Serviços Personalizados
artigo
Indicadores
Compartilhar
Psicologia: teoria e prática
versão impressa ISSN 1516-3687
Psicol. teor. prat. vol.23 no.2 São Paulo maio/ago. 2021
http://dx.doi.org/10.5935/1980-6906/ePTPPA12940
ARTICLES
PSYCHOLOGICAL ASSESSMENT
Relationship between depression and global and specific personality global functioning
Relación entre la depresión y el funcionamiento global de la personalidad global y específica
Lucas de F. Carvalho ; Makilim N. Baptista
; Makilim N. Baptista ; Midiã Beatriz Guillen
; Midiã Beatriz Guillen ; André P. Gonçalves
; André P. Gonçalves ; Aline P. C. Miskulin
; Aline P. C. Miskulin
São Francisco University (USF), Campinas, SP, Brazil
ABSTRACT
This study aimed to investigate the relationship between depressive symptoms and pathological personality functioning (PPF) and specific indicators of pathological personality patterns. The participants were 446 adults from the general population. Part of the sample (n = 237) answered scales evaluating the PPF (Dimensional Clinical Personality Inventory - screening (IDCP-Screening)) and symptoms of depression (Baptist Depression Scale - screening (EBADEP-Screening)); another part (n = 209) answered tests evaluating personality disorders (PD) (SCID-II personality questionnaire; SCID-II-PQ) and symptoms of depression (EBADEP-screening). The results indicated that both PPF and PD showed positive associations with depressive symptoms, although associations with PPF were stronger. The PD most associated with depressive symptoms were avoidant, dependent, and borderline. Findings suggest that PPF and specific pathological patterns are risk factors for the onset of depressive symptoms.
Keywords: major depressive disorder; personality traits; personality assessment; psychopathology; mental health.
RESUMEN
El objetivo del presente estudio fue investigar las relaciones entre los síntomas depresivos y el funcionamiento patológico de la personalidad (PPF) y los indicadores específicos de los patrones patológicos de la personalidad. 446 adultos de la población general participaron en el estudio. Una parte de la muestra (n = 237) respondió a las pruebas que evaluaban PPF (Inventario Dimensional Clinico de Personalidad Dimensional (IDCP)) y síntomas de depresión (Escala de Depresión Baptista - (EBADEP)); otra parte (n = 209) respondieron pruebas que evaluaban TP (cuestionario de personalidad SCID-II; SCID-II-QP) y síntomas de depresión (cribado EBADEP). Los resultados indicaron que tanto PPF como TP mostraron asociaciones positivas con síntomas depresivos, aunque las asociaciones con PPF fueron más fuertes. Las TB más asociadas con síntomas depresivos fueron evitantes, dependientes y dudosas. Los hallazgos sugieren que PPF y patrones específicos son factores de riesgo para la aparición de síntomas depresivos.
Palabras clave: trastorno depresivo mayor; rasgos de personalidad; evaluación de personalidad; psicopatología; salud mental.
1. Introduction
The pathological manifestation of personality traits characterizes pathological personality functioning (PPF) in a dimensional perspective, and high levels cause damage to the person's life (Skodol et al., 2011; Widiger & Costa, 2013). Current literature indicates a global pathological component of personality (e.g., Kotov et al., 2017; Widiger et al., 2019), and this study understands this component as the PPF. Previous evidence indicates a positive relationship between PPF and depressive symptomatology, i.e., people high in PPF are more likely to have higher levels of depressive symptomatology (Gonçalves, Pimentel, & Carvalho, 2020; Sevilla-Llewellyn-Jones et al., 2018; Tsanas et al., 2016).
The most extreme cases of PPF are characterized by personality disorders (PD). The prevalence of PD in association with depressive symptomatology can range from 20% to 50% in hospitalized patients and from 50% to 85% in outpatients, besides being associated with environmental and biological/genetic factors (Corruble, Ginestet, & Guelfi, 1996; Czajkowski, Røysamb, Ørstavik, & Neale, 2010; Fava et al., 1996; Reichborn-Kjennerud, Lingjaerde, & Dahl, 1994).
Understanding the relationship between symptoms of depression and PPF may be central in several ways, such as helping to elucidate the more proximal processes involved in the development of mood disorders, in planning specific interventions, and in predicting responses to treatment (Gabbard, Simonsen, & College, 2007; Lahey, 2004; Quilty et al., 2008). Although associations between PPF and depression symptoms are evident, previous studies indicate that some PDs are more associated with these symptoms compared to others. The presence of specific PD also increases the chances of recurrence of depressive episodes and vice-versa. Despite the controversial results in the literature, in general, there is an agreement that depressive patients with comorbidities of PD develop affective disorders earlier, are more often hospitalized, have a more compromised social support (e.g., separation, divorce), have a lower quality of life and more stressful life conditions, and present more suicidal ideations and attempts (Brieger et al., 2002; Oumaya et al., 2008; Pompili, Girardi, Ruberto, & Tatarelli, 2009; Tyrer, Reed, & Crawford, 2015). Furthermore, the literature also mentions this association in community samples (Newton-Howes et al., 2014).
Some PD are more clearly associated with depressive symptoms. Hirschfeld (1999) reports that patients with avoidant, borderline, and histrionic PD can be susceptible to insults and frustrations, which would favour the onset of dysphoria and depression. Wongpakaran, Wongpakaran, Boonyanaruthee, Pinyopornpanish, & Intraperset (2015) interviewed 85 depressed outpatients and concluded that the PDs most closely related to depressive symptoms are borderline and obsessive-compulsive. Kool et al. (2005) also found a higher prevalence of dependent, paranoid, avoidant, borderline, and obsessive-compulsive PD in outpatients with major depression and double depression. Finally, Hirschfeld (1996) conducted a review of six studies with a sample of 1,624 depressed patients, concluding that the PDs most present in patients with depression and double depression were the avoidant, borderline, self-defeating, dependent, and obsessive-compulsive. These results indicate that, although PPF is associated with depressive symptoms, specific PDs are even more related than PPF.
Our broad scope was to present empirical data on the associations between depression and pathological personality traits, adding evidence to the previous literature. Moreover, we could not find studies conducted in Brazil reporting findings on both PPF and PDs associations with depressive symptoms. The present study aimed to investigate relationships between depressive symptoms and global (PPF) and specific (PD) indicators of pathological personality patterns. We hypothesized for this study that: h1) PPF should be positively related to depressive symptoms (Gonçalves et al., 2020; Sevilla-Llewellyn-Jones et al., 2018; Tsanas et al., 2016); and h2) PD showing higher associations with depressive symptoms should be obsessive-compulsive, dependent and borderline (Gunderson, Herpertz, Skodol, Torgersen, & Zanarin, 2018; Mulder, Joyce, & Frampton, 2010; Alnaes & Torgersen, 1997; Hirschfeld, 1999; Gamez, Watson, & Doebbeling, 2007; Reichborn-Kjennerud et al., 1994; Ramklint & Ekselius, 2003; Garyfallos et al., 1999; Wongpakaran et al., 2015; Kool et al., 2005).
2. Method
2.1 Sample
Using a cross-sectional design, we recruited two convenience samples (n1 = 237; n2 = 209) from the community. One sample was composed of people ranging from 18 to 65 years of age (M = 28; SD = 8.9), mostly female (78.9%), and 51% reported having participated in psychotherapy. The other sample was composed of students who attended a Psychology course at a university in the countryside of the State of São Paulo, Brazil. Most of them were female (78.5%), age ranged from 18 to 51 (M = 23.22; SD = 7.25), and 35.5% reported having had psychotherapy.
The first group is identified as a PPF sample because we administered scales measuring PPF in these participants (EBADEP-screening and IDCP-SV). The second group is identified as a PD sample (EBADEP-screening and SCID-PQ-II) because they answered scales assessing specific PD.
2.2 Instruments
• Baptista Depression Scale - screening version (EBADEP-screening; Baptista & Carvalho, 2018): The EBADEP-screening was developed based on the adult version of EBADEP (EBADEP-A) and aims to track depression symptoms. We selected 15 items from the short version of EBADEP-A, with the descriptors most commonly used in psychiatric manuals (core symptoms), i.e., items related to sad mood, anhedonia, guilt, fatigue, concentration, suicidal ideation, and sleep. In the development study (Baptista & Carvalho, 2018), EBADEP-screening was able to discriminate between 40 patients diagnosed with depression by SCID-I and 40 people without depression with sensitivity equal to 95.0 and specificity 87.5. We used as cut-off a score equal to 19, i.e., people with a score of 19 or more were considered positive for depression. In this research, EBADEP-screening presented a Cronbach's alpha internal consistency reliability of .88.
• Dimensional Clinical Personality Inventory - screening version (IDCP-SV; Carvalho, Pianowski, & Reis, 2017): The IDCP-SV was developed based on the full version of IDCP, a test to measure pathological personality traits. The instrument consists of 15 items arranged on a 4-point Likert scale, in which 1 stands for "nothing to do with me" and 4 "everything to do with me." The IDCP-SV's instructions comprise a section with socio-demographic questions used for analysis in this research. We used a cut-off score equal to 10, i.e., people with a score of 10 or more were considered positive for PD (positive group). We tested for the Cronbach's alpha internal consistency reliability of the IDCP-SV, which was .83.
• Structured Clinical Interview for DSM-IV Personality Questionnaire (SCID-PQ-II; First, Gibbon, Spitzer, Williams, & Benjamin, 1997): The SCID-PQ-II was developed to assess the 10 personality disorders included in the DSM-IV Axis II, besides the two personality disorders not included (Depressive, Passive-Aggressive). It is a self-report instrument consisting of 119 items that should be answered with yes or no. Psychometric properties demonstrated adequacy in the present study. The SCID-II-PQ presented Cronbach's alpha internal consistency reliability higher than or equal to .60 for some of the scales but ranged from .06 to .52 for Obsessive-compulsive, Passive-Aggressive, Paranoid, Schizotypal, Schizoid, Histrionic and Narcissist. We did not include the Depressive and Passive-aggressive scales once the current psychiatry manuals do not use this diagnostic.
2.3 Procedure
A Brazilian Research Ethics Committee approved this study. For the PPF sample, data collection was done online, via Google Forms. The link inviting individuals to participate in the study was shared on the social media website Facebook and by e-mail, using the snowball effect to reach the maximum number of people. To these participants, the IDCP-SV and the EBADEP-screening were administered. For the PD sample, data collection was conducted face to face and collectively in classrooms of the Psychology course of a university placed in a country city of São Paulo State. To this sample, the SCID-II-PQ and the EBADEP-screening were administered.
2.4 Statistical analysis
For data analysis, with the SPSS statistical software version 21, we used the previous cut-offs from the literature for the IDCP-SV and the EBADEP-screening. Statistical analyses were separately conducted, as the PPF sample answered the EBADEP-screening and the IDCP-SV, and the PD sample answered the EBADEP-screening and the SCID-PQ-II. Mean comparisons were conducted using the t-test, and Cohen's d was calculated (h1). Pearson correlations were performed between the IDCP-SV scores and the depression scores (h1). Finally, we conducted Pearson's correlation between PD and depression symptomatology (h2). We consider significant differences when p <.05 and magnitudes are above .30.
3. Results
Figure 3.1 presents the mean comparison between two groups established from the IDCP-SV score on the EBADEP-screening factors.
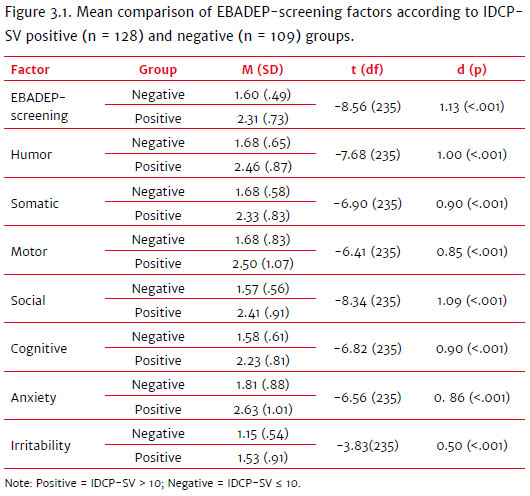
Comparisons showed significant differences between groups, and the IDCP-SV positive group (IDCP-SV > 10) presented the highest means in the EBADEP-screening factors in comparison to the negative group (IDCP-SV < 10). Most of the effects were high, especially for the Social and Humour factors.
Complementing findings observed in Figure 3.1, we performed correlations between IDCP-SV and EBADEP-screening. The correlation between the EBADEP-screening and the IDCP-SV total score was .64 (p <.01). The correlations of IDCP-SV with specific depression factors were: Humour (r = .56; p <.01); Somatic (r = .58; p <.01); Motor (r = .48; p <.01); Social (r = .57; p <.01); Cognitive (r = .53; p <.01); Anxiety (.50; p <.01), and Irritability (.44 p< .01). All correlations were positive and significant, most with high or moderate effects. Figure 3.2 shows the correlations between EBADEP-screening and each of the PD through SCID-II-PQ.
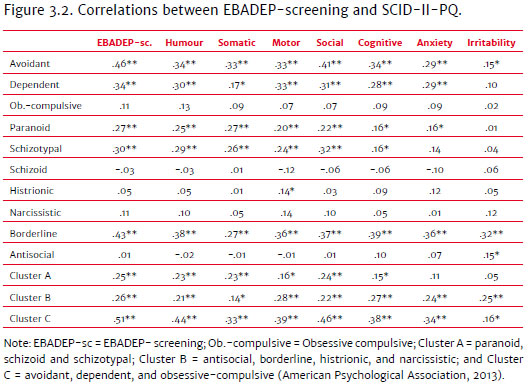
Correlations were positive between PD and depression scores, in general. The strongest correlations with EBADEP-screening scores were avoidant, dependent, schizotypal, and borderline. Cluster C PD score was the cluster with a higher association with depression scores.
4. Discussion
This study aimed to investigate relationships between depressive symptomatology and global (PPF) and specific (10 PD) indicators of pathological personality patterns. In general, the hypotheses elaborated for this study were confirmed by the empirical findings: H1) the PPF presented a positive and significant relationship with depressive symptoms; H2) except for obsessive-compulsive PD, borderline and dependent PDs were the most associated with depressive symptoms. These results indicate that personality functioning changes are related to depressive symptoms, suggesting that people with PPF are part of a risk group for depressive symptoms. Results are discussed in detail in the following paragraphs.
PPF was positively associated with depressive symptoms, corroborating H1, as indicated in previous evidence (Gonçalves et al., 2020; Sevilla-Llewellyn-Jones et al., 2018; Tsanas et al., 2016). This result suggests PPF as a risk factor for depressive symptoms. These findings agree with previous studies, showing that people with increased pathological features are more likely to manifest depressive symptoms (Gonçalves et al., 2020; Alizadeh et al., 2018; Crempien et al., 2017; van der Wal et al., 2018).
Regarding h2, in general, the data confirms previous literature, as avoidant, dependent, and borderline were the PDs most related to depressive symptomatology (Gunderson et al., 2008; Mulder et al., 2010; Torgersen, 1997). Only obsessive-compulsive PD, previously associated with depressive symptoms (Gunderson et al., 2008; Gamez et al., 2007; Reichborn-Kjennerud et al., 1994; Ramklint & Ekselius, 2003; Wongpakaran et al., 2015; Kool et al., 2005), did not show a significant relationship in the present study. Moreover, schizotypal PD had one of the highest associations with depressive symptoms. Although this result was not expected, it can be explained by the schizotypal PD's tendency to present more losses than other PDs (Skodol et al., 2002), along with the borderline, for example (Millon, 2016). In addition to the specific relationship with some PDs, as predicted in the literature (e.g., Gunderson et al., 2008, Mulder et al., 2010; Wongpakaran et al., 2015), cluster C was also more associated with depressive symptomatology. Indeed, cluster C encompasses some of the PDs most associated with depression individually, so there is an inflation of this cluster.
Our findings indicate that both the global PPF and specific PD presented significant relationships with depressive symptoms, although PPF showed stronger associations. Moreover, we can observe that obsessive-compulsive PD had a low correlation magnitude, approaching zero. This result indicates that the relation between the obsessive-compulsive PD and depression symptoms tends to occur specifically in more severe PD cases, since the comparison between groups showed a significant difference. Future studies should seek to replicate these data, focusing specifically on the relationship between these conditions. Regarding depressive symptoms, humour, somatic, motor, social, and cognitive factors shared more variance with borderline, avoidant, and dependent PD, being these relations among the highest observed. The irritability factor presented a tendency for lower correlations, being the highest correlations with borderline PD and cluster B, which encompasses borderline. These results are coherent, considering borderline functioning (American Psychological Association, 2013; Kotov et al., 2017), but need to be further explored in future studies. Also, the anxiety factor shared variance mainly with avoidant, dependent, paranoid, and borderline PDs. As some of these PDs compose cluster C (i.e., anxious cluster; American Psychological Association, 2013), the literature supports these findings.
Our findings should be weighed according to the main limitations of this study. First, the samples did not include people with known PD diagnosis, which may have limited the variability in the responses observed. Second, the samples were mainly formed by women and with a large dispersion on age, which may bias our findings. Moreover, one sample was composed exclusively of college students, which may also have limited responses. Nevertheless, more than half of this sample reported having participated in psychotherapy, which could also be a bias. Future studies should seek to replicate this research's findings, including people with a known diagnosis of depression and PD.
References
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington: APA [ Links ]
Alizadeh, Z., Feizi, A., Rejali, M., Afshar, H., Hassanzadeh Keshteli, A., & Adibi, P. (2018). The predictive value of personality traits for psychological problems (stress, anxiety and depression): Results from a large population based study. Journal of Epidemiology and Global Health, 8(3-4),124-133. doi: 10.1016/j.jegh.2017.11.003 [ Links ]
Alnaes, R., & Torgersen, S. (1997). Personality and personality disorders predict development and relapses of major depression. Acta Psychiatrica Scandinavica, 95(4),336-342. [ Links ]
Baptista, M. N. (2012). Escala Baptista de Depressão - Versão Adulto (EBADEP-A). [Baptista Depression Scale - Adult Version]. São Paulo: Vetor Editora. [ Links ]
Baptista, M. N., & Carvalho, L. D. F. (2018). Diagnostic accuracy of a Brazilian depression self-report measure (EBADEP): Original and short versions. Avaliação Psicológica, 17(4),484-492. doi: 10.15689/ap.2018.1704.8.08 [ Links ]
Brieger, P., Ehrt, U., Bloeink, R., & Marneros, A. (2002). Consequences of comorbid personality disorders in major depression. The Journal of Nervous and Mental Disease, 190(5),304-309. doi: 10.1097/00005053-200205000-00006 [ Links ]
Carvalho, L. D. F., Pianowski, G., & Reis, A. M. (2017). Development and Diagnostic Accuracy of the Screening of the Dimensional Clinical Personality Inventory. Psicologia: Ciência e Profissão, 37(4),1011-1024. doi: 10.1590/1982-3703003082016 [ Links ]
Corruble, E., Ginestet, D., & Guelfi, J. D. (1996). Comorbidity of personality disorders and unipolar major depression: A review. Journal of Affective Disorders, 37(2-3),157-170. doi: 10.1016/0165-0327(95)00091-7 [ Links ]
Crempien, C., Grez, M., Valdés, C., López, M. J., de la Parra, G., & Krause, M. (2017). Role of Personality Functioning in the Quality of Life of Patients with Depression: The Journal of Nervous and Mental Disease, 205(9),705-713. doi: 10.1097/NMD.0000000000000676 [ Links ]
Czajkowski, N., Røysamb, E., Ørstavik, R. E., & Neale, M. C. (2010). Major depression and dimensional representations of DSM-IV personality disorders: A population-based twin study. Psychological Medicine, 40(9),1475-1484. doi: 10.1017/S0033291709991954 [ Links ]
Fava, M., Alpert, J. E., Borus, J. S., Nierenberg, A. A., Pava, J. A., & Rosenbaum, J. F. (1996). Patterns of personality disorder comorbidity in early-onset versus late-onset major depression. American Journal of Psychiatry, 153(10),1308-1312. doi: 10.1176/ajp.153.10.1308 [ Links ]
First, M. B., Gibbon, M., Spitzer, R. L., Williams, J. B. W., & Benjamin, L. S. (1997). SCID-II Personality Questionnaire. Washington, DC: American Psychiatric Press. doi: 10.1007/978-1-4419-1005-9_66 [ Links ]
Gabbard, G. O., Simonsen, E., & College, B. (2007). Complex Case The impact of personality and personality disorders on the treatment of depression. Personality and Mental Health, 175,161-175. doi: 10.1002/pmh.21 [ Links ]
Gamez, W., Watson, D., & Doebbeling, B. N. (2007). Abnormal personality and the mood and anxiety disorders: Implications for structural models of anxiety and depression. Journal of Anxiety Disorders, 21(4),526-539. doi: 10.1016/j.janxdis.2006.08.003 [ Links ]
Garyfallos, G., Adarnopoulou, A., Karastergiou, A., Voikli, M., Sotiropoulou, A., Donias, S., ... Paraschos, A. (1999). Personality disorders in dysthymia and major depression. Acta Psychiatrica Scandinavica, 99(5),332-340. doi: 10.1111/j.1600-0447.1999.tb07238.x [ Links ]
Gonçalves, A. P., Pimentel, R. P. F. A., Carvalho, L.F (2020). Funcionamento patológico da personalidade para predição da depressão, qualidade de vida e esperança. Interação em Psicologia, 24(01),12-19. doi: 10.5380/psi.v24i1.62784 [ Links ]
Gunderson, J. G., Herpertz, S. C., Skodol, A. E., Torgersen, S., & Zanarini, M. C. (2018). Borderline personality disorder. Nature Reviews Disease Primers, 4,18029. doi: 10.1038/nrdp.2018.29 [ Links ]
Hirschfeld, R. M. A. (1999). Personality Disorders and Comorbidity. Depression and Anxiety, 10,142-146. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/10690575 [ Links ]
Hopwood, C. J., Bagby, M., Gralnick, T. M., Ro, E., Ruggero, C., Mullins-Sweatt, S., ... Zimmermann, J. (2018, December 8). Integrating psychotherapy with the Hierarchical Taxonomy of Psychopathology (HiTOP). PsyArXiv Preprints. doi: 10.31234/osf.io/jb8z4 [ Links ]
Kool, S. (2005). Comorbidity of depression and personality disorders. (PhD Thesis). Faculty of Medicine (AMC-UvA), Amsterdam. Retrieved from http://dare.uva.nl/search? metis.record.id=243192 [ Links ]
Kotov, R., Krueger, R. F., Watson, D., Achenbach, T. M., Althoff, R. R., Bagby, R. M. ... Zimmerman, M. (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4),454-477. doi: 10.1037/abn0000258 [ Links ]
Lahey, B. B. (2004). Commentary: Role of temperament in developmental models of psychopathology. Journal of Clinical Child & Adolescent Psychology, 33(1),88-93. doi: 10.1207/S15374424JCCP3301_9 [ Links ]
Millon T. (2016). What is a personality disorder? Journal of Personality Disorders, 30(3),289-306. doi: 10.1521/pedi.2016.30.3.289 [ Links ]
Mulder, R. T., Joyce, P. R., Frampton, C. M. A. (2010). Personality disorders improve in patients treated for major depression. Acta Psychiatrica Scandinavica, 122(3),219-225. doi: 10.1111/j.1600-0447.2009.01502.x [ Links ]
Newton-Howes, G., Tyrer, P., Johnson, T., Mulder, R., Kool, S., Dekker, J., & Schoevers, R. (2014). Influence of Personality on the Outcome of Treatment in depression: Systematic review and meta-analysis. Journal of Personality Disorders, 28(4),577-593. doi: 10.1521/pedi_2013_27_070 [ Links ]
Oumaya, M., Friedman, S., Pham, A., Abdallah, T., Guelfi, J. D., & Rouillon, F. (2008). Borderline personality disorder, self-mutilation and suicide: Literature review. Encephale, 34(5),452-458. doi: 10.1016/j.encep.2007.10.007 [ Links ]
Pompili, M., Girardi, P., Ruberto, A., & Tatarelli R. (2009). Suicide in borderline personality disorder: A meta-analysis. Nordic Journal of Psychiatry, 59(5),319-324. doi: 10.1080/08039480500320025 [ Links ]
Quilty, L. C., De Fruyt, F., Rolland, J. P., Kennedy, S. H., Rouillon, P. F., & Bagby, R. M. (2008). Dimensional personality traits and treatment outcome in patients with major depressive disorder. Journal of Affective Disorders, 108(3),241-250. doi: 10.1016/j.jad.2007.10.022
Ramklint, M., & Ekselius, L. (2003). Personality traits and personality disorders in early onset versus late onset major depression. Journal of Affective Disorders, 75(1),35-42. doi: 10.1016/S0165-0327(02)00028-9 [ Links ]
Reichborn-Kjennerud, T., Lingjaerde, O., & Dahl, A. A. (1994). Personality disorders in patients with winter depression. Acta Psychiatrica Scandinavica, 90(6),413-419. doi: 10.1111/j.1600-0447.1994.tb01616.x [ Links ]
Sevilla-Llewellyn-Jones, J., Camino, G., Russo, D. A., Painter, M., Montejo, A. L., Ochoa, S., ... Perez, J. (2018). Clinically significant personality traits in individuals at high risk of developing psychosis. Psychiatry Research, 261,498-503. doi: 10.1016/j.psychres.2018.01.027 [ Links ]
Skodol, A. E., Clark, L. A., Bender, D. S., Krueger, R. F., Morey, L. C., Verheul, R., ... Oldham, J. M. (2011). Proposed changes in personality and personality disorder assessment and diagnosis for DSM-5 Part I: Description and rationale. Personality disorders: theory, research, and treatment, 2(1),4. doi: 10.1037/a0021891 [ Links ]
Tsanas, A., Saunders, K. E. A., Bilderbeck, A. C., Palmius, N., Osipov, M., Clifford, G. D., ... De Vos, M. (2016). Daily longitudinal self-monitoring of mood variability in bipolar disorder and borderline personality disorder. Journal of Affective Disorders, 205,225-233. doi: 10.1016/j.jad.2016.06.065 [ Links ]
Tyrer, P., Reed, J. M., Crawford, M. J. (2015). Classification, assessment, prevalence, and effect of personality disorder. Lancet (London, England), 385(9969),717-726. doi: 10.1016/S0140-6736(14)61995-4 [ Links ]
van der Wal, S. J., Bienvenu, O. J., Romanoski, A. J., Eaton, W. W., Nestadt, G., & Samuels, J. (2018). Longitudinal relationships between personality disorder dimensions and depression in a community sample. Neurology, Psychiatry and Brain Research, 30,56-61. doi: 10.1016/j.npbr.2018.05.005 [ Links ]
Widiger, T. A., Bach, B., Chmielewski, M., Clark, L. A., DeYoung, C., Hopwood, C. J., ... Mullins-Sweatt, S. N. (2019). Criterion A of the AMPD in HiTOP. Journal of Personality Assessment, 101(4),345-355. doi: 10.1080/00223891.2018.1465431 [ Links ]
Widiger, T. A., & Costa, P. T., Jr. (Eds.). (2013). Personality disorders and the five-factor model of personality (3rd ed.). American Psychological Association. doi: 10.1037/13939-000 [ Links ]
Wongpakaran, N., Wongpakaran, T., Boonyanaruthee, V., Pinyopornpanish, M., & Intraperset, S. (2015). Comorbid personality disorders among patients with depression. Neuropsychiatric Disease and Treatment, 11,1091-1096. doi: 10.2147/NDT.S82884 [ Links ]
 Correspondence:
Correspondence:
Lucas de Francisco Carvalho
R. Waldemar César da Silveira, 105, Jardim Cura D'ars
Campinas, SP, Brazil. CEP 13045-510
E-mail: lucas@labape.com.br
Submission: 14/11/2019
Acceptance: 24/02/2020
Authors' note: Lucas de F. Carvalho, Psychology Department, São Francisco University (USF); Makilim N. Baptista, Psychology Department, São Francisco University (USF); Midiã Beatriz Guillen, Psychology Department, São Francisco University (USF); André P. Gonçalves, Psychology Department, São Francisco University (USF); Aline P. C. Miskulin, Psychology Department, São Francisco University (USF).














