Serviços Personalizados
artigo
Indicadores
Compartilhar
Temas em Psicologia
versão impressa ISSN 1413-389X
Temas psicol. v.16 n.1 Ribeirão Preto jun. 2008
ARTIGOS
General distress, posttraumatic stress symptoms, and coping strategies in parents of children with cancerI
Estrella Durá FerrandisI; Yolanda Andreu VailloI; María José Galdón GarridoI; Sonia Hernández LópezII; Concepción López SolerII,III
I Universidad de Valencia
II Hospital Universitario Virgen de la Arixaca de Murcia
III Universidad de Murcia
ABSTRACT
This study assesses symptoms of emotional and post-traumatic distress in 73 parents of children with cancer, as well as coping strategies adopted by these parents. A comparison of 35 parents whose child is in the treatment stage vs. 38 parents whose child has already ended the treatment was carried out and differences between both subgroups were not found in any of the considered variables. Reviewing the total sample, an estimated prevalence of clinically significant emotional distress has been obtained in 36% of the parents and clinically significant symptoms of post-traumatic stress in 49% of the cases. Coping strategies that predict greater emotional distress and greater symptoms of post-traumatic stress are guilt and denial. Implications are derived at the level of psychological intervention in parents of child cancer patients.
Keywords: Distress, Posttraumatic stress, Coping, Parents, Childhood cancer.
Survival in childhood cancer has substantially increased in recent years. (Brenner, 2003; Gatta, Capocaccia, Coleman, Gloeckler Ries, & Berrino, 2002). The survival rate in Spain, in particular, has increased from 54% between 1980 and 1984 to 74% between 1997 and 2000 (Peris & Giner, 2006). Despite this, diagnosis and treatment of childhood cancer represents a highly threatening situation both for the children and their families, especially parents and siblings. Throughout the diagnosis and treatment process of childhood cancer, both the child and the parents are confronted with multiple stressors ranging from hospitalization and aggressive treatments with side effects to the threat of death, while undergoing considerable changes in daily routines and alterations in family and social roles.
Psychological factors in children who have (or have had) cancer have been widely studied. Psychosocial repercussions most frequently cited are: mood changes, irritability (in occasions in form of anger toward the parents and health care staff), separation anxiety, withdrawal, fear of medical procedures, sadness, changes in sleep behavior and dreams (nightmares), anorexia, silence and regressive behavior, among others. Moreover, these reactions may vary in intensity. In some cases, they can be considered as normal adaptive reactions in handling a situation whereas, in other cases, they can become so intense that they lead to more serious psychopathological disorders, such as adaptive and behavioral disorders, behavioral changes or posttraumatic stress symptoms, regressive syndrome, depression and anxiety, mainly (for revision: Die-Trill, 2000, 2003; Die-Trill & Stuber, 1998; Eiser, 2004; Hill & Stuber, 1998).
Studies on this topic have also indicated a series of variables that influence these effects, such as the type of treatment, the age and maturity level of the sick child, variables of the illness itself (type of cancer, prognosis), the existence of genetic associations to specific illnesses, the way in which each family member reacts and copes with the childs illness, the characteristics of family functioning, the presence of other concurrent stressors, social and economic support available and the sociocultural environment, among other factors.
The childs family has been pointed out to be a central element and key to the stress adaptation process of the child to the illness, influencing this process and helping to explain, together with other factors, the variability of results obtained by empirical studies which analyze psychological reactions of children with cancer coming to terms with their illness (Kazak, Simms, & Rourke, 2002; Robinson, Gerhardt, Vannatta, & Noll, 2007). Furthermore, the family itself suffers a series of psychosocial consequences arising from the diagnosis and treatment of the childs illness. Numerous studies have demonstrated that the diagnosis of cancer in a child provokes a crisis, which presents challenges both to the stability and adaptive functioning of the entire family system. The psychological and social welfare of the family and, in particular the parents, is seen as enormously affected by the uncertainty of the diagnosis (Allen, Newman, & Souhami, 1997), by the immediate experience of seeing the child suffer (Enskär, Carlsson, Golsater, Hamrin, & Chesney, 1997), the concerns regarding the efficacy of the therapeutic procedures and the quality of care (Lozowski, Chesler, & Chesney, 1993), the side effects of the treatment (Bryant, 2003), the long-term consequences (Pendley, Dahlquist, & Dreyer, 1997), the change in daily routine and social structure of the family (Kazak et al., 2002; Woodgate, Degner, & Yanofsky, 2003) and even the consequences at the economic and professional level (Sloper, 1996).
Most studies on parents of children with cancer have focused on identifying the presence of different psychological distress symptoms: mainly anxiety, depression, mental health, psychosomatic symptoms, stress symptoms, posttraumatic stress, problems in the relationship of the couple and quality of life. The results, in general, indicate that parents of children with cancer experience psychological problems and symptoms of distress above the normal population or in comparison with groups of parents of healthy children (Dahlquist et al., 1993; Grootenhuis & Last, 1997; Hoekstra-Weebers, Jaspers, Kamps, & Klip, E., 1998; Kazak et al., 1997; Sawyer, Antoniou, Toogood, Rice, & Baghurst, 1993). However, other studies have not found differences at the level of psychological adaptation among parents of children with cancer and comparison groups (Radcliffe, Bennet, Kazak, Foley, & Phillips, 1996; Speechley & Noh, 1992). This discrepancy in the results might be due to several methodological factors including a small sample size in some studies, and, above all, the sample heterogeneity regarding the specific type of diagnosis of the children, the medical treatment received, the age of the children at the moment of diagnosis and at the time of psychological assessment of the parents, or the time passed since the moment of diagnosis (Klassen, Raina, Reineking, Dix, Pritchard, & O´Donnell, 2007; Pai, Greenley, Lewandowski, Drotar, Youngstrom, & Peterson, 2007).
Moreover, it has been noted that several psychosocial variables can modulate the adaptation response of parents coming to terms with the illness of their child. Among those that stand out are: previously established family dynamics and structure, the way the family communicates, their cultural and spiritual values, personality characteristics of each parent, if they have more children or not, previous experience with cancer, the network of social support available to the nuclear family, the existence of other situations that generate tension simultaneously affecting this nuclear family or the coping strategies and attitudes of each member towards the illness itself (Die-Trill & Kovalcik, 1997; Fadiman, 1997; McDaniel, Hepworth, & Doherty, 1992; Rowland, 1989; for revision see Klassen et al., 2007).
In this research context, the present study analyzes general and posttraumatic distress in a sample of parents of children with cancer and their relation with possible modulating variables related with both the illness (stage) and with certain characteristics of the parents (coping strategies adopted to confront the illness).
Method
Sample and procedure
The sample comes from the Pediatric Oncohematology Unit at the Hospital Universitario Virgen de la Arrixaca in Murcia, the only reference center in this Autonomous Region for the treatment of childhood cancer. The initial sample was made up of a parent (father or mother) of each of the children cared for at this unit between December 2001 and October 2005 and met the following inclusion criteria: diagnosis of a malignant tumor in the child (benign tumor patients were ruled out), Spanish was the native language both for the child and parent, and there was no evident presence of mental retardation or serious mental disturbance in the child or the parent. The final sample was made up of a total of 73 parents, 56 of whom were mothers and 17 fathers. The average age of the mothers was 35 (SD=6.22) and of the fathers was 39 (SD=4.11).
With regard to the characteristics of the children, it is worth mentioning the following: 40 boys (55%) and 33 girls (45%), with ages ranging between 9 months and 17 years old (the average was 7 years and 6 months, with a standard deviation of 3 years and 7 months). Of those, 35 (48%) were undergoing active medical treatment at the time of assessment of the parents for this study, whereas 38 (52%) had completed treatment and were attending medical follow-ups (the time range since the end of the treatment was from one month to seven years). Regarding the medical diagnosis, the most frequent tumors were leukemia (N=23, 31.5% of the sample), and the central nervous system (N=18, 24.7% of the sample). The rest of the diagnosis did not affect more than five cases in the sample and included the following: Hodgkins lymphoma, LAM, Neuroblastoma, Histiocytosis, Non-Hodgkins lymphoma, Wilms tumor, Rhabdomyosarcoma and Non-rhabdomyosarcoma soft tissue sarcoma. With regard to medical treatment, the majority had received only chemotherapy (N=31, 42.5% of the sample); 13 (17.8%) had undergone a bone marrow transplant, combined with or without other treatments; 10 had received surgery plus chemotherapy (13.7%); and the rest had received different combinations of surgical treatment, chemotherapy and/or radiation therapy (in no case did these different combinations affect more than 5 subjects in the sample).
The sample assessment was carried out in a hospital by a trained psychologist. Informed consent was requested from the parents in order to participate in this study and in all cases the responses were anonymous.
Instruments used and variables assessed
Brief Symptom Inventory 18 (BSI-18) (Derogatis, 2001). A self-report measure made up of 18 items recorded on a 5-point Likert-type scale – from 0 (nothing) to 4 (a lot). The subject has to respond to each item in terms of how he/she has felt in the past seven days. The instrument enables obtaining a total score (GSI, Global Severity Index), from the sum of all of these items, and a score for each of the three scales – somatization, depression and anxiety – which comprise the instrument. Each of these is made up of 6 items. The somatization scale reflects discomfort caused by the perception of body problems, focusing on symptoms that appear in cardiovascular, gastrointestinal, or other systems related to the autonomous nervous system. The depression scale makes reference to the wide range of symptoms present in clinical depression such as negative affect, anhedonia, hopelessness and/or suicide ideation. Lastly, the anxiety scale considers a series of symptoms present in the majority of anxiety disorders, such as nervousness, tension, motor restlessness or apprehension.
Although the BSI-18 is a recently created instrument, it derives from widely-used instruments (BSI and SCL-R-90) that have demonstrated highly-satisfactory psychometric properties (Derogatis, 2001). For this study, the translation and adaptation to Spanish carried out by Derogatis (2001) himself was used. Instrument reliability (internal consistency) in our sample was adequate, both for the total score (.91), and for subscales (.82 in three cases).
Impact of Event Scale-Revised (IES-R) (Weiss & Marmar, 1997). A self-report measure consisting of 22 items that assess, through a 4-point Likert scale, the three symptom clusters characteristic of posttraumatic stress following the DSM-IV criteria: intrusion (7 items), avoidance (8 items), and arousal (7 items). The instrument enables obtaining a total score from the sum of the scores in all scale items. The instrument assesses the degree in which these symptoms have appeared as a response to a particular stressor, in this case the illness of the child, in the past week.
Both the IES-R and the original IES scale (Horowitz, Wilner, & Alvarez 1979) have been widely used in the oncology population, including children with cancer and their parents. The instrument reliability (internal consistency) in our sample was the following: total score .92, Intrusion .85, Avoidance .75 and Arousal .81.
Brief COPE (Carver, 1997). A self-report measure from the original COPE Inventory (Carver, Scheier, & Weintraub 1989) based on Lazarus and Folkmans coping model (1984) and self-regulation of behaviour (Carver & Scheier 1981, 1990). The COPE Inventory, made up of 60 items grouped into 15 scales referring to different styles of coping with stress, has demonstrated its psychometric bond in numerous studies related to health (Carver, Scheier, & Weintraub 1989). The abbreviated version reduces the number of items to 28 and the scales or coping strategies to 14. Although this version has been used in fewer studies, the brevity of the instrument was best for our research.
The coping strategies assessed by the Brief COPE are the following: Self-distraction (evasion mechanism through the use of active distraction); Active coping (carrying out actions and make efforts to eliminate or alleviate the problem); Denial (attempting to reject the reality of the stressful event); Substance use (drinking alcohol or taking other substances to cope with the stressor); Use of emotional support (obtaining sympathy or emotional support from other persons); Use of instrumental support (looking for help, information or advice on what to do); Behavioral disengagement or Claudication (giving up any effort or abandoning any attempt to reach an objective the problem is interfering with); Venting (placing more attention on the emotional discomfort itself, accompanied by a tendency to express or unload these feelings); Positive reframing (ability of the subject to make the most of the situation with the aim of developing oneself as a person or viewing it from a more favorable perspective); Planning (thinking of how to handle the stressor and planning active coping efforts); Humor (joking about the problem or the situation); Acceptance (accepting the fact that the event has occurred and is real, as well as how to live with it); Religion (becoming more involved in religious or spiritual activities, praying or meditating); Self-blame (criticizing and blaming oneself for the presence of the stressor).
Reliability analysis (internal consistency) of the instrument scales in our sample show that five did not reach a satisfactory Cronbachs alfa (less than .60), so it was decided not to use them in this study. The Substance use scale was eliminated due to its null variability. The scales maintained in our analysis and the reliability indices reached were the following: active coping (.76), denial (.80), use of emotional support (.77), use of instrumental support (.80), positive reframing (.74), acceptance (.77), religion (.86), and self-blame (.82).
Analyses performed
In the first place, multiple variable analyses were conducted to contrast the considered psychological variables in the two subgroups of parents: those whose child was undergoing treatment and those whose child had already completed treatment and were attending regular medical follow-ups. In the second place, descriptive analyses were performed to estimate the prevalence of significant clinical symptoms at the general distress and posttraumatic stress level. Lastly, several regression analyses were performed considering, as a dependent variable, the total scores of general distress and posttraumatic stress symptomatology on the one hand, and their respective subscales on the other; in all cases the predictor variables considered were the coping strategies assessed by the Brief COPE.
The statistics package SPSS, version 14 was used.
Results
1. Differences between the subgroup of parents whose child was undergoing treatment (N=35) and the subgroup of parents whose child was in the follow-up stage (N=38)
Before analyzing the differences in psychological variables (general distress, posttraumatic stress symptoms, and coping strategies) between the two subgroups of parents, homogeneity between both groups in other variables was established in order to rule out the existence of differences in these latter variables that could be modulating possible differences between both groups in the assessed psychological variables. None of the analyzed variables (sex of the child, age of the child at the moment of diagnosis, or the sex of the parent being assessed) showed statistically significant differences between both subgroups of parents.
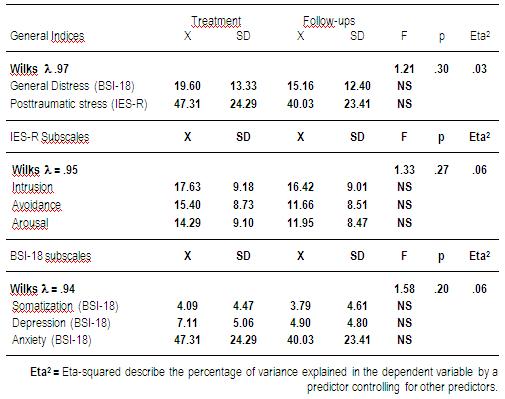
The results obtained for the psychological variables in Table 1 show that the group of parents of children who were undergoing treatment or attending follow-up visits did not differ in the general distress indices or in the posttraumatic stress symptomatology (Wilks λ= 0.97; F= 1.21, p=0.30). Likewise, differences were not observed between these groups of parents in the scales that integrate both indices. Multivariate analysis of the variance was not significant in the dimensions of the IES-R (Wilks λ= 0.95; F= 1.33; p=0.27) or the BSI-18 (Wilks λ= 0.94; F= 1.58, p=0.20).
Table 1: MANOVAs and post-hoc tests. Means and standard deviations of the BSI-18 and the IES-R and their respective subscales in groups of parents of children undergoing treatment (N=35) and attending follow-up visits (N=38).
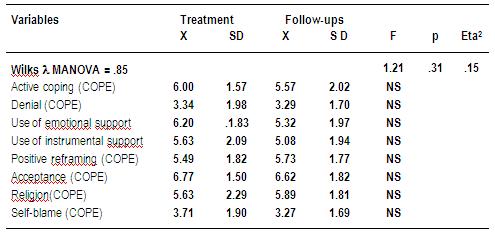
Moreover, the multivariate analysis regarding the coping style used by the childrens parents (see Table 2) did not reveal differences according to the follow-up or treatment groups, and thus was not significant overall (Wilks λ= 0.85; F= 1.21, p=0.31).
Table 2: MANOVA and post-hoc tests. Mean and standard deviation of the Brief COPE subscales in groups of parents of children undergoing treatment (N=35) and follow-ups (N=38).
It was decided to consider the total sample of parents (N=73) in the following analyses since the stage of the childs illness (treatment or follow-up) did not establish differences in the symptomatology of general and posttraumatic distress that the parents exhibit, or in coping strategies that parents adopt to confront the illness of their child.
2. Prevalence of general distress and posttraumatic stress disorder in the total sample (N= 73)
In order to estimate the percentage of patients having a clinically significant general distress response in the study sample, the criterion proposed by Derogatis (2001) in the BSI-18 manual was taken in account. This criterion consists of identifying all of those subjects that have obtained a T-score of 63 or above in the general distress index (GSI), as well as adding all those cases with T-scores of 63 or above in two of the three instrument subscales – somatization, depression and anxiety – without reaching this score in the total. For the conversion of direct-scores in T-scores, Derogatis suggests to follow standards designed for the normal population in which the T-score of 63 corresponds to the 90th percentile.
Using this criterion, the results show that 35.6% of our sample (26 parents) showed clinical symptoms of general distress versus 64.4% (47 parents) that did not.
In order to estimate the prevalence of PTSD, the symptom method has been followed, used by a large number of authors when estimating the prevalence of clinical cases of PTSD from self-report questionnaires (Andrykowski & Cordova, 1998; Andrykowski, Cordova, McGrath, Sloan, & Kennady, 2000; Cordova, Studts, Hann, Jacobsen, & Andrykowski, 2000; Kornblith et al., 2003; Norberg, Lindblad, & Boman, 2005b; Smith, Redd, Peyser, & Vogl, 1999). This procedure is based on prevalence after meeting the criteria referring to symptoms established in the DSM-IV, and assessed from the questionnaire items. In our case, the responses to each item were dichotomized considering the response categories sometimes and often as symptom presence and considering the categories never and seldom as symptom absence. Finally, we think a person is susceptible to a PTSD diagnosis when symptom presence is shown in: i) at least one of the seven items that make up the intrusion subscale; ii) at least two of the seven items that make up the arousal subscale; and iii) at least three of the eight items that make up the avoidance subscale.
Using the aforementioned estimation criterion of PTSD prevalence, the results reveal that 36 parents (49.3 %) showed clinical posttraumatic stress symptoms, versus 37 parents (50.7%) that did not.
3. Predictors of general distress and the posttraumatic stress symptoms in the total sample (N=73)
Prior to regression analysis, correlations were obtained between the considered predictor variables (coping strategies assessed by the Brief COPE) and the criteria variables (general and posttraumatic stress, both total score and subscales), with the aim of including in regression analysis only those variables that showed significant correlations with the corresponding criterion.
The analysis of correlations (see Table 3) shows that the correlated variables with general distress are denial (r=.31, p≤.01), positive reframing (r= -0.24; p≤.01) and self-blame (r= 0.34; p≤.01). The three dimensions of BSI-18 correlated with denial (r= 0.29, p≤.05; r=0.26, p≤.05; r=0.28, p≤.05, respectively) and self-blame (r= 0.28, p≤.05; r=0.36, p≤.01; r=0.25, p≤.05, respectively). In the case of depression, positive reframing (r=-0.28, p≤.05) is added.
Table 3: Significant correlations between predictor variables (coping Brief COPE) and dependent variables (IES-R and BSI-18) (N=73).
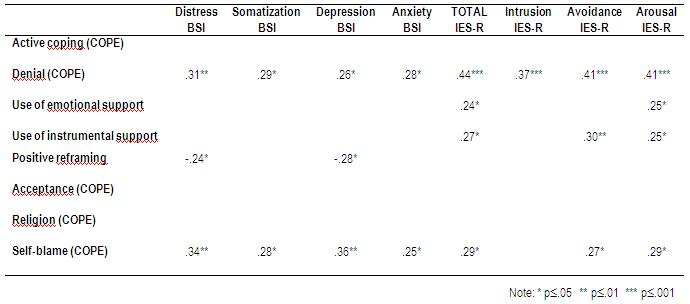
With respect to posttraumatic stress symptoms, the general index correlated with denial (r= 0.44, p≤.001), with the use of both emotional and instrumental support (r= 0.24, p≤.05 and r=0.27, p≤.05) and self-blame (r= 0.29, p≤.05). Finally regarding the IES-R scales, intrusion correlated only with denial (r= 0.37, p≤.001), whereas avoidance and arousal scales correlated with the same coping strategies as the general index, with similar Pearson values and significance (r= 0.41, p≤.001 with denial in both cases; r= 0.25, p≤.05 between both types of use of emotional support and arousal; r= 0.30, p≤.05 between the use of instrumental support and avoidance; and r=0.27 and r=0.29, p≤.05 between self-blame and both scales of posttraumatic symptoms, respectively).
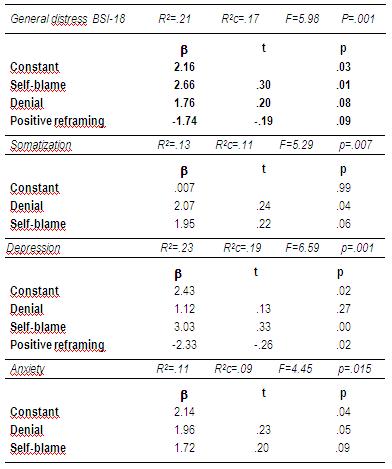
The results of regression analyses reveal that, with regard to general distress (see Table 4), self-blame was the only significant variable (p<0.01), explaining 17% of the score variance (p<0.001). Regarding the distress dimensions, denial (p<0.05) explained 11% of the variance in somatization scores (p<0.01), and 9% of the variance in anxiety scores (p<0.01); meanwhile, self-blame (p<0.001) and positive reframing (p<0.02) were able to explain 19% of the depression scores (p<0.001).
Table 4: Regression analysis. Dependent variables: General distress and subscales (BSI-18). Predictor variables: coping strategies (Brief COPE) (N=73).
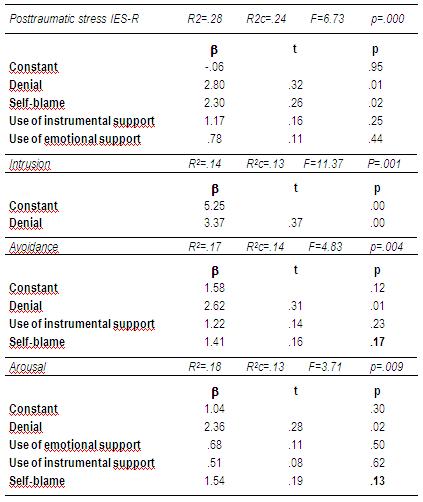
Regarding the total posttraumatic stress symptomatology (see Table 5), the proportion of explained variance reached 24% (p<0.001) from significant contributions of self- blame (p<0.01) and denial (p<0.01). In the case of posttraumatic stress subscales, denial was the only significant predictor in all cases (p<0.001; p<0.01; p<0.05, respectively), explaining 13%, 14% and 13% of the variance in intrusion, avoidance, and arousal scores, respectively.
Table 5: Regression analysis. Dependent variables: Posttraumatic stress and subscales (IES-R). Predictor variables: coping strategies (Brief COPE) (N=73).
Discussion
The negative impact that a cancer diagnosis in a child has on the psychological welfare of their parents is a widely documented issue. Empirical research on this topic currently attempts to study the factors that modulate this impact in depth, with the aim of specifically orientating psychological interventions directed at reducing distress in parents and that, on occasions, may reach clinically significant levels (Klassen et al., 2007).
One of these factors that seem especially relevant is the time period since the diagnosis and, in relation with this, if the child is still undergoing treatment or has already completed treatment. Several studies have concluded that distress in parents increases during the diagnostic stage but decreases until reaching normal levels throughout the first two years after diagnosis (Dahlquist, Czyzewski, & Jones, 1996; Hoekstra-Weebers et al., 1999; Grootenhuis & Last, 1997; Patenaude & Kupst, 2005; Sahler et al., 2002), although 25-33% of parents continue exhibiting clinically significant distress (Boman et al., 2003; Kupst et al. 1995; Hoekstra-Weebers et al., 1999; Kazak et al., 2003; Wijnberg-William, Kamps, Klip, & Hoekstra-Weebers, 2006). The most recent revisions and meta-analysis on this topic (Klassen et al., 2007; Pai et al. 2007) confirm that distress in parents is greater around the time of diagnosis, making the first year after diagnosis the most vulnerable period.
In our study, we have not found statistically significant differences at the distress level between parents whose child is undergoing treatment and those whose child has already completed treatment. Two characteristics of our study may have limited reaching clear conclusions. On the one hand, its transversal design is less sensitive to changes that occur over time than longitudinal designs, which are more methodologically adequate to deal with this issue. On the other hand, the variable spans of time since ending treatment in the subgroup of parents whose child had already completed treatment (from one month to seven years) confers a heterogeneous character to this subgroup, making it difficult to outline the psychological impact in parents according to the time passed since the diagnosis of the child.
Despite these limitations, the relatively wide sample of parents in our study (N=73), considering both subgroups, enables analyzing other aspects of great relevance in the context of research on psychological distress in parents of children with cancer, such as its prevalence and predictors. In this study we have assessed two types of psychological distress: general and posttraumatic (in the latter case, considering any aspect related with the childs illness as a stressful event).
With regard to general distress, the prevalence estimated in clinically significant cases in our sample (35%) is slightly higher than prevalence found in other studies (around 25-33%, as we indicated previously), thereby confirming that an important percentage of parents of children with cancer exhibit psychological symptoms, as a result of the childs illness, which may lead to psychological disorders requiring professional assistance; in addition, our results indicate that this symptomatology might be prolonged over time, affecting parents even years after medical treatment has ended.
Regarding the estimated prevalence of posttraumatic stress in our sample, results reveal that 49% of parents show posttraumatic stress symptoms that would be susceptible to a psychiatric diagnosis of posttraumatic stress disorder (PTSD). The results of the studies on this topic have shown a wide range of prevalence of PTSD from 6-10% (Barakat et al., 1997; Kazak et al. 1997; Manne, Du Hamel, Gallelli, Sorgen, & Redd, 1998) to 71% (Landolt, Boehler, Schwager, Schallberger, & Nuessli, 1998), while other studies have revealed moderate values between 25% and 40% (Brown, Madan-Swain, & Lambert, 2003; Kazak et al., 2004; Niles, 1996; Pelcovitz et al. 1996; Stuber, Christakis, Houskamp, & Kazak, 1996). These diverse results have brought up several issues related with both applicability of the PTSD concept to the case of cancer as well as its assessment. From a theoretical perspective it is thought that cancer in general, and pediatric cancer in particular, may not adequately adjust to the concept of ¨traumatic event¨ susceptible of provoking PTSD symptoms (Phipps, Larson, Long, & Rai, 2006; Phipps, Long, Hudson, & Rai, 2005; Stuber, Kazak, Meeske, & Barakat, 1998; for revision see Pérez & Galdón, 2001). At the methodological level, clear existing differences are noted among those studies that have assessed the prevalence of PTSD as a clinical syndrome, using structured clinical interviews with diagnostic aims and the others, the majority, that have used self-report instruments measuring posttraumatic symptoms but do not enable establishing a definitive clinical diagnosis, only an estimation from the presence of clinically significant symptoms.
Despite these controversies and difficulties, the majority of authors agree on the need to continue researching posttraumatic stress reactions in the oncology population and in family members, given the interest for clinical practice. Thus, it is pointed out that knowing the specific posttraumatic stress symptoms, even though the criteria of psychiatric diagnosis are not met or a diagnosis is not carried out, might help professionals to identify and attend to the specific issues of the patients or parents of the child in a more adequate way (Kazak Boeving, Alderfer, Hwang, & Reilly, 2005; Norberg et al., 2005b). The majority of studies dealing with psychological aspects of parents of children with cancer have focused on, as we have seen, general psychological distress, showing mainly the emotional symptomatology of anxiety and depression. As an addition, assessment of intrusive thoughts that assail parents about diagnosis or other aspects related to the illness and treatment of their child, assessment of physiological arousal associated with these memories, and assessment of cognitive and behavioral efforts to avoid thoughts about the illness of their child, common in an important percentage of parents as shown reiteratively in the bibliography, may facilitate the professional in identifying more specific symptomatology, and above all, in the development of psychological intervention strategies to help cope with it.
Furthermore, the identification of risk factors than can favor the development of this type of symptomatology in parents of children with cancer allows early detection in those at greater risk. In this respect, our study has analyzed coping strategies adopted by parents to come to terms with their childs illness as symptom predictors in both general and posttraumatic distress. The results have identified two strategies that predict greater psychological distress in parents: Denial and Self-blame (although the former only showed a tendency of significance as a predictor of general distress). Denial turned out to be, in addition, the only predictor of all the specific symptoms of posttraumatic stress (intrusion, avoidance, and arousal) and, together with self-blame (although this only showed a tendency of significance) of two of the specific symptoms of emotional distress (somatization and anxiety). Moreover, self-blame, together with positive reframing (in reverse order), specifically predicted the symptoms of depression.
Thus, according to our results, rejecting the reality of what happened or blaming oneself is clearly shown as maladaptative coping strategies in parents of children with cancer, associated with greater general distress and posttraumatic stress symptoms. Of the remaining strategies, only positive reframing appears as a predictor in the specific case of depression, revealing itself as an adaptive strategy: the parents who are able to perceive positive or favorable aspects in what happened show less depressive symptomatology. These results coincide with those obtained by the scarce studies that have assessed the relation between specific coping strategies adopted by parents of children with cancer and psychological distress shown by the parents: all point out that avoidance strategies, versus active strategies or focused on the problem, are associated with greater distress (Norberg, Lindblad, & Boman, 2005a; Sloper, 2000; Trask et al., 2003; Wittrock, Larson, & Sandgren, 1994).
To sum up, our study demonstrates that childhood cancer provokes, in parents of these children, general distress and posttraumatic stress symptomatology that can reach clinically significant levels in an important percentage of cases, even once the medical treatment has finished and several years later. Furthermore, our study demonstrates that psychological stress is associated with the adoption of avoidance coping strategies by parents confronting the illness of their child. This all leads to the need to offer programs of psychological attention to parents of children with cancer in order to reduce emotional and cognitive psychopathology that they may present, and thus training parents specifically in the adoption of the coping strategies that seem to be more effective to psychologically adapt themselves.
References
Allen, R., Newman, S. P., & Souhami, R. L. (1997). Anxiety and depression in adolescent cancer: findings in patients and parents at the time of diagnosis. European Journal of Cancer, 33(8), 1250-1255. [ Links ]
Andrykowski, M., & Cordova, M. (1998). Factors associated with PTSD symptoms following treatment for breast cancer: Test of Andersen Model. Journal of Traumatic Stress, 11(2), 189-203. [ Links ]
Andrykowski, M., Cordova, M., McGrath, P., Sloan, D., & Kennady, D. (2000). Stability and change in posttraumatic stress disorder following breast cancer treatment: A 1 year follow-up. Psycho-oncology, 9(1), 69-78. [ Links ]
Barakat, L., Kazak, A., Meadows, A., Casey, R., Meeske, K., & Stuber, M. (1997). Families surviving childhood cancer: A comparison of posttraumatic stress symptoms with families of healthy children. Journal of Pediatric Psychology, 22, 843-859. [ Links ]
Boman, K., Lindahl, A., & Bjork, O. (2003). Disease-related distress in parents of children with cancer at various stages alter the time of diagnosis. Acta Oncologica, 42, 137-146. [ Links ]
Brenner, H. (2003). Up-to-date survival curves of children with cancer by period analysis. British Journal of Cancer, 88, 1693-1697. [ Links ]
Brown, R. T., Madan-Swain, A., & Lambert R. (2003). Posttraumatic stress symptoms in adolescent survivors of childhood cancer and their mothers. Journal of Traumatic Stress, 16, 309-18. [ Links ]
Bryant, R. (2003). Managing side effects of childhood cancer treatment. Journal of Pediatric Nursing, 18, 113-125. [ Links ]
Carver, C. S. (1997). You want to measure coping but your protocol´s too long: Consider the Brief COPE. International Journal of Behavioral Medicine, 4, 92-100. [ Links ]
Carver, C. S., & Scheier, M. F. (1981). Attention and self regulation: A control theory approach to human behaviour. New York: Springer-Verlag. [ Links ]
Carver, C. S., & Scheier, M. F. (1990). Principles of self regulation. Action and emotion. In: E.F. Higgins & R.M. Sorrentino (Eds.), Handbook of motivation and cognition: Foundations of social behaviour (pp. 3-52). New York: Guilford. [ Links ]
Carver, C. S., Scheier, M. F., & Weintraub, J. K. (1989). Assessing coping strategies: A theoretically bases approach. Journal of Personality and Social Psychology, 56, 267-283. [ Links ]
Cordova, M. J., Studts, J. L., Hann, D. M., Jacobsen, P. B., & Andrykowski, M. A. (2000). Symptom structure of PTSD following breast cancer. Journal of Traumatic Stress, 13, 301-319. [ Links ]
Dahlquist, L., Czyzewski, D., & Jones, C. (1996). Parent of children with cancer: A longitudinal study of emotional distress, coping styles, and marital adjustment two and twenty months after diagnosis. Journal of Pediatric Psychology, 21, 541- 554. [ Links ]
Dahlquist, L., Czyzewski, D., Copeland, K., Jones, C., Taub, E., & Vaughan, J. (1993). Parents of children newly diagnosed with cancer: Anxiety, coping and marital distress. Journal of Pediatric Psychology, 18, 365-376. [ Links ]
Derogatis L. R. (2001). Brief Symptom Inventory 18 (BSI-18). Minneapolis: National Computer Systems Pearson, Inc. [ Links ]
Die-Trill, M. (2000). El reto de enfrentarse a un cáncer infantil: Trastornos psicológicos y psiquiátricos más frecuentes y su tratamiento. In: F. Gil (Ed.), Manual de Psico-oncología (pp. 109-136). Barcelona: Nova Sidonia – Oncología. [ Links ]
Die-Trill, M. (2003). El niño y el adolescente con cáncer. In:M. Die-Trill (Ed.), Psico-Oncología (pp. 85-101). Madrid: Ades. [ Links ]
Die-Trill, M., & Kovalcik, R. (1997). The child with cancer. Influence of culture on truth-telling and patient care. Annals of the New York Academic of Sciences, 809, 197-210. [ Links ]
Die-Trill, M., & Stuber, M. L. (1998). Psychological problems of curative cancer treatment. In: J. C. Holland (Ed.), Psycho-Oncology (pp. 897-906). New York: Oxford University Press. [ Links ]
Eiser, C. (2004). Children with Cancer. The Quality of Life. Mahwah, New Jersey: Lawrence Erlbaum Associates Publishers. [ Links ]
Enskär, K., Carlsson, M., Golsater, M., Hamrin, E., & Chesney, (1997). Parental reports of changes and challenges that result from parenting a child with cancer. Journal of Pediatric Oncology Nursing, 14(3), 156-163. [ Links ]
Fadiman, A. (1997). The spirit catches you and you fall down. New York: Farrar, Straus & Giroux. [ Links ]
Gatta, G., Capocaccia, R., Coleman, M. P., Gloeckler Ries, L.A., & Berrino, F. (2002). Childhood cancer survival in Europe and the United States. Cancer, 95 (8), 1767-1772. [ Links ]
Grootenhuis, M. A., & Last, B. F. (1997). Predictors of parental emotional adjustment to childhood cancer. Psycho-Oncology, 62, 115-128. [ Links ]
Hill, J. M., & Stuber, M. L. (1998). Long-term adaptation, psychiatric sequelae, and posttraumatic stress disorder. In: J. Holland (Ed.), Psycho-Oncology (pp. 923-929). New York: Oxford University Press. [ Links ]
Hoekstra-Weebers, J. E., Jaspers, J. P., Kamp, W. A., & Klip, E. C. (1999). Risk factors for psychological maladjustment of parents of children with cancer. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1526-1535. [ Links ]
Hoekstra-Weebers, J., Jaspers, J., Kamps, W., & Klip, E. (1998). Marital dissatisfaction, psychological distress and the coping of parents of pediatric cancer patients. Journal of Marriage and the Family, 60, 1012-1021. [ Links ]
Horowitz, M J., Wilner, M., & Alvarez, W. (1979). Impact of Events Scale: A measure of subjective stress. Psychosomatic Medicine, 41, 209-218. [ Links ]
Kazak, A. E., Alderfer, M., Rourke, M., Simms, S., Streisand, R., & Grossman, J. (2004). Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. Journal of Pediatric Psychology, 29, 211-219. [ Links ]
Kazak, A. E., Barakat, L., Meekske, K., Christakis, D., Meadows, A., Casey, R., Penati, B., & Stuber, M. L. (1997). Posttraumatic stress, family fuctioning, and social support in survivors of childhood leukemia and their mothers and fathers. Journal of Consulting and Clinical Psychology, 65, 120-129. [ Links ]
Kazak, A. E., Boeving, C. A., Alderfer, M. A., Hwang, W., & Reilly, A. (2005). Posttraumatic stress symptoms during treatment in parents of children with cancer. Journal of Clinical Oncology, 23(30), 7405-7410. [ Links ]
Kazak, A. E., Cant, C., Jensen, M. M., McSherry, M., Rourke, M. T., Hwang W., Alderfer, M. A., Beele, D., Simms, S., & Lange, B. C. (2003). Identifying psychosocial risk indicative of subsequent resource use in families of newly diagnosed oncology patients. Journal of Clinical Oncology, 21, 3220-3225. [ Links ]
Kazak, A., Sims, S., & Rourke, M. T. (2002). Family systems practice in pediatric psychology. Journal of Pediatric Psychology, 27, 133-143. [ Links ]
Klassen, A., Raina, P., Reineking, S., Dix, D., Pritchard, S., & O´Donnell, M. (2007). Developing a literature base to understand the caregiving experience of parents of children with cancer: a systematic review of factors related to parental health and well-being. Support Care Cancer, 15, 807-818. [ Links ]
Kornblith, A. B., Herndon, J. E., Weiss, R. B., Zhang, Ch., Zuckerman, E. L., Rosenberg, S., Mertz, M., Payme, D., Massie, M. J., Holland, J. F., Wingate, P., Norton, L., & Holland, J. C. (2003). Long-term adjustment of survivors of early-stage breast carcinoma, 20 years after adjuvant chemotherapy. Cancer, 98(4), 679-689. [ Links ]
Kupst, M., Natta, M., Richardson, C., Schulman, J., Lavigne, J., & Das, L. (1995). Family coping with pediatric leukaemia: Ten years after treatment. Journal of Pediatric Psychology, 20, 601-617. [ Links ]
Landolt, M. A., Boehler, U., Schwager, C., Schallberger, U., & Nueslli, R. (1998). Post-traumatic stress disorder in paediatric patients and their parents: an exploratory study. Journal of Paediatrics and Child Health, 34, 539-543. [ Links ]
Lazarus, R. S., & Folkman, S. (1984). Stress, Appraisal and Doping. New Cork: Springer. [ Links ]
Lozowski, S., Chesler, M. A., & Chesney, B. K. (1993). Parental intervention in the medical care of children with cancer. Journal of Psychosocial Oncology, 11(3), 63-88. [ Links ]
Manne, S. L., Du Hamel, K., Gallelli, K., Sorgen, K., & Redd, W. H. (1998). Posttraumatic stress disorder among mothers of pediatric cancer survivors : diagnosis, comorbidity, and utility of the PTSD checklist as a screening instrument. Journal of Pediatric Psychology, 23, 357-366. [ Links ]
McDaniel S. H., Hepworth, J., & Doherty, W. J. (1992). Medical Family Therapy. New York: Basic Books Inc. [ Links ]
Niles, M. (1996). Posttraumatic stress in response to childhood cancer: An examination to child/adolescent cancer survivors and their parents. Dissertation Abstracts International: Seccion B: The Sciences and Engineering, 56(9-b), 5179. [ Links ]
Norberg, A. L., Lindblad, F., & Boman, K. K. (2005a). Coping strategies in parents of children with cancer. Social Science & Medicine, 60, 965-975. [ Links ]
Norberg, A. L., Lindblad, F., & Boman, K. K. (2005b). Parental traumatic stress during and after paediatric cancer treatment. Acta Oncologica 44, 382-388. [ Links ]
Pai, A. L., Greenley, R. N., Lewandowski, A., Drotar, D., Youngstrom, E., & Peterson, C. C. (2007). A meta-analitic review of the influence of pediatric cancer on parent and family functioning. Journal of Family Psychology, 21, 407-415. [ Links ]
Patenaude, A. F., & Kupst, M. J. (2005). Psychosocial functioning in pediatric cancer. Journal of Pediatric Psychology, 30, 9-27. [ Links ]
Pelcovitz, D., Goldenberg, B., Kaplan, S., Weinblatt, M., Mandel, F., Meyers, B., & Vinciguerra, V. (1996). Posttraumatic stress disorder in mothers of pediatric cancer survivors. Psychosomatics, 37, 116-26. [ Links ]
Pendley, J. S., Dahlquist, L. M., & Dreyer, Z. (1997). Body image and psychosocial adjustment in adolescent cancer survivors. Journal of Pediatric Psychology, 22(1), 29-43. [ Links ]
Pérez, S., & Galdón, Mª J. (2001). Trastorno de estrés postraumático y cáncer. In:M.R. Dias & E. Durá (Coords.), Territórios da Psicologia Oncológica (pp. 493-525). Lisboa: Climepsi Editores. [ Links ]
Peris, R., & Giner, B. (2006) Incidencia y supervivencia del cáncer en la infancia. In:F. Antillon, E. Bernaola, A. Patiño & L. Sierrasesumaga (Eds.), Tratado de Oncología pediátrica (pp. 1-15). Madrid: Pearson Educación. [ Links ]
Phipps, S., Larson, S., Long, A., & Rai, S. (2006). Adaptative style and symptoms of posttraumatic stress in children with cancer and their parents. Journal of Pediatric Psychology, 31(3), 298-309. [ Links ]
Phipps, S., Long, A., Hudson, M., & Rai, S. (2005). Symptoms of posttraumatic stress in children with cancer and their parents: effects of informant and time from diagnosis. Pediatric Blood Cancer, 45, 952-959. [ Links ]
Radcliffe, J., Bennet, D., Kazak, A., Foley, B., & Phillips, P. (1996). Adjustment in childhood brain tumor survival: Child, mother, and teacher report. Journal of Pediatric Psychology, 21, 529-539. [ Links ]
Robinson, K. E., Gerhardt, C. A., Vannatta, K. & Noll, R. B. (2007). Parent and family factors associated with child adjustment to pediatric cancer. Journal of Pediatric Psychology, 32(4), 400-410. [ Links ]
Rowland, J. H. (1989). Developmental stage and adaptation: Child and adolescent model. In: J. C. Holland & J. H. Rowland (Eds.), Handbook of Psycho-oncology (pp. 519-543). New York: Oxford University Press. [ Links ]
Sahler, O. J., Varni, J. W., Fairclough, D. L., Butler, R. W., Noll, R. B., Dolgin, M. J., Phipps, S., Copeland, D. R., Katz, E. R., & Mulhern, R. K. (2002). Problem-solving skills training for mothers of children with newly diagnosed cancer: a randomized trial. Journal of Developmental and Behavioral Pediatrics, 23(2), 77-86. [ Links ]
Sawyer, M., Antoniou, G., Toogood, L., Rice, M., & Baghurst, P. (1993). A prospective study of the psychological adjustment of parents and families of children with cancer. Journal of Paediatrics and Child Health, 29, 352-356. [ Links ]
Sloper, P. (1996). Needs and responses of parents following the diagnosis of childhood cancer. Child: Care, Health, and Development, 22, 187-202. [ Links ]
Sloper, P. (2000). Predictors of distress in parents of children with cancer: a prospective study. Journal of Pediatric Psychology, 25 (2), 79-91. [ Links ]
Smith,M. Y., Redd,W. H., Peyser, C., & Vogl, D. (1999). Post-traumatic stress disorder in cancer: A review. Psycho-Oncology, 8, 521–537. [ Links ]
Speechley, K., & Noh, S. (1992). Surviving childhood cancer, social support, and parents psychological adjustment. Journal of Pediatric Psychology, 17, 15-31. [ Links ]
Stuber, M. L., Christakis, D. A., Houskamp, B., & Kazak, A.E. (1996). Posttrauma symptoms in childhood leukemia survivors and their parents. Psychosomatics, 37, 254-261. [ Links ]
Stuber, M. L., Kazak, A. E., Meeske, K., & Barakat, L. (1998). Is posttraumatic stress a viable model for understanding responses to childhood cancer?. Child and Adolescent Psychiatric Clinics of North America, 7, 169-82. [ Links ]
Trask, P. C., Paterson, A. G., Trask, C. L., Bares, C. B., Birt, J., & Maan, C. (2003). Parent and adolescent adjustment to pediatric cancer: associations with coping, social support, and family function. Journal of Pediatric Oncology Nursing, 20(1), 36-47. [ Links ]
Weiss, D. S., & Marmar, C. R. (1997). The Impact of Event Scale – Revised. In: J. P. Wilson & T.M. Keane (Eds.), Assessing Psychological Trauma and PTSD (pp. 399-411). New York: Guilford Press. [ Links ]
Wijnberg-Williams, B. J., Kamps, W. A., Klip, E. C., & Hoekstra-Weebers, J. (2006). Psychological adjustment of parents of pediatric cancer patients revisited: five years later. Psycho-Oncology, 15, 1-8. [ Links ]
Wittrock, D. A., Larson, L. S., & Sandgren, A. K. (1994). When a child is diagnosed with cancer: II. Parental coping, psychological adjustment, and relationships with medical personnel. Journal of Psychosocial Oncology, 12(3), 17-32. [ Links ]
Woodgate, R. L., Degner, L. F., & Yanofsky, R. (2003). A different perspective to approaching cancer symptoms in children. Journal of Pain & Symptom Management, 26, 800-817. [ Links ]
 Correspondence
Correspondence
Estrella Durá Ferrandis
Departamento de Personalidad, Evaluación y Tratamientos Psicológicos. Facultad de Psicología
Avnda. Blasco Ibáñez, 21 (46010 Valencia, España)
Tlfn: + 34 96 3864476
Fax: + 34 96 3864669
E-mail: estrella.dura@uv.es
Enviado em Março de 2009
Aceite final em Abril de 2009
Publicado em Dezembro de 2009
I Nota das autoras:Estrella Durá Ferrandis, Ph.D. Profesora Titular. Departamento de Personalidad, Evaluación y Tratamientos Psicológicos. Facultad de Psicología. Universidad de Valencia. Yolanda Andreu Vaillo. Ph.D. Profesora Titular. Departamento de Personalidad, Evaluación y Tratamientos Psicológicos. Facultad de Psicología. Universidad de Valencia. María José Galdón Garrido. Ph.D. Profesora Titular. Departamento de Personalidad, Evaluación y Tratamientos Psicológicos. Facultad de Psicología. Universidad de Valencia. Sonia Hernández López. Ph.D. Unidad de Psicología Clínica. Hospital Universitario Virgen de la Arixaca de Murcia. Concepción López Soler. Ph.D. Profesora Titular. Facultad de Psicología. Universidad de Murcia. Vinculada clínica a Pediatría del Hospital Universitario Virgen de la Arixaca de Murcia.














