Serviços Personalizados
Journal
artigo
Indicadores
Compartilhar
Psicologia: teoria e prática
versão impressa ISSN 1516-3687
Psicol. teor. prat. vol.23 no.1 São Paulo jan./abr. 2021
https://doi.org/10.5935/1980-6906/ePTPC1913976
10.5935/1980-6906/ePTPC1913976 COVID-19
Coping strategies in health professionals facing Covid-19: s systematic review
Estratégias de enfrentamento em profissionais de saúde diante do Covid-19: revisão sistemática
Estrategias de afrontamiento en profesionales de la salud ante Covid-19: revisión sistemática
Willian Roger DulliusI ; Silvana Alba ScortegagnaI
; Silvana Alba ScortegagnaI ; Lynn McClearyII
; Lynn McClearyII
IUniversity of Passo Fundo (UPF), Passo Fundo, RS, Brazil
IIBrock University, St. Catharines, ON, Canada
ABSTRACT
Given the importance of developing protective actions to mental health in pandemic contexts, this study aimed to gather evidence about coping mechanisms that health professionals use during the Covid-19 pandemic. This systematic review, developed from international and Brazilian databases between November/2019 and July/2020, identified 3821 potentially relevant articles published in English and Portuguese. Checking the articles' appropriateness to the objective of the review resulted in the selection of 23 articles that were read in full, eight of which were selected for this review. The main coping mechanisms described were psychological support from relatives, colleagues, institutions, and patients; availability of continuing education and Personal Protective Equipment (PPE); spirituality; and time for hobbies. Promoting effective and sustainable coping strategies is vital to enable health professionals to feel capable of facing one of the major contemporary humanitarian challenges - the Covid-19 pandemic.
Keywords: mental health; resilience; coping styles; emotional adjustment; health personnel.
RESUMO
Considerando a importância do desenvolvimento de ações protetivas à saúde mental diante de pandemias, este estudo buscou reunir evidências sobre os mecanismos de enfrentamento empregados por profissionais de saúde em tempos de Covid-19. A revisão sistemática realizada em bases de dados internacionais e brasileiras, entre os meses de novembro/2019 e julho/2020, resultou em 3821 materiais publicados em inglês e português. A verificação da adequação dos materiais ao objetivo proposto derivou na seleção de 23 artigos para a leitura na íntegra, dos quais foram selecionados oito para compor esta revisão. Os principais mecanismos de enfrentamento descritos foram suporte psicológico oriundos de familiares, colegas, instituições, pacientes; disponibilidade de educação continuada e Equipamentos de Proteção Individual (EPIs); espiritualidade; tempo para hobbies. Promover estratégias de enfrentamento eficazes e sustentáveis é vital para que os profissionais da saúde possam se sentir capazes de enfrentar um dos maiores desafios humanitários contemporâneos - a pandemia do Covid-19.
Palavras-chave: saúde mental; resiliência; estilos de enfrentamento; ajustamento emocional; pessoal da saúde.
RESUMEN
Considerando la importancia de desarrollar acciones de protección a la salud mental ante a pandemia, este estudio buscó recopilar evidencia sobre los mecanismos de afrontamiento empleados por los profesionales de la salud en tiempos de Covid-19. La revisión sistemática desarrollada en bases de datos internacionales y brasileñas, entre los meses de noviembre/2019 y julio/2020, resultó en 3821 materiales publicados en inglés y portugués. La verificación de la adecuación de los materiales al objetivo propuesto llevó a la selección de 23 artículos para la lectura completa, de los cuales ocho fueron seleccionados para esta revisión. Los principales mecanismos de afrontamiento descritos fueron soporte psicológico, oriundos de familiares, colegas, instituciones, pacientes; disponibilidad de educación continuada y Equipo de Protección Personal (EPP); espiritualidad; tiempo para hobbies. Promover estrategias de afrontamiento eficaces y sustentables es vital para que los profesionales de salud puedan sentirse capaces de enfrentar un de los mayores retos humanitarios contemporáneos - la pandemia de Covid-19.
Palabras clave: salud mental; resiliencia; estilos de enfrentamiento; adaptación emocional; personal de salud.
1. Introduction
At the end of 2019, the novel coronavirus (SARS-CoV-2), often referred to as Covid-19, the disease it causes, began its spread in the Chinese city of Wuhan. It quickly spread, becoming a pandemic. By the first week of August 2020, there were 18.614,177 cases of Covid-19 in the region of the Americas. Of these, 702,642 people died, and 5.089,581 people recovered from the infection (OPAS, 2020).
This adverse scenario has a significant impact on daily life and can lead to several mental health problems, both in the general population and in specific situations of greater vulnerability (Albott et al., 2020; Barbosa, Gomes, Souza, & Gomes, 2020; Huang et al., 2020; Ornell, Schuch, Sordi, & Kessler, 2020; Pimentel & Silva, 2020). A literature review by Barbosa et al. (2020) describes that hysteria and paranoia in the general public are part of the context of pandemics. Other authors observe a wider range of mental health problems, varying according to the kinds of activities people are engaged in, highlighting a greater disposition to psychic complications among health professionals (Aksoy & Koçak, 2020; Cipolotti, Chan, Murphy, Harskamp, & Foley, 2020; Dong et al., 2020; Liu et al., 2020; Ornell et al., 2020; Pimentel & Silva, 2020; Schechter et al., 2020).
Specifically, those at the "front-line," such as nursing professionals, provide emergency, acute, and end-of-life care to Covid-19 patients over extended periods and may present greater proneness to mental health problems. During the Severe Acute Respiratory Syndrome (SARS) epidemic, anxiety and fear were common in front-line workers (Chong et al., 2020). As learned from Ebola outbreaks and epidemics, an absence of mental health and psychosocial support systems increases the risks of psychological distress and progression toward psychopathology in medical staff (Zhang, Wu, Zhao, & Zhang, 2020). A higher prevalence of psychological symptoms was found among medical health workers during Covid-19 compared to previous pandemics and epidemics (Yang et al., 2020).
The psychosocial and economic crisis caused by the Covid-19 pandemic generates extensive negative consequences associated with the need for mental health care. Therefore, studies that address psychological support needs and interventions for health professionals are necessary both in the emerging period of the pandemic and in the post-pandemic period (Pimentel & Silva, 2020).
Among the negative consequences of the pandemic on the mental health of health professionals who provide daily care for people affected by Covid-19, high levels of anxiety and stress stand out. These professionals lack the knowledge and protection to work with Covid-19 patients (Huang et al., 2020) and experience other stressors related to their work. These include uncertainty about resources, skills, and risks in the work environment and significant psychic suffering associated with the life-threatening nature of Covid-19 for their patients and the number of deaths they witness. This tends to lead to high levels of anxiety, fear, stress, and burnout syndrome in the short and long term (Albott et al., 2020; Chong et al., 2004; Maunder et al., 2006), and demand coping resources and protective support and care measures.
There is limited empirical evidence on mental health interventions for front-line professionals in direct interaction with the infected patients. The literature emphasizes the need for studies aimed at providing psychological support to nursing professionals (Aksoy & Koçak, 2020; Cipolotti et al., 2020; Schechter et al., 2020) and the importance of coping strategies, i.e., behavioral patterns that reduce threats to physical and mental integrity. Coping strategies operate at the intrapsychic, interpersonal, and intergroup levels (Breakwell, 2015). Coping strategies such as accepting the need for social distancing, for example, can contribute to mitigating risks. Maintaining interpersonal connections online can reduce feelings of loneliness and participating in group activities can provide feelings of belonging. Thus, by supporting coping, there is potential to enhance individual and collective positive actions in response to the threats of Covid-19.
Given the importance of supporting mental health in the face of pandemics, the study inquiry was "What coping mechanisms do health professionals who provide care for patients with Covid-19 use?". To answer the question, this systematic review aims to summarize and describe existing research about the coping mechanisms that health professionals use in the face of the Covid-19 pandemic.
2. Method
The systematic review involves a detailed and comprehensive plan with a priori research strategies, aiming to minimize biases through the identification, evaluation, and synthesis of studies relevant to the subject being studied (Uman, 2011). In this perspective, this systematic review was conducted according to the recommendation proposed by the PRISMA guideline - Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Moher, Liberati, Tetzlaff, & Altman, 2009).
2. 1 Criteria for material inclusion in the review
The material selected for this study consisted of empirical articles, with qualitative, quantitative, and/or mixed designs, about health professionals' coping mechanism(s) to face the Covid-19 pandemic. The eligibility criteria were: articles published in 2019 or 2020, in peer-reviewed, indexed journals, available in full text, in Portuguese or English, and classified as open access in their respective scientific journals. The outcome evaluated was indicators related to health professionals' use of coping strategies in the context of Covid-19. The exclusion criteria were duplicate publications in the databases, comments publications, editorials, scientific literature, review articles, grey literature, and articles that referred to the pandemic's effects in health professionals but did not mention coping mechanisms.
The articles' search covered an eight-month period from November/2019 to July/2020, thus including publications from the pandemic's beginning. The databases searched for this review were PsycINFO, PMC-NCBI, SciELO (Scientific Electronic Library online), MEDLINE, PubMEd, and LITCOVID-NCBI. These databases are relevant to the review question as they consider the content and coverage of multidisciplinary studies, contemplating Brazilian and international publications, methodological approaches, and the targets of this study.
2. 2 Documentary data collection procedures
Initially, searches were performed in the Medical Subject Heading of the US National Library of Medicine (MeSH) and the Health Sciences Descriptors (DeCS) to identify the descriptors defined together with the Boolean operators. A Boolean strategy was employed, using the descriptors "pandemic" OR "COVID-19" AND "coping" OR "resilience" AND "health professional" with the respective corresponding terms in Portuguese. The choice of the keywords aimed to discover the largest number of articles involving indicators of coping.
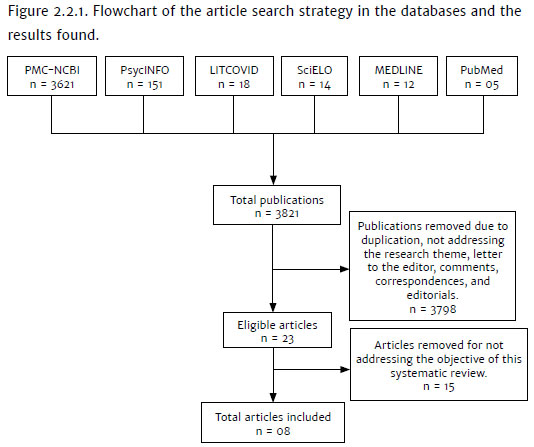
The search identified 3821possible publications in PMC-NCBI (n = 3621), PsycINFO (n = 151), LITCOVID-NCBI (n = 18), SciELO (n = 14), MEDLINE (n = 12), and PubMed (n = 05). For the remaining publications (n = 3821), the title and abstract were read, and the inclusion criteria were applied. Next, 3798 publications were excluded because they did not comply with the inclusion criteria in this review, such as letters to the editor, opinion articles, reviews, duplicated articles, publications that did not address the topic of interest or involved another type of participants, had variables unrelated to coping mechanisms of health professionals, and the language of publication.
The selected articles (n = 23) were, then, read in full. Of these, 15 articles were excluded, considering the inclusion and exclusion criteria, for the following reason: describing psychologic effects on health professionals instead of coping mechanisms. Accordingly, eight articles were elected to compose the qualitative analysis, which aimed to summarize and describe existing research about the coping mechanisms that health professionals use in the face of the Covid-19 pandemic. Figure 2.2.1 shows the article search strategy in this systematic review and the results achieved.
3. Results
Figure 3.1 displays the following information about the studies in this systematic review: authors, year and country of research, objective, study design, population, sample characteristics, instruments, statistical analysis, and coping mechanisms identified in the results.
Figure 3.1 shows that the study design is predominantly cross-sectional. Some used validated psychological measures, but most of them used a questionnaire created by the authors. There is a preponderance of international studies, with no Brazilian research. Sample sizes ranged from 9 to 4,618. The field's average length of professional experience varied considerably within the nine studies, between 6.5 and 19 years of experience.
The studies show different coping mechanisms developed by health professionals at the front line in the care of individuals suspected of or diagnosed with Covid-19. Figure 3.2 illustrates three types of coping mechanisms described in the studies: personal practices, social support, and actions to reduce the personal risk of Covid-19 infection.

Figure 3.2 shows that the most reported way of coping was through informal and formal social support - by talking to colleagues, friends, family, and others or talking with a psychologist. The next most reported strategy was continuing education and learning more about Covid-19, and infection control was also reported across studies. Regulating exposure to news about Covid-19 was reported in several studies. Other personal coping practices included engaging in a hobby or pastime, physical activity, other healthy lifestyle practices, religious and spiritual practices, regulating workload, trying not to think about Covid-19, and positive thinking. Minimizing the risk of Covid-19 infection at work and outside of work was also reported across studies.
4. Discussion
The literature review on the coping mechanisms that the health professionals use in response to the Covid-19 pandemic shows that the Brazilian literature presents an important lack of publications on the theme, as the Covid-19 pandemic began later, as well as research about the impact of the pandemic in the health professionals' daily activities. There is a predominance of international publications, which are, nevertheless, scarce. The largest number of publications come from the Asian continent, as the beginning of the pandemic occurred on that continent, as well as the development of research and intervention measures for health professionals.
Concerning the health professionals' experience, the results point to an extensive work period, ranging from 6.5 to 19 years of service. This is interesting when observing that women with more than ten years of experience, concomitant chronic illnesses and a history of mental disorders were more susceptible to stress, depression, and anxiety during the outbreak (Zhu et al., 2020). Thus, the experience factor does not seem to guarantee better resources for coping with Covid-19, and the mental health conditions of health professionals seem to require constant assistance and evaluation.
Some studies highlight that nursing professionals are at risk of greater vulnerability to mental health and experience greater difficulty using coping strategies (Aksoy & Koçak, 2020; Cipolotti et al., 2020; Dong et al., 2020; Schechter et al., 2020). Reasons for this include long hours of work, lack of protective equipment and shortage of masks, high risks of contracting an infection, having physical fatigue, and suffering separation from families, as well as problems in interpersonal interaction because they are potential vectors of virus transmission. The lack of positive coping measures was related to major mental health impairments (Dong et al., 2020). These results corroborate previous studies showing that, after the SARS outbreak in 2003, about 77% of the health professionals who were in contact with infected patients during the outbreak had mental distress symptoms, ranging from anxiety to depression, and somatic symptoms (Chong et al., 2004). One year after the epidemic, they had a higher prevalence of burnout, distress, and Post-Traumatic Stress Disorder (Maunder et al., 2006).
The health professionals' stress tends to disturb their emotions and weaken their coping behavior. For example, being quarantined is significantly and positively associated with avoidance behavior (Chong et al., 2004). Impaired interpersonal communication by wearing an N95 mask and protective clothing can induce a bad mood (Dong et al., 2020). Combining the aforementioned emotional losses makes us think of the need for support to promote favorable response strategies to reduce situational stress and decrease its lasting effects.
In this perspective, the availability of multiple sources of support, coming from different areas, such as health institutions (hospitals and basic health units), in offering psychological and mental health care through a virtual route (Aksoy & Koçak, 2020; Liu et al., 2020; Sun et al., 2020), family support, friends, patients, and society (Cipolotti et al., 2020; Liu et al., 2020), the willingness of family and friends to talk about the experiences at work (Cai et al., 2020; Dong et al., 2020; Liu et al., 2020) and contact with co-workers and people from the institution (Austin & Gregory, 2020; Liu et al., 2020) were widely highlighted in the studies listed in this article. The use of these strategies shows that maintaining interpersonal connections can provide feelings of belonging, even if sometimes one cannot reach a consensus of ideas. Sharing experiences and anxieties can bring positive experiences and strengthen the sense of identity, confirming literature data (Jaspal & Nerlich, 2020).
Other important elements are greater access to the use of PPE and the flexibility of the work shift, reduction of the daily workload, continuing education (Austin & Gregory, 2020; Cipolotti et al., 2020; Liu et al., 2020), compliance with the safety measures described in the protocols (Dong et al., 2020) and religious beliefs (Munawar & Choudhry, 2020). For some professionals, being informed with news about Covid-19 was mentioned as coping resources (Cipolotti et al., 2020; Dong et al., 2020), but, for others, focusing on work and avoiding news about the pandemic was a more effective help measure (Liu et al., 2020).
It is observed that the way people react to potentially threatening situations reveals specific characteristics of their cognitive, behavioral skills and are also influenced by their beliefs and cultural aspects. Some people can absorb and relate with new information without any critical judgment; others can add meaning and value to the information and read the reality critically. Considering the identity process theory (Breakwell, 2015; Jaspal & Breakwell, 2014), it can be assumed that, when identity processes are unable to operate according to the coherent principles of identity itself, the accumulation of adverse information about the threats of Covid-19 can challenge the individual's sense of continuity and operate to intensify the traumatic psychological effect of the pandemic.
In view of the diversity of emotional reactions and coping strategies adopted, this study highlights the importance of offering personalized psychological support services, adapted according to each group of professionals. This validates authors who recommend such services, in addition to the application of generic approaches, to reduce stress, and to achieve positive and protective responses by health professionals against Covid-19 (Shanafelt, Ripp, & Trockel, 2020).
Some experiences of the primary author of this study as a nursing professional working at the front line in the care for individuals suspected or diagnosed with Covid-19 attest to the relevance of the findings. The author experienced several of the stressors identified in the research. Limited availability of PPE and the uncertainties about how to proceed due to the different changes in the care flow and care for the users of the public health system (SUS) resulted in fear and anxiety because of the insecurity about transmitting the disease to relatives, particularly the elderly in the risk group who shared the same housing, showed to be potential factors for the emergence of instability and emotional frailty. In combination, isolation at home, away from the family, as a protective measure of the loved ones, due to the possibility of contamination with Covid-19 during professional practice, was considered an important potentiating factor of adverse emotional effects.
Given the harmful psychological effects resulting from the necessary adaptations as a nursing professional in the line of care for infected patients, at least three coping mechanisms employed, which corroborate this systematic review's findings, should be highlighted. First of all, the daily reflection on the capacity to act in times of crisis, helping to minimize anxiety and strengthen the sense of independence and security; second, to provide care considering that all individuals with signs and symptoms of a respiratory problem are suspected cases of Covid-19 and, for this reason, the protective care of the nursing staff in patient care, needs to be doubled; and third, the dialogue with colleagues about other topics than work; these contributed as coping mechanisms to alleviate the stress and anxiety that develop in the environment of professional practice. The case report ratifies preview studies that recommend the provision of mental health interventions by institutions to minimize the impacts of the pandemic and contribute to the successful development of coping mechanisms in health professionals (Aksoy & Koçak, 2020; Austin & Gregory, 2020; Cipolotti et al., 2020; Schechter et al., 2020).
To better exemplify the theme addressed in this study, it is worth mentioning that many hospital institutions in Brazil do not provide professionals to offer mental health care to the professionals who work directly in the care for Covid-19 patients, a factor that could contribute to support the emotional frailties in situations of collective psychological trauma, as is the case of this pandemic. The importance of mental health care availability in work institutions has been widely highlighted in other countries' studies (Aksoy & Koçak, 2020; Liu et al., 2020; Sun et al., 2020).
As for organizations' support strategies, these should be adopted through active communication, using clear protocols for the PPE, professional action guidelines, and prevention measures to prevent the virus's spread. It is important to recognize the normality of negative reactions to the pandemic and emphasize the use of preventive interventions, combat stigmas, and promote collective efficacy.
Institutions need to make efforts to provide resources in interventions aimed at minimization, promotion, and prevention in the mental health of health professionals who act on the front line against Covid-19 (Aksoy & Koçak, 2020; Ornell et al., 2020; Schechter et al., 2020), but should also provide resources to the other professionals, as they are all facing atypical situations that promote negative effects on the physical and mental integrity. Among the mental health actions the governmental entities and individuals develop, the following are cited: the creation of protocols and training for the professionals, the standardization of medication and resources to be offered to the infected patients, the availability of appropriate infrastructure to enable the health professionals to act, making available educative materials and support networks and, finally, the data collection to analyze the situation presented in each region, so that protective measures can be created and developed in favor of physical and mental health, following the statistics that were presented (Ornell et al., 2020).
Some limitations are evidenced in the studies, such as the fact that the professionals answering the questionnaires were mainly nurses and physicians, given the gap in the literature about the other health professionals' perspectives on coping mechanisms. It is comprehensible that most health professionals working on the front line are nurses and physicians, but the group of health professionals contains other areas that cannot be excluded, as they are impacted too (Austin & Gregory, 2020; Cai et al., 2020; Liu et al., 2020). Some limitations related to statistical analysis are verified in the study by Austin & Gregory (2020), as neither a pilot version nor a test of the adopted framework was elaborated. Also, in the study by Munawar & Choudhry (2020), an in-depth analysis of the analysis strategy was not found.
Related to the participants' gender, the prevalence of the female gender was higher in the studies. The coping mechanisms' data could differ if the sample's gender representation were more homogeneous (Aksoy & Koçak, 2020; Cai et al., 2020; Cipolotti et al., 2020; Dong et al., 2020; Liu et al., 2020). Also, the data collection period was short and covered the middle of the pandemic, so these aspects change the impact on health professionals; the coping mechanisms could change among the different periods of the pandemic, evidencing different effects (Cai et al., 2020; Cipolotti et al., 2020). Shechter et al. (2020) developed a strategy to follow participants during three months, providing a positive reflection about the pandemic's evaluation during this period.
Some studies recommend mental health interventions for health professionals (Aksoy & Koçak, 2020; Austin & Gregory, 2020; Cai et al., 2020; Cipolotti et al., 2020; Munawar & Choudhry, 2020; Schechter et al., 2020). These interventions are applied in the instrument developed by Albott et al. (2020) and Ornell et al. (2020), both promoting mental health care and individual support, focusing on three main areas: self-care, self-efficacy, and social connection. For the authors, health professionals exposed to higher stress experiences should be encouraged to find mental health support. Also, in situations related to isolation and isolation related to social distancing, these professionals should find engagement strategies with remote social connection, promote collective effectiveness, witness and share personal stories, share positive emotions of altruism, preserve good humor, and cultivate feelings of gratitude.
In view of this systematic review's findings, the need to offer interventions aimed at the problems presented by health professionals at the front line of care for Covid-19 patients, and provide help for the use of coping mechanisms, services need to be developed for this population. Group psychotherapy, based on the cognitive-behavioral theory (CBT), focal therapies, with structured sessions and behavioral techniques such as relaxation, diaphragmatic breathing, body scan, cognitive psychoeducation techniques, and role-plays and self-monitoring can be a good option for care and treatment. The use of the fundamentals and techniques of contextual therapies of mindfulness, acceptance and commitment, and emotional regulation techniques can be fundamental to this audience's emotional balance process.
This study's findings point to the health professionals' psychic suffering in the face of threatening situations and great uncertainties experienced in the pandemic. Therefore, and in an attempt to strengthen the emotional resources of coping, the creation and implementation of transdisciplinary care devices are also suggested, aimed at the promotion, prevention, and strengthening of mental health. The services managed by psychologists, psychiatrists, and related areas could include collective online conversation groups and address the effects of the pandemic in the context of emergency emotional problems, especially related to work, and increase the different coping mechanisms that can be employed.
Finally, some limitations of this study need to be mentioned. Important variables to be taken into account are: the selection of articles restricted to those classified as open access, the restriction to the language of publication of the articles, the period of the research, and the fact that the grey literature and articles describing psychological effects in health professionals related to the pandemic were not considered. In this context, it is observed that many studies sought to investigate issues related to health professionals in the period prior to the increased care demand for users diagnosed with Covid-19. In addition, the different phases in the evolution of the pandemic and their respective outcomes in terms of recovered cases and deaths can affect the professionals' socio-emotional experiences and aggravate or mitigate their effects according to the work, hospital, or primary health care environments. In view of these limitations, the increase of publications focusing on the coping mechanisms of health professionals should be encouraged, which may lead to a greater understanding of the means of support employed and contribute to the development of strategies to prevent and intervene in the negative consequences of the Covid-19 pandemic in mental health.
References
*Aksoy, Y., & Koçak, V. (2020). Psychological effects of nurses and midwives due to COVID-19 outbreak: The case of Turkey. Archives of Psychiatric Nursing, 34(5),427-433. doi:10.1016/j.apnu.2020.07.011 [ Links ]
Albott, C. S., Wozniak, J. R., McGlinch, B. P., Wall, M. H., Gold, B. S., & Vinogradov, S. (2020). Battle Buddies: Rapid deployment of a psychological resilience intervention for health care workers during the COVID-19 pandemic. International Anesthesia Research Society, 131(1),43-54. doi:10.1213/ANE.0000000000004912 [ Links ]
*Austin, Z., & Gregory, P. (2020). Resilience in the time of pandemic: The experience of community pharmacists during COVID-19. Research in Social and Administrative Pharmacy. doi:10.1016/j.sapharm.2020.05.027 [ Links ]
Barbosa, D. J., Gomes, M. P., Souza, F. B. A., & Gomes, A. M. T. (2020). Fatores de estresse nos profissionais de enfermagem no combate à pandemia da COVID-19: Síntese de evidências. Comunicação em Ciências da Saúde, 31(1),31-47. [ Links ]
Breakwell, G. M. (2015). Coping with threatened identities. London: Psychology Press. doi:10.4324/9781315733913 [ Links ]
*Cai, H., Tu, B., Ma, J., Chen, L., Fu, L., Jiang, Y., & Zhuang, Q. (2020). Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID19) in Hubei, China. Medical Science Monitor, 26,e924171, 1-16. doi:10.12659/MSM.924171 [ Links ]
*Cipolotti, L., Chan, E., Murphy, P., Harskamp, N., & Foley, J. A. (2020). Factors contributing to the distress, concerns, and needs of UK Neuroscience health care workers during the COVID-19 pandemic. Psychology and Psychotherapy: Theory, Research and Practice, e12298. doi:10.1111/papt.12298 [ Links ]
Chong, M. Y., Wang, W. C., Hsieh, W. C., Lee, C. Y., Chiu, N. M., Yeh, W.C., ... Chen, C. L. (2004). Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. The British Journal of Psychiatry, 185(2),127-33. doi:10.1192/bjp.185.2.127 [ Links ]
*Dong, Z., Ma, J., Hao, Y., Shen, X., Liu, F., Gao, Y., & Zhang, L. (2020). The social psychological impact of the COVID-19 pandemic on medical staff in China: A cross-sectional study. European Psychiatry, 63(1),e65,1-8. doi:10.1192/j.eurpsy.2020.59 [ Links ]
Huang, L., Wang, Y., Liu, J., Ye, P., Cheng, B., Xu, H., ... Ning, G. (2020). Factors associated with resilience among medical staff in radiology departments during the outbreak of 2019 novel coronavirus disease (COVID-19): A cross-sectional study. Medical Science Monitor, 26,e925669. doi:10.12659/MSM.925669 [ Links ]
Jaspal, R., & Breakwell, G. M. (2014). Identity process theory: Identity, social action and social change. Cambridge, UK: Cambridge University Press. doi:10.1017/CBO9781139136983 [ Links ]
Jaspal, R., & Nerlich, B. (2020). Social representations, identity threat, and coping amid COVID-19. Psychological Trauma, 12(S1),S249-S251. doi:10.1037/tra0000773 [ Links ]
*Liu, Q., Luo, D., Haase, J., Guo, Q., Wang, X., Liu, S., ... Yang, B. (2020). The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. The Lancet Global Health, 8(6),e790-e798. doi:10.1016/S2214-109X(20) 30204-7 [ Links ]
Maunder, R. G., Lancee, W. J., Balderson, K. E., Bennett, J. P., Borgundvaag, B., Evans, S., ... Wasylenki, D. A. (2006). Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infectious Diseases Journal, 12(12),1924-1932. doi:10.3201/eid1212.060584 [ Links ]
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7),e1000097. doi:10.1371/journal.pmed.1000097 [ Links ]
*Munawar, K., & Choudhry, F. (2020). Exploring stress coping strategies of frontline emergency health workers dealing covid-19 in Pakistan: A qualitative inquiry. American Journal of Infection Control, 00,1-7. doi:10.1016/j.ajic.2020.06.214 [ Links ]
Organização Pan-Americana da Saúde - OPAS (2020, Agosto 7). Folha informativa - COVID-19 (doença causada pelo novo coronavírus). Retrieved from https://www.paho.org/bra/index.php?option=com_content&view=article&id=6101:covid19&Itemid=875 [ Links ]
Ornell, F., Schuch, J. B., Sordi, A. O., & Kessler, F. H. P. (2020). Pandemia de medo e covid-19: Impacto na saúde e possíveis estratégias. Revista Debates in Psychiatry, Advance online publication. Retrieved from http://www.ufrgs.br/ufrgs/noticias/arquivos/pandemia-de-medo-e-covid-19-impacto-na-saude-mental-e-possiveis-estrategias [ Links ]
Pimentel, A. S. G., & Silva, M. N. R. M. O. (2020). Saúde psíquica em tempos de corona vírus. Research, Society and Development, 9(7),1-35. doi:10.33448/rsd-v9i7.4548 [ Links ]
Shanafelt, T., Ripp, J., & Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA, 323(21),2133-2134. doi:10.1001/jama.2020.5893 [ Links ]
*Shechter, A., Diaz, F., Moise, N., Anstey, D., Ye, S., Agarwal, S., ... Abdalla, M. (2020). Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. General Hospital Psychiatry, 66,1-8. doi:10.1016/j.genhosppsych.2020.06.007 [ Links ]
Sun, D., Yang, D., Li, Y., Zhou, J., Wang, W., Wang, Q., ... Zhang, Q. (2020). Psychological impact of 2019 novel coronavirus (2019-nCoV) outbreak in health workers in China. Epidemiology and Infection, 148,e96,1-6. doi:10.1017/S0950268820001090 [ Links ]
Uman, L. S. (2011). Information management for the busy practitioner: Systematic reviews and meta-analyses. Journal of the American Academy of Child and Adolescent Psychiatry, 20(1),57-59. doi:10.1016/j.revmed.2014.05.011 [ Links ]
Yang, Y., Li, W., Zhang, Q., Zhang, L., Cheung, T., & Xiang, Y. (2020). Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry, 7(4),e19. doi:10.1016/S2215-0366(20)30079-1 [ Links ]
Zhang, J., Wu, W., Zhao, X., Zhang, W. (2020). Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: A model of West China Hospital. Precision Clinical Medicine, 3(1),3-8. doi:10.1093/pcmedi/pbaa006 [ Links ]
Zhu, Z., Xu, S., Wang, H., Liu, Z., Wu, J., Li, G., ... Wang, W. (2020). COVID-19 in Wuhan: Immediate psychological impact on 5062 health workers. EClinical Medicine, 24,100443. doi:10.1016/j.eclinm.2020.100443 [ Links ]
 Correspondence:
Correspondence:
Willian Roger Dullius
Graduate Program in Human Aging-University of Passo Fundo (RS), Campus I
Bairro São José, BR 285, Km 171
Passo Fundo, RS, Brazil. Cx. Postal 611. CEP 99052-900
E-mail: rogerdullius@gmail.com
Submission: 29/08/2020
Acceptance: 30/10/2020
Funding: This work was supported by the Higher Education Personnel (Capes) and the Rio Grande do Sul State Research Support Foundation (FAPERGS).
Authors' notes:
Willian Roger Dullius, Department of Faculty of Physical Education and Physiotherapy (FEFF), University of Passo Fundo (UPF); Silvana Alba Scortegagna, Department of Faculty of Physical Education and Physiotherapy (FEFF), University of Passo Fundo (UPF); Lynn McCleary, Department of Nursing, Brock University.














