Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Psicologia: teoria e prática
versão impressa ISSN 1516-3687
Psicol. teor. prat. vol.22 no.3 São Paulo set./dez. 2020
RTICLES
CLINICAL PSYCHOLOGY
Evaluation of depressive symptoms in a sample with social anxiety disorder
Evaluación de sintomas depresivos en una muestra con transtorno de ansiedad social
Bruna F. RiosI ; Priscila de C. PalmaI
; Priscila de C. PalmaI ; Kátia Alessandra de S. CaetanoII
; Kátia Alessandra de S. CaetanoII ; Luciano D. de MattosIII
; Luciano D. de MattosIII ; Carmem Beatriz NeufeldI
; Carmem Beatriz NeufeldI
IUniversity of São Paulo (USP), Ribeirão Preto, SP, Brazil
IIEast Behavior Therapy Center, California, CA, United States
IIIPelotas Catholic University (UCPEL), Pelotas, RS, Brazil
ABSTRACT
Individuals with Social Anxiety Disorder (SAD) often also experience depression. This study's objective was to verify the levels of depression present in a sample of individuals diagnosed with SAD and to characterize this sample according to sociodemographic variables. There were 104 participants diagnosed with SAD from a pre-existing database. The sociodemographic and clinical data were analyzed through descriptive statistics, as well as inferential statistics on levels of social anxiety and depressive symptoms, obtained through the Social Anxiety Inventory (SPIN) and Beck Depression Inventory (BDI-II). It was found that more than half of the people had Major Depressive Disorder as a secondary diagnosis and that higher levels of social anxiety correlated positively with higher levels of depressive symptoms. These data show the relationship between depression and social anxiety and corroborate the findings of the literature.
Keywords: social anxiety disorder; depression; comorbidity; correlation; SAD.
RESUMEN
Las personas con trastorno de ansiedad social (TAS) a menudo también experimentan depresión. El objetivo de este trabajo fue verificar los niveles de depresión presentes en una muestra de individuos diagnosticados con TAS, así caracterizar esta muestra de acuerdo con las variables sociodemográficas. Hubo 104 participantes diagnosticados con TAS provenientes de una base de datos preexistente. Los datos sociodemográficos y clínicos fueron analizados mediante estadística descriptiva, así como estadísticas inferenciales sobre los niveles de ansiedad social y síntomas depresivos, obtenidos a través del Inventario de Ansiedad Social (SPIN) y el Inventario de Depresión de Beck (BDI-II). Se encontró que más de la mitad de las personas tenían un trastorno depresivo mayor como diagnóstico secundario, y que los niveles más altos de ansiedad social se correlacionaron positivamente con niveles más altos de síntomas depresivos. Estos datos destacan la relación entre la depresión y la ansiedad social, y corroboran los hallazgos de la literatura.
Palabras clave: trastorno de ansiedad social; depresión; comorbilidad; correlación; TAS.
1. Introduction
According to the Diagnostic and Statistical Manual of Mental Disorders - DSM-5 (American Psychiatry Association [APA], 2013), Social Anxiety Disorder (SAD) is characterized by intense feelings of fear or anxiety in social situations, especially when the individual feels that there is a possibility of being evaluated by others, fearing ridicule. The individual is concerned about receiving a negative evaluation from other people, being afraid of acting inappropriately, or showing anxiety symptoms such as flushing, trembling, sweating, or inattention. Worrying social situations will often be avoided or endured with intense fear and anxiety. Social Anxiety Disorder, due to its acute symptoms, generally negatively affects academic performance, productivity, interpersonal relationships, and the quality of life (Taylor et al., 2018).
It can start early, developing mainly in children who suffer bullying, rejection, exposure to ridicule, humiliation, or other stressful situations seen as traumatic, such as the divorce of the parents, sexual abuse, and conflicts in the family environment. Also, there is evidence that genetic factors have a major influence on the occurrence of the disorder. However, it is not yet known how the genotype acts to change the behavioral mechanism (Nardi, Quevedo, & Silva, 2014).
Women present SAD more frequently, starting in childhood or adolescence and quickly becoming chronic (Kuru et al., 2017). It has a lifetime prevalence of 12.1% and is characterized as the fourth most recurrent psychiatric disorder (Ito, Roso, Tiwari, Kendall, & Asbahr, 2008). In addition, SAD is the most common anxiety disorder, often being underdiagnosed and untreated, resulting in severe functional impairments, as spontaneous remission does not occur in most cases (Gonçalves et al., 2014; Muller, Trentini, Zanini, & Lopes, 2015).
Social Anxiety Disorder is related to lower levels of education and unemployment, representing a high cost for society, in addition to the suffering generated for the individual (APA, 2013; Nardi et al., 2014). The vast majority of individuals diagnosed with SAD also have additional comorbid psychiatric conditions, mainly depression and other anxiety disorders (APA, 2013).
Even with the high rate of SAD and depressive disorder comorbidities, the literature is still unclear about which disorder precedes the other. Nardi et al. (2014) found that patients presenting diagnostic criteria for SAD exhibit a "general demoralization syndrome," responsible for symptoms of depressed mood, causing depressed patients to restrict their social activities due to loss of interest and pleasure and not due to anxiety symptoms. Stein et al. (2001) found that anxiety disorder preceded depression. The chronic social isolation that SAD generates can lead to a Major Depressive Disorder (MDD), preceding it in 70% of cases (Wong, Morrison, Heimberg, Goldin, & Gross, 2014). In addition, the risks of suicide associated with depression are even more evident when this disorder is combined with social anxiety (APA, 2013). Therefore, SAD can directly influence mood disorders' risks and development (Stein et al., 2001).
A recent study by Hamilton et al. (2016) found indications that depression could precede social anxiety. Vaananen et al. (2014) conducted a study with 2,070 adolescents, in which they measured levels of depressive symptoms and social anxiety through the Beck Depression Inventory (BDI) and the Social Phobia Inventory (SPIN), with a further application of these instruments carried out after two years, in order to verify possible associations between the symptoms. They found that the variable related to low self-esteem mediated the association between SAD and depression differently between genders, finding that, in boys, there was a primary appearance of SAD. However, in girls, this variable partially mediated the primary development of depression.
Therefore, the presence of SAD and depression presents unique characteristics for the individual, and the condition cannot be understood as the simple sum of two different psychiatric diagnoses, once they are related. Some models postulate the existence of unique vulnerabilities for anxiety and depressive disorders. The vulnerability related to negative affectivity, conceptualized as a predisposition to experience negative or even aversive emotions, predisposes the individual to develop intolerance to high uncertainty, that is, the inability to withstand aversive sensations triggered by lack of certainty about current or future events. In addition, intolerance to uncertainty is related to increased anxiety and depressive symptoms (Allan et al., 2018).
Although still inconclusive, the literature highlights that the association of social anxiety and depression worsens the psychosocial impact that these disorders already have independently, aggravating their symptoms and consequences, generating the presence of a more negative prognosis, more debilitated psychological functioning and increased risk of relapse after treatment (Stein et al., 2001; Wong et al., 2014). In addition, it is known that higher levels of depression are predictive of less decline in social anxiety over time, in which the presence of depression comorbidity appears to be a variable that affects the response to cognitive-behavioral therapy (McLaughlin & King, 2015).
Since little is known about the functioning of individuals with SAD and comorbid depressive symptoms, the comprehension of the relationship between social anxiety and depression seems essential (Cecconello, Batistella, Wahl, & Wagner, 2013; Kircanski, Joormann & Gotlib, 2015; McLaughlin & King, 2015; Adams, Balduena, Meng, & Asmudson, 2016; Hamilton et al., 2016). Accordingly, this study aimed to characterize the presence of depression in a sample of individuals diagnosed with SAD, aiming to boost research on the relationship between this condition and depression. Understanding it could result in an improvement in therapeutic techniques and the establishment of more effective treatments. In addition, the study aimed to characterize this sample according to sociodemographic variables.
2. Method
2.1 Design
This was a quantitative cross-sectional study. The levels of depression (minimum, mild, moderate, or severe) present in a sample of 104 people diagnosed with SAD were measured, with 66 of these individuals also presenting depressive symptoms, 12 presenting other anxiety symptoms, 3 substance abuse, and 23 without any comorbidity. Of the participants that presented comorbid Major Depressive Disorder (MDD), 30 had only MDD, while 24 had MDD and other anxiety disorders. From this, a non-experimental design was carried out, in which the sample was characterized based on the sociodemographic (age, sex, educational level, work/occupational activity, and psychiatric medication) and clinical variables (diagnosis of SAD and depressive symptoms) present, as well as the results obtained from the Beck Depression Inventory (BDI-II). In addition, there was a correlation between the levels of the BDI-II and the Social Anxiety Inventory (SPIN), using a total sample of 104 people.
2.2 Participants
The participants in this study were selected from a preexisting database, originating from a randomized clinical trial that aimed to compare the effect of two cognitive-behavioral interventions on social anxiety symptoms (Neufeld, 2017).
For the composition of this database, a disclosure process was necessary (in universities, health centers, and hospitals), in which the opportunity to participate in a study with a free intervention for SAD was disclosed. However, different participants, with different complaints, sought the treatment. Among those that expressed an interest, 158 participants sent their personal data and scheduled initial interviews. Of these, 148 participants underwent the initial assessment, with 44 excluded from the study because they did not have SAD as a primary diagnosis, were under 18 years of age or over 45 years of age. Therefore, the study included 104 people diagnosed with primary SAD, aged between 18 and 45 years.
Additional exclusion criteria were: the presence of psychotic symptoms and marked cognitive deficits, undergoing therapy, and not wanting to interrupt the treatment and the use of psychiatric medication for less than a month.
2.3 Instruments
The clinical sample was characterized based on sociodemographic variables (age, sex, education level, work/occupational activity, and use of psychiatric medication). In addition, the instruments were used to diagnose SAD and evaluate the presence of comorbidities. Depressive, anxiety, and social anxiety symptoms were also assessed.
• Structured Clinical Interview for DSM-IV - Clinician Version (SCID-CV) (First, Spitzer, Gibbon, & Williams, 1997): the interview aims to elaborate a psychiatric diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders - 4th edition (DSM-IV) criteria. The instrument consists of 6 diagnostic modules, with modules A (mood episodes), B (psychotic and associated symptoms), E (alcohol and other substance use disorders), and F (anxiety disorders and other disorders) used in the present study for the diagnosis of comorbidities. The interview was validated in Brazil by Del-Ben et al. (2001), in which good reliability indices were found, obtaining a weighted reliability coefficient for the main diagnosis of .83.
• Social Phobia Inventory - SPIN (Connor et al., 2000): this self-report scale is composed of 17 items, which aim to measure the physical symptoms, fear, and avoidance of social situations present in SAD. The score can vary from 0 to 68 and, according to Connor et al. (2000), has greater sensitivity for the assessment of symptoms of social anxiety using a cutoff point 19. In the original English version, the instrument demonstrated good internal consistency (alpha ranging from .82 to .94) and good test-retest reliabil ity, in which Spearman's correlation coefficient ranged from .78 to .89. It was adapted for the Brazilian context by Osório, Crippa, and Loureiro (2009), who obtained an adequate correlation of the items, varying between .44 and .71, as well as the internal consistency, which varied between .71 and .90.
• Beck Depression Inventory - BDI-II (Beck, Ward, Mendelson, Mock & Erbaugh, 1961): This is a self-report scale, composed of 21 items, which allow a clas sification of the intensity levels of the depression, in which 0 to 11 points represents minimum depression; 12 to 19 mild depression; 20 to 35 moderate depression; and 36 to 63 severe depression. The reliability estimates of the original study vary between .79 and .90, which represents satisfactory internal consistency, both in clinical and non-clinical groups (Beck et al., 1961). The original instrument was adapted to Portuguese by Cunha (2001), the most recent version being adapted by Gorenstein, Pang, Argimon, and Werlang (2011). In this more recent study, the alpha coefficient of the instrument's internal consistency was .93, while the intraclass correlation co efficient was .89, demonstrating its reliability and validity for the Brazilian population.
2.4 Data collection and analysis procedures
Initially, a wide dissemination of the study was carried out between the end of 2014 and the beginning of 2015, started by providing brochures in health units and universities, and the use of local media. The brochure briefly presented the concept of social anxiety with the following explanation "Severe and persistent fear of social situations or performance; Fear of acting in a humiliating or shameful way; Social situations are avoided or endured with intense dread." In addition, it briefly presented Cognitive-Behavioral Therapy. The folder instructed people interested in sending an e-mail to an address created exclusively for the study with some personal data.
Interested participants signed up via e-mail, providing a contact number, and through telephone contact, a face-to-face interview was scheduled in order to complete the questionnaires and conduct the diagnostic interview. Scores above 19 points in the Social Phobia Inventory (SPIN) indicate the presence of symptoms of SAD, and with that, the diagnosis was confirmed through the Structured Clinical Interview for the DSM-IV – Clinician Version (SCID-CV). In view of the study's ethical aspects, participants who did not meet the inclusion criteria were referred to other health services, when necessary.
The collected data were entered into a database and analyzed with the aid of the Statistical Package for the Social Sciences (SPSS) for Windows, version 16.0 (Nie, Hull, & Bent, 2003) software. First, a descriptive analysis of the clinical sample was performed based on demographic data, with the depression levels of the sample, according to the results of the BDI-II, also analyzed. The Kolmogorov-Smirnov normality test was performed on the total sample, in which p >.05 was obtained for all variables, indicating the normal distribution of the sample and the use of parametric statistics. Accordingly, in a second step, through inferential analysis, the t-test for independent samples was used, seeking to verify the significance of the differences in the means obtained from the sociodemographic and clinical data results. In addition, an effect size estimate was calculated using Cohen's d coefficient, where d < 0.19 = insignificant effect; > 0.20 = small effect; > 0.50 = medium effect; >0.80 = large effect; and >1.30 = very large effect. Pearson's r correlation test was also applied, seeking to ascertain the correlation between the intensity of social anxiety and depressive symptoms, which can be classified into correlations of small, medium, or large effect, with the values: 10, 30, and 50, respectively (Cohen, 1992). Finally, those with p < .05 were considered statistically significant.
2.5 Ethical aspects
This research project is part of a Regular Research Grant project that received support from the São Paulo Research Foundation (FAPESP) and was submitted for analysis by the Research Ethics Committee (CEP) of the Faculty of Philosophy, Sciences and Letters at Ribeirão Preto, having been approved on February 21, 2014 (CAAE nº 23789213.2.0000.5407). Therefore, this study had already been approved by the CEP, and data stored in the database can be used to perform analyses.
3. Results
Females constituted 59.6% (n = 62) of the sample, which presented a mean age of 28.77 years (± 5.70), with 57.7% (n = 60) of the individuals performing some paid activity. Almost half of the sample, 43.3% (n = 45) had completed Higher Education, 27.9% (n = 29) reported incomplete Higher Education and 26.9% (n = 28) High School Education.
Furthermore, 65.4% (n = 68) of the subjects did not have a family history of psychiatric disorders, and 68.3% (n = 71) did not use psychiatric medication. In addition, 76.9% (n = 80) of the sample had no previous diagnosis of SAD, while 76.0% presented a comorbidity of another psychiatric disorders (n = 79), mainly Major Depressive Disorder, in 63.5% (n = 66), and Generalized Anxiety Disorder, in 34.6% (n = 36), which appeared as joint comorbidities in 23.1% (n = 24) of the cases. The mean value of the SPIN observed was 44.17 points (± 10.13), and the mean of the BDI-II was 20.20 points (± 9.60), which is indicative of moderate depression. It was found that 44.2% (n = 46) of the sample presented moderate depressive symptoms according to the BDI-II.
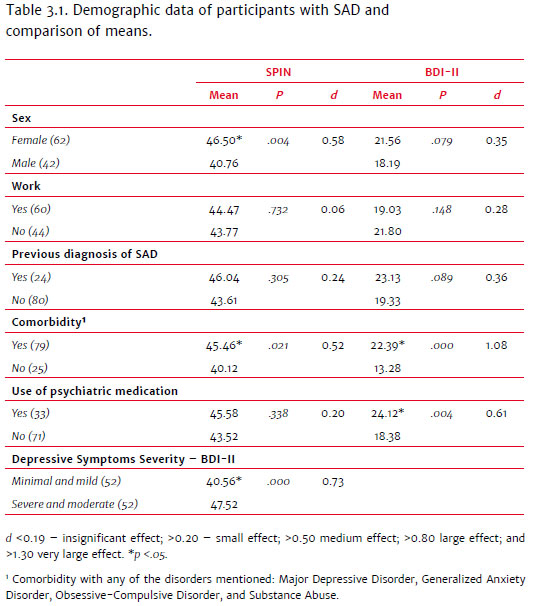
There were no statistically significant results regarding the difference in the means of the SPIN scores between the categories of variables related to formal work [t (102) = 0.534, p = .732, d = 0.06], and having already been previously diagnosed with SAD [t (102) = 1.328, p = .305, d = 0.24]. The same was observed between the BDI-II scores and the formal work [t (102) = -1.610, p = .148, d = 0.28] and previous diagnosis [t (102) = 1.536, p = .089, d = 0.36] variables. The female participants, however, presented higher mean levels of social anxiety symptoms [t (102) = 2.950, p <.01, d = 0.58] than the male participants, with no significant differences in the levels of depressive symptoms [t (102) = 1.775, p = .07, d = 0.35]. In relation to the use of medication and comorbidity, participants that used some psychiatric medication [t (102) = 2.939, p <.01, d = 0.61] and those that had some type of comorbidity [t (102) = 4.503, p <0.01, d = 1.08], presented higher scores for depressive symptoms when compared to those that did not use psychiatric medication or did not have a comorbidity, respectively. Also with regard to the presence of a comorbidity, those individuals that presented some comorbidity had higher SPIN scores, therefore exhibiting higher levels of social anxiety symptoms [t (102) = 2.345, p < .03, d = 0.52].
While those that exhibited depressive symptoms at clinically significant levels (moderate or severe) presented higher levels of social anxiety when compared to the individuals that presented minimal or mild (non-clinically significant) depressive symptoms [t (102) = -3.710, p <.00, d = 0.73].
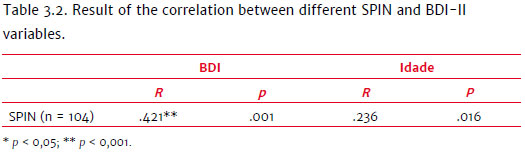
Finally, using data from all the study participants (clinical sample and no clinical symptoms), Pearson's r correlation test demonstrated that higher SPIN scores were positively correlated with higher BDI II scores (r = .42), with this correlation having a medium and significant effect (p < .01). That is, it was found that higher levels of social anxiety equated to higher levels of depressive symptoms, as shown in Table 3.2. In addition, it was found that age was positively related to the SPIN score (r = .23, p = .01), with older ages equated to higher scores for social anxiety symptoms (small effect).
4. Discussion
The present study identified the association between the intensity of social anxiety symptoms and the severity of depressive symptoms in a sample of patients diagnosed with SAD. It characterized the correlation of these symptoms and the presence of psychiatric comorbidities with the intensity of depressive symptoms and social anxiety in these patients. It also identified a higher intensity of the symptoms investigated in females. According to the data obtained, there was a prevalence of females in the sample, which confirms the literature that indicates the greater prevalence of SAD among women in the general population (APA, 2013). Studies also show that SAD is related to unemployment and lower levels of education (APA, 2013; Nardi et al., 2014), however, in this study, a greater number of people that had completed a higher education course were found. It is hypothesized that, as the study was carried out within the university campus and not in health centers, the data on the level of education may have been influenced by the specific characteristics of the sample recruited.
Although no statistical differences were found between working or not concerning levels of social anxiety and depressive symptoms, 42.3% did not perform paid work. Considering that the mean age of the sample was approximately 30 years, it was expected that more people would be included in the labor market. The high number of individuals that did not work observed in the sample of this study is in agreement with the data observed in the literature, which indicates higher levels of unemployment among individuals with SAD (APA, 2013; Nardi et al., 2014). In addition, a high percentage of the absence of a previous diagnosis of SAD was observed, with 76.9% of the participants never having been diagnosed, which may indicate that SAD is still underdiagnosed. The main reasons cited in the literature for the underdiagnosis of SAD refer to the masking of symptoms due to comorbidities, and the difficulty patients have to report their difficulties (Dams et al., 2017). Another relevant fact is that, even when people with SAD seek treatment, only 15% actually start it (Heeren, Mogoaşe, McNally, Schmitz, & Philippot, 2015).
It is important to note that 68.3% of the participants with SAD did not use psychiatric medication. Those individuals who used it had higher levels of depressive symptoms than those who did not use it. This finding is in line with the literature that highlights that individuals with SAD tend to seek treatment when there is some comorbidity associated with the disorder, especially depression (Adams et al., 2016).
It was also found that individuals who presented comorbidities had higher levels of depressive symptoms and higher levels of social anxiety. This information corroborates the literature that emphasizes the high presence of depression in people with SAD (Stein et al., 2001; Wong et al., 2014). In addition, this data reinforces the literature that indicates that the presence of comorbidity, especially depression, increases the severity of the SAD symptoms (social anxiety and social avoidance), implying greater functional, occupational, and quality of life impairments (Adams et al., 2016; Wong et al., 2014). Authors have pointed out that patients with SAD develop depressive conditions due to a demoralization syndrome, in which experiencing intense chronic anxiety and the limitations caused by social inhibition lead to the occurrence of depressive symptoms (Nardi et al., 2014).
The mean BDI-II value was indicative of moderate depression, with a high standard deviation, which suggests diversification of the severity of symptoms of depression within the sample. In addition, more than half of the people had Major Depressive Disorder as a secondary diagnosis, with 44.2% of the people scoring for moderate depression (indicative of clinical value), higher than the 20.0% with moderate symptoms found in the study by Cecconello et al. (2013). This study's results indicate that individuals who exhibited depressive symptoms at clinically significant levels had higher levels of social anxiety, as well as that higher levels of social anxiety were positively correlated with higher levels of depressive symptoms. These data evidence the relationship between depression and social anxiety and corroborate the findings in the literature that indicate that SAD is a predictor of depression (APA, 2013).
It is important to emphasize that the design of the present study does not allow inferences of causality; therefore, we were unable to test these hypotheses and premises, since the longitudinal method was not incorporated into the study design. The presence of depression implies greater psychosocial impairments, increasing the severity of the SAD. This association reinforces the need for more refined diagnoses for the condition of SAD, so that this condition is identified and treated as soon as possible, thus decreasing the likelihood of the symptoms and impairments associated with social anxiety worsening and the development of a more severe depressive disorder (Adams et al., 2016; Stein et al., 2001). Some methodological limitations may also have influenced the study results, such as the sample being from a university and not recruited from mental health care units. Therefore, it is believed that it would be beneficial to carry out other Brazilian studies with this population. Finally, psychotropic drugs' use can also be considered a limitation of the study, affecting all the variables studied.
In the clinical population studied, the intensity of the symptoms of social anxiety and depression was correlated. This evidences the joint occurrence of distinct dysfunctionalities in individuals diagnosed with SAD, with this characterization providing a high potential for worsening of the clinical condition.
References
Adams, G. C., Balduena, L., Meng, X., & Asmudson, G. J. (2016). When social anxiety and depression go together: A population study of comorbidity and associated consequences. Journal of Affective Disorders, 206,48-54. doi: 10.1016/j.jad.2016.07.031 [ Links ]
Allan, N. P., Cooper, D., Oglesby, M. E., Short, N. A., Saulnier, K. G., & Schimidt N. B. (2018) Lower-order anxiety sensitivity and intolerance of uncertainty dimensions operate as specific vulnerabilities for social anxiety and depression within a hierarchical model. Journal of Anxiety Disorders, 53, 91-99. doi: 10.1016/j.janxdis.2017.08.002 [ Links ]
American Psychological Association - APA (2013). Manual diagnóstico e estatístico de transtornos mentais - DSM-5 (5ª ed.). Porto Alegre: Artmed. [ Links ]
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. (1961) An inventory for measuring depression. Archives of General Psychiatry, 4,561-571. [ Links ]
Cecconello, W. W., Batistella, F., Wahl, S. D. Z., & Wagner, M. F. (2013). Avaliação de sintomas depressivos e de fobia social em estudantes de graduação. Aletheia, 42,71-81. [ Links ]
Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1),155-159. doi: 10.1037/ 0033-2909.112.1.155 [ Links ]
Connor, K. M., Davidson, J. R. T., Churchill, L. E., Sherwood, A., Foa, E. B., & Weisler, R. H. (2000). Psychometric properties of the Social Phobia Inventory (SPIN): A new self-rating scale. The British Journal of Psychiatry, 176(4),379-386. doi: 10.1192/ bjp.176.4.379 [ Links ]
Cunha, J. A. (2001). Manual da versão em português das Escalas Beck. São Paulo: Casa do Psicólogo. [ Links ]
Dams, J., König, H., Bleibler, F., Hoyer, J., Wiltink, J., Beutel, M. E., ... Konnopka, A. (2017). Excess costs of social anxiety disorder in Germany. Journal of Affective Disorders, 213,23-29. doi: 10.1016/j.jad.2017.01.041 [ Links ]
Del-Ben, C., Vilela, J. A. A., Crippa, J. A. de S., Hallak, J. E. C., Labate, C. M., & Zuardi, A. W. (2001). Confiabilidade da entrevista clínica estruturada para o DSM-IV: Versão clínica traduzida para o português. Revista Brasileira de Psiquicatria, 23(3),156-159. doi: 10.1590/S1516-44462001000300008 . [ Links ]
First, M. B, Spitzer, R. L, Gibbon, M., Williams, J. B. W. (1997). Structured clinical interview for DSM-IV axis I disorders: clinician version (SCID-CV). Washington: American Psychiatric Press. [ Links ]
Gonçalves, D. A., Mari, J. J., Bower, P., Gask, l., Dowrick, C., Tófoli, L. F., ... Fortes, S. (2014). Brazilian multicentre study of common mental disorders in primary care: Rates and related social and demographic factors. Cadernos de Saúde Pública, 30(3),623-632. doi: 10.1590/0102-311X00158412 [ Links ]
Gorenstein, C., Pang, W. Y., Argimon, I. L., & Werlang, B. S. G. (2011). Inventário Beck de Depressão II. Manual. São Paulo: Casa do Psicólogo. [ Links ]
Hamilton, J. L., Potter, C. M., Olino, T. M., Abramson, L. Y., Heimberg, R. G., & Allo, L. B. (2016). The Temporal Sequence of Social Anxiety and Depressive Symptoms following Interpersonal Stressors during Adolescence. Journal of Abnormal Child Psychology, 44(3),495-509. doi: 10.1007/s10802-015-0049-0 [ Links ]
Heeren, A., Mogoaşe, C., McNally, R. J., Schmitz, A., & Philippot, P. (2015). Does attention bias modification improve attentional control? A double-blind randomized experiment with individuals with social anxiety disorder. Journal of Anxiety Disorders, 29,35-42. doi: 10.1016/j.janxdis.2014.10.007 [ Links ]
Ito, L. M., Roso, M. C., Tiwari, S., Kendall, P. C., & Asbahr, F. R. (2008). Terapia cognitivocomportamental da fobia social. Revista Brasileira de Psiquiatria, 30,96-101. doi: 10.1590/S1516-44462008000600007 [ Links ]
Kircanski, K., Joormann, J., & Gotlib, I. H. (2015). Attention to Emotional Information in Social Anxiety Disorder with and without Co-Occurring Depression. Cognitive Therapy and Research, 39(2),153-161. doi: 10.1007/s10608-014-9643-7 [ Links ]
Kuru, E., Safak, Y., Ozdemir, I., Tulaci, R. G., Ozdel, K., Ozkula, H. G., & Orser, S. (2017). Cognitive Distortions in patients with social anxiety disorder: Comparison of a clinical group and healthy controls. The European Journal of Psychiatry, 32(2),97-104. doi: 10.1016/j.ejpsy.2017.08.004 [ Links ]
McLaughlin, K. A., & King, K. (2015). Developmental trajectories of anxiety and depression in early adolescence. Journal of Abnormal Child Psychology, 43(2),311-323. doi: 10.1007/s10802-014-9898-1 [ Links ]
Muller, J. L., Trentini, C. M., Zanini, A. M., & Lopes, F. M. (2015). Transtorno de Ansiedade Social: Um estudo de caso. Contextos Clínicos, 8(1),67-78. doi: 10.4013/ctc.2015.81.07 [ Links ]
Nardi, A. E., Quevedo, J., & Silva, A. G. (2014). Transtorno de ansiedade social: teoria e clínica. Porto Alegre: Artmed. [ Links ]
Neufeld, C. B. (2017). Efeito de diferentes intervenções cognitivo-comportamentais sobre a ansiedade social: um ensaio clínico randomizado. Universidade de São Paulo, Ribeirão Preto. Retrieved from http://www.teses.usp.br/teses/disponiveis/59/ 59137/tde-05092017-163256/ [ Links ]
Nie, N. H., Hull, C. H., & Bent, D. H. (2003). Statistical Package for the Social Sciences (Versão 12.0) [Software computacional]. São Paulo: SPSS Inc. [ Links ]
Osório, F. L., Crippa, J. A., & Loureiro, S. R. (2009). Cross-cultural validation of the Brazilian Portuguese version of the Social Phobia Inventory (SPIN): Study of the items and internal consistency. Revista Brasileira de Psiquiatria, 31(1),25-29. doi: 10.1590/S1516-44462008005000018 [ Links ]
Stein, M. B., Fuetsch M., Muller N., Höfler M., Lieb R., & Wittchen H. U. (2001). Social anxiety disorder and the risk of depression: a prospective community study of adolescents and young adults. Arch Gen Psychiatry, 58(3),251-256. doi: 10.1001/archpsyc.58.3.251 [ Links ]
Taylor, J. H., Landeros-Weisenberger, A., Coughlin, C., Mulqueen, J., Johnson, J. A., Gabriel, D., ... Bloch, M. H. (2018). Ketamine for Social Anxiety Disorder: A randomized, placebo-controlled crossover trial. Neuropsychopharmacology, 43(2),325-333. doi: 10.1038/npp.2017.194 [ Links ]
Vaananen, J. M., Isomaa, R., Kaltiala-Heino, R., Frojd, S., Helminen, M., & Marttunen, M. (2014). Decrease in self-esteem mediates the association between symptoms of social phobia and depression in middle adolescence in a sex-specific manner: A 2-year follow-up of a prospective population cohort study. BMC Psychiatry, 14(1),1-8. doi: 10.1186/1471-244X-14-79 [ Links ]
Wong, J., Morrison, A. S., Heimberg, R. G., Goldin, P. K., & Gross, J. J. (2014). Implicit associations in social anxiety disorder: The effects of comorbid depression. Journal of anxiety disorders, 28(6),537-546. doi: 10.1016/j.janxdis.2014.05.008 [ Links ]
 Correspondence:
Correspondence:
Bruna Filliettaz Rios
Rua Rui Barbosa, 505, apto 62, Centro
Ribeirão Preto, SP, Brazil. CEP: 14015-120
E-mail: rios.bruna@hotmail.com
Submission: 04/26/2019
Acceptance: 06/23/2020
Support: National Council for Scientific and Technological (CNPq) and São Paulo State Research Support Foundation (Fundação de Amparo à Pesquisa do Estado de São Paulo - Fapesp).
Authors notes
Bruna F. Rios, Faculty of Philosophy, Sciences and Letters of Ribeirão Preto (FFCLRP), Department of Psychology, University of São Paulo (USP); Priscila de C. Palma, Faculty of Philosophy, Sciences and Letters of Ribeirão Preto (FFCLRP), Department of Psychology, University of São Paulo (USP); Kátia Alessandra de S. Caetano, East Behavior Therapy Center; Luciano D. de Mattos, Faculty of Psychology, Catholic University of Pelotas (UCPel); Carmem Beatriz Neufeld, Ribeirão Preto Faculty of Philosophy, Sciences and Letters (FFCLRP), Department of Psychology, University of São Paulo (USP).














