Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Psicologia: teoria e prática
versão impressa ISSN 1516-3687
Psicol. teor. prat. vol.21 no.1 São Paulo jan./abr. 2019
https://doi.org/10.5935/1980-6906/psicologia.v21n1p170-185
ARTICLES
HUMAN DEVELOPMENT
Parents seeking a diagnosis of Autism Spectrum Disorder for their child
Los padres en busca de diagnóstico para Trastorno del Espectro Autista para el hijo
Jucineide S. XavierI; Thais MarchioriII; José Salomão SchwartzmanIII
IMackenzie Presbyterian University (UPM)
IIMackenzie Presbyterian University (UPM)
IIIDevelopment Disorders Graduate Program, Mackenzie Presbyterian University (UPM)
ABSTRACT
This study examined the parents' journey in the search of a diagnosis of Autism Spectrum Disorder (ASD) for their child and it was accomplished in two stages. The Stage 1 included the analysis of 20 records of children diagnosed with ASD attended in a clinic (2015-2017). We verified that the symptoms had been noticed between ages 13-24 months by most parents; the most reported symptom was verbal communication delay and different neuropediatricians were suspicious of the diagnosis; the most performed treatment was speech therapy. The Stage 2 was implemented to complement the findings of stage 1 and to characterize the clinic (311 cases in total). In this sample, we verified that 65.5% of the children were diagnosed with ASD; the parents and a single neuropediatrician were responsible for the referral. Despite the early detection of changes and seeking help, the parents sometimes received guidance that the child's development matched the expected for the age.
Keywords: Autism Spectrum Disorder; parents path; first symptoms; treatment; professionals.
RESUMEN
Este estudio determinó el recorrido de los padres en busca del diagnóstico del Trastorno del Espectro Autista (TEA). Se llevó a cabo en dos fases: 1) análisis de 20 registros médicos de personas atendidas en una clínica (2015-2017) y que recibieron diagnóstico del TEA. La mayoría de los padres percibieron los síntomas entre 13-24 meses; lo más reportado era retardo de lenguaje; profesionales que levantaron la sospecha del TEA fueron diversos neuropediatras; terapia del habla fue tratamiento más logrado; 2) para complementar los hallazgos de la fase 1 y caracterizar la clínica, se analizó su base de datos (total: 311 casos): 65,5% de los casos tenía el diagnóstico del TEA; origen de la mayoría de los referidos: un solo neuropediatra y padres. A pesar de detectar cambios en las edades tempranas y buscar ayuda, los padres a veces recibieron orientación que el desarrollo del niño era apropiado para la edad.
Palabras clave: Trastorno del Espectro Autista; trayectoria de los padres; primeros síntomas; tratamiento; profesionales.
1. Introduction
Autism is a neurodevelopmental disorder with a multifactorial etiology (American Psychiatric Association, 2014; Schwartzman, 2015). It is present in about 1.5 million Brazilians, according to international data (Paula, Fombonne, Gadia, Tuchman, & Rosanoff, 2011), being four times more frequent in boys than in girls (American Psychiatric Association, 2014). The latest publications on the subject have started to use the term Autism Spectrum Disorder (ASD), which encompasses conditions such as autistic disorder, Asperger's disorder, and global developmental disorder without other specifications that were previously diagnosed separately (Zanon, Backes, & Bosa, 2014). In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders - DSM-5 (American Psychiatric Association, 2014) there were some changes in the diagnostic criteria, which were classified in two groups: social interaction and communication deficits and repetitive, and restricted patterns of behaviors, interests or activities. Language impairment then ceased to be a criterion that defines ASD and moved to the category of associated characteristics that support the diagnosis (American Psychiatric Association, 2014).
Hyper or hypoactivity to sensorial stimuli; unusual interest for sensory aspects, such as indifference to pain/temperature and fascination with lights or movement; fixed and highly restricted interests; motor movements; insistence on the same things, little tolerance for change, aggressiveness, and self-aggressive behavior; deficit in developing, maintaining or understanding relationships; impairment in communication and difficulty in establishing a conversation or responding to social interactions can be observed among the manifestations of ASD that appear in the DSM-5 (American Psychiatric Association, 2014). This complexity and heterogeneity in the manifestations of the disorder make it difficult for parents to identify them in children with milder symptoms (Larsen, 2015). In addition, ASD is often associated with psychiatric problems, epilepsy, and genetic syndromes (Noterdaeme & Hutzelmeyer-Nickels, 2010; Schwartzman, 2015).
In a study of 141 parents of Indian children diagnosed with TEA, Chakrabarti (2009) observed that speech delay was the symptom that most caught the attention of parents and caused them to seek professional help. Noterdaeme and Hutzelmeyer-Nickels (2010) carried out a study in Germany with 601 children diagnosed with autism and found that the first symptoms perceived by the parents in their sample were language impairments (48% of cases) and deficits in social interactions (25% of cases). Sampedro-Tobón, González-González, Vélez-Vieira, & Lemos-Hoyos (2013) performed a retrospective study by reviewing medical records and performing semi-structured interviews with parents of 42 Colombian children diagnosed with ASD, and found that the initial symptoms that made the parents suspicious of atypical development were social interaction impairments in 92% of the cases and language impairments in 50% of them. According to Cortez Bellotti de Oliveira and Contreras (2007), both longitudinal and transversal studies indicate that the symptoms observed tend to change according to the child's age and level of development. For changes observed at early ages, such as impairment in non-verbal communication, they are different from those reported at a later age: deficits in social interaction skills (Becerra-Culqui, Lynch, Owen-Smith, Spitzer, & Croen, 2018).
In recent years, researchers have been investigating, through interviews with parents, the age at which they identified the early symptoms of ASD (Zanon et al., 2014). According to Visani and Rabello (2012), in 36.4% of the cases, the child was 12 months or younger when the first symptoms were observed; in 27.3% of these cases, when the child was at 24 months, and in 18.2% of the cases when the child was 36 months of age. On the other hand, Fortea Sevilla, Escandell Bermúdez, & Castro Sánchez (2013) reported that in 9% of cases the suspicion of atypical development occurred when the child was less than 12 months of age; 40% between 12 and 18 months of age; 23% between 24 and 36 months and only 10% after 36 months.
In their study, Sampedro-Tobón et al. (2013) found that the parents perceived the first signs of ASD (59.5% of cases), followed by education professionals (21.4%), and physicians (only 2.4% of cases). Some studies emphasize the importance of receiving an early diagnosis to perform the treatment and alleviate the daily stress experienced by the families seeking it (Gomes, Lima, Bueno, Araújo, & Souza, 2015; Noterdaeme & Hutzelmeyer-Nickels, 2010). In a review of the literature on the screening procedures adopted in Europe, García-Primo et al. (2014) discuss the issue of diagnosis in very young children, since difficulties in differentiating ASD from other developmental disorders at a very early age may lead to false positives. In general, it is not possible to safely establish the diagnosis of autism before the age of three, even if the child has some symptoms of the disorder. However, this does not prevent treatments directed toward the child's difficulties from being carried out. These should be continued until the suspicious signs and symptoms disappear or continue with the diagnosis if it is clear that ASD is actually present (Schwartzman, 2015).
According to Paula et al. (2011), although the number of Brazilian studies on ASD has increased in recent years, they are not focused on how to promote adequate care in the Brazilian Health System. However, this scenario is changing. In 2013, for example, the Ministry of Health launched two booklets: one about care guidelines for the rehabilitation of the people with ASD and the other about the line of care in the Brazilian National Health System for people with autism and their family members. These documents emphasize the importance of the articulation between the health systems in order to promote the inclusion of people with ASD in the labor market, in social activities, and in activities of daily living, as well as the respect for the singularity of each individual in the creation of a Unique Therapeutic Project (Oliveira, Feldman, Couto, & Lima, 2017). These measures are significant and help guide the behavior of the professionals working in the Brazilian National Health System. Because autism cannot be considered a rare disorder, public health and education agencies must be able to receive and treat people with the disorder (Wilkinson, 2011).
There is often a considerable delay between the first parental concerns and the diagnosis of ASD. According to the study of Araujo (2012), conducted in the city of Barueri (São Paulo) with 38 parents of children with ASD, almost 90% of the families took more than a year to obtain the diagnosis. The study of Ribeiro, Paula, Bordini, Mari, & Caetano (2017) with 19 Brazilian mothers of children with autism found that, in some cases, the visits to clinics, hospitals, and health professionals can last up to three years. According to Wilkinson (2011) and Sampedro-Tobón et al. (2013), families usually visit an average of four to five health professionals to obtain or confirm the diagnosis. On other occasions, the number of health professionals and institutions attended can reach six (Visani & Rabello, 2012).
The diagnosis of ASD should be performed by a multidisciplinary team, that is, a team that includes professionals with knowledge about both the typical developmental stages and the symptoms of the disorder (Fortea Sevilla et al., 2013; Larsen, 2015). For Cortez Bellotti de Oliveira and Contreras (2007), Favero-Nunes and Santos (2010), and Zanon et al. (2014), coupled with the fact that the professionals that provide care to children under three years of age often do not receive adequate and continuous training, there is a shortage of specialized health equipment and multidisciplinary teams that could facilitate the detection of the signs and symptoms of the disorder. It is recommended, therefore, that professionals adopt scales and tests the conclusion of the diagnostic. Professionals not adequately trained may generate delays in the diagnosis, in the intervention planning and in the medical and educational services; services to which the child must have access (Fortea Sevilla et al., 2013).
Thus, the general aim of this study was to investigate the course of parents who sought and obtained the diagnosis of ASD for their children, through the specialized service of a clinic at Mackenzie Presbyterian University. The clinic has a specific protocol for the diagnosis of ASD, and the entire evaluation process is performed exclusively by the service team that is composed of: a neuropediatrician, a geneticist, a psychologist, a speech therapist, a psychiatrist, and a psychopedagogist. The specific objectives were: to identify the age of the child when the parents suspected atypical development; what the first symptoms detected by the parents were; how long after the suspicion did the parents seek professional help; which professionals first suggested the diagnosis of ASD; to check that the parents had obtained treatment for their children and what type of intervention they had access to; to ascertain the origin and amount of referrals received by the clinic; to determine how many people had a diagnosis of ASD, and, finally, to compare these data with the findings in the literature about the subject.
2. Method
2.1 Sample
This study was carried out in two stages and that is why it contains two distinct samples. Stage 1: the general aim was to investigate the parents' search for a diagnosis for their children. For this purpose, 20 medical records (convenience sample) were analyzed for cases diagnosed with ASD by the clinic between the first half of 2015 until the first half of 2016. These diagnoses were performed in the clinic, with the same professional team and met the DSM-5 criteria. The period was selected due to the fact that the clinic underwent a process of updating the evaluation protocols in 2015 and these files contained more robust and up-to-date information. As the exclusion criterion in this stage, the cases treated in the same period that did not have the confirmed diagnosis of ASD were excluded from the sample.
Stage 2: in order to complement the findings of Stage 1, a complete analysis of the clinic's database was performed, which included all the cases seen in the service between 2005 and 2016: 311 cases. This increase in the sample was performed for the general characterization of the clinic, analyzing the number of visits performed, the number of diagnoses of ASD, as well as the profile of the origins of the referrals received. As the purpose of this stage was to characterize the service, no case was excluded from the sample.
2.2 Procedures
Initially, the physical files of the last cases treated that had a closed diagnosis (total of 20 records) were consulted to collect the data concerning the age of the child when the parents suspected atypical development, what were the first symptoms observed, which professional raised the suspicion ASD, and what treatment the child had access to after the diagnosis. Subsequently, the database was consulted to characterize the service. The data used in this study came from cases in which the parents or caregivers signed the Informed Consent Form (mandatory for scientific research with human subjects), with the study approved by Mackenzie Presbyterian University ethics committee under authorization n. 658.06.04.
3. Results
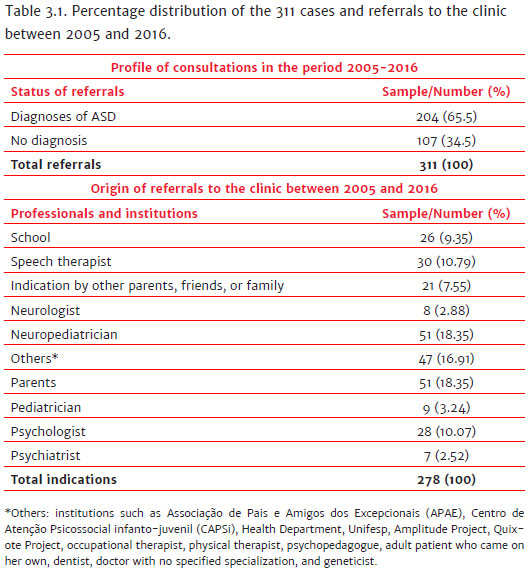
Between 2005 and 2016, the clinic received 311 referrals (Table 3.1). Of these, 204 (65.5%) were diagnosed with ASD, while 107 (34.5%) did not receive the diagnosis. It was possible to verify the origin of the referrals in 278 medical records since some (11.0%) did not contain the referral information or were part of specific research projects; in these cases, the records remained in possession of the researcher responsible. From the 278 records, it was understood that those people that performed the most referrals were: a single neuropediatrician (18.35%), the parents (18.35%), speech therapists (10.79%), psychologists (10.07%), schools (35.00%), indicated by other parents, friends or family members (7.55%), pediatricians (3.24%), neurologists (2.88%), psychiatrists (2.52%), and others (16.71%).
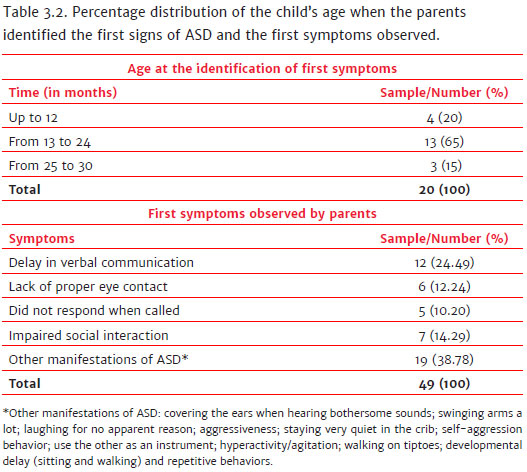
In relation to the 20 cases treated between 2015 and 2017, as presented in Table 3.2, in 65% of the cases, the parents detected the first signs of atypical behavior when the children were between 13 and 24 months of age, with this being noticed in 20% before 12 months and 15% between 25 and 30 months. Each family reported having observed more than one sign that the child's development was not occurring in line with that expected for the age. According to Table 3.2, the first symptoms that caught the attention of family members were: verbal communication delay (24.49%), social interaction impairment (14.29%), lack of appropriate eye contact (12.24%), lack of response when called (10.20%), along with other manifestations of ASD (group of symptoms mentioned by the parents) found in 38.78% of the cases.
As soon as they realized these changes in the development of their children, 40% of the parents immediately sought professional help, while 35% took up to 6 months to do so. A total of 15% of the parents had sought help between 7 and 12 months and 10% after more than 12 months. However, it was not possible to measure how much time elapsed between seeking help and the parents receiving the diagnosis of ASD, since the records contained only the date of the first screening, without the date of the diagnostic conclusion or of informing the family members.
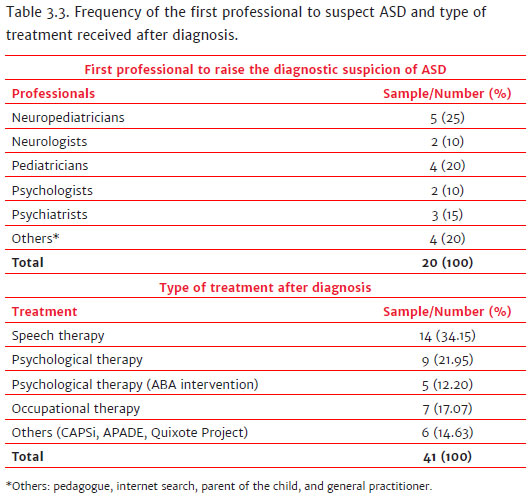
Table 3.3 shows that neuropediatricians were, in most cases, the first professionals to raise the diagnostic suspicion of autism (25%), in the cases observed in this study, these are numerous neuropediatricians, unlike Table 3.1, in which a single professional was responsible for referring many of the patients to the clinic. Secondly, pediatricians (20%) suspected ASD, followed by psychiatrists (15%), neurologists (10%), psychologists (10%), and others (pedagogue; internet research conducted on the subject by the adult patient; the child's own parents, since the pediatrician did not agree with the suspicion; and a clinical doctor) in 20% of the cases. However, since the sample was composed of charts with diagnoses closed between 2015 and the first half of 2017, it was not possible to verify, in two of the cases diagnosed in the first half of 2017, the type of treatment that the child had access to since the diagnoses were recent. Thus, of the total of 20 charts analyzed, information was obtained on the type of treatment for 18 of them. Each child had access to more than one type of intervention after receiving the diagnosis (Table 3.3), these being: speech therapy (34.15%); psychological therapy (21.95%); psychological therapy, based on Applied Behavior Analysis - ABA (12.20%); occupational therapy (17.07%); and others (CAPSi, APADE, Quixote Project) in 14.63% of the cases.
4. Discussion
One of the primary sources of referral to the clinic, according to Table 3.1, was a single ASD specialist neuropediatrician. This may justify the fact that 65.5% of the patients were diagnosed with the disorder since the population that arrives at the clinic through this professional was highly indicative of ASD. As autism is a disorder that is reasonably heterogeneous in its manifestation, the diagnosis is only closed when there is a consensus among the multidisciplinary team that they are dealing with a case of ASD. Also in Table 3.1, it can be seen that 34.5% of the cases did not obtain any diagnosis, since the clinic exclusively carries out research and diagnosis of autism, therefore, when there is suspicion that it is another developmental disorder the professionals inform the parents that the child does not have autism and advise them to visit other places or professionals to continue investigating their child's condition.
The parents are the first to suspect something different in their child's development. In the study of Fortea Sevilla et al. (2013), for example, in 79% of the cases, it was the family that perceived atypical development, while in 15% it was education professionals, and in 6% health professionals (4% pediatricians and 2% psychologists). Of the total number of parents (51 cases, equivalent to 18% of the sample) who spontaneously sought the clinic to obtain the diagnosis, 82% were mothers. According to Favero-Nunes & Santos (2010) and Gomes et al. (2015), it is usually the mother that seeks professional help and takes responsibility for caring for the child, often giving up her professional career to have more time to dedicate herself exclusively to the child, a factor that can generate a physical and emotional overload, according to the authors.
Araujo (2012) found that, on average, the first symptoms were observed around 21 months of age. These data, added to those described by both national and international studies, like Chakrabarti (2009), Cortez Bellotti de Oliveira and Contreras (2007), Noterdaeme and Hutzelmeyer-Nickels (2010), Ribeiro et al. (2017), and Sampedro-Tobón et al. (2013), in which the average age at which the parents reported suspicion of altered child development was between 12 and 24 months, are consistent with the finding of the present study, that indicated (Table 3.2), in 65% of the cases, that the parents were more sensitive to detect signs of atypical development when the child was between 13 and 24 months of age. Overall, the studies cited show that the time when parents most notice signs of ASD in children are in their first 24 months of life.
The main complaint reported by the parents (Table 3.2) was the delay in verbal communication (24.49%), followed by impairment in social interactions (14.29%), lack of appropriate eye contact (12.24%), lack of response by the child when called (10.20%), along with other manifestations of ASD present in 38.78% of the cases. In this sample of 20 Brazilian families, the first symptoms that parents perceived in their children were similar to those observed by other families around the world, with the delay in verbal communication also reported in the Brazilian study by Araujo (2012) as the chief complaint in 42.10% of the cases. In addition, studies in India (Chakrabarti, 2009), Germany (Noterdaeme & Hutzelmeyer-Nickels, 2010), Brazil (Ribeiro et al., 2017), and Colombia (Sampedro-Tobón et al., 2013) also reported language impairments as a frequent complaint in their samples, as well as deficits in relation to social interaction (Noterdaeme & Hutzelmeyer-Nickels, 2010; Sampedro-Tobón et al., 2013).
In their study, Sampedro-Tobón et al. (2013) observed that the child neurologist was the professional who most performed the diagnosis of autism. Araujo (2012) also reported that it was the neurologist who most suggested ASD as a diagnosis and, furthermore, in 60.5% of the cases, the first professionals to whom the parents were referred did not provide any diagnostic hypothesis. Therefore, the data found in this study, according to Table 3.3, differ from the findings of Araujo (2012) and Sampedro-Tobón et al. (2013), as neuropediatricians were the first professionals to suspect autism in 25% of cases; followed by pediatricians (20%); other sources (including professionals such as a pedagogue; a doctor with no defined specialization; internet searches and the parents) in 20% of the cases; psychiatrists (15%); psychologists (10%); and neurologists (10%). Although the difference between the findings of this study and those of Araujo (2012) and Sampedro-Tobón et al. (2013) may indicate a possible change in the profile of the professionals who first detect autism, it would be interesting to conduct a study with a larger sample to confirm whether early childhood professionals are actually more alert to signs that indicate developmental disorders.
Three of the families in the study sample reported that after learning that there was something wrong with their child's development they sought help, however, the professionals consulted did not agree with their suspicions. One reported that the pediatrician informed her that there was nothing atypical about the development of the child. Not satisfied, the family attended the clinic in which they had their suspicion of autism confirmed. Unfortunately, these accounts are not isolated; in their Brazilian studies, Araujo (2012) and Ribeiro et al. (2017) also described a scenario of similar helplessness: in seeking help, parents often received guidance that they have no reason to worry. According to Ribeiro et al. (2017), the lack of appreciation of parents' perceptions regarding the child's development by pediatricians may contribute to the delay in the formal diagnosis of ASD.
The studies of Araujo (2012), Chakrabarti (2009), Fortea Sevilla et al. (2013), and Ribeiro et al. (2017) present data that show that in many cases the pediatrician was the first professional to whom the parents took their children seeking a diagnosis of ASD. However, it is not this professional who usually suggests the disorder as a diagnosis. In 2017, Law No. 13.438 (2017, April 26) was published in the Official Journal of the Union, which makes it mandatory for the Brazilian National Health System to adopt instruments or protocols to evaluate all children in the first 18 months of life. It is expected that with this obligation the pediatricians who work in the Brazilian National Health System are more instrumentally supported to perform diagnoses.
Regarding the treatment, according to Table 3.3, all the children had access to more than one type of intervention, with the majority of them performing or having performed speech therapy (34.15%), psychological therapy (21.95%) and occupational therapy (17.07%), while 14.63% (category "other" in the results table) received treatment in child care institutions and 12.20% psychological treatment based on the ABA method. The main complaint reported by the parents of these children and that made them seek help was the delay in verbal communication. This delay may have contributed to the parents seeking, on their own or through other professionals, speech therapy for their children. This hypothesis would explain the fact that speech therapy treatment was the most performed by the patients after obtaining the diagnosis.
Because this was a study based on parents' memories about the age and first symptoms observed in the children and contain a small sample, it cannot be said that there is a complete picture of the course they traveled from the suspicion to the diagnosis of the child. Although a study with a larger sample is needed to obtain a complete picture of the trajectory of the parents seeking the diagnosis, this study demonstrated that more than half of the population that went to the clinic at Mackenzie Presbyterian University to investigate the condition of the child received a diagnosis of ASD. Also, the majority of the parents presented a good perception of the child's development, since they were able to identify signs of autism (often delayed verbal communication) when the child was, in most cases, between 13 and 24 months of age. Besides, we verified that pediatricians were the professionals who suggested the diagnosis of ASD for the first time and that speech-language therapy was the intervention most performed after the diagnosis. In addition, the majority of the data found in the literature on the subject was corroborated by this study. Despite detecting changes at an early age and seeking help, the parents sometimes received guidance that the child's development was occurring within the expected age range. Thus, it is necessary that the professionals who work with children are attentive not only to the signs of disturbances but also to the complaints reported by the parents because they are the ones who live with the child and, in most cases, perceive the atypical development.
References
American Psychiatric Association. (2014). Manual diagnóstico e estatístico de transtornos mentais DSMV- TR (5 ed.). Porto Alegre: Artmed. [ Links ]
Araujo, R. R. de (2012). Estudo piloto para o mapeamento da trajetória em busca de diagnóstico e tratamento do Transtorno do Espectro do Autismo no município de Barueri em São Paulo. (Master's dissertation). Retrieved from http://tede.mackenzie.br/jspui/handle/tede/1581 [ Links ]
Becerra-Culqui, T. A., Lynch, F. L., Owen-Smith, A. A., Spitzer, J., & Croen, L. A. (2018). Parental first concerns and timing of Autism Spectrum Disorder diagnosis. Journal of Autism and Developmental Disorders, 2018. doi: 10.1007/s10803-018-3598-6 [ Links ]
Brasil. Lei nº 13.438, de 26 de abril de 2017. (2017, 26 abril). Torna obrigatória a adoção pelo Sistema Único de Saúde (SUS) de protocolo que estabeleça padrões para a avaliação de riscos para o desenvolvimento psíquico das crianças e altera a Lei nº 8.069, de 13 de julho de 1990 (Estatuto da Criança e do Adolescente). Diário Oficial da União, seção 1. [ Links ]
Chakrabarti, S. (2009). Early identification of Autism. Indian Pediatrics, 46(17),412-414. Retrieved from http://imsear.li.mahidol.ac.th/bitstream/123456789/144034/1/ip2009v46n5p412.pdf [ Links ]
Cortez Bellotti de Oliveira, M., & Contreras, M. M. (2007). Diagnóstico precoz de los trastornos del espectro autista en edad temprana (18-36 meses). Archivos Argentinos de Pediatría, 105(5),418-426. Retrieved from http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S0325-00752007000500008&lng=es&tlng=es [ Links ]
Favero-Nunes, M. A., & Santos, M. A. dos. (2010). Itinerário terapêutico percorrido por mães de crianças com transtorno autístico. Psicologia: Reflexão e Crítica, 23(2),208-221. doi:10.1590/S0102-79722010000200003 [ Links ]
Fortea Sevilla, M. D. S., Escandell Bermúdez, M. O., & Castro Sánchez, J. J. (2013). Detección temprana del autismo: Profesionales implicados. Revista Española de Salud Pública, 87(2),191-199. doi:10.4321/S1135-57272013000200008 [ Links ]
García-Primo, P., Hellendoorn, A., Charman, T., Roeyers, H., Dereu, M., Roge, B., ... Canal-Bedia, R. (2014). Screening for Autism Spectrum Disorders: State of the art in Europe. Eur Child Adolesc Psychiatry, 23(11),1005-1021. doi: 10.1007/s00787-014-0555-6 [ Links ]
Gomes, P. T. M., Lima, L. H. L., Bueno, M. K. G., Araújo, L. A., & Souza, N. M. (2015). Autism in Brazil: A systematic review of family challenges and coping strategies. Jornal de Pediatria, 91(2),111-121. doi:10.1016/j.jped.2014.08.009 [ Links ]
Larsen, K. (2015). The early diagnosis of preschool children with Autism Spectrum Disorder in Norway: A study of diagnostic age and its associated factors. Scandinavian Journal of Child and Adolescent Psychiatry and Psychology, 3(2),136-145. Retrieved from http://www.sjcapp.org/article/view/20239 [ Links ]
Noterdaeme, M., & Hutzelmeyer-Nickels, A. (2010) Early symptoms and recognition of pervasive developmental disorders in Germany. Autism, 14,575-588. doi: 10.1177/1362361310371951 [ Links ]
Oliveira, B. D. C. de, Feldman, C., Couto, M. C. V., & Lima, R. C. (2017). Políticas para o autismo no Brasil: Entre a atenção psicossocial e a reabilitação. Physis: Revista de Saúde Coletiva, 27(3),707-726. doi: 10.1590/s0103-73312017000300017 [ Links ]
Paula, C. S., Fombonne, E., Gadia, C., Tuchman, R., & Rosanoff, M. (2011). Autism in Brazil: Perspectives from science and society. Revista da Associação Médica Brasileira, 57(1),2-5. doi:10.1590/S0104-42302011000100002 [ Links ]
Ribeiro, S. H., Paula, C. S. de, Bordini, D., Mari, J. J., & Caetano, S. C. (2017). Barriers to early identification of autism in Brazil. Revista Brasileira de Psiquiatria, 39(4),352-354. doi: 10.1590/1516-4446-2016-2141 [ Links ]
Sampedro-Tobón, M. E., González-González, M., Vélez-Vieira, S., & Lemos-Hoyos, M. (2013). Detección temprana en trastornos del espectro autista: Una decisión responsable para un mejor pronóstico. Boletín médico del Hospital Infantil de México, 70(6),456-466. Retrieved from http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S1665-11462013000600006&lng=es&tlng=es [ Links ]
Schwartzman, J. S. (2015). Transtornos do Espectro do Autismo: Características gerais. In M. E. F. D'Antino, D. Brunoni, & J. S.Schwartzman (Org.), Contribuições para inclusão escolar de alunos com necessidades especiais: Estudos interdisciplinares em educação e saúde em alunos com Transtornos do Espectro do Autismo no município de Barueri, SP (pp.13-24). São Paulo: Memnon. [ Links ]
Visani, P., & Rabello, S. (2012). Considerações sobre o diagnóstico precoce na clínica do autismo e das psicoses infantis. Revista Latinoamericana de Psicopatologia Fundamental, 15(2),293-308. doi:10.1590/S1415-47142012000200006 [ Links ]
Wilkinson, L. A. (2011) How many doctors does it take to diagnose an autism spectrum disorder? Autism, 1, 101. doi: 10.4172/2165-7890.1000e101 [ Links ]
Zanon, R. B., Backes, B., & Bosa, C. A. (2014). Identificação dos primeiros sintomas do autismo pelos pais. Psicologia: Teoria e Pesquisa, 30(1),25-33. doi:10.1590/S0102-37722014000100004 [ Links ]
 Mailling address:
Mailling address:
Jucineide S. Xavier
Rua Itápolis, 188, Cotia
São Paulo, SP, Brazil. CEP 06716-235
E-mail: juxavier03@gmail.com
Submission: 18/12/2017
Acceptance: 14/11/2018












 Curriculum ScienTI
Curriculum ScienTI

