Services on Demand
article
Indicators
Share
Psicologia: teoria e prática
Print version ISSN 1516-3687
Psicol. teor. prat. vol.23 no.1 São Paulo Jan./Apr. 2021
http://dx.doi.org/10.5935/1980-6906/ePTPC1913554
COVID-19
Parents' mental health and children's emotional regulation during the COVID-19 pandemic
Saúde mental parental e regulação emocional infantil durante a pandemia de COVID-19
Salud mental parental y regulación emocional infantil durante la pandemia de COVID-19
Cíntia R. MartinsI,II ; Ana Carolina L. NeivaI
; Ana Carolina L. NeivaI ; Andrea F. BahiaI
; Andrea F. BahiaI ; Clara X. OliveiraI
; Clara X. OliveiraI ; Maria Isabel S. CardosoI
; Maria Isabel S. CardosoI ; José Neander S. AbreuI
; José Neander S. AbreuI
IFederal University of Bahia (UFBA), Salvador, BA, Brazil
IIState University of Feira de Santana (UEFS), Feira de Santana, BA, Brazil
ABSTRACT
The objectives of the study were to investigate parents' mental health before and during the COVID-19 pandemic; to find correlations between parents' mental health and their perceptions of risk, virus exposure, use of preventive measures, COVID-19 knowledge, and social distancing practices; and to analyze correlations between parents' mental health and their perception about children's emotional regulation (ER). Participants were 69 parents of children aged between 5 and 12. The instruments used were ERC, HADS, ABEP, and a questionnaire about COVID-19. Descriptive analyses, the Wilcoxon test, and Spearman's correlation were conducted. The results indicated increased parental anxiety and depression during the pandemic, and a weak negative correlation between parental anxiety and their children's ER. The pandemic acts as a stressor, which impacts the mental health of both parents and children.
Keywords: mental health; emotional regulation; social distancing; quarantine; COVID-19.
RESUMO
Os objetivos do estudo foram investigar a saúde mental parental antes e durante a pandemia da COVID-19; verificar as associações entre saúde mental parental e suas percepções de risco, exposição ao vírus, uso de medidas preventivas, conhecimento sobre a COVID-19 e práticas de distanciamento social; e analisar as relações entre saúde mental parental e suas percepções sobre a Regulação Emocional (RE) infantil. Os participantes desta pesquisa foram 69 pais de crianças entre 5 e 12 anos. Os instrumentos utilizados foram: ERC, HADS, ABEP e questionário sobre a COVID-19. Foram realizadas análises descritivas, Teste de Wilcoxon e correlação de Spearman. Foram encontrados aumento dos níveis de ansiedade e depressão parental durante a pandemia, bem como uma correlação negativa fraca entre ansiedade parental e RE infantil. A pandemia, enquanto agente estressor, tende a impactar a saúde mental de pais e crianças.
Palavras-chave: saúde mental; regulação emocional; distanciamento social; quarentena; COVID-19.
RESUMEN
Los objetivos del estudio fueron investigar la salud mental de los padres antes y durante la COVID-19; comprobar relaciones entre la salud mental de los padres y sus percepciones de riesgo, exposición a virus, uso de medidas preventivas, conocimiento de COVID-19 y prácticas de distanciamiento social y analizar las correlaciones entre la salud mental de los padres y su percepción sobre la Regulación Emocional (RE) de los niños. Los participantes fueron 69 padres de niños de entre 5 y 12 años. Los instrumentos utilizados fueron ERC, HADS, ABEP y un cuestionario sobre COVID-19. Se realizaron análisis descriptivos, la prueba de Wilcoxon y la correlación de Spearman. Los resultados indicaron aumento en la ansiedad y depresión de los padres; correlación negativa débil entre la ansiedad de los padres y la ER de sus hijos. La pandemia actúa como un factor de estrés, que tiene un impacto en la salud mental de padres e hijos.
Palabras-clave: salud mental; regulación emocional; distanciamiento social; cuarentena; COVID-19.
1. Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic has affected over 6 million people worldwide (as of the beginning of June 2020). Brazil is now the third country globally with the most cases and second in the number of deaths. COVID-19 is a highly infectious disease that can cause symptoms ranging from a mild cough to severe respiratory infection, respiratory distress syndrome, acute respiratory failure, and other critical complications (Jiang, Nan, Lv, & Yang, 2020). Studies show that the present pandemic may cause serious mental health issues, increasing the levels of stress, anxiety, and depressive symptoms in the overall population (Brooks et al., 2020; Cluver et al., 2020; Shevlin et al., 2020).
The rapid spread of the virus, fear of infection, uncertainties about how to control the disease and its severity, the unpredictability of the pandemic's duration and its consequences, as well as changes in routines and family relationships, are all considered risk factors for people's mental health (Schmidt, Crepaldi, Bolze, Neiva-Silva, & Demenech, 2020). The pandemic has forced us to deal with fear, which leads to increased anxiety, causes higher stress levels in healthy individuals, and intensifies the symptoms of those with pre-existing psychiatric disorders. Moreover, the quarantine process is a key factor in developing acute stress disorder and post-traumatic stress (PTS) symptoms since its consequences are strong stressors to people's mental health, both during this experience and beyond. These consequences include a heightened fear of infection, frustration and boredom, a feeling of having inadequate supplies and/or information, as well as financial loss and issues of stigma (Brooks et al., 2020). A Brazilian study conducted by Barros et al. (2020) indicates that, throughout the pandemic, approximately 40% of adults feel sad or depressed; 53% feel anxious or nervous; 43.5% have developed sleep problems, and 48% have experienced aggravated sleep problems.
Mental health issues can impact important socio-affective and adaptive functions, such as emotional regulation (ER) (Kerns, Pincus, McLaughlin, & Comer, 2017). ER comprises a set of extrinsic and intrinsic processes responsible for the adequate management of emotional activation (Reis et al., 2016). Emotional lability, a process intrinsically linked to ER, is defined as reactivity or sensitivity to emotion-eliciting events and is usually related to experiencing greater emotional responses to negative and positive emotions (Oattes, Kosmerly, & Rogers, 2018). In children, high emotional lability has been associated with anxiety, attention difficulties, and internalizing or externalizing problems. Additionally, ER and emotional lability are inversely related, indicating that individuals who experience high emotional lability have greater difficulty regulating their emotions (Oattes et al., 2018). Both processes are crucial to children's interpersonal relationships, academic success, and mental health (Morris, Criss, Silk & Houltberg, 2017; Oattes et al., 2018).
Parents' mental health can directly impact a child's development, and their anxiety can contribute to their own children's emotional, behavioral, and physiological dysregulation (Smith, Jones, Charman, Clackson, Mirza, & Wass, 2019). Moreover, parents' mental health is one of the most influential factors in children's emotional development. Family, parent-child, attachment relationships, and parenting styles influence how children experience feelings of safety and their ability to express emotions and effective ER (Morris et al., 2017).
The lack of vaccines and effective evidence-based treatments for the current pandemic has led most countries, including Brazil, to adopt mitigation strategies such as social distancing, quarantine, and geographical lockdown, aiming to reduce transmission and avoid overloading the healthcare system. Accordingly, certain routine activities have been suspended, such as school classes and regular day-to-day work, resulting in more than a billion children worldwide being confined to their homes, without formal school or childcare activities, as well as many parents struggling to work remotely or being unable to work. This context is particularly concerning because it contributes to elevated anxiety and depressive symptoms in parents (Shevlin et al., 2020) and leads to increased vulnerability of children (Cluver et al., 2020).
Certain environmental and psychological variables can influence the pandemic's course and its corresponding impact on mental health. The public's reaction to this situation is particularly relevant in gauging health emergencies' response since it affects risk management and communication strategies. Risk perception is defined as experiencing a feeling about the severity of the risk and how risk is managed. It is an interpretation of the world, influenced by beliefs, experiences, and attitudes, and can produce a sense of outrage and indignation that increases anxiety, stressing its relation to fear and mental health (Cori, Bianchi, Cadum, & Anthonj, 2020).
Voluntary exposure and knowledge levels are among the key factors involved in risk perception and its association with decision-making (Cori et al., 2020). According to the Knowledge, Attitudes and Practices (KAP) theory, an individual's adherence to protective measures is influenced by KAP factors, highlighting the role of knowledge in combatting infectious diseases such as COVID-19. A recent study reported that a 'COVID-19 knowledge score' was significantly associated with a lower likelihood of negative attitudes and preventive practices towards the new disease, which are important factors in influencing government and health institutions' policies to reduce the spread of disease (Zhong et al., 2020).
The level of exposure has been strongly associated with emotional distress. Jiang et al. (2020) reported that participants with greater exposure to COVID-19 experienced more PTS symptoms and used more ER strategies related to psychopathology. This result reinforces previous findings, which suggested that the level and type of psychological impact on individuals during an epidemic depend on the degree of exposure experienced.
Early stressful experiences can promote the emergence of toxic stress in children if they occur without protective factors such as adequate care. This is especially important during the COVID-19 pandemic due to children's increased vulnerability (Cluver et al., 2020) and the epidemic's mental health impact on the general population (Brooks et al., 2020; Shevlin et al., 2020). In this context, parental stress, concern about household chores, fear of losing work, and the impact of the economic crisis can generate an increase in anxiety and irritability, leaving parents with less patience to deal with daily life and their children's needs (Cluver et al., 2020). However, few studies address parents' mental health issues in different contexts. Regarding the coronavirus pandemic in Brazil, little is known about the pandemic's effects on parents' mental health and how this affects children's ER.
This study's initial objective was to investigate parents' mental health and, specifically, their levels of anxiety and depression symptoms, both before and during the COVID-19 pandemic in Brazil. Secondly, we aimed to investigate the association between these mental health indicators and parents' perceptions of risk, virus exposure, use of preventive measures, COVID-19 knowledge, and the practice of social distancing. Lastly, our goal was to analyze relations between parents' mental health and their perception of children's ER. Thus, the study hypotheses were: 1) increased symptoms of parental anxiety and depression during the coronavirus pandemic; 2) a. the higher the scores on the variables related to the pandemic (for example, perceived risk and exposure to the virus), the more the parents will report anxiety and/or depressive symptoms; b. the greater the knowledge about the virus, the less the parents will report symptoms of anxiety and/or depression; and 3) the more symptoms of anxiety and/or depression, the worse the children's emotional regulation.
2. Method
2.1 Study Design
The study followed an empirical, repeated measure, and comparative design, in which all participants answered a questionnaire over the same period, i.e., before the pandemic arrived in Brazil and between 60 and 75 days after social distancing was in place. The COVID-19 pandemic in Brazil began on February 26, 2020.
2. 2 Participants
The participants were 69 parents (18-62 years of age; M=38.97, SD=8.32) of children aged 5 to 12. The majority were female (85.5%) and either in informal work (37.7%) or unemployed (34.8%). The majority of the sample (60.9%) was classified as being from economic class C (having a family income of two minimum monthly wages, approximately USD 600), according to the Brazilian Economic Classification Criteria (created by ABEP - the Brazilian Association of Market Research Companies, 2018), which uses a questionnaire to identify social-economic distribution in Brazil.
2. 3 Instruments
Socio-Demographic Questionnaire: collects data on participants' age, gender, current work situation, education level, as well as their children's age, gender, education, and type of school (private or public).
ABEP Questionnaire: measures participants' socioeconomic level according to the Brazilian Association of Market Research Companies' 2018 classification. The socioeconomic classification is obtained based on a set of questions that determine the number of material goods or services that the participant has at home. It also records the level of education of the head of the household. Each answer receives a certain number of points, and a final score is recorded for each participant, resulting in their socioeconomic level (ABEP, 2018).
Emotion Regulation Checklist (ERC, Shields & Cicchetti, 1997): This questionnaire comprises 24 items that describe children's behavior and its frequency, which is hetero-evaluated on a four-point Likert scale (1 = "Never" to 4 = "Almost Always"). The items are distributed across two subscales: Emotion Regulation (ER) and Emotional Lability/Negativity (L/N). ER is associated with emotional expressions, empathy, and emotional self-awareness, and L/N is associated with inflexibility, rage dysregulation, and mood lability. Data on the psychometric properties and validity of ERC in Brazil is available in Reis et al. (2016).
COVID-19 questionnaire: this 58-item questionnaire was based on studies carried out by McFadden, Malik, Aguolu, Willebrand, & Omer (2020) and Oliver, Barber, Roomp, & Roomp (2020). It includes questions about risk perception and virus exposure risk, using a five-point Likert scale (1= "Totally Disagree" to 5= "Totally Agree") and includes questions about social distancing and COVID-19 knowledge, using dichotomous items (yes or no answers).
Hospital Anxiety and Depression Scale (HADS, Zigmond & Snaith, 1983): consists of 14 multiple-choice items for assessing anxiety and depression. It is divided into two subscales of 7 items, one for anxiety and one for depressive symptoms. The global score in each subscale ranges from 0 to 21. Data on the psychometric properties and validity of HADS in Brazil is available in Botega, Bio, Zomignani, Garcia & Pereira (1995).
2. 4 Procedures
The Research Ethics Committee of the Federal University of Bahia approved this study (No. 3.895.888). It was ongoing during the pandemic, and the goal was to evaluate children's ER. Following the COVID-19 outbreak, other objectives were included to compare parents' mental health symptoms (anxiety and depression) with children's ER, as perceived by the parents, during this period.
The study occurred in two phases: one before the COVID-19 pandemic and one during this health emergency. The first took place in February 2020 at various children's schools and was carried out during family meetings scheduled with school coordinators, parents, and a researcher. This was before the dissemination of COVID-19 in Brazil. Parents who agreed to be part of the study signed the Informed Consent Form before answering the questionnaires. Data collected on this visit included socio-demographic information, socioeconomic status, and an assessment of children's ER before the pandemic.
Due to the necessity for social distancing during the pandemic, the second phase interview and data collection procedure were carried out through telephone/internet in May 2020. This took place between 60 and 75 days after mitigation strategies had been in place. Parents/legal guardians were then asked if they still wanted to continue participating in the study. In this phase, participants were asked about their mental health during and before the COVID-19 pandemic and they answered the COVID-19 and ERC questionnaires. Before the pandemic, parents' mental health was investigated to ascertain if there was a connection between their anxiety and/or depression and their children's ER. Researchers carefully read out the questionnaire items for each participant and asked them to answer according to their perceptions and experiences. The protocol was completed in approximately 45 minutes.
2. 5 Data analysis
Data were analyzed using SPSS Statistics 27.0 for Windows (Statistical Package for Social Sciences). The database preparation stage began with the input process, involving an analysis of missing data and a verification of the sample distribution using Kolmogorov-Smirnov and Shapiro-Wilk Tests. Both tests indicated a non-normal distribution of the sample, leading to the use of a non-parametric test to proceed with the analysis. To achieve the study's goal, descriptive statistics for analysis of frequency, mean, standard deviation, minimum and maximum scoring, and non-parametric statistics, for intragroup comparisons (Wilcoxon test) and correlation (Spearman Correlation/ Spearman ρ (rs)), were carried out. The strength of the relationship among variables was based on coefficient value. The correlation was classified as weak (0.10 to 0.30), moderate (0.40 to 0.60) or strong (0.70 to 0.90) according to Dancey & Reidy (2018).
3. Results
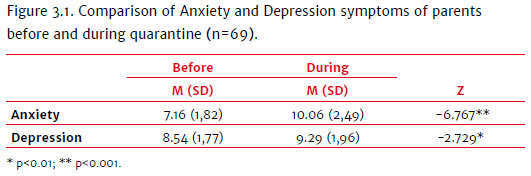
Statistically significant differences (Z= -6.767; p<0.001) were found between parents' anxiety before (M=7.16; DP=1.82) and during (M=10.06; SD=2.49) the pandemic. Another similar result (Z= -2.729; p<0.01) was obtained regarding depressive symptoms scores before (M=8.54; SD=1.77) and during (M=9.29; SD=1.96) the pandemic.
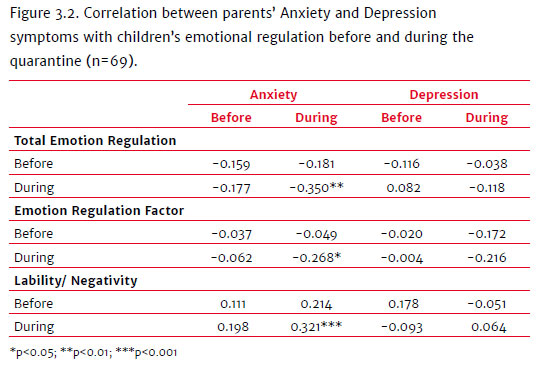
A weak negative correlation between parental anxiety scores during the social distancing period and the total ER (rs (69) = -0.350; p < 0.01) and the ER factor (rs (69) = -0.268; p < 0.05) was presented. Parent's anxiety scores presented a weak positive correlationwith children's lability/negativity factor (rs (69) = 0.321; p < 0.01). No significant correlations were found between parents' depressive symptoms and children's ER.
Regarding the perception of the total risk exposure, a weak positive correlation between parent's anxiety before (rs (69) = 0.330; p < 0.01) and during (rs (69) = 0.379; p < 0.01) the pandemic was found. Some specific items were associated with anxiety before and during quarantine, including: "My health will be severely damaged if I contract coronavirus" [before: (rs (69) = 0.321; p < 0.01) and during: (rs (69) = 0.350; p < 0.01)]; "The coronavirus will cause serious damage in my neighborhood" [before: (rs (69) = 0.258; p < 0.05) and during: (rs (69) = 0.311; p < 0.01)]; "The coronavirus will spread widely in Brazil" [before: (rs (69) = 0.295; p < 0.05) and during: (rs (69) = 0.242; p < 0.05)]. The item "I am more likely to get the coronavirus than others" exhibited correlation only between anxiety levels during the pandemic (rs (69) = 0.334; p < 0.01). There were no correlations between risk exposure perception and parent's depressive symptoms.
Concerning the virus exposure levels, a weak negative correlation was observed before and during quarantine, between depression and the item "Did you have or are you experiencing any symptom of COVID-19?", respectively [(rs (69) = - 0.277; p < 0.05); (rs (69) = - 0.265; p < 0.05)]; and between depression and the item "Do you live with people suspected of carrying the virus (based on some evidence/symptom) COVID-19?"( rs (69) = - 0.260; p < 0.05). No significant correlation was found between anxiety (before or during the COVID-19 pandemic) and the varying levels of exposure to the virus.
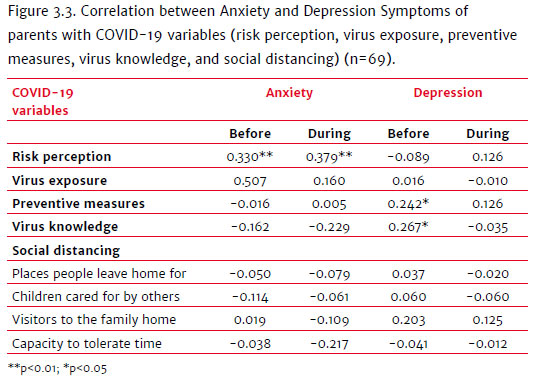
There was a weak negative correlation between anxiety before (rs (69) = - 0.261; p < 0.05) and during the pandemic (rs (69) = - 0.250; p < 0.05) and the item "Stay at home when you're sick", a preventive measure. In addition, depressive symptoms manifested before the pandemic had a weak positive correlation with these measures in general (rs (69) = 0.242; p < 0.05), and with the items "Avoid traveling" (rs (69) = 0.361; p < 0.01); "Use alcohol gel to clean your hands" (rs (69) = 0.274; p < 0.05); and "Consume a balanced diet" (rs (69) = 0.265; p < 0.05); as well as with knowledge of the virus (rs (69) = 0.267; p < 0.05).
4. Discussion
The COVID-19 pandemic is having a detrimental effect on people's mental health around the world. Little is known, however, about its impact on parents' mental health and children's ER. To address this gap, this study's first goal was to compare parents' mental health (levels of anxiety and depressive symptoms) before and during the pandemic. Secondly, we aimed to investigate associations between these mental health indicators and parents' perceptions of risk, level of exposure, use of preventive measures, COVID-19 knowledge, and the practice of social distancing. Another objective of this study was to verify the relationship between parents' mental health and perceptions about their children's ER.
Regarding this study's first objective, results showed that parents' anxiety and depressive symptoms increased during the present pandemic. This result corroborates the hypothesis that these symptoms increased in parents compared to their mental health condition prior to the pandemic. Similar results were found in longitudinal research involving an adult population in the United Kingdom (Shevlin et al., 2020). There are several reasons for this increase, such as 1) the sudden realization that immediate plans have been interrupted; 2) decreased or absence of mobility, as well as separation from social context; 3) concerns about the individual's own health, as well as that of the family, friends, and neighbors; 4) concern about the inability to work or to provide for the family due to illness (Huremović, 2019). The increase could also be associated with unexpected changes to the children's routine, in which they are obliged to stay at home, leading to emotional overload for the parents and a corresponding negative impact on their mental health (Cluver et al., 2020). According to recent studies, children's presence at home during this health emergency is a predictor for the development of anxiety and depressive symptoms (Shevlin et al., 2020). It can reasonably be assumed that uncertainties and new demands in the face of an unforeseen health situation and changing economic and social conditions due to the pandemic impact parents' mental health.
Concerning the pandemic's impacts on mental health, we investigated associations between environmental and psychological variables in parents' mental health outcomes. Certain COVID-19 variables (perceptions of risk, virus exposure, use of preventive measures, COVID-19 knowledge, and the practice of social distancing) were correlated between anxiety and/or depression symptoms, partially corroborating the study's second hypothesis. The data revealed a positive correlation between anxiety and total perception of risk both before and during the pandemic. These results suggest that risk perception may increase anxiety (Cori et al., 2020; Shevlin et al., 2020) even when the pandemic begins to subside. On the other hand, before and during the pandemic, anxiety symptoms did not correlate between the virus exposure variables, preventive measures, COVID-19 knowledge, or social distancing. Symptoms of high levels of anxiety are associated with increased risk perception, as well as the fact that perceived risk increases anxiety. Individuals with higher anxiety symptoms will probably perceive more risk factors whether they occur in times of stress (such as during a pandemic). Those with a more anxious profile habitually tend to perceive more risk regardless of a pandemic. Thus, the trigger is in interpreting events and not in the degree of exposure to the virus, in the time spent social distancing, whether or not preventive measures are used, or in the extent of knowledge about COVID-19. At the time of data collection for this study, the pandemic was still a relatively recent phenomenon in Brazil (approximately two months since its onset). This was when individuals were on alert, demanding cognitive and emotional resources to understand and adapt to the demands of the new scenario (Huremović, 2019).
Regarding mental health conditions, there are possible emotional consequences that are yet to unfold. According to Huremović (2019), an emotional epidemiological path manifests itself during a pandemic in two stages. At first, individuals with increased anxiety and depression symptoms during social distancing appear to be on alert, a phase in which they make efforts to adapt to the environment's new requirements. Later, the individual first perceives a lack of information about the disease (misinformation), then, as access to information becomes more widely available, he/she experiences concerns about the disease and the pandemic's impact on daily life (uncertainty), which contributes to the individual or collective fear/panic (anxiety) and necessitates new coping strategies at an individual and collective level. This concept aligns with previous studies that point to the COVID-19 pandemic as a risk factor for mental health (Schmidt et al., 2020). In China, for example, where the pandemic started, important consequences for the population's mental health have already been reported. Relationships were found between the risk of exposure leading to the development of PTS symptoms and emotional distress caused by the COVID-19 pandemic (Jiang et al., 2020).
Regarding the emotional epidemiological path, depressive symptoms evolve in a slightly different way. The first phase of the pandemic is unlikely to trigger depressive symptoms. However, these symptoms could appear later with the continued presence of the stressor and its consequences. Individuals with a previous depressive diagnosis could present a gradual worsening of their condition during a pandemic. A study conducted by Barros et al. (2020) in Brazil during the pandemic found prevalent symptoms, such as sadness, depression, anxiety, nervousness, sleeping problems in young adults, women, and individuals with a prior diagnosis of depression. This study also shows an increase in depressive symptoms. Given the tendency for negative perceptions of the current environment to remain bleak for the future, individuals with depressive and anxiety symptoms are more likely to present expected behaviors in keeping with the disclosure of negative information. In this study, individuals with higher levels of depression before the pandemic tended to have more knowledge about the virus and use more preventative measures, such as avoiding traveling, using alcohol gel to clean their hands, and having a balanced diet. Accordingly, the cognitive profile of individuals with depressive and anxiety symptoms is a possible explanation for these anticipated behaviors.
Although the deterioration of the symptoms of anxiety and depression presented by parents in this sample did not reach the psychopathological level, it does suggest an increase in irritability and pessimism, behaviors which have a probable association with the fear emotion, leading to avoidance behaviors. In the context of a pandemic, keeping "safe" and attempting to maintain a sense of proportion with these vulnerabilities leads to more preventative measures. Therefore, the "fear" may be a normal and important functional response within this context (Harper, Satchell, Fidos, and Latzman, 2020). This study sample presented more anxiety symptoms than depressive symptoms, indicating a more anxiety-driven cognitive and behavioral profile.
Our final aim was to analyze possible associations between parents' mental health and their perception of their children's ER. Parents' anxiety impacts children's overall regulation (Smith et al., 2019). The study revealed a weak negative relationship between parents' anxiety and the total ER and the ER factor during the pandemic. Mothers with higher negative affection indices tend to present difficulties in maintaining adequate ER strategies, switching between them over a short period (Kerns et al., 2017). Thus, the lack of consistency in the application of assertive strategies by caregivers can impair children's learning processes, preventing them from developing more effective ways of dealing with stressful and abrupt situations, like the pandemic.
An inconsistent parental emotional management can potentially worsen children's emotional lability, as indicated in the results, when a weak positive correlation was found between parental anxiety and children's lability during the pandemic. Oattes et al. (2018) reported similar data when they found that children's emotional lability was positively related to their mothers' general psychological functioning, to her psychological suffering (compulsion, obsession, anxiety, and depression symptoms), and to difficulties in regulating her emotions. However, in that study, no significant correlations between the children's ER and the maternal psychological state were found (Oattes et al., 2018). This finding corroborates results obtained during the period before the pandemic, in which no statistically significant correlations were found between parents' symptoms of anxiety and depression and their children's total and ER factor. The same was true with signs of depression in parents during the pandemic in Brazil.
Correlating parents' mental health and children's ER makes it possible to infer differences between normal and adverse conditions. The pandemic could trigger increased parental anxiety and fewer ER resources. Therefore, it is possible to argue that, as the pandemic unfolds, the higher the levels of parental anxiety, the less effective the ER strategies and the more intense the children's emotional lability. This association was not found in the parents' depressive symptoms, despite their relatively low increase. Our sample had a more anxiety-related profile since higher anxiety levels were observed compared to depressive symptoms, explaining the correlation differences. These results partially corroborate this study's initial assumption, which posited that the higher the parents' level of anxiety and depression, the worse the children's ER. The hypothesis that there is a negative correlation between parents' mental health and children's ER was only corroborated in respect of anxiety.
The relationship between environment and parents' behavioral models through their children's emotional and cognitive development is characterized by a bidirectional influence that could go in a positive or negative direction. As a stressor sets in during the pandemic, there are chances that the parents' mental health (levels of anxiety and depressive symptoms) negatively impact children's behavior. Similarly, a child's challenging ER could trigger a worsening in parents' anxiety and depressive symptoms. It is worth mentioning that impacts of this type of universal global stressor tend to have gradual effects on all behavioral states, especially psychological and social-emotional ones, over the short, medium, and long terms. For this reason, it is essential to adopt measures to preserve, prevent and promote mental health as a matter of priority.
This research contributes to an initial mapping of parents and children's psychological and emotional health during the initial phase of the COVID-19 pandemic in Brazil. The establishment of validated instruments in the Brazilian context should be considered first to assess variables related to crises in public health and secondly for the assessment of mental health and ER, given the limitation on the availability of this information in this study. Another limitation of the metrics applied to this study is that they are based on self-report measures, contributing to social desirability. Additionally, our study's results should not be generalized due to the sample size. Further studies should include a larger sample and variables to explore differences between gender, age group, and ER strategies. Finally, these results should be considered an important indicator for adopting preventive and intervention measures for parents' and children's mental health through psychoeducational and intervention programs both during and following the COVID-19 pandemic.
References
Associação Brasileira de Empresas de Pesquisa - ABEP. (2018). Critério de Classificação Econômica Brasil. Retrieved from http://www.abep.org/ [ Links ]
Barros, M. B. A., Lima, M. G., Malta, D. C., Szwarcwald, C. L., Azevedo, R. C. S., Romero, D., ... Gracie, R. (2020). Relato de tristeza/depressão, nervosismo/ansiedade e problemas de sono na população adulta brasileira durante a pandemia de COVID-19. Epidemiologia e Serviços de Saúde, 29(4),e2020427. doi:10.1590/s1679-49742020000400018 [ Links ]
Botega, N. J., Bio, M. R., Zomignani, M. A., Garcia Jr, C., & Pereira, W. A. (1995). Transtornos do humor em enfermaria de clínica médica e validação de escala de medida (HAD) de ansiedade e depressão. Revista de Saúde Pública, 29(5),355-363. doi:10.1590/S0034-89101995000500004 [ Links ]
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227),912-920. doi:10.1016/S0140-6736(20)30460-8 [ Links ]
Cluver, L., Lachman, J. M., Sherr, L., Wessels, I., Krug, E., Rakotomalala, S., ... McDonald, K. (2020). Parenting in a time of COVID-19. The Lancet, 395(10231), Article e64. doi:10.1016/s0140-6736(20)30736-4 [ Links ]
Cori, L., Bianchi, F., Cadum, E., & Anthonj, C. (2020). Risk Perception and COVID-19. International Journal of Environmental Research and Public Health, 17(9), Article 3114. doi:10.3390/ijerph17093114. [ Links ]
Dancey, C. P., & Reidy, J. (2018). Estatística Sem Matemática para Psicologia (7a ed.). Porto Alegre: Penso. [ Links ]
Harper, C. A., Satchell, L. P., Fido, D., & Latzman, R. D. (2020). Functional Fear Predicts Public Health Compliance in the COVID-19 Pandemic. International Journal of Mental Health and Addiction. Advance online publication. doi:10.1007/s11469-020-00281-5 [ Links ]
Huremović, D. (2019). Psychiatry of Pandemics: A Mental Health Response to Infection Outbreak. New York: Springer. [ Links ]
Jiang, H. J., Nan, J., Lv, Z. Y., & Yang, J. (2020). Psychological impacts of the COVID-19 epidemic on Chinese people: Exposure, post-traumatic stress symptom, and emotion regulation. Asian Pacific Journal of Tropical Medicine, 13(6),252-259. Retrieved from http://www.apjtm.org/article.asp?issn=1995-7645;year=2020;volume=13;issue=6;spage=252;epage=259;aulast=Jiang [ Links ]
Kerns, C. E., Pincus, D. B., McLaughlin, K. A., & Comer, J. S. (2017). Maternal emotion regulation during child distress, child anxiety accommodation, and links between maternal and child anxiety. Journal of Anxiety Disorders, 50,52-59. doi:10.1016/j.janxdis.2017.05.002 [ Links ]
McFadden, S. M., Malik, A. A., Aguolu, O. G., Willebrand, K. S., & Omer, S. B. (2020). Perceptions of the adult US population regarding the novel coronavirus outbreak. PloS one, 15(4), Article e0231808. doi:10.1371/journal.pone.0231808 [ Links ]
Morris, A. S., Criss, M. M., Silk, J. S., & Houltberg, B. J. (2017). The impact of parenting on emotion regulation during childhood and adolescence. Child Development Perspectives, 11(4),233-238. doi:10.1111/cdep.12238 [ Links ]
Oattes, N., Kosmerly, S., & Rogers, M. (2018). Parent emotional well-being and emotion lability in young children. Journal of Child and Family Studies, 27(11),3658-3671. doi:10.1007/s10826-018-1188-z [ Links ]
Oliver, N., Barber, X., Roomp, K., & Roomp, K. (2020). The Covid19 Impact Survey: Assessing the Pulse of the COVID-19 Pandemic in Spain via 24 questions. arXiv preprint arXiv:2004.01014. Retrieved from https://arxiv.org/abs/2004.01014 [ Links ]
Reis, A. H., Oliveira, S. E. S. D., Bandeira, D. R., Andrade, N. C., Abreu, N., & Sperb, T. M. (2016). Emotion regulation checklist (ERC): Estudos preliminares da adaptação e validação para a cultura brasileira. Temas em Psicologia, 24(1),77-96. doi:10.9788/TP2016.1-06 [ Links ]
Schmidt, B., Crepaldi, M. A., Bolze, S. D. A., Neiva Silva, L., & Demenech, L. M. (2020). Saúde mental e intervenções psicológicas diante da pandemia do novo coronavírus (COVID-19). Estudos de Psicologia (Campinas), 37, Article e200063. doi:10.1590/1982-0275202037e200063 [ Links ]
Shevlin, M., McBride, O., Murphy, J., Gibson Miller, J., Hartman, T. K., Levita, L.,... Bentall, R. P. (2020). Anxiety, Depression, Traumatic Stress, and COVID-19 Related Anxiety in the UK General Population During the COVID-19 Pandemic. PsyArXiv. doi:10.31234/osf.io/hb6nq [ Links ]
Shields, A. M., & Cicchetti, D. (1997). Emotion regulation in school age children: The development of a new criterion Q-sort scale. Developmental Psychology, 33,906-916. doi:10.1037//0012-1649.33.6.906 [ Links ]
Smith, C., Jones, E. J., Charman, T., Clackson, K., Mirza, F., & Wass, S. (2019). Anxious parents show higher physiological synchrony with their infants. PsyArXiv. doi:10.31234/osf.io/m2rsg [ Links ]
Zhong, B. L., Luo, W., Li, H. M., Zhang, Q. Q., Liu, X. G., Li, W. T., & Li, Y. (2020). Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. International Journal of Biological Sciences, 16(10),1745-1752. doi:10.7150/ijbs.45221 [ Links ]
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta psychiatrica Scandinavica, 67(6),361-370. doi:10.1111/j.1600-0447.1983.tb09716.x [ Links ]
 Correspondence:
Correspondence:
Neander Abreu
Instituto de Psicologia, Programa de Pós-Graduação em Psicologia Universidade Federal da Bahia (UFBA)
Rua Professor Aristides Novis, 197 -Federação
Salvador, BA, Brazil. CEP 40210-630
E-mail: neandersa@hotmail.com
Submission: 21/06/2020
Acceptance: 30/10/2020
Author's notes
Cíntia R. Martins, Auxiliar Professor, State University of Feira de Santana (UEFS) and Post Graduate Program in Psychology, Federal University of Bahia (UFBA); Ana Carolina L. Neiva, Post Graduate Program in Psychology, Federal University of Bahia (UFBA); Andrea F. Bahia, Post Graduate Program in Psychology, Federal University of Bahia (UFBA); Clara X. Oliveira, Institute of Psychology, Federal University of Bahia (UFBA); Maria Isabel S. Cardoso, Post Graduate Program in Clinical Psychology, Federal University of Bahia (UFBA); José Neander S. Abreu, Associate Professor, Federal University of Bahia (UFBA).














