Services on Demand
article
Indicators
Share
Psicologia: teoria e prática
Print version ISSN 1516-3687
Psicol. teor. prat. vol.23 no.1 São Paulo Jan./Apr. 2021
http://dx.doi.org/10.5935/1980-6906/ePTPC1913976
10.5935/1980-6906/ePTPC1913976 COVID-19
Mental health in health professionals facing Covid-19: a systematic review
Saúde mental em profissionais de saúde no enfrentamento ao covid-19: revisão sistemática
Salud mental en profesionales de la salud frente a covid-19: revisión sistemática
Silvana Alba ScortegagnaI ; Eduardo dos S. de LimaI
; Eduardo dos S. de LimaI ; Sonia Regina PasianII
; Sonia Regina PasianII ; Deise M. do AmparoIII
; Deise M. do AmparoIII
IUniversity of Passo Fundo (UPF), Passo Fundo, RS, Brazil
IIUniversity of São Paulo (USP), São Paulo, SP, Brazil
IIIUniversity of Brasília (UnB), Brasília, DF, Brazil
ABSTRACT
The objective was to systemically review the scientific literature findings on mental health indicators of health professionals engaged in coping with the Covid-19 pandemic. The review followed the PRISMA guideline recommendations, including articles published on this theme, excluding comments, editorials, and literature review articles. Twenty-eight articles were investigated concerning their country of origin, participants, methods used, mental health indicators (symptoms described), and main conclusions. There was great variation in the methodological strategies used in the studies (number of participants and instruments). However, the findings consistently appointed relevant alterations in recurring symptoms of anxiety, depression, and sleep changes in health professionals at the frontline in the fight against the pandemic. Interventions through online conversation groups conducted by mental health professionals could help combat the pandemic's effects concerning the development of emotional problems.
Keywords: health professionals; Covid-19; mental health; anxiety disorders; depression.
RESUMO
Este estudo objetivou revisar, de forma sistemática, achados da literatura científica relativos a indicadores de saúde mental em profissionais de saúde no enfrentamento à pandemia de Covid-19. A revisão seguiu as recomendações do PRISMA, incluindo artigos publicados nesta temática, excluindo-se comentários, editoriais e artigos de revisão da literatura. Foram examinados 28 artigos científicos considerando seu país de origem, participantes, métodos utilizados, indicadores relativos à saúde mental (sintomas descritos) e principais conclusões. Houve grande variabilidade nas estratégias metodológicas utilizadas nos estudos (número de participantes e instrumentos), porém os achados foram consistentes em apontar alterações relevantes em termos de sintomas de ansiedade, depressão e alterações no sono como recorrentes em profissionais de saúde atuantes no combate à pandemia. Intervenções por meio de grupos de conversação, realizados on-line, conduzidos por profissionais da área da saúde mental, poderiam auxiliar a combater os efeitos da pandemia referentes ao desenvolvimento de problemas emocionais.
Palavras-chave: profissionais de saúde; Covid-19; saúde mental; distúrbio da ansiedade; depressão.
RESUMEN
Este estudio de revisión sistemática de la literatura científica se centró en los indicadores de salud mental en los profesionales de la salud para hacer frente a la pandemia de Covid-19. Siguió una guía PRISMA, incluyendo artículos publicados sobre este tema, excluidos comentarios, editoriales y artículos de revisión de literatura. Se examinaron 28 artículos según: país de origen, participantes, métodos, indicadores de salud mental (síntomas descritos) y principales conclusiones. Hubo gran variabilidad en las estrategias metodológicas utilizadas en los estudios (número de participantes, instrumentos), pero los hallazgos apuntaron cambios relevantes en términos de síntomas de ansiedad, depresión y cambios en el sueño como recurrentes en los profesionales de la salud que trabajan en la lucha contra la pandemia. Las intervenciones a través de grupos de conversación online, realizadas por profesionales de la salud mental, podrían ayudar a combatir los efectos de la pandemia respecto al desarrollo de problemas emocionales.
Palabras-clave: profesionales de la salud; Covid-19; salud mental; trastornos de la ansiedad; depresión.
1. Introduction
On March 31, 2020, the World Health Organization (WHO) defined the coronavirus outbreak as a pandemic. The associated disease was called Covid-19 (Coronavirus disease 2019) and is spreading rapidly, while scientists are still trying to understand its mechanisms of action (Organização Mundial da Saúde, 2020).
As a way of coping with Covid-19, one of the most accepted strategies is social distancing to avoid contact with infected people. People are encouraged to stay at home, use masks, tighten hygiene habits, and keep physical distance from other people. Nevertheless, the health professionals working to combat the new virus need to be in daily contact with infected people as part of the treatment offered to patients (Lai et al., 2020; Liu et al., 2020; Zhang et al., 2020), constituting a vulnerable group to Covid-19, due to the high risk of infection they are exposed to. Acting against highly transmissible diseases can increase feelings of fear, anxiety, despair, and stress. Health professionals in contact with mucous membranes or aerosols produced by infected patients, as happens in procedures such as tracheal intubation, tracheostomy, noninvasive ventilation, and manual ventilation, present an even greater risk of contamination (Civantos et al., 2020; Fawaz & Samaha, 2020; D. Sun et al., 2020; Zerbini, Ebigbo, Reicherts, Kunz, & Messman, 2020).
To protect their families and friends, it is common for these professionals to physically distance themselves from these people (Fawaz & Samaha, 2020; Lai et al., 2020), decreasing their affective-social support network. This distancing, combined with the stress and exhaustion they are subject to due to the increased daily workload (Civantos et al., 2020; Sethi, Sethi, Ali, & Aamir, 2020; Sun et al., 2020) and redoubled care for equipment and procedures (Lai et al., 2020; Xing, Sun, Xu, Geng, & Li, 2020), can weaken their psychic balance and mental health.
Signs of destabilization in mental health can emerge from behavioral changes and impairments in physical health conditions (Chong et al., 2004; Kröger, 2020; Xing et al., 2020). The effects of a high-stress burden can continue acting beyond one year after the critical period of a pandemic, as shown by McAlonan et al. (2007). Therefore, the effects of post-traumatic stress for health professionals at a greater risk of infection with Covid-19 can be persistent.
Collaborative, multidisciplinary, and large-scale actions need to be taken in order to understand the psychological effects of the Covid-19 pandemic. Assessing health professionals makes it possible to prevent symptoms of anxiety and depression (common in extraordinary circumstances, such as a pandemic) from persisting and generating harmful behaviors such as self-mutilation or suicide (Holmes et al., 2020).
This perspective requires a systematic study of the theme and compilation of the knowledge produced thus far to develop care strategies for health professionals so they can perform their work under appropriate conditions. To be able to offer more appropriate actions and interventions, knowledge is needed on the weaknesses related to the mental health of this professional group. Based on these premises, this study aimed to conduct a systematic review of the scientific literature to identify indicators related to health professionals' mental health conditions in coping with the current pandemic of Covid-19.
2. Method
This systematic review of the scientific literature was conducted according to the PRISMA guideline recommendations - Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Moher, Liberati, Tetzlaff, & Altman, 2009). As eligibility criteria for this literature review, we included published articles that conducted mental health assessments of health professionals coping with Covid-19. Comments, editorials, and scientific literature review articles were excluded. The outcome evaluated was indicators related to mental health conditions in health professionals in coping with Covid-19.
A bibliometric study was carried out, between May and June, to analyze the scientific production on mental health in health professionals after the onset of the pandemic, in which articles were included whose abstracts were available in English. This choice aimed to grant visibility to the studies representative of this pandemic period and which addressed the theme of mental health in health professionals, disseminated in English, given its international reach.
Considering that the pandemic officially began in early 2020 (World Health Organization, 2020), all articles located were published in the same year. The search for the studies was carried out in the Pubmed, PsycINFO, PePSIC, and Scielo databases. The choice of these databases was due to their relevance and scope concerning the proposed research theme. The keywords used were "saúde mental e Covid-19," "saúde mental e Covid19," "saúde mental e Covid 19," and their correlates in English "mental health and Covid-19," "mental health and Covid19," and "mental health and Covid19", respectively. The keywords choice was intended to cover as many articles as possible involving indicators related to mental health. We opted for the specific use of the terminology "mental health" to focus on these indicators.
The authors of this study independently evaluated the titles and abstracts of the studies identified through the search strategy. Initially, the duplicated titles were excluded. Then, comments, editorials, letters to the editor, and scientific literature review articles were excluded. The final stage excluded articles that addressed other participants' mental health and that did not include health professionals. All studies that did not provide sufficient information in their respective abstracts to ground their compliance with the inclusion and exclusion criteria used were evaluated in full and selected according to the eligibility criteria adopted here. The authors individually extracted the data regarding the methodological characteristics of the studies, their data regarding mental health indicators, and their conclusions, reaching a systematic compilation of these analyses by consensus among independent examiners.
3. Results
The results of the scientific literature search in the Brazilian and international databases totaled 1,158 publications. Figure 3.1 displays the flowchart of the search strategy used in this work.
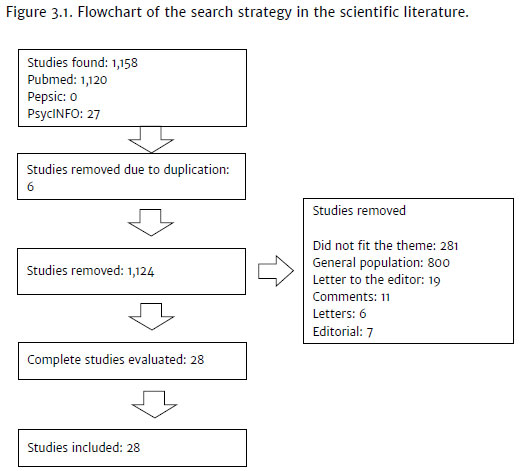
Six duplicated studies were identified and they were removed. In total, 1,124 articles did not comply with the criteria for inclusion in this review because they involved another type of participants and variables not related to health professionals' mental health. Thus, 28 scientific articles remained for a detailed examination.
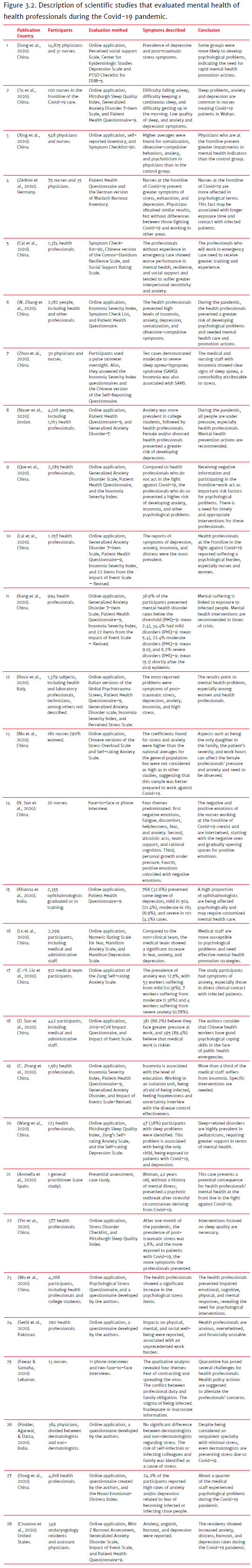
The reading and analysis of the 28 selected articles enabled the verification and systematization of their various technical characteristics, involving methodological and content aspects. The variables related to the country of origin of the studies, their participants, methods used in scientific research, indicators related to mental health (symptoms described), and the main conclusions of each of these studies were highlighted. Figure 3.2 presents the studies analyzed that evaluated the mental health of health professionals coping with Covid-19.
Of the 28 articles selected, most of them originated in China (n = 19; 67.85%), followed by India (n = 2; 7.14%) and Germany, Italy, Jordan, Spain, Pakistan, Lebanon, and the United States (n = 1; 3.57%). No Brazilian study was found. In 22 articles (78.57%), the data collection process through the application of instruments was carried out entirely by digital means (computer or smartphone) and, in two of them (7.14%), the data collection was mixed, including a face-to-face interview with the participants. In one of the studies (3.57%), the assessment happened face-to-face, being a case study, and, in two articles (7.14%), no description was found on how the data were collected in the study.
The samples evaluated in the selected studies (Anmella et al., 2020) ranged from one person to 14,866 participants (Song et al., 2020). Four studies evaluated only physicians (Anmella et al., 2020; Civantos et al., 2020; Khanna et al., 2020; Podder et al., 2020); three studies evaluated only nurses (Mo et al., 2020; N. Sun et al., 2020; Tu et al., 2020); 10 studies evaluated physicians and nurses (Fawaz & Samaha, 2020; Kang et al., 2020; Lai et al., 2020; Que et al., 2020; Song et al., 2020; S. Wang et al., 2020; Xing et al., 2020; Zerbini et al., 2020; W. Zhang et al., 2020; Zhuo et al., 2020); one study evaluated physicians and dentists (Sethi et al., 2020); six studies evaluated physicians, nurses and administrative staff (Dong et al., 2020; Liu et al., 2020; Lu et al., 2020; Rossi et al., 2020; D. Sun et al., 2020; Yin et al., 2020); one study evaluated physicians, nurses, technicians, pharmacists, logistics, and social media staff (Cai et al., 2020); one study evaluated physicians, nurses, pharmacists, residents, and other unspecified professionals (Naser et al., 2020); and two studies did not specify the health professionals evaluated (W. Wu et al., 2020; C. Zhang et al., 2020).
Among the professionals surveyed, physicians participated in more studies (n = 23, 82.14%), followed by nurses (n = 16, 69.56%). However, in the samples, the population of nurses could be found in numbers up to 7 times greater than that of physicians (physicians n = 183, nurses n = 811, Kang et al., 2020).
The most frequently used instruments in the studies were the Generalized Anxiety Disorder 7-Item Scale (n = 8; 28.57%) and the Patient Health Questionnaire-9 (n = 8; 28.57%), followed by the Insomnia Severity Index (n = 7; 25.00%), and an Inventory or Questionnaire developed by the researchers (n = 7; 25.00%). Thus, the researchers focused on indicators related to anxiety, depression, and insomnia, which are more frequent among psychic symptoms in different population groups.
Among the mental health indicators for the participants in this set of 28 published studies, the information could be systemized by the most frequently mentioned disorders. These data are displayed in Figure 3.3.

Anxiety was the most described symptom in the articles (n = 13; 46.42%), followed by depressive symptoms (n = 11; 39.28%). Subsequently, problems with sleep (N = 8; 28.57%), stress (n = 5; 17.85%), exhaustion (n = 4; 14.28%), and fear (n = 4; 14.28%) were the symptoms that most appeared among health professionals who are working to combat Covid-19. In this scientific literature survey, we aimed to picture the mental health indicators according to their technical classifications, even if they were emerging from various data collection processes, given the methodological variability among the different studies examined.
4. Discussion
When analyzing the scientific production on health professionals' mental health conditions in coping with Covid-19, we can observe a series of negative effects and symptoms of illness associated with these professionals' daily work. Their professional activity conditions, full of additional risks during the pandemic, have promoted reports of exhaustion and intense personal wear (Civantos et al., 2020; Sethi et al., 2020; Sun et al., 2020), with recurring symptoms of anxiety, depression, and sleep-related problems.
As verified, anxiety was the most frequent symptom described in the studies (Civantos et al., 2020; Dong et al., 2020; Lai et al., 2020; Liu, Zhang, Wong, Hyun, & Hahm, 2020; Lu et al., 2020; Mo et al., 2020; Naser et al., 2020; Que et al., 2020; Rossi et al., 2020; Sun et al., 2020; Tu et al., 2020; Xing et al., 2020; Zhang et al., 2020). The frequent exposure to infected patients and the high rate of transmission of the Covid-19 may be one reason associated with the health professionals' threatening psychic experiences. For example, in the quarantine environment, one cannot observe where the virus is, even knowing that it is around (Ruiz & Gibson, 2020), which ends up enhancing the need for self-care and increased anxiety.
Unlike care for other diseases, no thorough understanding of the SARS-CoV-2 virus exists yet. Thus, the exposure of professionals to infected patients is fraught with uncertainty about the technical safety of clinical procedures and whether the measures being taken are fit to avoid infection risk (Liu et al., 2020; Zhang et al., 2020).
Not rarely, anxiety symptoms can turn into obsessive-compulsive behaviors, such as attempts to control the threats experienced (Xing et al., 2020; Zhang et al., 2020). The feeling of anxiety and fear, mixed with the complex procedure of the constant change of clothing and protective equipment, can induce professionals to adopt obsessive-compulsive behaviors to reduce the risk of infection.
In this sense, the lack of specific interventions aimed at supporting the mental health of professionals active in coping with Covid-19 and the increase in the reported anxiety levels can lead to the somatization of the anxieties faced (Xing et al., 2020; Zhang et al., 2020). The studies repeatedly argue about the professionals' complaints regarding the difficulty to cope with their burden of feelings and the overload imposed by the working hours. These experiences, associated with the lack of mental health promotion interventions, can favor that their bodies end up being the escape route for their anguish.
The second most cited change in the articles identified in this scientific literature review was depression symptoms (Civantos et al., 2020; Dong et al., 2020; Khanna et al., 2020; Lai et al., 2020; Lu et al., 2020; Naser et al., 2020; Rossi et al., 2020; Song et al., 2020; Tu et al., 2020; Zerbini et al., 2020; Zhang et al., 2020). The social distancing imposed by the quarantine, combined with the high risk of contagion of professionals at the frontline against Covid-19, induces a decrease in contacts with their own families and friends, variables that would naturally function as social support for stressful moments in life. This reality can weaken these professionals' mental health in the sense of emerging depression symptoms related to the various losses experienced in this process (Dong et al., 2020; Lai et al., 2020). The fear of infecting people from one's own family has been mentioned in different studies, functioning as a variable that strongly mobilizes one's emotions.
Also, daily, these professionals need to cope with ethical and professional dilemmas in choosing who will receive the care and treatment equipment available in the care centers, given the frequent lack of respirators and other inputs (Borges, Barnes, Farnsworth, Bahraini, & Brenner, 2020; Khanna et al., 2020). The number of daily deaths, the increase in the number of infected people, and the uncertainties about the treatment and cure of Covid-19 can further weaken these professionals, who need to cope with life and death issues every day.
The results found in this current scientific literature review are similar to those found in Pappa et al. (2020) when evaluating 13 articles on professionals' mental health. Their findings indicated the prevalence of anxiety and depression as the main symptoms found in health professionals, highlighting the magnitude of the traumatic effect of working in coping with Covid-19.
The combination of anxiety and depression can lead to a fairly common third outcome: sleep problems (C. Zhang et al., 2020; Lai et al., 2020; Que et al., 2020; Rossi et al., 2020; Tu et al., 2020; Wang et al., 2020; W. R. Zhang et al., 2020; Zhuo et al., 2020). In addition, the increase in alcohol consumption, the lack or decrease in healthy habits, and constant access to negative information about the advancement of the disease also contribute to increased insomnia (Que et al., 2020).
Indirectly, the lack of properly qualified professionals and in physical and age conditions compatible with the health agencies' recommendations to act in the fight against Covid-19 also favors sleep-related disorders (Tu et al., 2020). Without enough professionals, health professionals (especially nurses) need to increase their working hours and undergo more time in contact with infected patients. Thus, they tend towards a greater concern with their health, leading to greater anxiety. Furthermore, Tu et al. (2020) also mentioned the stress of the work environment as a reason for nurses to sleep less and worse. Conversely, poor sleep quality also triggers increased anxiety and depression, which ends up generating a symptomatic cycle.
Finally, it is important to mention the most extreme symptom described in health professionals, which is psychoticism. Stress, anxiety, and sleep problems, when in excess, can lead to increased symptoms of psychoticism, even in people without a history of psychiatric problems (Anmella et al., 2020; Xing et al., 2020). These empirical findings serve as an alert for professional practice, and special attention is required due to the personal characteristics and limits within health work.
Physicians and nurses were the most researched health professionals. This fact is justified by these professionals' role in the front line of care for patients with Covid-19. Although many studies have included both in their samples, the results do not allow a clear comparison of mental health conditions. Even though they divide the workspace, the activities performed by physicians and nurses, as well as the way they encountered patients, are different and may lead to distinct emotional responses. Thus, personalized psychological approaches can be an important component in dealing with mental health in complex conditions, coping mechanisms, and prevention (Holmes et al., 2020). This data could guide interventions focused on groups of professionals that present greater vulnerability and psychic suffering.
Fear of contamination, death, lack of vaccines, and proper protective materials draw attention and show how unprepared the world is to face a pandemic. Health professionals have no help in dealing with their psychological issues, or the means are still insufficient. Current public policy models to address pandemics are still flawed, overburden professionals, and cause psychological suffering, as observed in the reactions presented in the articles.
In this sense, Arbix (2020) recommends that public policies increasingly focus on science and technology investment, as has been done in more developed countries, such as the United States, Germany, and the United Kingdom. Making up for the lack of basic materials so that they are available to health professionals in appropriate quantity and quality, as well as equipment of high complexity, can be a first step towards reducing the symptoms of anxiety and depression in these professionals. Also, international cooperation efforts in spreading knowledge about the new virus, vaccine development, and other treatments can contribute positively to maintaining mental health.
Research aimed at the mental health of health professionals may offer subsidies so that the knowledge acquired be applied at similar times in the future. Offering better working conditions and more effective psychological support, with the use of new technologies and personalized to the demands, can be an important mechanism to intervene in and prevent the psychological effects that are being observed (Holmes et al., 2020).
Therefore, the findings of this systematic scientific literature review show the urgency of creating and implementing strategies aimed at promoting and strengthening mental health for this group of health professionals who showed to be vulnerable to the traumatic effects of the pandemic. Specific interventions to address the weaknesses found could help these professionals maintain better mental health conditions and prevent the aggravation of possible socio-emotional instabilities. Specifically, interventions for the benefit of mental health through online conversation groups, conducted by properly trained professionals in the psychic field (psychologists and psychiatrists) and related areas, in a transdisciplinary perspective, could contain part of the effects of the pandemic concerning the emergence of emotional disorders. They would function as social and institutional support resources for professionals working in the health area during this pandemic, given the clear existing evidence of the psychic trauma they all experience, which can generate great individual and collective psychic vulnerability.
Another no less important point to consider, taking into account the results of this study and the need to assess health professionals' mental health, is the development of psychological tests that can be applied through remote (online) resources. Studies on the development of these psychological assessment tools (creation) and their applicability (indicators of validity, potentialities, and limits) in these conditions, through digital means, are scarce, with still incipient results.
This systematic review of the scientific literature identified indicators related to mental health conditions in health professionals working in the current pandemic, but also brought inquiries that can contribute to the development of science regarding the care of these professionals, as well as conditions for their proper performance in health. It should be kept in mind, however, that this study comes with limitations. When the research was conducted, time was an important variable, as many articles evaluated the professionals in periods of higher incidence of Covid-19. Searches covering other periods may find different results. The evolution curve of the cases and their respective recovery or death outcomes certainly affect these professionals' socio-emotional experiences and may change with the course of the pandemic, its aggravation, or resurgence in the different studied scenarios. Given this universal instability because of the current pandemic, new scientific investigations focused on health professionals' mental health conditions become relevant and necessary, especially over time, in order to verify the effects of Covid-19 longitudinally.
References
*Anmella, G., Fico, G., Roca, A., Gómez-Ramiro, M., Vázquez, M., Murru, A., ... Vieta, E. (2020). Unravelling potential severe psychiatric repercussions on healthcare professionals during the COVID-19 crisis. Journal of Affective Disorders, 273(1),422-424. doi:10.1016/j.jad.2020.05.061 [ Links ]
Arbix, G. (2020). Ciência e Tecnologia em um mundo de ponta-cabeça. Estudos Avançados, 34(99),65-76. doi:10.1590/s0103-4014.2020.3499.005 [ Links ]
Borges, L. M., Barnes, S. M., Farnsworth, J. K., Bahraini, N. H., & Brenner, L. A. (2020). A commentary on moral injury among health care providers during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1),S138-S140. doi:10.1037/tra0000698 [ Links ]
*Cai, W., Lian, B., Song, X., Hou, T., Deng, G., & Li, H. (2020). A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian Journal of Psychiatry, 51(April),1-4. doi:10.1016/j.ajp.2020.102111 [ Links ]
Chong, M.-Y., Wang, W.-C., Hsieh, W.-C., Lee, C.-Y., Chiu, N.-M., Yeh, W.-C., ... Chen, C.-L. (2004). Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. British Journal of Psychiatry, 185(2),127-133. doi:10.1192/bjp.185.2.127 [ Links ]
*Civantos, A. M., Byrnes, Y., Chang, C., Prasad, A., Chorath, K., Poonia, S. K., ... Rajasekaran, K. (2020). Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: National study. Head and Neck, 42(7). doi:10.1002/hed.26292 [ Links ]
*Dong, Z.-Q., Ma, J., Hao, Y.-N., Shen, X.-L., Liu, F., Gao, Y., & Zhang, L. (2020). The social psychological impact of the COVID-19 pandemic on medical staff in China: A cross-sectional study. European Psychiatry, 63(1),e65,1-8. doi:10.1192/j.eurpsy.2020.59 [ Links ]
*Fawaz, M., & Samaha, A. (2020). The psychosocial effects of being quarantined following exposure to COVID-19: A qualitative study of Lebanese health care workers. International Journal of Social Psychiatry, 66(6)560-565. doi:10.1177/ 0020764020932202 [ Links ]
Holmes, E. A., O'Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., ... Bullmore, E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6),547-560. doi:10.1016/S2215-0366(20)30168-1 [ Links ]
*Kang, L., Ma, S., Chen, M., Yang, J., Wang, Y., Li, R., ... Liu, Z. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain, Behavior, and Immunity, 87(July),11-17. doi:10.1016/j.bbi.2020.03.028 [ Links ]
*Khanna, R. C., Honavar, S. G., Metla, A. L., Bhattacharya, A., & Maulik, P. K. (2020). Psychological impact of COVID-19 on ophthalmologists-in-training and practising ophthalmologists in India. Indian Journal of Ophthalmology, 68(6),994-998. doi:10.4103/ijo.IJO_1458_20 [ Links ]
Kröger, C. (2020). Shattered Social Identity and Moral Injuries: Work-Related Conditions in Health Care Professionals During the COVID-19 Pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1),S156-S158. doi:10.1037/tra0000715 [ Links ]
*Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., ... Hu, S. (2020). Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open, 3(3),1-12. doi:10.1001/jamanetworkopen. 2020.3976 [ Links ]
*Liu, C.-Y., Yang, Y., Zhang, X.-M., Xu, X., Dou, Q.-L., Zhang, W.-W., & Cheng, A. S. K. (2020). The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiology and Infection, 148,1-7. doi:10.1017/S0950268820001107 [ Links ]
Liu, C. H., Zhang, E., Wong, G. T. F., Hyun, S., & Hahm, H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research, 290(April),1-7. doi:10.1016/j.psychres.2020.113172 [ Links ]
*Lu, W., Wang, H., Lin, Y., & Li, L. (2020). Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Research, 288(April),1-5. doi:10.1016/j.psychres.2020.112936 [ Links ]
McAlonan, G. M., Lee, A. M., Cheung, V., Cheung, C., Tsang, K. W. T., Sham, P. C., ... Wong, J. G. W. S. (2007). Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Canadian Journal of Psychiatry, 52(4),241-247. doi:10.1177/070674370705200406 [ Links ]
*Mo, Y., Deng, L., Zhang, L., Lang, Q., Liao, C., Wang, N., ... Huang, H. (2020). Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. Journal of Nursing Management, 28(5)1002-1009. doi:10.1111/jonm.13014 [ Links ]
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine, 6(7),e1000097. doi:10.1371/journal.pmed.1000097 [ Links ]
*Naser, A. Y., Dahmash, E. Z., Al-Rousan, R., Alwafi, H., Alrawashdeh, H. M., Ghoul, I., ... Alyami, H. S. (2020). Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: A cross-sectional study. Brain and Behavior, 10(8),June, 1-13. doi:10.1002/brb3.1730 [ Links ]
Organização Mundial da Saúde. (2020). Folha informativa - COVID-19. Brasil: OMS. Retrieved from https://www.paho.org/bra/index.php?option=com_content&view=article&id=6101:covid19&Itemid=875 [ Links ]
Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G., Papoutsi, E., & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity, 88(August),901-907. doi:10.1016/j.bbi.2020.05.026 [ Links ]
*Podder, I., Agarwal, K., & Datta, S. (2020). Comparative analysis of perceived stress in dermatologists and other physicians during home-quarantine and COVID-19 pandemic with exploration of possible risk factors: A web-based cross-sectional study from Eastern India. Dermatologic Therapy, 33(4),May, 1-7. doi:10.1111/dth.13788 [ Links ]
*Que, J., Shi, L., Deng, J., Liu, J., Zhang, L., Wu, S., ... Lu, L. (2020). Psychological impact of the COVID-19 pandemic on healthcare workers: A cross-sectional study in China. General Psychiatry, 33(3),e100259. doi:10.1136/gpsych-2020-100259 [ Links ]
*Rossi, R., Socci, V., Pacitti, F., Di Lorenzo, G., Di Marco, A., Siracusano, A., & Rossi, A. (2020). Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Network Open, 3(5),e2010185. doi:10.1001/jamanetworkopen.2020.10185 [ Links ]
Ruiz, M. A., & Gibson, C.-A. M. (2020). Emotional impact of the COVID-19 pandemic on U.S. health care workers: A gathering storm. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S153-S155 doi:10.1037/tra0000851 [ Links ]
*Sethi, B. A., Sethi, A., Ali, S., & Aamir, H. S. (2020). Impact of Coronavirus disease (COVID-19) pandemic on health professionals. Pakistan Journal of Medical Sciences, 36(COVID19-S4). doi:10.12669/pjms.36.covid19-s4.2779 [ Links ]
*Song, X., Fu, W., Liu, X., Luo, Z., Wang, R., Zhou, N., ... Lv, C. (2020). Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain, Behavior, and Immunity, 88(June), 60-65. doi:10.1016/j.bbi.2020.06.002 [ Links ]
*Sun, D., Yang, D., Li, Y., Zhou, J., Wang, W., Wang, Q., ... Zhang, Q. (2020). Psychological impact of 2019 novel coronavirus (2019-nCoV) outbreak in health workers in China. Epidemiology and Infection, 148,1-6. doi:10.1017/S0950268820001090 [ Links ]
*Sun, N., Wei, L., Shi, S., Jiao, D., Song, R., Ma, L., ... Wang, H. (2020). A qualitative study on the psychological experience of caregivers of COVID-19 patients. American Journal of Infection Control, 48(6),592-598. doi:10.1016/j.ajic.2020.03.018 [ Links ]
*Tu, Z., He, J., & Zhou, N. (2020). Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak. Medicine, 99(26),e20769. doi:10.1097/MD.0000000000020769 [ Links ]
*Wang, S., Xie, L., Xu, Y., Yu, S., Yao, B., & Xiang, D. (2020). Sleep disturbances among medical workers during the outbreak of COVID-2019. Occupational Medicine (Oxford, England),2-7. doi:10.1093/occmed/kqaa074 [ Links ]
*Wu, W., Zhang, Y., Wang, P., Zhang, L., Wang, G., Lei, G., ... Luo, M. (2020). Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. Journal of Medical Virology, 92(10),1-9. doi:10.1002/jmv.25914 [ Links ]
*Xing, J., Sun, N., Xu, J., Geng, S., & Li, Y. (2020). Study of the mental health status of medical personnel dealing with new coronavirus pneumonia. PLoS ONE, 15(5),1-10. doi:10.1371/journal.pone.0233145 [ Links ]
*Yin, Q., Sun, Z., Liu, T., Ni, X., Deng, X., Jia, Y., ... Liu, W. (2020). Post-traumatic stress symptoms of health care workers during the corona virus disease 2019. Clinical Psychology and Psychotherapy, 27(3),384-395. doi:10.1002/cpp.2477 [ Links ]
Zerbini, G., Ebigbo, A., Reicherts, P., Kunz, M., & Messman, H. (2020). Psychosocial burden of healthcare professionals in times of Covid-19: A survey conducted at the university hospital Augsburg. GMS German Medical Science, 18, 1-9. doi:10.3205/000281 [ Links ]
*Zhang, C., Yang, L., Liu, S., Ma, S., Wang, Y., Cai, Z., ... Zhang, B. (2020). Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Frontiers in Psychiatry, 11(April),1-9. doi:10.3389/fpsyt.2020.00306 [ Links ]
*Zhang, W. R., Wang, K., Yin, L., Zhao, W. F., Xue, Q., Peng, M., ... Wang, H. X. (2020). Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychotherapy and Psychosomatics, 89(4),242-250. doi:10.1159/000507639 [ Links ]
*Zhuo, K., Gao, C., Wang, X., Zhang, C., & Wang, Z. (2020). Stress and sleep: a survey based on wearable sleep trackers among medical and nursing staff in Wuhan during the COVID-19 pandemic. General Psychiatry, 33(3),e100260. doi:10.1136/gpsych-2020-100260 [ Links ]
 Correspondence:
Correspondence:
Silvana Alba Scortegagna
Graduate Program in Human Aging, Universidade de Passo Fundo (RS), Campus I
Bairro São José, BR 285, Km 171
Passo Fundo, RS, Brazil. Cx. Postal 611. CEP 99052-900
E-mail: silvanalba@upf.br
Submission: 26/08/2020
Acceptance: 30/10/2020
Funding: Rio Grande do Sul Research Support Foundation (FAPERGS).
Authors' notes:
Silvana Alba Scortegagna, Department of Psychology, University of Passo Fundo (UPF); Eduardo dos S. de Lima, Department of Psychology, University of Passo Fundo (UPF); Sonia Regina Pasian, Department of Psychology, University of São Paulo (USP-FFCLRP); Deise M. do Amparo, Department of Clinical Psychology, University of Brasília (UnB).














