Serviços Personalizados
artigo
Indicadores
Compartilhar
Psicologia: teoria e prática
versão impressa ISSN 1516-3687
Psicol. teor. prat. vol.21 no.1 São Paulo jan./abr. 2019
http://dx.doi.org/10.5935/1980-6906/psicologia.v21n1p328-343
ARTICLES
CLINICAL PSYCHOLOGY
Anxiety and depression in family members of people hospitalized in an intensive care unit
Ansiedad y depresión en familiares de personas ingresadas en terapia intensiva
Gabriella M. FonsecaI; Katia S. FreitasII; Aloisio M. da S. FilhoIII; Pollyana P. PortelaIV; Elaine G. FontouraV; Marluce A. N. OliveiraIV
IDepartment of Health, State University of Feira de Santana (UEFS)
IIDepartment of Health, State University of Santana (UEFS)
IIIDepartment of Exact Sciences, State University of Feira de Santana (UEFS)
IVDepartment of Health, State University of Feira de Santana (UEFS)
VDepartment of Health, State University of Feira de Santana (UEFS)
VIDepartment of Health, State University of Feira de Santana (UEFS)
ABSTRACT
This is a cross-sectional study that aimed to analyze the prevalence of anxiety and depression in the relatives of people hospitalized in an intensive care unit and associated factors. The sample consisted of 135 family members of hospitalized adults in the interior of Bahia. The sociodemographic data sheet and the Hospital Anxiety and Depression Scale were applied. Concerning anxiety, 39.3% presented the symptoms and 28.9% of the relatives had symptoms of depression. According to the logistic regression model, being familiar with less than 40 years of age (OR 2.20, CI 1.049-4.6540, p = 0.037) and living with the relative hospitalized (OR 2.37, CI 1.121-5.024, p = 0.024) was associated with the presence of anxiety symptoms. As for depression, the degree of kinship was associated (OR 2.52, CI 1.096-5.814, p = 0.003). The results reinforce the evidence of association between the hospitalization process and the mental state of the family.
Keywords: anxiety; depression; family; intensive therapy; hospitalization.
RESUMEN
Estudio transversal que objetivó analizar la presencia de ansiedad y depresión en familiares de personas internadas en unidad de terapia intensiva y los factores asociados. Participaron 135 familiares de personas hospitalizadas en el interior de Bahía. Se aplicaron la ficha de datos socio demográficos y la Escala de Hospitalar de Ansiedad y Depresión. En relación a la ansiedad, el 39,3% presentó y el 28,9% de los familiares tuvieron síntomas de depresión. Enel modelo de regresión logística, ser familiar con edad inferior a 40 años (OR 2,20, IC 1,049-4,6540, p = 0,037) y vivir con el pariente internado (OR 2,37, IC 1,121-5,024, p = 0,024) se asoció la presencia de síntomas de ansiedad. Cuanto a la depresión, estuvo asociado el grado de parentesco (OR 2,52, IC 1,096-5,814, p = 0,003). Los resultados refuerzan las evidencias de asociación entre el proceso de hospitalización y el estado de salud mental de la familia.
Palabras clave: ansiedad; depresión; familia; terapia intensiva; hospitalización.
1. Introduction
Acute diseases affect all the dimensions of the personal and social lives of individuals who become ill and their families, constituting a disorganizing factor of family dynamics that require the restructuring of life aspects to adapt to this new condition (Schmidt & Azoulay, 2012). The experience of the hospitalization of a family member in an Intensive Care Unit (ICU) can advance the development of psychic problems that are detrimental to the physical and mental integrity of the family. Due to the changes imposed by the insertion into a new environment and coupled with the uncertainty of the recovery of the person who falls ill, the family starts to live in a crisis that can have a significant effect on their lives (Maruiti, Galdeano, & Farah, 2008). Among these changes, there is a consensus in the literature of the area regarding the state of severe discomfort caused by the anguish due to the possible loss of the relative, physical and emotional separation, increased responsibility and difficult decision making that can devastate the family well-being. In addition, changes in the social and professional life, associated with the impairment of work, study and leisure activities, as well as the attention centered on the hospitalized relative, culminate in the difficulty to care for oneself and one's individual needs, such as sleep, rest and eating, which are detrimental in the short and long term (Freitas, Mussi, & Menezes, 2012; Schmidt & Azoulay, 2012).
The family experiences moments of tension stemming from both individuals' feelings about the person being hospitalized and their coping capacity, as well as from the environment, especially in the ICU, which is a hospital space associated with negative impressions, related to death and disability, the representation of which threatens the integrity, security and vulnerability of the family group. Such experiences contribute to the emergence of psychological changes in the family (Davidson et al., 2017). Added to this, the ICU is a hospital environment associated with negative impressions, related to death and disability, which can pose a threat to the integrity, security, and vulnerability of the family group. All these factors contribute to the emergence of depression and anxiety, especially in the family members of unconscious patients, who are responsible for decision making in problem situations that pose a risk to the relative's health (Köse et al., 2015).
Given the importance of the role of family support in the care, family-centered care has been prioritized in intensive care. Thus, the prevalence of anxiety and depression in family members have been proposed as markers for the quality of the care and information provided to the family members (Belayachi et al., 2014; Köse et al., 2015). However, relatively high prevalence rates for symptoms related to anxiety and depression have been identified. For example, international investigations have reported the prevalence of anxiety among relatives of ICU patients at 72.8% (Rusinova, Kukal, Simek, & Cerny, 2014) and 69.1% (Pochard et al., 2001) and prevalence of depression at 53.6% (Rusinova et al., 2014) and 53.8% (Kourti, Christofilou, & Kallergis, 2015).
Furthermore, there are gaps in the Brazilian literature on the subject. A review of the SciELO, LILACS, and MEDLINE databases showed that, in the international context, the investigation of the psychological impact of the hospitalization of a relative in the ICU context has been the focus of several studies, mainly in relation to the prevalence of anxiety and depression (Anderson, Arnold, Angus, & Bryce, 2008; Fumis & Deheizelin, 2009; Fumis, Ranzani, Faria, & Schettino, 2015; Hwang et al., 2014; McAdam & Puntillo, 2009; Pochard et al., 2001). However, in the national literature, only two studies have evaluated the symptoms of anxiety and depression in family members in the ICU context: Fumis & Deheizelin (2009) and Maruiti et al. (2008). Thus, this study aimed to verify the existence of the prevalence of factors associated with symptoms of anxiety and depression in family members of people hospitalized in ICUs and to estimate them.
2. Method
A cross-sectional study was conducted in two ICUs of a public hospital in the municipality of Feira de Santana, Bahia's second largest city, from July 2015 to February 2017.
2.1 Participants
The participants were 135 family members of people hospitalized in the ICU who fulfilled the selection criteria. A non-probabilistic type by convenience sampling technique was used and up to two family members per hospitalized person were chosen for the study, in order to capture the diversity of the experience within the same family group. The criterion adopted for the sample size considered at least ten cases of the outcome event (dependent variable) for each independent variable included in the final multivariate logistic regression model (Peduzzi, Concato, Kemper, Holford, & Feinstein, 1996).
After a period of more than 48 hours of hospitalization of the patient in the ICU, the family members were approached and included in the study when they were 19 years of age or older, they had visited the patient at least once and were considered to be close to the hospitalized person (information obtained from the family members). In this study, the family was considered to be a group of individuals with emotional, affective bonds, linked or not by consanguinity, who have a sense of membership, live together or lived together for a certain period of time, with commitments, duties, and responsibilities to care for each other.
2.2 Procedures
The selection of family members was initially performed after the daily check of the ICUs in order to identify people hospitalized for more than 48 hours and to verify their clinical characteristics. The approach took place in the ICU waiting room, before or after the visiting hours, in the morning and afternoon, with the possibility of up to two relatives visiting per shift. The family members that agreed to participate in the study were invited to go to a private room near the waiting room to guarantee their privacy. The data were collected through an interview, after signing the consent form. The study was registered on the Plataforma Brasil and approved under CAAE no. 25608213.8.0000.0053.
2.3 Instruments
The questionnaire used was composed of sociodemographic and clinical variables, as well as topics related to the relative and hospitalized person. The analysis of anxiety and depression was carried out using the Hospital Anxiety and Depression Scale (HADS), validated and translated to the Brazilian context (Botega, Bio, Zomignani, Garcia Jr, & Pereira, 1995). This scale is easy to apply, has a small number of items, has shown good psychometric properties in several contexts, and is, therefore, widely used as an indicator in screening for anxiety and depression in relatives of people hospitalized in an ICU (DeSousa, Moreno, Gauer, Manfro, & Koller, 2013; Köse et al., 2015).
The HADS has 14 items, distributed in two subscales - seven items for anxiety and seven for depression. For each item, the response categories ranges from zero to three, on a four-point Likert-type scale, providing a total score that can range from zero to 21 points. The cut-off point was 10 points for each subscale, with lower values indicating the absence of symptoms of anxiety and depression.
2.4 Data analysis
The information collected was compiled in a database and analyzed using the Statistical Package for the Social Sciences (SPSS) statistical program, version 18.0, for Windows. To analyze the categorical variables related to the characterization of the family members and cases of anxiety and depression, absolute and relative frequencies were used. For the quantitative variables, the descriptive measures of centrality and dispersion were calculated.
The multivariate logistic regression model was used to verify the factors associated with anxiety, depression, and variables related to the family members and the hospitalized person, with stepwise input criterion, considering a p-value < 0.20, with the aim of including the maximum number of variables in the first step of the modeling. The dependent variables were anxiety and depression, tested separately, while the independent variables related to the hospitalized person were age and length of hospitalization and those related to the family member were sex, age, schooling, religion, kinship, living with the person hospitalized, and previous experience of the ICU. For analysis purposes, the continuous variables that entered the model were recategorized based on the theoretical framework.
After adjustment of the model using the "maximum likelihood" estimator, the significance of the model variables was evaluated through the Wald test. The Hosmer-Lemeshow test was used to assess the accuracy and quality of fit of the logistic model. After establishing the final multivariate model, the coefficients, estimated in terms of odds ratios (OR), were interpreted. The level of significance considered was 5%.
3. Results
The mean age of the hospitalized patients was 48 years, and the length of hospital stay was approximately 11 days. There was a prevalence of female family members (67.4%), with a mean age of 40 years, married (40.0%), catholic (51.7%), and with high school education (53.3%). The majority were children (29.6%), or with another family attachment - such as uncle/aunt, nephew/niece or cousin (22.2%). However, 61.5% did not live with the patient and had no previous experience of the ICU (68.1%).
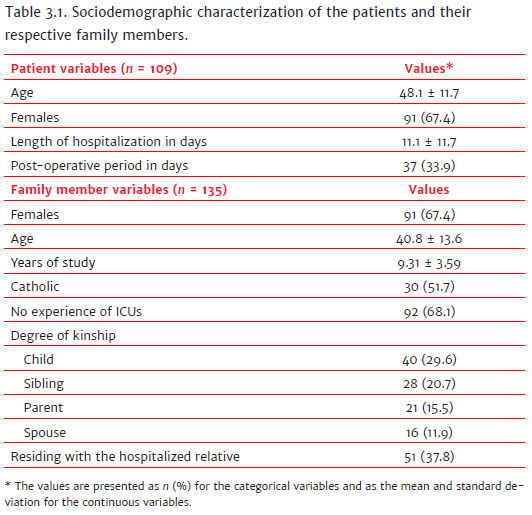
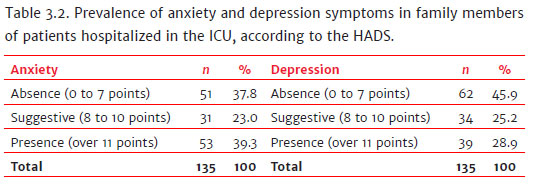
The prevalence of anxiety symptoms was 39.3% and 28.9% for symptoms of depression.
The prevalence of symptoms of anxiety and depression concerning the degree of kinship showed that the children presented more symptoms when compared to other members of the family. Of the children, 50.0% presented anxiety symptoms and 37.5% symptoms of depression. The symptoms of depression in spouses/parents and siblings showed very similar prevalences, 32.4%, and 32.1%, respectively. Also regarding the children, 27.5% presented symptoms of anxiety or depression, and 30.0% presented both symptoms at the same time. However, uncles, nephews, and cousins presented a higher prevalence (36.67%) of anxiety or depression symptoms, as well as a lower prevalence of these symptoms together (3.33%).
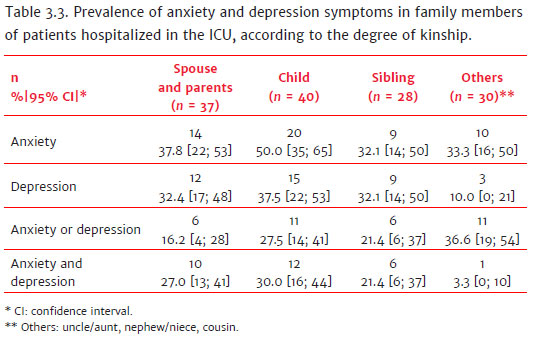
The final regression model identified that being a family member less than 40 years of age and living with the hospitalized relative was associated with cases of anxiety in the study population with the following data, respectively: (OR 2.20, CI 1.049-4.6540, p = 0.037) (OR 2.37, CI 1.121-5.024, p = 0.024). Regarding the presence of signs of depression, these were associated with the degree of kinship variable, which indicates the following finding: parents, children, and spouses present a potential for the onset of depression (OR 2.52, CI 1.096-5.814, p = 0.003).

4. Discussion
In recent decades there has been a growing number of investigations aimed at assessing the mental health of people in hospitalization situations and their family members. The focus of the research regarding the family in the ICU environment was centered on the needs and satisfaction of this group. However, in the last ten years, there has been a significant increase in the number of studies focused on the psychological changes undergone by the family (Fumis et al., 2015; Hwang et al., 2014; Kourti et al., 2015; McAdam & Puntillo, 2009; Rusinova et al., 2014; Schmidt & Azoulay, 2012). In the international context, there are initiatives in this direction with an emphasis on more structured studies which are reproducing the research. In the Brazilian scenario, this evaluation is still incipient, with few studies. However, these already allow the impressions of researchers in the area to be confirmed (Fumis & Deheizelin, 2009; Fumis et al., 2015; Maruiti et al., 2008). In this sense, the present study emerges as a new possibility of analysis of the symptoms of anxiety and depression in the national scenario.
The analysis of the prevalence of anxiety showed that 39.3% of the relatives presented these symptoms. Anxiety can trigger several negative consequences in the lives of individuals, such as the inability to perform daily tasks, loss of appetite and weight, gastric discomfort, excessive sweating, headaches, and changes in sleep patterns. For the family with a hospitalized relative, these consequences can be exacerbated by the feeling of uncertainty that is permanently established, as a result of frequent fluctuations in patients' clinical conditions (Schmidt & Azoulay, 2012).
At the national level, two investigations have evaluated the symptoms of anxiety in family members who had relatives hospitalized in the ICU. The first one was performed in a private general ICU, in the city of São Paulo, with 39 family members, in which 43.6% presented probable anxiety symptoms (Maruiti et al., 2008). The second, by Fumis and Deheizelin (2009), evaluated 300 relatives of cancer patients hospitalized in the ICU, with a mean of 9 days of hospitalization, and found a prevalence of anxiety symptoms higher than 71%. The prevalence was justified by the association between these symptoms and the clinical conditions of the hospitalized relative, on prolonged mechanical ventilation, with the presence of metastasis or progressive disease, recognized as indicatives of a poor prognosis. In the study by Maruiti et al. (2008), as well as in this study, the lower levels of anxiety were justified by the family's hope of recovery followed by the return of the hospitalized person to the social life.
In this study, living together with the family member and their age were identified as possible factors associated with anxiety. Thus, younger relatives and those who lived with the hospitalized patient presented higher chances of manifesting anxiety. The data found in this study, therefore, corroborate those of the study of Pochard et al. (2005), in which a younger age was also associated with higher chances of developing anxiety.
Regarding the aspect of living together, the results were similar to those investigated by Rusinova et al. (2014), that found that sharing the same residence was associated with higher chances of developing anxiety and depression. Thus, having a hospitalized relative that lived with the family member primarily generated an impact from the physical separation, due to interrupting the life together and preventing routine life activities, as well filling the gap of absence on the day to day. This absence in the family environment is expressed as an early loss due to the probability of a definitive split that causes the family to face the unknown, uncertainty, vulnerability and, consequently, generates mental suffering (Freitas et al., 2012).
In contrast, the development of anxiety symptoms has been related to the female sex, being the spouse of the hospitalized relative, the diagnosis of the patient associated with neurological diseases and traumatic injuries, a lower level of education, not having regular meetings with doctors and nurses, not having a specific meeting room, wanting guidance from a professional psychologist for coping strategies, and if the family has unmet needs (McAdam & Puntillo, 2009).
Thus, knowing the behavior of these variables in relatives of people hospitalized in the ICU is relevant so that action indicators can be proposed to reduce the impact of hospitalization on the mental health of the family members. According to Davidson et al. (2017), when the family receives effective support, anxiety symptoms are minimized. Support is related to the offer of assistance and help to the family members to provide them conditions to express their feelings and emotions. Thus, they can cope better with the experience, a factor reflected in the support provided by friends, professionals, and other family members, or spiritual support - which together can function as a support network for the family (Freitas et al., 2012).
Belayachi et al. (2014) correlated symptoms of anxiety and the lack of effective communication, and emphasized that anxiety and depression are likely to affect understanding, reasoning, and communication performance, a fact that should be considered when giving information in the hospital environment. In this context, a high level of anxiety may require the health care team to establish a qualified listener to continuously provide information. However, care should be taken regarding the quality of information provided by health services, which must be precise and provided comprehensibly. Also, the complexity of the information should be considered, taking into account those with a lower level of education (Davidson et al., 2017).
The analysis of depression prevalence in family members showed that 28.9% had probable symptoms of depression, that is, they presented a score higher than ten points when responding to the HADS evaluation instrument. The symptoms of depression in individuals, in general, are related to difficulty in concentrating, fatigue, and discouragement that consequently interfere in the daily routine, work, study, and leisure, as well as being linked to crying spells, hopelessness, negative thoughts, and difficulty to care for one self(Schmidt & Azoulay, 2012). In addition, it was possible to note family members evaluation through the HADS that other symptoms were present - such as not feeling enjoyment for the same things, slow thinking about daily activities and performing them, not being able to laugh or feel cheerful, difficulty in feeling pleasure in routine activities, which can therefore be confirmed as a case of depression so that those family members can undergo complementary analysis.
In the national context, the evaluation of depressive symptoms in family members who have relatives hospitalized in the ICU has been limited. Maruiti et al. (2008) found that 17.9% of the family members presented symptoms of depression. However, in a study carried out for the depression evaluation in an ICU for cancer patients in São Paulo, 50.3% of the family members presented symptoms of the disorder (Fumis & Deheizelin, 2009). In the present study, the family members that were children, parents, and spouses showed a higher tendency to develop depressive symptoms when compared to siblings, uncles/aunts, nephews/nieces, and cousins, data corroborated by the studies of Pochard et al. (2001, 2005).
This result can be deduced from the concept that the sudden absence of the family member generates greater vulnerability for children, parents, and spouses. Usually, they are the ones that establish relationships with the hospitalized member, due to the close affective bond, daily coexistence, and emotional dependence. Besides, these family members, with a narrower or first-degree relationship, have more responsibilities and are more burdened with the hospitalization of a member, or because they are the primary reference for the team at the moment of making decisions related to treatments and providing authorization for examinations. These family members are often solely responsible for transmitting information and communicating to other family members about the hospitalized relative (Pochard et al., 2005). These factors highlight the vulnerability of this group, indicating that special attention should be given to them - since they are the most overloaded during the hospitalization.
Although, in the present study, depressive symptoms were associated with the degree of kinship, international studies also found an increase in the possibility of developing depressive symptoms related to female family members, information transmitted inconsistently by the team, the desire for more information on the prognosis, and the desire for psychological support (Rusinova et al., 2014; Schmidt & Azoulay, 2012; Pochard et al., 2001).
The association of symptoms of anxiety and depression with the length of stay in the ICU was not evidenced in this study. This association has, however, been highlighted in discussions on the subject.
Regarding anxiety, the study by Kourti et al. (2015) did not show differences between periods of hospitalization. Although, in one study that evaluated the anxiety of family members of people with a mean hospitalization in the ICU of 5 to 8 days, the prevalence was lower (15.1%) (Hwang et al., 2014).
Symptoms of anxiety and depression tend to decrease after the hospital discharge of the relative. Nonetheless, they can persist for months or years after the experience. Coupled with these factors, after discharge from the ICU, family members may be at risk of developing post-traumatic stress symptoms and, after two months of hospital discharge or death, post-traumatic stress symptoms may begin to appear, as well as complicated mourning (Anderson et al., 2008; Davidson et al., 2017), events that require additional investigations in the Brazilian reality.
Therefore, it is highlighted that the hypothesis of family inclusion as a focus of care should be reinforced in the hospital setting. Davidson, Daly, Agan, Brady, & Higgins (2010), when writing about a family support program in intensive care, highlighted that interventions should be directed towards identifying and satisfying family's information needs, training them how to visit and satisfy their own needs, and providing them with support and possibilities for meaningful bedside activities.
The assessment of the mental health of the family members to screen for possible psychic changes during the period of hospitalization by the psychology team and other health providers is essential. The routine evaluation by health providers of family members, especially those with a history of psychic problems, should be implemented. It is also necessary to institute preventive strategies aimed at improving family well-being, essential factors to make this experience more comfortable and prevent the exacerbation of these symptoms. Examples of such initiatives include regular group meetings and the implementation of the open visit in the ICU. Because of the scarcity of studies investigating family conditions after ICU hospitalization, early interventions aimed at reducing the psychological burden of the family are feasible. Schmidt and Azoulay (2012) caution that some consequences may occur due to intense exposure to anxiety symptoms, such as the progression to Generalized Anxiety Disorder, or the symptoms of depression progressing to Major Depressive Disorder.
The hospitalization experience is inherently stressful and upsetting for the family. In this way, proper screening and referral become critical steps in reducing the adverse effects of this experience, both mentally and physically. For this purpose, professionals must incorporate care for the family member into their practice. However, for primary and quality care it is necessary for health providers to know the role of the family members in the period of hospitalization, as well as their needs and the psychological load that the hospitalization entails. It is necessary to replace a hospital practice that is essentially normative, controlling and hierarchical, with a praxis that incorporates ethical, sensitive, supportive and responsible care to achieve integral and quality care (Carlson, Spain, Muhtadie, McDade-Montez, & Macia, 2015).
Some limitations of the study can be highlighted, for example, the size of the sample and the cross-sectional, intentional or convenience type design. The study was carried out in a public institution of Bahia. Therefore the results obtained may not be extended to all relatives that have a member in an ICU. It is also believed that further studies should be performed to evaluate the HADS performance in this group.
References
Anderson, G., Arnold, R. M., Angus, D. C., & Bryce, C. L. (2008). Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. Journal of General Internal Medicine, 23(1),1871-1876. doi: 10.1007/s11606-008-0770-2 [ Links ]
Belayachi, J., Himmich, S., Madani, N., Abidi, K., Dendane, T., Zeggwagh, A. A., & Abouqal, R. (2014). Psychological burden in patient relatives: The forgotten side of medical management. QJM, 107(2),115-122. doi: 10.1093/qjmed/hct210 [ Links ]
Botega, J. N., Bio, M. R., Zomignani, M. A., Garcia Jr, C., & Pereira, W. A. B. (1995). Transtornos do humor em enfermaria de clínica médica e validação de escala de medida (HAD) de ansiedade e depressão. Revista de Saúde Pública, 5(29),355-363. doi: 10.1590/S0034-89101995000500004 [ Links ]
Carlson, E. B., Spain, D. A., Muhtadie, L., McDade-Montez, L., & Macia, K. S. (2015). Care and caring in the ICU: Family members' distress and perceptions about staff skills, communication, and emotional support. Journal Critical Care, 30(3),557-561. [ Links ]
Davidson, J. E., Daly, B. J., & Agan, D. (2010). Facilitated sensemaking: A feasibility study for the provision of a family support program in the intensive care unit. Critical Care Nursing Quarterly, 33(2),177-189. doi: 10.1097/CNQ.0b013e3181d91369 [ Links ]
Davidson, J. E., Aslakson, R., Long, A., Puntillo, K., Kross, E., Hart, J., ... Curtis, J. (2017). Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Critical Care Medicine, 45(1),103-128. doi: 10.1097/CCM.0000000000002169 [ Links ]
DeSousa, D. A., Moreno, A. L., Gauer, G., Manfro, G. G., & Koller, S. H. (2013). Revisão sistemática de instrumentos para avaliação de ansiedade na população brasileira. Avaliação Psicológica, 12(3),397-410. [ Links ]
Freitas, K. S., Mussi, F. C., & Menezes, I. G. (2012). Desconfortos vividos no cotidiano de familiares de pessoas internadas na UTI. Escola Anna Nery, 16(4),704-711. doi: 10.1590/S1414-81452012000400009 [ Links ]
Fumis, R. R. L., & Deheizelin, D. (2009). Family members of critically ill cancer patients: Assessing the symptoms of anxiety and depression. Intensive Care Medicine, 35(5),899-902. doi: 10.1007/s00134-009-1406-7 [ Links ]
Fumis, R. R., Ranzani, O. T., Faria, P. P., & Schettino, G. (2015). Anxiety, depression, and satisfaction in close relatives of patients in an open visiting policy intensive care unit in Brazil.Journal of Critical Care, 30(20),440.e1-440.e6. doi: 10.1016/j.jcrc.2014.11.022 [ Links ]
Hwang, D. Y., Yagoda, D., Perrey, H. M., Currier, P. F., Tehan, T. M., Guanci, M., ... Rosand, J. (2014). Anxiety and depression symptoms among families of adult intensive care unit survivors immediately following brief length of stay. Journal of Critical Care, 29(2),278-282. doi: 10.1016/j.jcrc.2013.11.022 [ Links ]
Kourti, M., Christofilou, E., & Kallergis, G. (2015). Anxiety and depression symptoms in family members of ICU patients. Avances en Enfermería, 33(1),47-54. doi: 10.15446/av.enferm.v33n1.48670 [ Links ]
Köse, I., Zincircioğlu, Ç., Öztürk, Y. K., Çakmak, M., Güldoğan, E. A., Demir, H. F., ... Gonullu, M. (2015). Factors affecting anxiety and depression symptoms in relatives of intensive care unit patients. Journal of Intensive Care Medicine, 31(9),611-617. doi: 10.1177/0885066615595791 [ Links ]
Maruiti, M. R., Galdeano, L. E., & Farah, O. G. D. (2008). Ansiedade e depressão em familiares de pacientes internados em unidade de cuidados intensivos. Acta Paulista de Enfermagem, 21(4),536-542. doi: 10.1590/S0103-21002008000400016 [ Links ]
McAdam, J. L., & Puntillo, K. (2009). Symptoms experienced by family members of patients in intensive care units. American Association of Critical Care, 18(3),200-209. doi: 10.4037/ajcc2009252 [ Links ]
Peduzzi, P., Concato, J., Kemper, E., Holford, T. R., & Feinstein, A. R. (1996). A simulation study of the number of events per variable in logistic regression analysis. Journal of Clinical Epidemiology, 49(12),1373-1379. [ Links ]
Pochard, F., Azoulay E., Chavret, S., Lemaire, F., Hubert, P., Canoui, P., ... French FAMIREA Group (2001). Symptoms of anxiety and depression in family members of intensive care unit patients: Ethical hypothesis regarding decision-making capacity. Critical Care Medicine, 29(10),1983-1987. [ Links ]
Pochard, F., Darmon, M., Fassier, T., Bollaert, P. E., Cheval, C., Coloigner, M., ... French FAMIREA Study Group (2005). Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death: A prospective multicenter study. Journal of Critical Care, 20(1),90-96. [ Links ]
Rusinova, K., Kukal, J., Simek, J., & Cerny, V. (2014). Limited family members/staff communication in intensive care units in the Czech and Slovak Republics considerably increases anxiety in patients relatives: The DEPRESS study. BMC Psychiatry, 14(21),1-7. doi: 10.1186/1471-244X-14-21 [ Links ]
Schmidt, M., & Azoulay, E. (2012). Having a loved one in the ICU: The forgotten family. Current Opinion in Critical Care, 18(5),540-547. doi: 10.1097/MCC.0b013e328357f141 [ Links ]
 Mailling address:
Mailling address:
Katia Santana Freitas
Universidade Estadual de Feira de Santana - UEFS - Departamento de Saúde, Módulo VI - MT 63
Av. Transnordestina, S/n, Novo Horizonte
Feira de Santana, BA, Brazil. CEP 44036-900
E-mail: ksfenfpro@hotmail.com
Submission: 17/05/2018
Acceptance: 20/12/2018











 texto em
texto em 


