcultural adaption of the Oldenburg, Burnout Inventory (OLBI) for Brazil and Portugal. Frontiers in Phychology, 10, 338. doi: 10.3389/fpsyg.2019.00338 [ Links ]
Sirois, F. M., & Owens, J. (2021). Factors associated with psychological distress in health-care workers during an infectious disease outbreak: A rapid systematic review of the evidence. Frontiers in Psychiatry, 11, 589545. doi: 10.3389/fpsyt.2020.589545 [ Links ]
Song, X., Fu, W., Liu, X., Luo, Z., Wang, R., Zhou, N., ... Lv, C. (2020). Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain, Behavior, and Immunity, 88, 60-65. doi: 10.1016/j.bbi.2020.06.002 [ Links ]
Szabó, M., & Lovibond, P. F. (2006). Anxiety, depression, and tension/ stress in children. Journal of Psychopathology and Behavioral Assessment, 28(3), 192-202. doi: 10.1007/s10862-005-9008-3 [ Links ]
Tironi, M. O. S., Teles, J. M. M., Barros, D. S., Vieira, D. F. V. B., Silva, C. M., Martins, D. F., ... Sobrinho, C. L. N. (2016). Prevalência de síndrome de burnout em médicos intensivistas de cinco capitais brasileiras. Revista Brasileira de Terapia Intensiva, 28(3), 270-277. doi: 10.5935/0103-507X.20160053 [ Links ]
Trevisan, R. L., Almeida, M. B. F., Baasch, D., Delben, P. B., Ródio-Trevisan, K. R., & Cruz, R. M. (2020). COVID-19: Clinical and epidemiological indicators of mental health in frontline professionals - A systematic review of the literature. Estudos de Psicologia (Natal), 25(3), 284-293. doi: 10.22491/1678-4669.20200029 [ Links ]
Vignola, R. C. B., & Tucci, A. M. (2014). Adaptation and validation of the depression, anxiety and stress scale (DASS) to Brazilian Portuguese. Journal of Affective Disorders, 155, 104-109. doi: 10.1016/j.jad.2013.10.031 [ Links ]
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus diease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. doi: 10.3390/ijerph17051729 [ Links ]
World Health Organization. (2020, January). Statement on the second meeting of the International Health Regulations (2005). Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Retrieved from https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-in-ternational-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) [ Links ]
 Endereço para correspondência:
Endereço para correspondência:
Avenida Nilo Peçanha, 301, Condomínio Floriano Cavalcante
Petrópolis, Natal/RN
CEP 59.012-300
Telefone: (84) 99680-3647
Email: fernandalnfreireuti@gmail.com
Received in 31.may.20
Revised in 21.sep.21
Accepted in 31.dec.21
Fernanda Lúcia Nascimento Freire Cavalcante, Mestre em Psicologia pelo Programa de Pós Graduação em Psicologia da Universidade Federal do Rio Grande do Norte (UFRN), é Psicóloga no Hospital Universitário Onofre Lopes – HUOL e no Hospital Giselda Trigueiro – HGT. ORCID: 0000-0001-6923-7696
Kamilla Sthefany Andrade de Oliveira, Mestre em Psicologia pelo Programa de Pós Graduação em Psicologia da Universidade Federal do Rio Grande do Norte (UFRN), é Psicóloga vinculada a Secretaria de Estado da Saúde Pública do Rio Grande do Norte - SESAP/RN. Email: millasthefany@gmail.com. ORCID: 0000-0001-6469-1523
Carla Larissa Fernandes Pinheiro Araújo, Mestre em Práticas de Saúde e Educação pela Universidade Federal do Rio Grande do Norte (UFRN), é Enfermeira Intensivista do Hospital Universitário Onofre Lopes (HUOL). Email: carlinhalfp@hotmail.com. ORCID: 0000-0001-8395-6275
Pedro Obede Medeiros Costa, Especialista em Psicologia da Saúde pela Universidade Federal do Rio Grande do Norte (UFRN), é Psicólogo Clínico (autônomo). Email: pedro.obedepsi@outlook.com. ORCID: 0000-0001-6964-5323
Eliane Pereira da Silva, Mestre em cardiologia pela Universidade Federal de São Paulo (UNIFESP), é Professora Assistente da Universidade Federal do Rio Grande do Norte (UFRN) e Chefe da Unidade de Cuidados Intensivos e Semi Intensivos do Hospital Universitário Onofre Lopes (UFRN). Email: eliane.pereira@ufrn.br. ORCID: 0000-0002-3364-5046
Eulália Maria Chaves Maia, Doutora em Psicologia Clínica pela Universidade de São Paulo (USP/SP), é Professora Titular e bolsista de produtividade (CNPq) da Universidade Federal do Rio Grande do Norte (UFRN). Email: eulalia.maia@yahoo.com.br. ORCID: 0000-0002-0354-7074














