Serviços Personalizados
artigo
Indicadores
Compartilhar
Psicologia: teoria e prática
versão impressa ISSN 1516-3687
Psicol. teor. prat. vol.24 no.1 São Paulo jan./abr. 2022
http://dx.doi.org/10.5935/1980-6906/ePTPCP14089.en
CLINICAL PSYCHOLOGY
Fear of childbirth: a review of interventions based on cognitive-behavioral therapy
Medo do parto: uma revisão das intervenções baseadas na terapia cognitivo-comportamental
Miedo al parto: una revisión de intervenciones basadas en terapia cognitivo-conductual
Lívia R. de C. NunesI ; Fernanda C. CoutinhoII
; Fernanda C. CoutinhoII ; Veruska Andréa dos SantosIII
; Veruska Andréa dos SantosIII
IPostgraduate Program in Social Psychology, Rio de Janeiro State University (UERJ)
IIPostgraduate Program in Cognitive-Behavioral Therapy, Pontifical Catholic University of Rio de Janeiro (PUC-Rio)
IIIPsychiatric Institute (IPUB), The Federal University of Rio de Janeiro (UFRJ)
ABSTRACT
Fear of vaginal birth is a very common phenomenon among women and may significantly impact maternal-infant health. The goal of this study is to investigate how Cognitive- @Behavioral Therapy (CBT) has been applied in cases of fear of childbirth and assess the efficacy of such interventions. A systematic review of these practices was made using the BVS Brazil, Scopus, and PubMed databases, from February to April 2019. After analyzing the inclusion and exclusion criteria, a total of six full studies were selected as the final sample for this research. Therapeutic techniques such as cognitive restructuring, exposure, and mindfulness have proven to be important means of developing a less catastrophic perception of childbirth along with greater self-confidence in the abilities to cope with labor. The review led to the conclusion that CBT does have the potential to treat fear of childbirth.
Keywords: childbirth, Cognitive-Behavioral Therapy, fear, pregnancy, tokophobia
RESUMO
O medo do parto vaginal é bastante comum e pode ter impactos relevantes na saúde materno-infantil. Este estudo teve como objetivos investigar de que forma a Terapia Cognitivo-Comportamental (TCC) tem sido aplicada em casos de medo do parto e avaliar a eficácia dessas intervenções. Realizou-se uma revisão sistemática da literatura por meio das bases de dados BVS Brasil, Scopus e PubMed, no período de fevereiro a abril de 2019. Após a análise dos critérios de inclusão e exclusão, um total de seis textos completos constituíram a amostra final. Técnicas terapêuticas como a reestruturação cognitiva, a exposição e a atenção plena demonstraram ser relevantes para a elaboração de uma percepção menos catastrófica do parto e para o desenvolvimento de maior confiança nas próprias habilidades de enfrentamento do trabalho de parto. Conclui-se que as intervenções em TCC apresentam potencial benefício para o tratamento do medo do parto.
Palavras-chaves: gravidez, medo, parto, Terapia Cognitivo-Comportamental, tocofobia
RESUMEN
El miedo al parto es muy común y puede afectar significativamente la salud materno-infantil. El objetivo de este estudio fue investigar cómo se ha aplicado la Terapia Cognitivo-Conductual (TCC) en casos de miedo al parto y evaluar la eficacia de las intervenciones. Se realizó una revisión sistemática a través de las bases de datos BVS Brasil, Scopus y PubMed, de febrero a abril de 2019. Después de analizar los criterios de inclusión y exclusión, un total de seis textos completos constituyeron la muestra final. Las técnicas terapéuticas como la reestructuración cognitiva, la exposición y la atención plena demostraron ser relevantes para la elaboración de una percepción menos catastrófica del parto y para el desarrollo de una mayor confianza en las capacidades propias para enfrentar el parto. La revisión llevó a la conclusión de que la TCC tiene potencial benéfico para tratar el miedo al parto.
Palabras-claves: embarazo, miedo, parto, Terapia Cognitivo-Conductual, tocofobia
It is known that the experience of giving birth is accompanied by a small risk of maternal morbidity and mortality (World Health Organization [WHO], 2019). In Brazil, in 2017, 60 maternal deaths were registered for every 100,000 live births (WHO, 2019). Thus, some level of fear related to childbirth is expected. However, other factors such as cultural influence, misinformation, the media, negative reports from other women, and the medicalizing obstetric care model can exacerbate this fear (Pereira et al., 2011). This care model has as a strong characteristic the doctor-patient power relationship. In this way, the doctor decides what information about pregnancy and childbirth will be offered to the woman. Often, the information (or the lack of it) facilitates the fear of vaginal birth and reinforces the choice of an elective cesarean section as a more practical, painless, and convenient option (Pereira et al., 2011).
Fear of childbirth can be classified according to the intensity of the emotion. A low level of fear can be understood as a manageable concern that helps a woman prepare for the moment of delivery. A moderate level represents a concern that is difficult to tolerate without support, but one that does not yet compromise a woman's mental health. Severe fear can compromise mental health and damage the connection with the baby. Phobic fear, also known as tokophobia or childbirth phobia, can even generate the avoidance of pregnancy or childbirth, even if the baby is wanted (Ryding, 2017). Other forms of avoidance include avoiding information about labor, avoiding participating in support groups, avoiding fear-related memories, and choosing cesarean section as the route of delivery (Hofberg & Brockington, 2000; Rondung et al., 2016).
The word "tokophobia" comes from the Greek term tokos, which means "childbirth". Currently, studies often refer to tokophobia as belonging to the domain of anxiety disorders (Hofberg & Ward, 2003; Rondung et al., 2016). It can be classified as primary or secondary tokophobia. Primary tokophobia usually starts in adolescence or early adulthood and can originate from different factors, including: indirect exposure to traumatic or stressful childbirth situations; obtaining negative information about childbirth; sexual abuse situations; and the generalization of other fears (e.g., blood phobia, injections, hospitals, among others) (Hofberg & Ward, 2003; Rondung et al., 2016).
Secondary tokophobia, on the other hand, is primarily caused by fear conditioning through a traumatic obstetric event. This event is most often related to a traumatic birth, but it can also occur after a miscarriage, an induced abortion, or in cases of a stillbirth. In these cases, fear of childbirth may be related to Post-Traumatic Stress Disorder (PTSD) (Hofberg & Ward, 2003; Rondung et al., 2016). The relationship between traumatic births, secondary tokophobia, and PTSD is especially relevant when we consider that 25% of women reported having suffered some type of violence during childbirth care in Brazil, according to data from a public opinion survey conducted in 2010 (Venturi et al., 2010).
There is an estimated 14% prevalence of tokophobia in the world population, a number that seems to have increased from the year 2000 onwards (O'Connell et al., 2017). However, this estimate is limited by the lack of consistency in the diagnosis of the disorder. In a study carried out in Finland, of the 329 pregnant women interviewed, 78% were afraid of pregnancy, childbirth, or both events (Melender, 2002). Another study carried out in Sweden, with 139 pregnant women, verified the presence of severe fear of childbirth in 9% of the research participants while 17% had moderate fear (Areskog et al., 1981). There is still no information on the prevalence of tokophobia in the Brazilian population. In 2021, Nunes et al. (2021) published the first instrument to measure childbirth phobia validated in the country: the Tokophobia Assessment Questionnaire (Questionário de Avaliação da Partofobia, in Portuguese).
Despite being a little researched topic in Brazil, fear of labor pain is pointed out as one of the main motivations for choosing an elective cesarean section (Pereira et al., 2011). One reason is the illusion of control that cesareans sections offer (Bewley & Cockburn, 2002). The large number of cesarean sections performed in the country received great attention with the results of the study Birth in Brazil (Nascer no Brasil) (Leal et al., 2012). Of the 23,894 women interviewed in the national territory, 52% had their children through cesarean section deliveries. Analyzing only the private sector, it was found that 88% of births were by cesarean sections, a number that is even more worrying, as surgeries of this type involve immediate and long-term risks (WHO, 2015). In contrast, approximately 70% of Brazilian women wanted a vaginal birth in early pregnancy. However, few were supported in their initial choices.
The difference between the number of women who want to give vaginal birth and the number of women who actually perform it may be related to the false idea that a cesarean section would be safer for the woman (even without a real medical reason) and to the lack of information offered to pregnant women during prenatal care. Consequently, women's power of autonomy is undermined by the impossibility of making an informed decision (Pereira et al., 2011).
Women undergoing cesarean section surgery without a real obstetric reason (Souza et al., 2010) are exposed, along with their children, to unnecessary morbidity and mortality risks (Leal et al., 2012). In this sense, there is an ethical conflict in performing an elective cesarean section in women who request it out of fear of childbirth without first providing attention and psychological support. If the woman opts for cesarean section surgery out of severe fear of childbirth, even after receiving psychological support, denying elective surgery would be cruel (Bewley & Cockburn, 2002). In any case, provided the necessary resources for a conscious choice, it is important that the woman's desire is respected, in accordance with her reproductive and sexual rights (Zorzam & Cavalcanti, 2016). In a study carried out by Hofberg and Brockington (2000), the denial of the route of delivery chosen by the woman was associated with the development of PTSD after delivery.
The support and psychological care offered to women with severe fear of childbirth is even more fundamental when we consider the vicious cycle of fear of childbirth. Women with high levels of prenatal fear of childbirth are at increased risk of feeling fear during labor and perceiving the situation as threatening. These circumstances can increase the chances of a negative birth experience, which can lead to fear related to a future birth (Rondung et al., 2016). However, therapeutic interventions focused on fear of childbirth differ in the methods of assessment, conceptualization, and application of interventions (Striebich et al., 2018). Among these, Cognitive-Behavioral Therapy (CBT) has been investigated in the treatment for fear of giving birth (Striebich et al., 2018).
CBT is a psychotherapy approach consisting of structured sessions with a limited duration. The approach is based on the cognitive model, according to which distorted or dysfunctional cognitions (affecting the patient's mood and behavior) are common to all psychological disorders. In this sense, realistic assessment and changes in thinking produce an improvement in mood and behavior (Beck, 2007). In addition to identifying and restructuring dysfunctional thoughts, the approach also encompasses techniques that aid in emotional regulation and behavioral change. Among the techniques used, we can mention psychoeducation, empathic confrontation, exposure, and relaxation (Beck, 2007).
Ghazaie et al. (2016) carried out a randomized clinical study with 25 women and concluded that CBT can lessen unnecessary cesarean sections by reducing the fear of childbirth and pain and by increasing the perception of self-efficacy. After the systematic review carried out by Striebich et al. (2018) on the use of different types of therapy in the management of fear of childbirth, this review can contribute to the matter by focusing on the use of CBT. Thus, the aim of this review was to investigate how CBT has been applied in cases of fear of childbirth and which studies have assessed its efficacy. It is hoped that this study will contribute to a better understanding of the psychological processes in women afraid of childbirth and will help identify the best forms of treatment and prevention based on CBT.
Method
As pointed out by Sampaio and Mancini (2007), the systematic review uses the existing literature on a particular topic as a data source and is intended to summarize and present evidence related to a specific intervention. This process takes place through the application of explicit and systematic methods of search, critical assessment, and synthesis of selected information (Sampaio & Mancini, 2007).
Material inclusion criteria
The search inclusion criteria were: full text in English or Portuguese languages; studies that include women (pregnant or not) afraid of childbirth; studies that had CBT or mindfulness practices as intervention. We chose to include studies whose interventions were based on mindfulness, due to the wide use of these practices in different contemporary behavioral and cognitive therapies (Vandenberghe & Sousa, 2006). The exclusion criteria were: literature reviews or comments; studies not focused on fear of childbirth; and studies that did not have CBT or mindfulness practices as an intervention. There was no restriction regarding the period of publication of the studies.
Documentary data collection procedures
The research questions that guided this study were: how has CBT been applied in cases of fear of childbirth? Have these interventions shown to be effective? The study was conducted using the BVS Brasil, Scopus, and PubMed databases, from February to April 2019. The following descriptors and Boolean operators were used: "Cognitive Therapy" OR "Cognitive-behavioral therapy" OR "CBT" AND "fear of birth" OR "fear of childbirth" OR "tokophobia". This combination was chosen through an articulation between the vocabulary control of the Medical Subject Headings (MeSH), the Descritores em Ciências da Saúde (DeCS, Health Sciences Descriptors), and the descriptors used by Striebich et al. (2018) in their systematic review of interventions for fear of childbirth. Therefore, the combination of the terms presented was intended to focus as much as possible on the topic of interest in this study.
Analysis Procedures
For the qualitative analysis of the results, the studies were categorized based on title, authorship, year of publication, country of origin, study objective, study design, target audience, instrument used in the assessment of fear of childbirth, intervention technique, and treatment efficacy.
Results
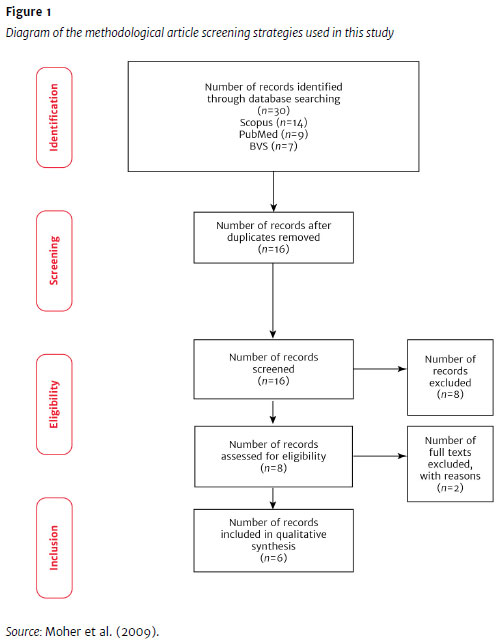
Initially, 30 articles were identified. After removing the duplicates, 16 articles were selected, eight of which were excluded in accordance with the inclusion and exclusion criteria of this review. Thus, a total of eight full studies were obtained, of which two were removed, as they represent study protocols. Finally, six articles were included in the qualitative synthesis. The total number of studies selected and eliminated in each of the steps of the systematic assessment process can be seen in the assessment process flowchart (Figure 1), according to the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses - PRISMA (Moher et al., 2009).
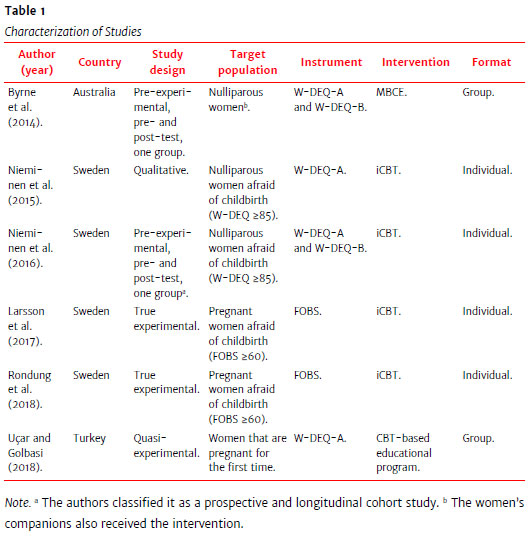
As shown in Table 1, of the six selected articles, four are Swedish, one is Australian and the other one is Turkish. All articles were published in English, from 2014 to 2018.
Instruments used to assess fear of childbirth
The most frequently used instrument was the Wijma Delivery Expectancy/Experience Questionnaire (W-DEQ) (Wijma et al., 1998). Developed by a group of Swedish researchers, the instrument consists of 33 items assessed by a six-point Likert scale. The questionnaire was designed with the intention of measuring fear of childbirth through the woman's cognitive assessments of childbirth (Wijma et al., 1998). The instrument measures both the fear related to childbirth during pregnancy and the fear related to childbirth during the puerperium, through questions about expectations regarding childbirth (version A) and experiences after childbirth (version B) (Wijma et al., 1998). The cutoff point ≥85 is considered adequate for identifying severe fear of childbirth (Nieminen et al., 2016)
Another instrument used was the Fear of Birth Scale (FOBS) (Ternström, 2018), a visual analogue scale that addresses two constructs: fear and worry. Respondents are asked to assess their feelings about the upcoming birth by answering the question: "How do you feel right now about the approaching birth?". The answer is given through a visual analogue scale anchored by the words "calm/worried" and "no fear/strong fear". The score can vary between 0 and 100 - the higher the score, the greater the fear of childbirth. The score used as a cutoff score to identify fear of childbirth is 60 (Ternström, 2018). Unlike other studies, the study by Byrne et al. (2014) and the one by Uçar and Golbasi (2018) did not have as inclusion criterion women previously identified with fear of childbirth/fear of birth (FOB). Thus, the instrument for assessing fear of childbirth was used at the beginning of the study, but there was no established cutoff point for the instrument's score.
Intervention techniques
As for the intervention techniques, the most used was the Internet-Based Cognitive-Behavioral Therapy (iCBT). It is usually applied through an online platform that provides self-guided modules with psychoeducational materials and CBT exercises (Berger, 2016). Platforms also allow the therapist to communicate with the patient privately and confidentially and monitor their development during treatment (Berger, 2016). In addition to the individual online version, CBT was also applied in person by Uçar and Golbasi (2018) in group meetings with five to nine people.
Another intervention used in the study by Byrne et al. (2014) was the Mindfulness-Based Childbirth Education (MBCE). The MBCE was developed especially for the study and was applied to groups of women who could be accompanied by a support person (partner, spouse, mother, friend, among others), who also received the intervention. Table 2 specifies the techniques used in each intervention. Some techniques such as "breathing techniques" and "relaxation techniques" are often present in mindfulness exercises but were only considered when the authors directly mentioned them.

Treatment efficacy
The publications by Larsson et al. (2017) and Rondung et al. (2018) are part of the same research project. Each publication assesses the same intervention related to different outcomes. The study by Larsson et al. (2017) aimed to investigate the preferences for the delivery procedure during pregnancy and after childbirth in randomized women for treatment with iCBT or counseling for fear of childbirth (standard treatment offered for the studied population). There was a drop in the preference for cesarean section in both groups from the beginning of the investigation until the 36th week of pregnancy. However, two weeks after delivery, the preference for cesarean section increased again in both groups, with no statistically significant change over time in terms of preference for the delivery procedure. In addition, women who received standard counseling were more satisfied with their treatment than those who received iCBT.
Some information, such as the treatment protocol used in the iCBT intervention and the number of participants in the intervention group who completed the treatment, could only be found in the study by Rondung et al. (2018). In this publication, the authors performed a comparison between the efficacy of the iCBT treatment and the efficacy of standard the counseling treatment on levels of fear of childbirth. Fear of childbirth did not differ between the two treatment groups after the intervention. One year after delivery, the participants who underwent the iCBT treatment had significantly lower levels of fear of childbirth.
The iCBT treatment protocol used in both studies, as noted in the publication by Rondung et al. (2018), consisted of nine modules, one of which was applied in postpartum follow-up. Of the 127 women allocated to the group that received the intervention, only 13 completed the first five modules. More than half of the participants (53%) completed only the first module. Therefore, poor adherence to treatment may have considerably affected the results found, as the sample size calculation suggested a total of 200 participants (100 per group) to detect a 20% reduction in fear of childbirth, with a power of 0.80 and a significance level of 5%. Thus, the result presented by Rondung et al. (2018) is difficult to interpret, given the poor adherence to treatment and the wide variety of potential mediating, moderating, and confounding variables during delivery and in the postpartum period.
Larsson et al. (2017) suggest that the emotional and cognitive transformations of pregnancy may not be a favorable period for learning new coping strategies. However, it is possible that the low adherence to treatment is related to the participants' low motivation to manage the fear of childbirth. In the investigations by Byrne et al. (2014) and Nieminen et al. (2015, 2016), the studies were disseminated, and the participants volunteered spontaneously. In the studies by Larsson et al. (2017) and Rondung et al. (2018), the participants were directly asked to take part in the research.
The aim of the study by Byrne et al. (2014) was to test the feasibility and efficacy of the MBCE in promoting mental health in pregnant women. Eighteen women were recruited, and all completed the program. However, data were fully available for only 12 of these, whose information was analyzed. The "self-efficacy related to childbirth" and "fear of childbirth" variables were appropriately adjusted to the expected power of the study, as a minimum sample of four participants was required. There was a significant reduction in fear of childbirth after the treatment, with a large effect size (Cohen's d=1.71), as well as a significant increase in self-efficacy related to childbirth, also with a large effect size (Cohen's d=-1.91). The absence of a control group and the small sample used are some of the factors that make it impossible to attribute the results observed to the MBCE intervention. However, the very large effect sizes associated with improvements in self-efficacy and fear of childbirth suggest that these effects may be related in some way to the intervention and not to random effects or natural processes such as regression to the mean (Byrne et al., 2014).
The study by Uçar and Golbasi (2018) aimed to determine the effect of a CBT-based educational program on fear of childbirth. A total of 111 participants were selected, of which 52 were part of the intervention group and 59 of the control group, not receiving any type of treatment. As stated by the authors, at the end of the study, the birth of all women was monitored. The first author not only observed all deliveries, but actively participated in the delivery of women who were part of the intervention group, reminding them of the information received during the program and offering them support to apply the learned pain coping methods (Uçar & Golbasi, 2018).
According to the authors, labor pain decreased, the second stage of labor was shorter, and birth was more satisfactory for the group that received the intervention than for the control group (p<0.05). The effect size was not informed but it was calculated from the data provided by the authors: mean, standard deviation, and number of women in each group. The magnitude of the difference between the groups after the intervention was large for labor pain (Cohen's d=1.19), medium for the duration of the second stage of labor (Cohen's d=0.48), and medium for birth-related satisfaction (Cohen's d=0.63).
The first author's intervention during labor makes it difficult to attribute these results to the CBT-based educational program. Therapeutic intervention during labor is not part of CBT sessions, which considerably increases confounding variables. In the end, the authors found that fear of childbirth decreased in the intervention group and increased in the control group (p<0.001). The effect size was not informed either but, when calculated, it was large (Cohen's d=1.03).
The studies by Nieminen et al. (2015, 2016) are also part of the same research project. The study aimed to assess the feasibility of iCBT for the treatment of women with severe fear of childbirth (W-DEQ ≥85). The women were recruited through a website that explained the project and through which they could register for participation. Of the 42 women who registered on the site, 30 completed the registration form and met the research inclusion criteria. Of these, 15 completed all eight treatment modules established by the project. In the 2015 study, women's narratives about the impending delivery were collected at two moments (before treatment and eight weeks after treatment) and then were analyzed. To collect the narratives, the women were asked to perform a visualization exercise in which they should imagine and describe specific situations related to childbirth. The data collected before and after treatment were analyzed separately through thematic analysis.
Before treatment, women mainly reported feelings of anxiety, uncertainty, loneliness, hopelessness, lack of self-confidence, and use of avoidance strategies as ways of coping. The partner was associated with an idea of instability, while professionals were perceived as not very attentive or helpful. After the treatment, the women reported a mixture of doubt and hope, and a vision of themselves as active and prepared subjects. The partner also came to be seen as an active person and a supportive figure, just as professionals came to be seen as present, helpful, and available.
As described by Nieminen et al. (2015), the material collected before and after the intervention was analyzed separately and, thus, there was no comparison between the before and the after for each individual. Instead, an assessment of the main thematic domains presented was carried out. To avoid a social desire bias, the participants had contact with the therapist only through the internet. In addition, the imaginative exercise performed after the treatment took place at a time when the participants were no longer in virtual contact with the therapist. The study was reported as a descriptive and exploratory research and, therefore, it is not possible to assert causality between the therapy and the results found. Even so, it proves to be relevant for advancing new investigations.
The 2016 study, on the other hand, contains a quantitative analysis in which fear of childbirth was assessed before treatment, during treatment, and after the baby's birth. Fear of childbirth assessed before treatment and in the last week of treatment before childbirth decreased significantly (p<0.0005) and the effect size found was large (Cohen's d=0.95). According to the authors, Bonferroni's post hoc correction revealed that the decrease started after the third module of the treatment, which corresponds to the introduction of exposure tasks (Nieminen et al., 2016).
Of the 24 women who could be contacted for postpartum follow-up, 22 were satisfied with the intervention program and its ability to help them during pregnancy and childbirth. Therefore, it was concluded that the level of fear of childbirth measured with the W-DEQ is reduced when a group of motivated nulliparous women are treated with iCBT. However, this is a pre-experimental study, and the results need to be confirmed by randomized clinical trials.
Discussion
From the analysis of the studies presented, it was not possible to reach a conclusion about the efficacy of CBT in reducing fear of childbirth. However, as CBT has been shown to be so effective in the treatment of anxiety disorders (Olatunji et al., 2010), further studies deserve to be carried out. The establishment of an effective treatment to reduce the fear of childbirth could benefit the care offered to Brazilian pregnant women. The absence of specific guidelines for the management of fear of childbirth is serious, considering the association between fear of childbirth and cesarean section surgery (Leal et al., 2012; Pereira et al., 2011). Thus, offering consistent and scientific evidence-based support for the treatment of fear of childbirth, even if fear is not perceived as phobic, seems to be an important public health issue, as it addresses the high rates of elective cesarean sections.
In Brazil, standard care for low-risk prenatal care recommends that, in the third trimester, women be informed about the different stages of the evolution of pregnancy and childbirth: contractions, dilation, loss of the mucous plug, pre-labor rupture of membranes, and the postpartum period (Brasil, 2012). In addition, it is recommended that the primary health care professional prepare the pregnant woman for vaginal birth, help reduce her anxiety, insecurity, and fear of childbirth, pain, birth-related health problems to the baby, among other emotional issues (Brasil, 2012). Despite the recommendations for attentive listening and welcoming by the health professional, there is no objective recommendation on how this aid should be implemented.
Due to the relevance of the topic, Swedish researchers have shown great interest in defining, measuring, and treating fear of childbirth. The iCBT intervention used by Larsson et al. (2017) and Rondung et al. (2018) was inspired by the unified protocol for transdiagnostic treatment of emotional disorders, previous iCBT manuals for anxiety problems, and the third wave of CBT treatments. The use of the transdiagnostic protocol is coherent, since the fear of childbirth is still in the process of definition and seems to be associated with both anxiety and depression (Rondung et al., 2016).
The protocols used in the six previously addressed studies refer to different cognitive and behavioral techniques. Perinatal education is one of them and it seems to be of great importance for the woman to have knowledge of the physiology of pregnancy and childbirth, to know her own body's capacity to deal with labor and to confront myths through the acquisition of evidence-based knowledge. Of the studies presented, the articles by Larsson et al. (2017) and Rondung et al. (2018) are the only ones whose protocol does not directly mention perinatal education. Perinatal education has the potential to help manage dysfunctional beliefs about childbirth by providing useful material for the presentation of evidence for and against it, facilitating cognitive restructuring.
Another widely used technique was exposure, as observed in the studies by Nieminen et al. (2015, 2016), Larsson et al. (2017), and Rondung et al. (2018), seeming to be especially important in the study by Nieminen et al. (2016). This relevance is consistent with studies related to the treatment of specific phobias and it is worth emphasizing that the studies by Nieminen et al. (2015, 2016) were the only ones to use the identification of severe fear of childbirth in the participants in the inclusion criteria, which may be closer to the intensity of fear related to a specific phobia.
According to the American Psychological Association (APA, 2016), specific phobias are maintained due to the avoidance of the phobic stimulus that makes the individual not have the opportunity to develop tolerance to their own fear. By exposing themselves, individuals have the opportunity to observe that their physiological sensations decrease over time and that the feared results do not materialize or are not as bad as imagined (APA, 2016). Avoidance can occur by non-insertion or incomplete insertion into a situation, using resources as distraction, for example (APA, 2016). Thus, exposure therapies are designed to encourage the individual to engage in feared situations (in vivo or through imagination exercises) and try to stay in those situations (APA, 2016). In the case of childbirth-related fear, exposure techniques may include listening to other women's reports of childbirth, watching childbirth movies, or watching childbirth-related images (Nieminen et al., 2016; Rondung et al., 2018).
Mindfulness or meditation training was present in five of the six studies presented. Mindfulness has already been identified as an option for the treatment of chronic pain (Kabat-Zinn et al., 1986) and its benefits have the potential to be expanded into childbirth as well. The feeling of being overwhelmed by pain, the fear of not being able to cope with pain, and the fear of losing control and not performing well are frequently reported in relation to labor (Hofberg & Ward, 2003; Hughes et al., 2009; Rondung et al., 2016; Pereira et al., 2011). Hughes et al. (2009) suggest that meditative practices can help women to connect with the present moment and become aware of bodily sensations. Thus, it is expected that such practices help in coping with the intense sensations of labor without judgment or self-depreciation if the woman chooses analgesia (Hughes et al., 2009).
The study by Larsson et al. (2017) and the one by Rondung et al. (2018) also directly established the restructuring of catastrophic cognitions as a treatment strategy. According to Rondung et al. (2016), the cognitive concepts of self-efficacy, intolerance to uncertainty, and pain catastrophizing seem to be relevant for understanding the fear of childbirth. Gatchel et al. (2007) define pain catastrophizing as a negative and exaggerated orientation towards the current or expected pain experience. According to the authors, cross-sectional studies have shown that catastrophizing is associated with increased pain and psychological and physical dysfunction in clinical and non-clinical populations. Fear avoidance models are multifaceted and have affective (fear) and behavioral (avoidance) components; however, cognitions are identified as the core determinants of entering a negative pain cycle (Gatchel et al., 2007). Therefore, the CBT treatment seems to be a coherent therapeutic choice, through which beliefs related to catastrophizing can be confronted.
As for self-efficacy, the study by Byrne et al. (2014) suggests a large effect on increased self-efficacy, possibly related to the MBCE intervention. According to Bandura (1994), perceived self-efficacy is defined as the beliefs that a person has about their ability to perform as expected in activities that influence significant events in their lives. The author highlights that a strong perception of efficacy increases personal well-being in different ways. People with high confidence in their abilities face difficulties as challenges to be overcome, instead of seeing them as threats to be avoided (Bandura, 1994).
Furthermore, it is common for physiological reactions to stress to be interpreted as signs of poor performance, and the restructuring of distorted interpretations about the physiological state itself is one of the ways to promote the perception of self-efficacy (Bandura, 1994). Thus, more important than the intensity of emotional and physical reactions is how they are interpreted (Bandura, 1994). Therefore, mindfulness practices play an important role in the observation of bodily sensations and emotions without judgment, which would be directly related to the perception of self-efficacy as found by Byrne et al. (2014).
It is possible that CBT-based treatment protocols for fear of childbirth will be more effective if adapted to the social and cultural context of the countries in which they will be applied. None of the studies presented in this research questioned the universality of the protocols used. In Brazil, as already mentioned, due to the high rates of obstetric violence and cesarean section surgeries, the fear of being the victim of an unnecessary intervention (such as routine episiotomy or use of synthetic oxytocin) would not characterize a cognitive distortion, for example. Thus, interventions applied in Brazil could assess the benefits of problem-solving techniques, which were not addressed in the studies presented.
For women cared for in the public health system, there is no guarantee that childbirth assistance will be offered by a health professional they trust, as the assistance is provided by the medical team on duty. Thus, the Delivery and Birth Plan (Suárez-Cortés et al., 2015) can be an important option for women to assertively communicate what they expect from the care they will receive. The Delivery and Birth Plan can be prepared by the woman after receiving information about her pregnancy and childbirth. In this document, the woman begins to register which alternatives within the spectrum of good practices, under normal conditions, best contemplate her desires, expectations, values, and needs. The document is intended to guide the health care provided throughout the birth process (Suárez-Cortés et al., 2015) and encourages greater confidence and a sense of control related to childbirth. The perception of being in control of herself, of her body, and of the health care professionals' actions over her body are positively related to greater satisfaction with childbirth (Green, 1990).
Briefly, in this review, the studies that had the randomized clinical trial as a design (Larsson et al., 2017; Rondung et al., 2018) were hampered by sample losses and did not reach the expected results. This difficulty in adherence to treatment puts the efficacy of the iCBT intervention at risk for the studied population. The study by Uçar and Golbasi (2018) pointed out some benefits of the CBT-based educational program carried out in groups, but the methodological considerations highlighted make the results difficult to be interpreted. The studies by Byrne et al. (2014) and Nieminen et al. (2015, 2016) do not allow a causal attribution between the proposed treatment and the improvement in fear of childbirth but suggest possible benefits of CBT interventions for pregnant women.
It is important to emphasize that the lack of evidence-based information about childbirth, a medicalizing stance that reinforces the imbalance in the power relationship between the obstetric team and the woman, and the acquisition of tragic information about labor facilitate the perception of childbirth as a dangerous event (Melender, 2002; Pereira et al., 2011; Striebich et al., 2018). In this case, CBT could help to build a more realistic view of childbirth (Nieminen et al., 2015), as it is an approach that helps developing a mindset based on facts and evidence (Beck, 2007). However, while the reality of obstetric care is based on the lack of information offered to the woman, absence of an empathetic listening to the mother's needs and practice of obstetric violence, the fear related to childbirth will be structurally based.
Fear of childbirth is also related to each woman's cognitions and life experiences. Therefore, therapeutic techniques such as cognitive restructuring, exposure, and mindfulness prove to be relevant for the development of a less catastrophic perception of childbirth and for the development of greater confidence in their own coping skills in labor. We suggest that future studies investigate the efficacy of each of these techniques in reducing the fear of childbirth individually. Within the limitations of this systematic review, which include its descriptive and exploratory character, it is concluded that CBT is an intervention with potential benefit to reduce fear of childbirth. However, new randomized clinical trials are needed so that CBT can be considered effective in treating this fear.
References
American Psychological Association - APA. Division 12. (2016). Exposure therapies for specific phobias status: strong research support. https://www.div12.org/treatment/exposure-therapies-for-specific-phobias/ [ Links ]
Areskog, B., Uddenberg, N., & Kjessler, B. (1981). Fear of childbirth in late pregnancy. Gynecologic and Obstetric Investigation, 12(5),262-266. https://doi.org/10.1159/000299611 [ Links ]
Bandura, A. (1994). Self-efficacy. In V. S. Ramachaudran (Ed.), Encyclopedia of human behavior (Vol. 4, pp. 71-81). Academic Press. [ Links ]
Beck, J. S. (2007). Terapia cognitiva: Teoria e prática. Artmed. [ Links ]
Berger, T. (2016). Intervenções autoguiadas baseadas na internet: Uma entrevista com o Dr. Thomas Berger [Entrevista concedida a Rodrigo T. Lopes]. Revista Brasileira de Terapias Cognitivas, 12(1),57-61. https://doi.org/10.5935/1808-5687.20160009 [ Links ]
Bewley, S., & Cockburn, J. (2002). Responding to fear of childbirth. The Lancet, 359(9324),2128-2129. https://doi.org/10.1016/S0140-6736(02)09113-4 [ Links ]
Brasil. (2012). Cadernos da atenção básica: atenção ao pré-natal de baixo risco. Ministério da Saúde, Secretaria de Atenção à Saúde, Departamento de Atenção Básica. http://bvsms.saude.gov.br/bvs/publicacoes/cadernos_atencao_basica_32_prenatal.pdf [ Links ]
Byrne, J., Hauck, Y., Fisher, C., Bayes, S., & Schutze, R. (2014). Effectiveness of a mindfulness-based childbirth education pilot study on maternal self-efficacy and fear of childbirth. Journal of Midwifery & Women's Health, 59(2),192-197. https://doi.org/10.1111/jmwh.12075 [ Links ]
Gatchel, R. J., Peng, Y. B., Peters, M. L., Fuchs, P. N., & Turk, D. C. (2007). The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychological Bulletin, 133(4),581-624. https://doi.org/10.1037/0033-2909.133.4.581 [ Links ]
Ghazaie, M., Davoodi, I., Neysi, A., Mehrabizadeh, H. M., & Bassak Nejad, S. (2016). The effectiveness of cognitive-behavioral therapy on fear of childbirth, fear of pain, self-efficacy of childbirth and tendency to cesarean in nulliparous women. The Iranian Journal of Obstetrics, Gynecology and Infertility, 19(31),1-12. https://doi.org/10.22038/ijogi.2016.7989 [ Links ]
Green, J. M. (1990). "Who is unhappy after childbirth?": Antenatal and intrapartum correlates from a prospective study. Journal of Reproductive and Infant Psychology, 8(3),175-183. https://doi.org/10.1080/02646839008403622 [ Links ]
Hofberg, K., & Brockington, I. (2000). Tokophobia: An unreasoning dread of childbirth: A series of 26 cases. British Journal of Psychiatry, 176(1),83-85. https://doi.org/10.1192/bjp.176.1.83 [ Links ]
Hofberg, K., & Ward, M. R. (2003). Fear of pregnancy and childbirth. Postgraduate Medical Journal, 79(935),505-510. https://doi.org/10.1136/pmj.79.935.505 [ Links ]
Hughes, A., Williams, M., Bardacke, N., Duncan, L. G., Dimidjian, S., & Goodman, S. H. (2009). Mindfulness approaches to childbirth and parenting. British Journal of Midwifery, 17(10),630-635. https://doi.org/10.12968/bjom.2009.17.10.44470 [ Links ]
Kabat-Zinn, J., Lipworth, L., Burncy, R., & Sellers, W. (1986). Four-year follow-up of a meditation-based program for the self-regulation of chronic pain: Treatment outcomes and compliance. The Clinical Journal of Pain, 2(3),159-774. https://doi.org/10.1097/00002508-198602030-00004 [ Links ]
Larsson, B., Karlström, A., Rubertsson, C., Ternström, E., Ekdahl, J., Segebladh, B., & Hildingsson, I. (2017). Birth preference in women undergoing treatment for childbirth fear: A randomised controlled trial. Women and Birth, 30(6),460-467. https://doi.org/10.1016/j.wombi.2017.04.004 [ Links ]
Leal, M. C., Torres, J. A., Domingues, R. M. S. M., Theme Filha, M. M., Bittencourt, S., Dias, M. A. B., Pereira, M. N., Viellas, E. F., Diniz, C. S. G., d'Orsi, E., Silva, A. A. M., Pereira, A. P. E. Bastos, M. H., Moreira, M. E. L., Lansky, S., & Gama, S. G. N. da (2012). Nascer no Brasil: Sumário executivo temático da pesquisa. CCI/ENSP. http://www.ensp.fiocruz.br/portal-ensp/informe/site/arquivos/anexos/nascerweb.pdf [ Links ]
Melender, H.-L. (2002). Experiences of fears associated with pregnancy and childbirth: A study of 329 pregnant women. Birth: Issues in Perinatal Care, 29(2),101-111. https://doi.org/10.1046/j.1523-536X.2002.00170.x [ Links ]
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G., The PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. PLoS Medicine, 6(7),1-6. https://doi.org/10.1371/journal.pmed.1000097 [ Links ]
Nieminen, K., Andersson, G., Wijma, B., Ryding, E.-L., & Wijma, K. (2016). Treatment of nulliparous women with severe fear of childbirth via the Internet: A feasibility study. Journal of Psychosomatic Obstetrics & Gynecology, 37(2),37-43. https://doi.org/10.3109/0167482X.2016.1140143 [ Links ]
Nieminen, K., Malmquist, A., Wijma, B., Ryding, E.-L., Andersson, G., & Wijma, K. (2015). Nulliparous pregnant women's narratives of imminent childbirth before and after internet-based cognitive behavioural therapy for severe fear of childbirth: A qualitative study. BJOG: An International Journal of Obstetrics & Gynaecology, 122(9),1259-1265. https://doi.org/10.1111/1471-0528.13358 [ Links ]
Nunes, R. D., Traebert, E., Seemann, M., & Traebert, J. (2021). Tokophobia Assessment Questionnaire: A new instrument. Brazilian Journal of Psychiatry, 43(1),112-114. https://doi.org/10.1590/1516-4446-2020-1252 [ Links ]
O'Connell, M. A., Leahy-Warren, P., Khashan, A. S., Kenny, L. C., & O'Neill, S. M. (2017). Worldwide prevalence of tocophobia in pregnant women: Systematic review and meta-analysis. AOGS, Acta Obstetricia et Gynecologica Scandinavica, 96(8),907-920. https://doi.org/10.1111/aogs.13138 [ Links ]
Olatunji, B.O., Cisler J. M., & Deacon B. J. (2010). Efficacy of cognitive behavioral therapy for anxiety disorders: A review of meta-analytic findings. Psychiatric Clinics of North America, 33(3),557-577. https://doi.org/10.1016/j.psc.2010.04.002 [ Links ]
Pereira, R. R., Franco, S. C., & Baldin, N. (2011). Pain and the protagonism of women in parturition. Revista Brasileira de Anestesiologia, 61(3),382-388. https://doi.org/10.1590/S0034-70942011000300014 [ Links ]
Ryding, E. L. (2017). Medo do parto: Definição e diagnóstico. In U. Björklund & E. L. Ryding (Ed.), Medo do parto (pp. 7-14). Sociedade Sueca de Obstetrícia e Ginecologia. https://www.sfog.se/natupplaga/1005623_A2fb46497-d45b-466d-8126-c58e99fe856d.pdf [ Links ]
Rondung, E., Ternström, E., Hildingsson, I., Haines, H. M., Sundin, Ö., Ekdahl, J., Karlström, A., Larsson, B., Segeblad, B., Baylis, R., & Rubertsson, C. (2018). Comparing internet-based cognitive behavioral therapy with standard care for women with fear of birth: Randomized controlled trial. JMIR Mental Health, 5(3),1-16. https://doi.org/10.2196/10420 [ Links ]
Rondung, E., Thomtén, J., & Sundin, Ö. (2016). Psychological perspectives on fear of childbirth. Journal of Anxiety Disorders, 44,80-91. https://doi.org/10.1016/j.janxdis.2016.10.007 [ Links ]
Sampaio, R. F., & Mancini, M. C. (2007). Estudos de revisão sistemática: Um guia para síntese criteriosa da evidência científica. Brazilian Journal of Physical Therapy, 11(1),83-89. https://doi.org/10.1590/S1413-35552007000100013 [ Links ]
Souza, A. S. R., Amorim, M. M. R., & Porto, A. M. F. (2010). Condições frequentemente associadas com cesariana, sem respaldo científico. FEMINA, 38(10),505-516. http://files.bvs.br/upload/S/0100-7254/2010/v38n10/a1708.pdf [ Links ]
Striebich, S., Mattern, E., & Ayerle, G. M. (2018). Support for pregnant women identified with fear of childbirth (FOC)/tokophobia: A systematic review of approaches and interventions. Midwifery, 61,97-115. https://doi.org/10.1016/j.midw.2018.02.013 [ Links ]
Suárez-Cortés, M., Armero-Barranco, D., Canteras-Jordana, M., & Martínez-Roche, M. E. (2015). Use and influence of delivery and birth plans in the humanizing delivery process. Revista Latino-Americana de Enfermagem, 23(3),520-526. https://doi.org/10.1590/0104-1169.0067.2583 [ Links ]
Ternström, E. (2018). Identification and treatment of women with a fear of birth. [Unpublished Doctoral Thesis]. Universidade de Uppsala. http://uu.diva-portal.org/smash/record.jsf?pid=diva2%3 A1196389&dswid=4456 [ Links ]
Uçar, T., & Golbasi, Z. (2018). Effect of an educational program based on cognitive behavioral techniques on fear of childbirth and the birth process. Journal of Psychosomatic Obstetrics & Gynecology, 40(2)1-19. https://doi.org/10.1080/0167482X.2018.1453800 [ Links ]
Vandenberghe, L., & Sousa, A. C. A. (2006). Mindfulness nas terapias cognitivas e comportamentais. Revista Brasileira de Terapias Cognitivas, 2(1),35-44. http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1808-56872006000100004 [ Links ]
Venturi, G., Bokany, V., & Dias, R. (2010). Mulheres brasileiras e gênero nos espaços público e privado. Fundação Perseu Abramo & Serviço Social do Comércio. http://csbh.fpabramo.org.br/sites/default/files/pesquisaintegra.pdf [ Links ]
World Health Organization. (2015). Declaração da OMS sobre Taxas de Cesáreas. WHO. https://apps.who.int/iris/bitstream/handle/10665/161442/WHO_RHR_15.02_por.pdf?sequence=3 [ Links ]
World Health Organization. (2019). Trends in maternal mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: Executive summary. WHO. https://apps.who.int/iris/handle/10665/327596 [ Links ]
Wijma, K., Wijma, B., & Zar, M. (1998). Psychometric aspects of the W-DEQ: A new questionnaire for the measurement of fear of childbirth. Journal of Psychosomatic Obstetrics & Gynecology, 19(2),84-97. https://doi.org/10.3109/01674829809048501 [ Links ]
Zorzam, B., & Cavalcanti, P. (2016). Direitos das mulheres no parto: Conversando com profissionais da saúde e do direito (Cartilha). Coletivo Feminista de Sexualidade e Saúde. https://www.mulheres.org.br/direitos-das-mulheres-parto-com-profissionais-saude-direito/ [ Links ]
 Correspondence:
Correspondence:
Lívia Rangel de Christo Nunes
Rua São Francisco Xavier, 524, 10º andar, sala 10.009, bloco F, Maracanã
Rio de Janeiro, RJ, Brazil. CEP 20550-013
E-mail: psilivianunes@gmail.com
Received: September 30th, 2020
Accepted: August 9th, 2021











 texto em
texto em 


