Serviços Personalizados
artigo
Indicadores
Compartilhar
Psicologia: teoria e prática
versão impressa ISSN 1516-3687
Psicol. teor. prat. vol.21 no.3 São Paulo set./dez. 2019
http://dx.doi.org/10.5935/1980-6906/psicologia.v21n3p345-365
ARTICLES
CLINICAL PSYCHOLOGY
Effect of cognitive-behavioral therapy after treatment for adults with major depression
Efecto de la terapia cognitiva comportamental un año después tratamiento para transtorno depresivo mayor
Gessyka W. VeledaI; Mariane L. MolinaII; Ricardo A. da SilvaIII; Karen JansenIV; Carmem Beatriz NeufeldV; Luciano D. de M. SouzaVI
IDepartamento de Saúde e Comportamento, Universidade Católica de Pelotas (UCPel)
IIDepartamento de Saúde e Comportamento, Universidade Católica de Pelotas (UCPel)
IIIDepartamento de Saúde e Comportamento, Universidade Católica de Pelotas (UCPel)
IVDepartamento e Saúde e Comportamento , Universidade Católica de Pelotas (UCPel)
VDepartamento de Psicologia, Universidade de São Paulo (USP)
VIDepartamento e Saúde e Comportamento, Universidade Católica de Pelotas (UCPel)
ABSTRACT
In Brazil, little is known about the maintenance of results after treatment of cognitive-behavioral therapy (CBT) for major depressive disorder (MDD). The objective of this study was to verify the effectiveness of individual psychotherapeutic treatment from CBT for depressive symptoms within 6 and 12 months after the intervention. We evaluated 94 participants with MDD from the Beck Depression Inventory (BDI-II). There was significant posttreatment response (p < 0.001), with no difference between the end of the treatment and the symptom assessment at 6 (p = 0.486) and 12 months (p = 0.098). A significant positive correlation was observed between the intensity of depressive symptoms at the baseline and the reduction of initial symptoms for 12-month follow-up (r = 0.49; p < 0.001). CBT significantly reduces depressive symptoms by maintaining this condition up to 12 months post-intervention without significant influence of other characteristics beyond the intensity of depressive symptoms at the beginning of the therapeutic process.
Keywords: depressive disorder, depressive symptoms, cognitive Behavior therapy, follow up, effectiveness.
RESUMEN
Este estudio verificó la efectividad del tratamiento psicoterápico individual a partir de la terapia cognitiva conductual (TCC) para los síntomas depresivos dentro de los 6 y 12 meses post-intervención. Se evaluaron 94 participantes con TDM a partir del Inventario Beck de depresión (BDI-II). Se observó una respuesta significativa post-tratamiento (p < 0,001), no ocurrieron diferencias entre el final del tratamiento y la evaluación de los síntomas a los 6 (p = 0,486) y 12 meses (p = 0,098). Había una correlación positiva significativa entre la intensidad de los síntomas depresivos en el baseline y la reducción de los síntomas iniciales para el seguimiento de 12 meses (r = 0,49; p < 0,001). La TCC reduce significativamente los síntomas depresivos manteniendo esa condición hasta 12 meses después de la intervención sin influencia significativa de otras características además de la intensidad de los síntomas depresivos al inicio del proceso terapéutico.
Palabras clave: trastorno depresivo; síntomas depresivos; terapia cognitiva conductual; seguimiento; efectividad.
1. Introduction
Major depressive disorder (MDD) is known for being a common clinical condition that generates a big economic impact on health policies due to its high prevalence and its debilitating nature (Greenberg, Fournier, Sisitsky, Pike, & Kessler, 2015). Moreover, the impact of these symptoms in people's lives is very strong, causing clinically significant suffering and harm (Marcus & Olfson, 2010). Due to these characteristics, in the last decade, a substantial increase in the search for alternatives to the treatment of depression occurred, mainly on psychotherapeutic interventions. Controlled and comparative studies have been published showing the efficacy of psychological treatment in depressive symptom decrease (Cuijpers et al., 2011).
Among psychotherapeutic alternatives, cognitive behavioral therapy (CBT) is regarded as being the most suitable and the most researched for the treatment of depression in adults. This approach has been shown to be favorable for consisting of a brief model, prone to be empirically tested, with symptom decrease being demonstrated in the short term, besides showing lower relapse indices (Lang & Borgwardt, 2013).
In a meta-analysis carried out with 115 studies, which verified the effects of CBT compared to control groups, other psychotherapies, and pharmacologic intervention, it was shown that CBT is an effective treatment for depression in adults when compared to the control group (Cuijpers et al., 2013). These findings also seem to apply to depressed individuals who are resistant to treatment, given that two meta-analyses pointed out that CBT is as effective as antidepressant medication treatment by itself and that the combination of both significantly improve treatment efficacy (Cuijpers et al., 2014).
However, the biggest challenges found in depression treatment are related to relapse rates or symptom reoccurrence, which remain elevated and tend to increase with the number of prior episodes (Koster, Hoorelbeke, Onraedt, Owens, & Derakshan, 2017). After a first depression episode, the likelihood of an addition episode occurring is of approximately 50%; this raises to 70% after two episodes and 90% after a third episode (Burcusa & Iacono, 2007). Moreover, factors such as the age of the first episode, severity, comorbidity, Family history, dysfunctional cognitions, personality (neuroticism), poor social support and stressing life events are considered to be risk factors for the occurrence of new episodes (Kessler et al., 1996).
When evaluated in the medium and long terms, the benefits of CBT are maintained, supporting an effective response to treatment. In two randomized clinical trials (Nakagawa et al., 2017; Wiles et al., 2016) carried out with adults diagnosed with treatment-resistant MDD, it was observed 6 and 12 months after the intervention, the remission rates were significantly higher in the group exposed to CBT. The Beck Depression Inventory scores also decreased with time. In a study made by Wiles et al. (2016), the group treated with CBT, 46 months after the intervention, presented lower scores of depressive symptoms than the control group. In repeated measurements analysis, using data from 6, 12 and 46 months, the individuals in the intervention group showed a BDI-II score that was, on average, four points lower throughout the 46 months in comparison to the group with only psychotropics. However, the presence of relapse and reoccurrence was common, even among those who responded to CBT. Vittengl, Clark, Dunn e Jarrett (2007) conducted a meta-analysis research that gathered 28 studies including 1800 adults, concluded that in a year after treatment, 29% of patients showed a relapse episode or reoccurrence, increasing to 54% two years after.
Even with promising results, there are still gaps referring to CBT effectiveness in the medium and long term, especially in the Brazilian context. Thus, the objective of this study was to verify the impact of psychotherapeutic treatment in depressive symptom response within six months and a year after the intervention.
2. Method
2.1 Study and participant design
This is a quasi-experimental research of temporal series joined with randomized clinical trial research that began in July of 2012 and ended in January of 2017, approved by the Catholic University of Pelotas Committee (02855312.6.0000.5339). The objective of the clinical trial was to test the efficacy of two brief models of psychotherapy for depression (supportive-expressive dynamic psychotherapy and cognitive behavioral therapy). This paper will only present data referring to CBT. All participants were informed about the study and signed a consent form.
Individuals of ages between 18 and 60 were invited to participate in the study, chosen by convenience, through divulgation in the Basic Health Units (UBS), Psychosocial Attention Centers (CAPS) and other municipal healthcare services, aside from schools and communication methods in the city of Pelotas (newspapers, websites, radio and television). After diagnosed and evaluated by the research team, patients were randomized for both interventions in the bigger study, with 158 adults randomized for CBT treatment. Inclusion criteria were being between 18 and 60 years old, having been evaluated and diagnosed with MDD by the research team and participating at least until the third out of 16 sessions.
Exclusion criteria were individuals who at the moment of evaluation were being treated for MDD in another place, presented moderate or severe suicide risk, psychotic symptoms and psychoactive substance abuse (except for tobacco and alcohol), evaluated, respectively, by modules C, K, and L from Mini International Neuropsychiatric Interview in its Plus version (MINI Plus) (Sheehan et al., 1998). The final sample was made of 94 participants, out of these, 56 individuals concluded the intervention and went through the final evaluation, 65 answered the 6-month evaluation, and 61 were evaluated 12 months after treatment.
2.2 Instruments
The participants economic level was measured according to the Brazilian Economic Classification Criteria, made by the Brazilian Research Company Association (ABEP). This classification divides the population into five economic levels; A, B, C, D, and E. For data analysis, this variable was considered dichotomic; A/B or C/D/E.
MDD diagnosis, as well as the psychiatric comorbidities, were made using the Mini International Neuropsychiatric Interview in its Plus Version (MINI Plus). That is an interview adapted to clinical context and represents an adequate and less expensive alternative for patient selection and evaluation, following international criteria both in clinical studies and epidemiological studies (Azevedo Marques & Zuardi, 2008; Amorim, 2000).
We used the Millon Clinical Multiaxial Inventory - III (MCMI-III) to diagnose personality disorders. It is composed of 175 affirmatives, with "true" or "false" answer options. From this data, the indicators of schizoid, schizotypical, paranoid, borderline, anti-social, narcissist, histrionic, dependent, avoidant, and obsessive-compulsive personality disorders were presented (Rocha et al., 2011).
For the measuring and comparison of depressive symptoms of initial, final, 6-month and a year period after treatment, total scores from the Beck Depression Inventory were used. This self-applied scale is made of 21 items, each one measured by a 0 to 3-point Likert scale, generating a total score of 0 to 63 points representing depressive symptom severity (Gomes-Oliveira, Gorenstein, Lotufo, Andrade, & Wang, 2012). This instrument has been widely used to evaluate the presence and severity of depressive symptoms (Gomes-Oliveira et al., 2012). Through these evaluations, a quantitative variable was elaborated and named as Delta of depressive symptom reduction, which represents the difference of depressive symptom quantity at the beginning and 12 months after treatment.
2.3 Procedures
Patients eligible for this research answered a questionnaire with sociodemographic data (sex, age, economic level, schooling, occupation, marital status) and went through a symptomatology evaluation using BDI-II (Gomes-Oliveira et al., 2012). After that, patients received individual 14-session long CBT treatment, once a week, 50 minutes per session. Aside from these, two sessions, the first and the last one, were used for instrument application, adding up to 16 sessions in total. In the last session, just like in the first one, symptom evaluation was carried out using the same instrument.
In the CBT treatment process, the four initial sessions were used for patient psychoeducation on MDD and the cognitive model, as well as the development of the cognitive conceptualization (Beck, 2013). The next eight sessions were used to apply cognitive techniques (self-monitoring, Socratic questioning, problem-solving, pros, and cons, etc.) focusing on cognitive restructuring and behavioral activation. The techniques were adapted for the context and demand of each patient. Every session followed the session structure proposed by Beck (2013), and the topics of the session's agenda were suggested by the patients and chosen along with the psychotherapist. The last three sessions aimed to work on treatment ending and relapse prevention, followed by the final evaluation in the last session.
Psychotherapy was carried out at the Mental Health Research and Extension Outpatient Clinic by psychologists and senior students of the UCPel undergraduate course in the Psychology and the Postgraduate Program in Health and Behavior at the Catholic University of Pelotas. Each therapist received CBT training from the study coordinators and was supervised by one of the researchers, who have training and education in CBT and clinical psychology.
Patients were evaluated after the psychotherapeutic intervention and in two other moments, at 6 and 12 months after the intervention. From the available data, we made telephone calls to contact the patients after the intervention. In these follow-up evaluations, the depressive symptomatology was measured through BDI-II, as well as through a questionnaire containing the main clinical information of the patient in the post-treatment period.
2.4 Data processing and analysis
Data were processed on tablets using the Open Data Kit (ODK) system. After being transferred, they were analyzed in the Statistical Package for Social Sciences program (SPSS 21.0). Initially, a univariate analysis was performed in order to describe, through absolute and relative frequency, the qualitative variables of this study. In addition, in the univariate analysis, measures of central tendency and dispersion of the investigated quantitative variables were presented.
In order to perform the intention-to-treat analysis, the information lost on the BDI-II instrument at the end of treatment, follow-up evaluations of 6 months and 12 months were replaced by imputations according to the median presented by the group in question.
The Friedman test was used to compare the intensity of depressive symptoms at baseline, at the end, at six months and one year after treatment. The Wilcoxon test was used to evaluate the significance of depressive symptom reduction in relation to their intensity at the beginning of the psychotherapy, as well as the difference in the follow-ups in relation to end-of-treatment scores.
The Mann-Whitney U test was used to verify the distribution of the dichotomous independent variables in relation to the difference of the depressive symptoms at baseline and 12 months post follow up. For the variables with three categories, the Kruskal-Wallis test was performed. The Spearman Correlation coefficient was used to analyze the intensity of depressive symptoms at the beginning of treatment in relation to the difference in initial depressive symptoms and at 12 months post-treatment. Finally, we conducted an adjusted analysis using linear regression for the analysis of the Delta variable of reduction of depressive symptoms, without variable hierarchy, inserting those with significance value p < 0.20 in the crude analysis. Associations that presented p < 0,05 were considered statistically significant.
3. Results
Among the participants, the majority were women (87.2%), white (80.9%), and were 37 years old on average (19-59; ± 11.7), belonging to economic classes C, D or E (53.2%). More than half had 9 or more years of study (73.4%), worked and/or studied at the time of the interview (68.1%), had children (69.1%) and a partner (61.7%).
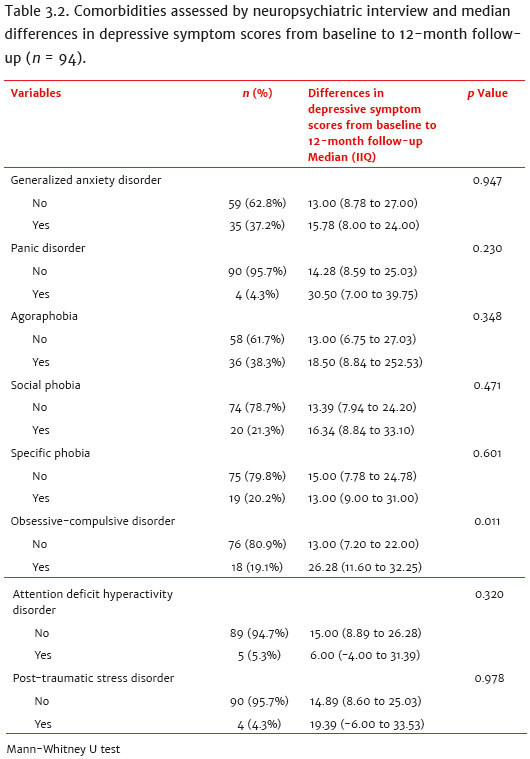
As for the clinical characterization of the sample, 80.9% of the participants had, in addition to MDD, other psychiatric comorbidities evaluated by the clinical MINI PLUS interview.
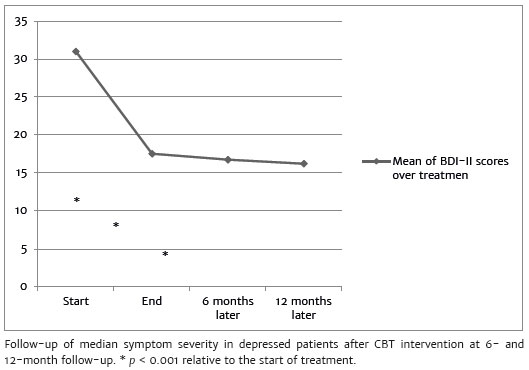
During treatment and subsequent evaluations, median scores for depressive symptoms dropped. The median BDI-II score was 31 points (IIQ 24.00 to 41.00) at the beginning of the treatment, dropping to 17.53 (IIQ 10.50 to 21.25) at the end of the psychotherapeutic intervention. In the 6 and 12-month follow-up after treatment, the median BDI-II were 16.74 (IIQ 7.00 to 20.00) and 16.22 (IIQ 7.00 to 16.41), respectively. There was a significant reduction of depressive symptoms from the beginning of the treatment to the end of the treatment (z = -7.599; p < 0.001), for the 6-month follow-up (z = -7,762, p < 0.001) and for the 12-month follow-up (z = -7,963, p < 0.001). There were no significant differences in the scores of depressive symptoms at the end of treatment when compared to the 6-month follow-up (z = -0.698; p = 0.486), indicating a continuity of these scores after the intervention, and a trend towards lower symptom intensity at 12 months (z = -1,659, p = 0.098)
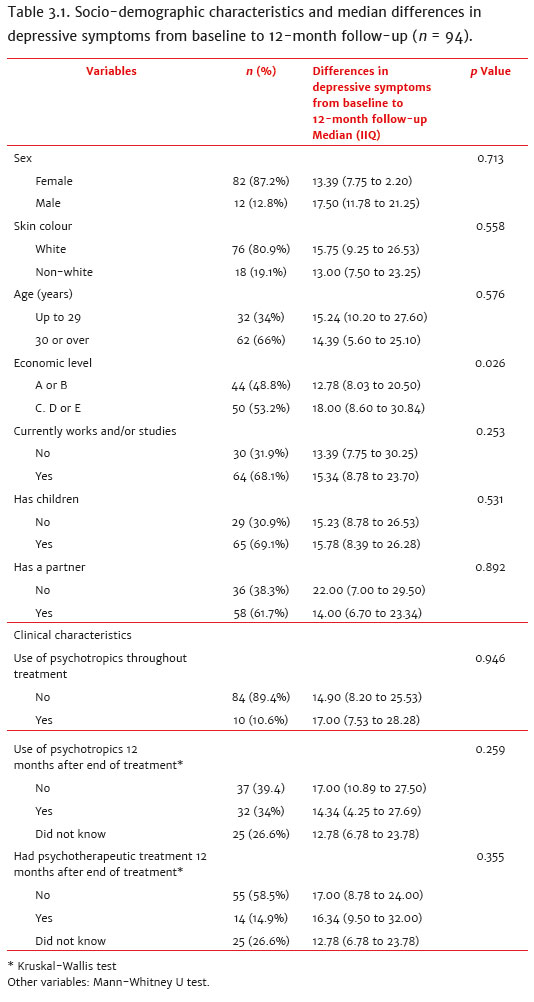
The difference in the depressive symptom score from the beginning of the treatment to the 12-month follow-up presented a median of 14.89 points in the BDI-II score (IIQ 8.59 to 26.03) (Table 3.1). Regarding the sociodemographic characteristics, there was a statistically significant difference between the economic class levels (p = 0.027). Participants in classes C, D or E showed greater differences in the scores of depressive symptoms (18.00, IIQ 8.6 to 30.84) when compared to participants in class A / B (12.78, IIQ 8.03 to 20.50).
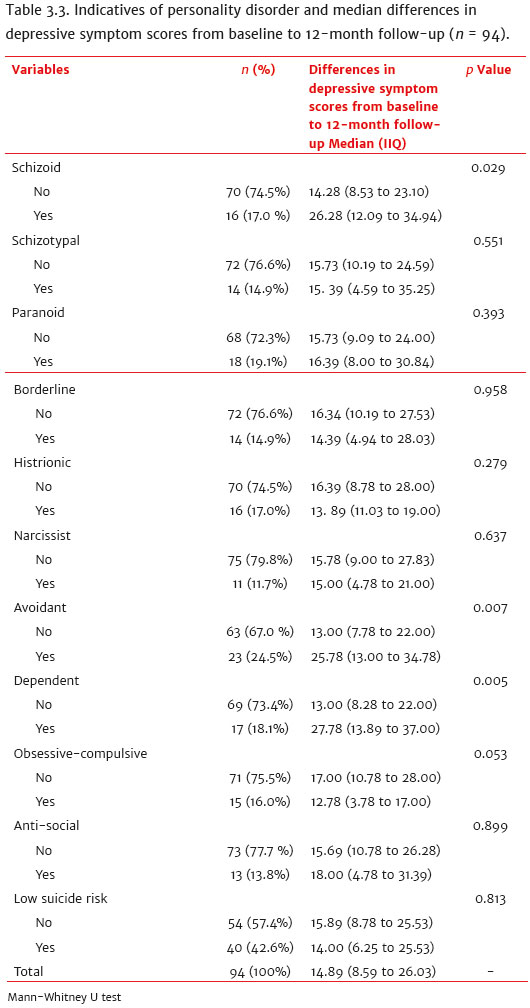
After analyzing the clinical variables, we discovered that the presence of obsessive-compulsive personality disorder (OCD) was significantly related (p = 0.012) to greater differences in BDI-II scores (26.28; IIQ 11.6; 32.25) when compared to participants without OCD (13.00, IIQ 7.20, 22.00) (Table 2). There were also significant differences between the participants with schizoid personality disorder (p = 0.030), avoidant (p = 0.008) and dependent (p = 0.006) differences in the initial and 12-month post-treatment depressive symptom scores. Among participants with these comorbidities, deltas were larger in comparison to participants without these comorbidities (Table 3). However, participants with OCD had a lower delta median (12.78; IIQ 3.78 to 17.00) compared to the participants without the disorder (17.00; IIQ 10.78 to 28.00), pointing to a significant difference (p = 0.054).
The intensity of depressive symptoms at the beginning of the treatment was moderately correlated to the difference in depressive symptoms between the beginning of the treatment and 12 months after treatment (r = 0.49, p < 0.001). Other sociodemographic and clinical variables did not present significant differences in relation to the medians of the difference in BDI-II scores at the baseline and at the 12-month follow-up (Table 3.1).
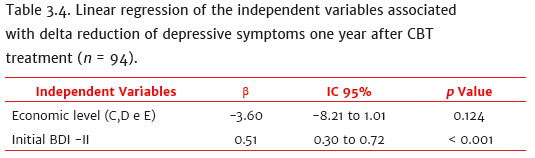
Multivariate analysis showed that only the initial depressive symptom score had a significant association with the decrease in depressive symptoms (p < 0.001). The economic level did not show a significant association to depressive symptom decrease, but remained in the analysis model (p = 0.123) (Table 4).
4. Discussion
The present study evaluated the effectiveness of CBT psychotherapeutic treatment in depressive symptoms within six months and one year after the intervention and found a significant decrease in depressive symptoms shortly after treatment, maintained 12 months post-treatment. Depressive symptom intensity at baseline is positively correlated with a decrease in depressive symptoms 12 months after treatment, without significant influence of other sociodemographic or clinical characteristics.
In a post-intervention follow-up, Wiles et al. (2016) also found a decrease in BDI-II scores over the 6- and 12-month periods, compared to the initial scores in a sample of 285 adults with treatment-resistant MDD, who received intervention in CBT plus pharmacotherapy. At the end of 46 months after follow-up, mean BDI-II scores were 19.2 points, with no significant difference in relation to scores of 6- and 12- month follow-up. Our results also indicate that depressive symptoms decrease shortly after the intervention, and over time, they do not undergo significant changes, reaching a median of 16.22 points, thus, demonstrating maintenance of the therapeutic gains. It is important to note that the median of the final scores, when compared to the median of the 12-month post-intervention scores, showed a tendency to lower symptoms, but not significantly. Despite the differences between the clinical aspects of the two samples, the depressive symptom scores evaluated through the same instrument were Yesilar at the beginning of treatment and at the 12-month follow-up, possibly showing the same phenomenon.
Using different instruments to evaluate depressive symptoms, other studies have also found benefits of CBT in the long term. Nakagawa et al. (2017), comparing subjects with treatment-resistant MDD who also received 16 sessions of CBT plus pharmacotherapy treatment with a group that received only medication, found a greater proportion of remission in depressive symptoms (evaluated by GRID-Hamilton Depression Rating Scale, altered version of the Hamilton scale) at the end of treatment in the CBT plus pharmacology group. At 6- and 12- month follow up, the severity of depressive symptoms remained even lower in the CBT group. It is important to emphasize that when these symptoms were analyzed from the BDI-II scale, no significant differences were found. Greater depressive symptom variability, made possible by BDI-II, may be related to these differences.
In addition to being effective, CBT seems to be indicated for different MDD diagnosed patient profiles. No evidence was found that socio-demographic characteristics such as gender, schooling, economic condition, or specific clinical aspects, such as comorbidity with other disorders, interfere with intervention outcome, except for depressive symptom severity at the beginning of treatment. Barth et al. (2016), in a meta-analysis with 198 randomized clinical trials, using different clinical interventions for the treatment of the major depressive disorder (including CBD) also found no difference in effect in different patient populations and intervention formats. Thus, people with different social and clinical characteristics appear to respond in a Yesilarly effective way to CBT treatment.
Yesilar to the correlation found between the intensity of depressive symptoms at the beginning of treatment and the reduction of these symptoms one year after the intervention, Hollon et al. (2014) found a significant improvement in patients with more severe depression, compared to long-term combination therapy (CBT plus pharmacotherapy), compared to exclusively pharmacological treatment.
Thus, it is suggested that individuals with more severe depressive symptoms ben efit more from both exclusive and combined psychotherapeutic interventions in the long term, although more research on the subject is necessary. However, there are no indications in the literature for significant improvement of depressive symptoms compared to their initial intensity when investigated exclusively for the effects of CBT. It should be noted that this study did not exclude patients with severe depression indicated by the BDI-II, but excluded individuals who could present greater therapeutic complexity for reporting moderate or severe suicide risk, psychotic symptoms and/or abusive use of some psychoactive substance in the initial evaluation.
One of the possibilities for explaining the expressive effect of CBT in long-term treatment is its psychoeducational characteristic. Through being taught new skills, patients learn to manage their moods better and therefore have cognitive and behavioral benefits that are kept even after the end of psychotherapy. Meta-analyses of trials in this area show that access to knowledge about the disorder and on the cognitive model proposed by CBT reduces the risk of depressive symptom relapse (Cuijpers et al., 2013, Vittengl et al., 2007). This possibility corroborates a qualitative study that interviewed nine individuals about their use of skills acquired in CBT treatment ten months after the end of treatment, demonstrating that patients still continued to use some of the skills learned (Glasman, Finlay, & Brock, 2004).
The findings of the study should be interpreted, considering some limitations. A significant number of patients did not a complete treatment or follow-up evaluations. However, the intention-to-treat analysis aims to minimize this potential setback (Barth et al., 2016). The use of only one instrument to evaluate the outcome also limits the conclusions. The BDI-II, although tested and reliable, proposes to evaluate only the depressive symptomatology, resulting in a lack of clinical analysis of MDD remission after follow-up. Moreover, the lack of a control group, such as a waitlist or exclusive use of pharmacological intervention group also limits the findings, since it could subsidize analyzes on the specific benefits of cognitive-behavioral intervention in comparison to other conditions.
Few studies used a single intervention model. In the study by Hollon et al. (2014), 114 individuals with severe and moderate major depressive disorder were randomized into three groups and followed up for 12 months: patients who responded to acute-phase Cognitive Therapy (CT) after 16 sessions (n = 35), patients who responded to treatment (n = 34) and patients who responded to pharmacological treatment in the acute phase, but the medication was removed and replaced by placebo (n = 35). Patients in the CT group had a significantly lower probability of relapse during the 12 months compared to patients who continued using placebo and were no more prone to relapse than patients who continued medication. Thus, like the results of the present study, exclusive CBT treatment presents satisfactory results after treatment, possibly reducing the risk of relapse
However, analyzing the cutoff points indicated by BDI-II for assessing the intensity of depressive symptoms, which are: minimal (0-13 points), mild (14-19 points), moderate (20-28 points), and severe (29-63 points) (Gorenstein, Pang, Argimon, & Werlang, 2011); it is observed that participants no longer fulfilled the criteria for predominantly severe depressive symptoms throughout 12 months (31.00; IIQ 24.00 to 41.00), now mainly fulfilling the criteria for the mild symptom group (16,22; HCl 7.00 to 16.41). Nonetheless, at the end of treatment, and one year later, these patients still had significant symptoms of depression and did not fit into the minimal symptom category. These results indicate the need for improvement in the practices of this intervention. An alternative for the improvement of results is the implementation of monthly maintenance sessions, as a continuation of treatment based on CBT. Vittengl et al. (2007), in a meta-analysis with 28 studies, found that a phase of treatment continuation significantly reduces relapse and/or recurrence compared to acute-phase treatments, during the period in which continuation treatment is in effect and after the end of the continuation phase in subsequent follow-ups. Further studies comprising monthly follow-up sessions should be performed to assess further depressive symptom reduction one year after weekly treatment totaling 16 sessions.
Finally, it was concluded that CBT was effective in reducing depressive symptoms at the end of the intervention and maintaining these gains over the following 12 months, even for patients with severe symptoms at the beginning of treatment, such symptom reduction remained the same regardless of the patient's sociodemographic profile.
References
Amorim, P. (2000). Mini International Neuropsychiatric Interview (MINI): Validação de entrevista breve para diagnóstico de transtornos mentais. Revista Brasileira de Psiquiatria, 22(3),106-15. doi:10.1590/S1516-44462000000300003 [ Links ]
Azevedo Marques, J. M. de, & Zuardi, A. W. (2008). Validity and applicability of the Mini International Neuropsychiatric Interview administered by family medicine residents in primary health care in Brazil. General Hospital Psychiatry, 30(4),303-310. doi:10.1016/j.genhosppsych.2008.02.001 [ Links ]
Barth, J., Munder, T., Gerger, H., Nüesch, E., Trelle, S., Znoj, H., Jüni P., & Cuijpers, P. (2016). Comparative efficacy of seven psychotherapeutic interventions for patients with depression: A network meta-analysis. Focus, 14(2),229-243. doi:10.1371/journal.pmed.1001454 [ Links ]
Beck, J. S. (2013). Terapia cognitivo-comportamental: Teoria e prática (S. Mallmannda Rosa, Trad.). Porto Alegre: Artmed. [ Links ]
Burcusa, S. L., & Iacono, W. G. (2007). Risk for recurrence in depression. Clinical Psychology Review, 27(8),959-985. doi:10.1016/j.cpr.2007.02.005 [ Links ]
Cuijpers, P., Berking, M., Andersson, G., Quigley, L., Kleiboer, A., & Dobson, K. S. (2013). A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. The Canadian Journal of Psychiatry, 58(7),376-385. doi:10.1177/070674371305800702 [ Links ]
Cuijpers, P., Clignet, F., Meijel, B., van, Straten, A., van, Li, J., & Andersson, G. (2011). Psychological treatment of depression in inpatients: A systematic review and meta-analysis. Clinical Psychology Review, 31(3),353-360. doi:10.1016/j.cpr.2011.01.002 [ Links ]
Cuijpers, P., Karyotaki, E., Weitz, E., Andersson, G., Hollon, S. D., & Straten, A., van (2014). The effects of psychotherapies for major depression in adults on remission, recovery and improvement: A meta-analysis. Journal of affective disorders, 159,118-126. doi:10.1016/j.jad.2014.02.026 [ Links ]
Glasman, D., Finlay, W. M. L., & Brock, D. (2004). Becoming a self-therapist: Using cognitive behavioural therapy for recurrent depression and/or dysthymia after completing therapy. Psychology and Psychotherapy: Theory, Research and Practice, 77(3),335-351. doi:10.1348/1476083041839385 [ Links ]
Gomes-Oliveira, M. H., Gorenstein, C., Lotufo, Neto, F., Andrade, L. H., & Wang, Y. P. (2012). Validation of the Brazilian Portuguese version of the Beck Depression Inventory-II in a community sample. Revista Brasileira de Psiquiatria, 34(4),389-394. doi:10.1016/j.rbp.2012.03.005 [ Links ]
Gorenstein, C., Pang, W. Y., Argimon, I. L., & Werlang, B. S. G. (2011). Inventário Beck de Depressão-II: Manual. São Paulo: Casa do Psicólogo. [ Links ]
Greenberg, P. E., Fournier, A. A., Sisitsky, T., Pike, C. T., & Kessler, R. C. (2015). The economic burden of adults with major depressive disorder in the United States (2005 and 2010). The Journal of Clinical Psychiatry, 76(2),155-162. doi:10.4088/JCP.14m09298 [ Links ]
Hollon, S. D., DeRubeis, R. J., Fawcett, J., Amsterdam, J. D., Shelton, R. C., Zajecka, J., Young P.R., & Gallop, R. (2014). Effect of cognitive therapy with antidepressant medications vs antidepressants alone on the rate of recovery in major depressive disorder: A randomized clinical trial. JAMA Psychiatry, 71(10),1157-1164. doi:10.1001/jamapsychiatry.2014.1054 [ Links ]
Kessler, R. C., Nelson, C. B., McGonagle, K. A., Edlund, M. J., Frank, R. G., & Leaf, P. J. (1996). The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. American Journal of Orthopsychiatry, 66(1),17-31. doi:10.1037/h0080151 [ Links ]
Koster, E. H., Hoorelbeke, K., Onraedt, T., Owens, M., & Derakshan, N. (2017). Cognitive control interventions for depression: A systematic review of findings from training studies. Clinical Psychology Review, 53,79-92. doi:10.1016/j.cpr.2017.02.002 [ Links ]
Lang, U. E., & Borgwardt, S. (2013). Molecular mechanisms of depression: Perspectives on new treatment strategies. Cellular Physiology and Biochemistry, 31(6), p.761-777. doi:10.1159/000350094 [ Links ]
Marcus, S. C., & Olfson, M. (2010). National trends in the treatment for depression from 1998 to 2007. Archives of General Psychiatry, 67(12),1265-1273. doi:10.1001/archgenpsychiatry.2010.151 [ Links ]
Nakagawa, A., Mitsuda, D., Sado, M., Abe, T., Fujisawa, D., Kikuchi, T., Iwashita S., Mimura M., & Ono, Y. (2017). Effectiveness of supplementary cognitive-behavioral therapy for pharmacotherapy-resistant depression: A randomized controlled trial. The Journal of Clinical Psychiatry, 78(8),1126-1135. doi:10.4088/JCP.15m10511 [ Links ]
Rocha, H. R., Rodrigues P. D., Sousa, H. K. C. D., Alchieri, J. C., Sales, E. D. A., & Alencar, J. C. N. D. (2011). Estudos de adaptação do Millon Clinical Multiaxial Inventory-III para avaliação de aspectos psicopatológicos da personalidade no Brasil. Jornal Brasileiro de Psiquiatria, 60(1),34-39. doi:10.1590/S0047-20852011000100007 [ Links ]
Vittengl, J. R., Clark, L. A., Dunn, T. W., & Jarrett, R. B. (2007). Reducing relapse and recurrence in unipolar depression: A comparative meta-analysis of cognitive-behavioral therapy's effects. Journal of Consulting and Clinical Psychology, 75(3),475-488. doi:10.1037/0022-006X.75.3.475 [ Links ]
Wiles, N. J., Thomas, L., Turner, N., Garfield, K., Kounali, D., Campbell, J., Kessler D., Kuyken W., Lewis G., Morrison J., Williams C., Peters T. J., & Williams, C. (2016). Long-term effectiveness and cost-effectiveness of cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary care: Follow-up of the CoBalT randomised controlled trial. The Lancet Psychiatry, 3(2),137-144. doi:10.1016/S2215-0366(15)00495-2 [ Links ]
 Mailling address:
Mailling address:
Gessyka Wanglon Veleda
Rua Gonçalves Chaves, 373, sala 418 C, Centro
Pelotas, Rio Grande do Sul, Brazil CEP 96015-560
E-mail: gessykawveleda@gmail.com
Submission: 19/10/2018
Acceptance: 03/06/2019











 texto em
texto em 


