Services on Demand
article
Indicators
Share
SMAD. Revista eletrônica saúde mental álcool e drogas
On-line version ISSN 1806-6976
SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. port.) vol.8 no.2 Ribeirão Preto Aug. 2012
ORIGINAL ARTICLE
Results of monitoring of users treated in the Psychosocial Care Center - Alcohol and Drugs (CAPS-AD)
Resultados del acompañamiento de los usuarios del Centro de Atención Psicosocial - Alcohol y Drogas (CAPS - AD)
Rivelilson Mendes de FreitasI; Helen Rute Rodrigues da SilvaII; Diego Santos de AraújoIII
IPhD, Adjunt Professor, Universidade Federal
do Piauí, Teresina, PI, Brazil
IIRN
IIIUndergraduate student in Nursing,
Universidade Federal do Piauí, Teresina, PI, Brazil
ABSTRACT
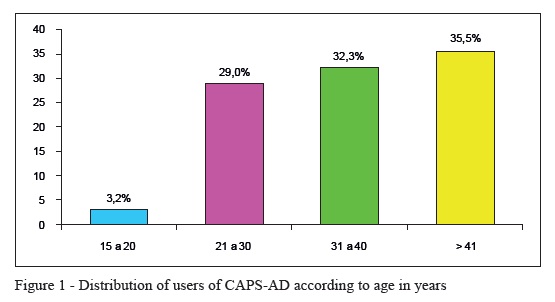
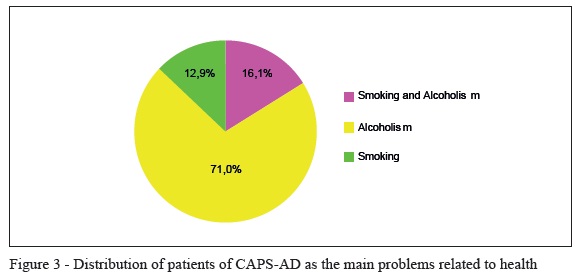
This study has drawn a line on health problems, diagnostic hypotheses, psychoactive substances used and if there is or not adherence to treatment among patients treated by the CAPS. The exploratory and descriptive research with a quantitative approach was conducted through an interview with all patients (n=31) under hospitality day at CAPS before their outpatient consultations. From all of them, 35.5% were older than 41 years, 83.9% had skin color self-reported as white and 71% were single, 74.2% had completed only primary education and 48.3% had a monthly income of up to a basic wage. The main health problem identified was alcoholism and the most common diagnostic hypothesis was smoking associated with alcoholism. Most users take their medication at the right time and do not practice self-medication.
Descriptors: Salud Pública; Epidemiología; Trastornos Mentales; Bebidas Alcohólicas; Drogas Ilícitas.
RESUMEN
El trabajo delineó los problemas de salud, las hipótesis diagnósticas, las substancias psicoactivas utilizadas y se hay o no adherencia a los tratamientos entre los pacientes atendidos por el CAPS. El estudio del tipo exploratorio descriptivo en abordaje cuantitativo fue realizado, por medio de una entrevista con todos los pacientes (n=31) en régimen de hospitalidad día en el CAPS antes de sus consultas de ambulatorio. 35,5% de los pacientes tenían edad superior a 41 años, 83,9% el color de la piel auto-referida blanca y 71% eran solteros. 74,2% tenían apenas la enseñanza fundamental y 48,3% tenían renta mensual de hasta un salario. El principal problema de salud identificado fue el etilismo y la hipótesis diagnóstica más común fue el tabaquismo asociado al etilismo. La mayoría de los usuarios administra sus medicamentos en la hora cierta y no practica automedicación.
Descriptores: Public Health; Epidemiology; Mental Disorders; Alcoholic Beverages; Street Drugs.
Introduction
Since the 80's, through the Psychiatric Reform, Brazil is building a new way of caring for patients with mental disorders, aiming at work reinvention with the development of new subjectivities, as a possibility to take responsibility for the individuals suffering, through a new paradigm centered on human care, supportive, affectionate and attempting to reconstruct the citizenship of these patients. This reform aimed at replacing the psychiatric hospitals (asylums) for new ways of care, such as day hospitals, Psychosocial Care Center (CAPS), Psychosocial Centers and others(1-2).
CAPS is a community service responsible of caring for people who suffer from mental disorders, especially chronic disorders. A few basic principles should be followed as the reception of these patients, ensuring the presence of a professional throughout the working period and to create a cozy therapeutic ambience that may include patients in the unit's activities. Furthermore, the actions of CAPS should be directed to the families and to commit to the development of social inclusion projects. It should also pay attention to case management and customize the project of each patient(3).
Studies on epidemiological and pharmacological treatments previously performed describe the main sociodemographic characteristics and also health problems and the consequences of a pharmacological treatment improperly performed by users of a Psychosocial Care Center located in the State of Ceará(3). Several other studies conducted with patients of CAPS unequivocally contribute to demonstrate the need for guidance on pathologies and pharmacological treatments for users, their families and health professionals involved in care activities at CAPS(4-5).
Currently, mental disorders generated by psychoactive substances are serious public health problems, which are often undiagnosed and improperly treated(6). Studies that focus on these disorders are intended to identify demographic variables, physiological, cultural and psychological which contribute to the use and substance dependence(6-7). Frequently, the addicts make use of various drugs, making the treatment more difficult and worsening their mental health, and may cause several other consequences such as hallucination, delirium, and other psychoses(8-9).
Given this context, this study aims to present the main data on the epidemiological profile, the main health problems, diagnostic hypotheses, the main psychoactive substances use and if there is or not adherence to treatment among patients with psychosocial disorders treated by the Psychosocial Care Center - Alcohol and Drugs (CAPS-AD) in the city of Picos, Piauí.
Material and methods
Study design
The results were obtained through an exploratory and descriptive research with a quantitative approach(10), by an interview directly with the patients for approximately 20 minutes before their outpatient consultations. During the interviews with all patients (n=31) under hospitality day at CAPS-AD in the city of Picos, Piauí, it was filled out a questionnaire with clear and objective questions. In the study it was included patients who underwent an appointment each month and those who were under hospitality day at the health service in the CAPS-AD. The interviews were conducted from April to November 2009. To avoid any methodological bias, the patients in the emergency room were not interviewed.
Study local
CAPS is a community health service of the Brazilian Unified Health System (SUS). It is a center of reference and treatment for people suffering from mental disorders, whose severity and/or persistence require intensive care, communitarian and customized(2). CAPS was established along with the Psychosocial Assistance Centers, through Ordinance SNAS No. 224(3). It is a local health center that has multidisciplinary care to a defined population and that provides intermediate care between outpatient and hospitalization in hospitality day(11-12).
CAPS aim at constituting a community service whose main role is caring for people who suffer from mental disorders, especially chronic disorders. Furthermore, the actions of CAPS should be directed to the families and to commit to the development of social inclusion projects, besides working with case management customizing the project of each patient. Among the most prevalent psychosocial disorders treated by CAPS, according to PAHO/WHO (2001), there are depressive disorders, disorders associated with the use of legal and illegal chemicals, schizophrenia, epilepsy, mental retardation and disorders of childhood and adolescence.
Data collection
Data collection of patients was performed by the students of Nursing School of the Federal University of Piauí, trained, supervised, and accomplished through direct interview with the patient for approximately 20 minutes before their consultation. During the interview it was filled out a questionnaire prepared according to the methodology described by Cipolle et al.,(10), with clear and objective questions in order to record the following information: age; self-reported skin color; marital status; education; family income; health problems; diagnostic hypotheses; the main psychoactive substances used and if there is or not adherence to treatment among patients with psychosocial disorders treated by CAPS-AD. Data on previous pathologies and diseases associated with addiction and/or chemical or physical addiction observed during consultations were analyzed and recorded directly from the medical records. We have considered as health problems self-reported by patients during interviews the factors more frequently associated during treatments, that is, alcoholism and/or smoking alone or combined with other factors.
The research protocol has accomplished the ethical principles of the Declaration of Helsinki and the rules of Resolution 196/96 of the National Health Council, and it was approved by the Ethics Committee of the Federal University of Piauí (CAAE: 0093.0.045.000-09).
Results
The studied health service refers to the Unified Health System (SUS) in the State of Piauí maintained by the Municipality of the city of Picos. Thus, these results have limitations, but they are representative as to the patients with psychosocial disorders treated in Piauí by SUS. From the 31 patients enrolled in the study, the majority is male (77.4%), 35.5% was older than 41 years (Figure 1), 83.9% was self-reported as white and 16, 1% was mulatto. As for marital status, 71% was single, 12.9% divorced, 9.7% was married and 6.4% was widowed. Those who reported having completed elementary education were 71%, 16.1% of them said they had attended secondary education and 9.7% are illiterate. The families with basic wage were 48% (Figure 2).
When asked about the number of children, 45.2% have no children, 38.6% have one or two children, and 16.1% have more than two children. With respect to type of residence, 61.3% of them have their own house, 29% live in rented house and 9.7% were unable to provide the type of property. These results make evident that due to the low education the patients work without being paid or work on family farming.
The main problem identified related to health was smoking associated with alcoholism 71% (Figure 3).
Among the diagnostic hypotheses found include alcoholism, drug addiction and smoking being alcoholism the main problem associated with smoking (45.2%, Figure 4). In turn, the higher frequency of substance addiction was associated with the use of marijuana and crack (55.5%, Figure 5).
With respect to adherence to prescribed pharmacological treatment, it was found that most patients take their medications on schedule (96.8%), however, 64.5% smoke and 22.6% drink during treatment. On the other hand, it was also detected that 93.6% do not perform self-medication and prefer medications prescribed by psychiatrists (74.2%).
Our study has also found that only a small number of patients forget to take the medicine at the right time (12.9%). And when that occurs most of them do not take the next dose (70.9%). In general, they prefer to take the medication with water (83.9%) and preferably after meals (54.8%). Another important data detected in the study was the low frequency of discontinuation of treatment after improvement (6.4%), since even with regression of signs and symptoms of mental disorders 83.9% continue making use of prescribed medication.
Discussion
The present study has identified the epidemiological profile, the main health problems, diagnostic hypotheses, the main psychoactive substances used and if there is or not adherence to treatment among patients with psychosocial disorders treated by CAPS-AD in the city of Picos, Piauí.
The age group above 40 years showed the highest prevalence among users treated at CAPS, this age group was identified in previous studies as a risk factor for the development of comorbidities(13-14). It was also observed a higher prevalence of consultations of male patients, probably because this health service deals mainly with disorders related to alcoholism and drugs addiction that are more frequent among men(15).
Mental disorders begin in adolescence, in the productive phase of life, insertion in the labor market and the emotional conflicts(16). The "mental illness" is not yet well understood by the society as a disease with a cause already well known, therefore, it has its setting based not only by biological factors, but by the determination and cultural values which results in social exclusion and isolation of these patients who do not fit within the usual standards, thus, hindering, their access to education and the establishment of a union status. These data corroborate those found in our study, since most patients do not have children nor has stable union status.
Most users has only primary education, which in most cases is incomplete, and many of them cannot read nor write correctly, which explains the high consumption of alcohol and tobacco, since the absence of knowledge of risks and consequences of the use of licit and illicit drugs can promote the use of these substances, as well as the physical and mental well-being they produce.
In the study it can be seen that most of them develop agricultural activities, has a low level of education and a household income of about basic wage. However, the type of house most frequent self-reported by patients was their own house, although it has been reported that they live with their families, since they cannot afford to keep a home.
The main problems related to health of certain patients were smoking and/or alcoholism. In turn, the diagnostic hypotheses with the highest prevalence among patients is alcoholism; alcoholism associated with drug addiction; drug addiction and chemical addiction. When they were asked about chemical addiction it was identified a high concomitant use of crack and marijuana. Among chemical addicts it was found that a small number of them do not use crack, revealing an increase in the use of this substance in our society, possibly due to its low cost and high addictive potential(17).
Although our data reveal an alarming situation regarding the use of drugs in the city of Picos, they also show that there is a demand for health care by patients and families, and that patients, most often, seek to adhere to treatment, since only 3.2 and 6.4% of these users state that they do not take the medication at the right time and that perform self-medication, respectively. Another important data observed in our study shows that there is a concern about the possible interactions between foods/nutrients with medication, since the treatments are administered one or two hours after meals with plenty of water. Although a small number of patients report not forget to take the medicine and not drink alcoholic beverages, it is important to note that even during the pharmacological treatment a significant number of users smoke, showing that it is necessary to introduce therapeutic workshops and pharmacological steering groups about the risks and consequences of use of licit and illicit drugs during treatment and for mental disorders(18).
It was also identified that patients continue the treatment even when there is a significant improvement of the signs and symptoms of mental disorders and that only take the medication prescribed by the psychiatrist. Thus, monitoring the correct treatment with psychotropic drugs aims at reducing the costs of medical care and ensures greater safety for users of CAPS. This process can be set up as being the responsible provision but the pharmacological treatment in order to achieve results that improve the quality of life of the patients(19-20).
These accompaniments are committed to reducing morbidity and mortality related to medication(21). In the absence of these, the process of healing and/or maintenance of health can be compromised, and may even lead to worsening the clinical condition(22-23), thus, generating inconvenience to the patient and losses to the health systems, with increase of cost of treatment and the number of hospitalization days of the patients.
Thus, this project had as main justification outlining necessary information for the implementation of therapeutic workshops and pharmacological steering groups, reviewing ways of approaches and treatments of mental illness at CAPS-AD in the city of Picos, since the literature emphasizes that the disease when diagnosed and treated avoids social and personal damage to the patient.
Final consideration
It is important that health professionals and the community may be able to recognize in patients with mental disorders, whole beings, worthy, with the right to liberty, physical and moral integrity, rehabilitation to work and quality of life. Within this context, CAPS has an important role, since it is the gateway to the patient's to the health care system and also has the responsibility of proposing new service strategies to increase network protection and attention to families union.
This study in quantitative approach was a direct result of the service to the users of CAPS. Considering that this is a reference institution for monitoring patients who use alcohol and drugs, there was great interest in tracing the profile of clients, so it could be able to recognize their characteristics and to identify risk factors that can be prevented or treated. The profile of users treated at CAPS is composed of adult men, with low education, single and have some activity with low payment. Most of them adhere to pharmacological treatment, do not practice self-medication and do not drink alcoholic beverages during treatment. In this CAPS it is believed to be appropriate to characterize the population and from the results to extend their actions to carry out education to users, their families and health professionals about the risks and consequences of the use of licit and illicit drugs.
References
1. Maia LC, Durante AMG, Ramos LR. Prevalência de transtornos mentais em área urbana no norte de Minas Gerais, Brasil. Rev Saúde Pública 2004;38(5):650-6. [ Links ]
2. Pelisoli CL, Moreira AK. Caracterização epidemiológica dos usuários do Centro de Atenção Psicossocial Casa Aberta. Rev. psiquiatr. Rio Gd. Sul 2005;27(3):270-7. [ Links ]
3. Oliveira CPA, Freitas RM. Instrumento Projetivo para Implantação da Atenção Farmacêutica aos Portadores de Transtornos Psicossociais: Atendidos pelo Centro de Atenção Psicossocial. SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. 2008;4(2):1-15. [ Links ]
4. Borges KD, Iodes AF, Freitas RM. Estudo do uso racional de medicamentos por usuários do Centro de Atenção Psicossocial. Rev. Bras. Farm. 2005;17:79-15. [ Links ]
5. Maia FD, Iodes AF, Freitas RM. Atenção farmacêutica aos usuários do Centro de Atenção Psicossocial VI. Rev. Bras. Farm. 2006;55: 12-16. [ Links ]
6. Passos SRL, Camacho LAB. Características da clientela de um centro de tratamento para dependência de drogas. Rev. Saúde Pública 1998;32(1):64-71. [ Links ]
7. Pinho PH, Oliveira MAR, Almeida MM. A reabilitação psicossocial na atenção aos transtornos associados ao consumo de álcool e outras drogas: Uma estratégia possível? Rev. psiquiatr. clín. 2008;35(suppl. 1):82-8. [ Links ]
8. Spricigo JS, Alencastre MB. O enfermeiro de unidade básica de saúde e o usuário de drogas – um estudo em Biguaçú-SC. Rev. Latino-Am. Enfermagem. 2004;12(spe):427-32. [ Links ]
9. Morgado AF, Coutinho ESF. Dados de epidemiologia descritiva de transtornos mentais em grupos populacionais do Brasil. Cad. de Saúde Pública 1985;1(3):327-47. [ Links ]
10. Cipolle RJ, Strand LM, Morley PC, Frakes M. Resultados del ejercicio de la Atencion Farmacéutica. Pharm Care Esp 2000;2:94-106. [ Links ]
11. Onocko-Campos RT, Furtado JP. Entre a saúde coletiva e a saúde mental: um instrumental metodológico para avaliação da rede de Centros de Atenção Psicossocial (CAPS) do Sistema Único de Saúde. Cad. Saúde Pública 2006;22(5):1053-62. [ Links ]
12. Andreoli SB, Ronchetti SSB, Miranda ALP, Bezerra CRM, Magalhães CCPB, Martin D, et al. Utilização dos Centros de Atenção Psicossocial (CAPS) na cidade de Santos, São Paulo, Brasil. Cad. Saúde Pública 2004;20(3):836-44. [ Links ]
13. Alberola GEC, Cruz ME, Cruz T. Farmacovigilancia em aténción primária: experiencia en centro de salud. Rev OFIL 1991;2:85-8. [ Links ]
14. Lima SL, Soares BGO, Mari JJ. Saúde e doença mental em Pelotas, RS: dados de um estudo populacional. Rev. Psiquiatr. Clín. 1999;26(5):225-35. [ Links ]
15. Figlie N, Fontes A, Moraes E, Payá R. Filhos de dependentes químicos com fatores de risco biopsicossociais: necessitam de um olhar especial? Rev. Psiquiatr. Clín. 2004;31(2):53-62. [ Links ]
16. Lima MCP, Menezes PR, Carandina L, Cesar CLG, Barros MBA, Goldbaum M. Transtornos mentais comuns e uso de psicofármacos: impacto das condições socioeconômicas. Rev. Saúde Pública 2008;42(4):717-23. [ Links ]
17. Fernandes LA, Philomena MSF, Leite SMS. O perfil dos pacientes com transtornos mentais atendidos em unidade de saúde 24 horas de Curitiba. Boletim de Enfermagem 2007;1:14-29. [ Links ]
18. Secretaria de Saúde do Estado do Ceará. Manual de Procedimentos de Atenção Farmacêutica da Teoria a Prática. Fortaleza: Secretaria de Saúde do Estado do Ceará, 2003. [ Links ]
19. Lopes CS, Coutinho ESF. Transtornos mentais como fatores de risco para o desenvolvimento de abuso/dependência de cocaína: estudo caso-controle. Rev. Saúde Pública. 1999;33(5):477-87. [ Links ]
20. Miranda SP, Vargas D. Satisfação de Pacientes de um Centro de Atenção Psicossocial Álcool e Drogas com o Atendimento do Enfermeiro. SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. 2009;5(2):1-15. [ Links ]
21. Marcelo PA. Aplicação da versão em português do instrumento de avaliação de qualidade de vida da Organização Mundial da Saúde (WHOQOL-100). Rev. Saúde Pública. 1999;33(2):198-205. [ Links ]
22. Silva RF, Freitas RM. Investigação sobre o uso racional de medicamentos no município de Quixadá. Revista Eletrônica de Farmácia 2008;3:28-32. [ Links ]
23. Afonso GMT, Puerta FAMC. Auto valoración social, economica y profesional del farmacéutico comunitário. Rev OFIL 1991;5:298-303. [ Links ]
Received: Feb. 5th 2010 Correspondence
Correspondence
Rivelilson Mendes de Freitas
Av. Cícero Eduardo, s/n
Bairro: Junco
CEP: 64607-675, Picos, PI, Brasil
E-mail: rivelilson@pq.cnpq.br
Accepted: Jan.
15th 2013











 text in
text in 

