Serviços Personalizados
artigo
Indicadores
Compartilhar
SMAD. Revista eletrônica saúde mental álcool e drogas
versão On-line ISSN 1806-6976
SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. port.) vol.8 no.2 Ribeirão Preto ago. 2012
ORIGINAL ARTICLE
Alcoholism in the midwest region of the state of Minas Gerais: sociodemographic, clinical profiles and geographical distribution
Alcoholismo en la región centro este de Minas Gerais: perfil socio-demográfico, clínico y distribución geográfica
Richardson Miranda MachadoI; Moacyr Lobo da Costa JúniorII
IPhD, Adjunt Professor, Universidade Federal
de São João del-Rei, São João del-Rei, MG, Brazil
IIPhD, Associate
Professor, Escola de Enfermagem de Ribeirão Preto, Universidade de São Paulo,
WHO Collaborating Centre for Nursing Research Development, Ribeirão Preto, SP,
Brazil
ABSTRACT
This is a retrospective and exploratory research, conducted at Clínica São Bento Menni aiming at to know the sociodemographic and clinical profiles of inpatients due to alcoholism and to identify the geographic distribution of the cases. There was a predominance of male individuals; from 41 to 50 years old; white; married; with fundamental level; self-employed; diagnosis of dependence syndrome; discharged from hospitals and referred for Psychosocial Care Centers. The municipalities of Leandro Ferreira with 2955 inhabitants and Araújos with 7201 inhabitants had the highest rate of hospitalization because of alcoholism.
Descriptors: Alcoholism; Epidemiology; Mental Health.
RESUMEN
Estudio retrospectivo y exploratorio, realizado en la Clínica São Bento Menni, con los objetivos: conocer el perfil socio-demográfico y clínico de los pacientes internados en ocurrencia del alcoholismo e identificar la distribución geográfica de los casos. Hubo una predominancia del sexo masculino; de la banda etaria de 41 a 50 años; del cutis blanca; de los casados; del nivel fundamental; de los trabajadores autónomos; de diagnósticos de síndrome de dependencia; de alta médica hospitalaria y de encaminamientos para los Centros de Atención Psicosocial. Los municipios de Leandro Ferreira con 2955 habitantes y Araújos con 7201 habitantes, tuvieron la mayor tasa de internación por alcoholismo.
Descriptores: Alcoholismo; Epidemiología; Salud Mental.
Introduction
Nowadays the use of alcohol is characterized as a social phenomenon that represents a serious worldwide public health problem, a fact that has aroused the health authorities' attention of several countries.
Alcoholism is, thus, considered one of the most serious worldwide public health problems. Its main characteristics, according to the World Health Organization (WHO), are the physical and psychological changes resulting from the ingestion of alcohol with the appearing of behavioral reactions that include compulsion for continuous or periodic ingestion of the substance. And the main purpose of its consumption is to experience the physical effects caused by the alcohol and to avoid the discomfort caused by its lack(1).
In Brazil, a nationwide survey showed that 12.3% of people aged between 12 and 65 years are dependent on alcohol, with a prevalence of 17.1% of males and 5.7% of female(2).
These percentages should be taken into account, since the abuse consumption causes numerous negative consequences for health and for quality of life of the individual and the population, contributing to the emergence of morbidities that cause death and functional limitations. As psychoactive substance, alcohol produces depressant effect or euphoric, and its consumption causes behavioral changes (e.g., aggressiveness, family conflicts, urban and domestic violence), as well as clinical problems (e.g., arterial hypertension, gastritis, cirrhosis, malnutrition) and psychological (e.g., depression and mental disorders), which also contribute to automobile accidents and absenteeism at work(3).
Alcoholism is a problem for the entire society and, especially, for patients who are, every day, in health services, since primary care to the hospital, due to the urgent need for treatment and chronicity of cases. However, they eventually fail into dependence due to lack of infrastructure of public health.
Thus, as the Unified Health System (SUS) has sought in a technical way to face the alcoholism problem and psychiatric hospitalizations, there is an urgent need to understand the sociodemographic and clinical profiles of inpatients as a result of alcoholism during the 28 years of Clínica São Bento Menni (CSBM), the only reference to psychiatric hospitalizations for the Midwest region of Minas Gerais, as well as to identify the geographical distribution of the cases. The information is crucial for the establishment of measures of treatment, monitoring and prevention, more specific and effective.
Certainly, before such information, it is possible through restructuring of Psychiatry, to turn effective the actions of Psychosocial Care Centers (CAPS) in the Midwest region of Minas Gerais, directing their work and guiding them with public health policies.
Methodology
This is a retrospective and exploratory research held at CSBM, which is a psychiatric hospital, a tertiary care center, philanthropic, medium-size hospital, with total installed capacity of 120 beds. It is considered the only reference center of the Unified Health System (SUS) for psychiatric hospitalizations in the Midwest region of Minas Gerais, caring for patients with acute and chronic mental disorders for propedeutics, psychiatric and outpatient treatments. It has diverse patients, with 85% of them from SUS, mostly patients from cities near Divinópolis/Minas Gerais, place of CSBM, located in the Midwest of Minas Genais.
The CSBM develops through its Hospitalizations System (SIH) the register, monitoring and archiving of information regarding admissions through medical records stored on its Medical Record and Statistics Sector (SAME). In this aspect, it developed an electronic system for data collection and admissions recording beginning in 1995, and it has electronic records of all existing data from the hospital since 1980, as manuscript format in its SAME.
This study was, therefore, done from the collection of information in SIH/CSBM database, with the approval by the Ethics Committee of the University of São Paulo (USP), which, from the data collected it was built a new database with information about alcoholism patients.
The criteria chosen were: 1) inpatients due alcoholism in CSBM, from October 20, 1980 (opening of the clinic) to December 31, 2008; 2) inpatients in CSBM for over 24 hours; and 3) inpatients who were assisted from admission until discharge or transfer. The exclusion criteria were: patients with incomplete and/or misconceptions data that could not be completed and/or corrected.
Thus, when the information were extracted from SIH, the 50 groupings of information presented by the item "Access", the admissions were transformed into variables in nominal and ordinal categories, which were inserted in the software Microsoft Excel - version 2003 and Statistical Package for the Social Sciences (SPSS) - version 13.0. The information was inserted twice, verifying, thus, typographical errors. The statistical programs have enabled the treatment of collected variables and a descriptive presentation of the results and through figures presentation.
Among the 25 variables generated, three - psychopharmacology, psychotherapy and occupational therapy - were excluded from the study findings. The first was excluded due to range and complexity of the data related to psychotropic drugs, which deserve a specific study. The second and third were excluded due to non-fulfillment of such information in the SIH of CSBM.
Thus, among the 22 final variables, 19 have made possible sociodemographic outcomes and three, clinical outcomes. All of them are related to the first admission of each patient (n=2203).
They are: number of hospitalizations; gender; age; skin color; marital status; education; profession; city of reference; origin of the patient; followed for hospitalization; voluntary or involuntary hospitalization; diagnosis of the first hospitalization; medical insurance; first year of hospitalization; restriction of visits; license restriction; restriction of rehospitalization; discharge restriction; duration of first hospitalization; type of discharge; diagnosis of the first hospitalization and referral service.
Results and Discussion
From October 20, 1980 (opening of the CSBM) to December 31, 2008, 28,078 patients were hospitalized, and 2,203 of these patients were admitted because of alcoholism.
Regarding the number of hospitalizations, it was observed that the highest number of alcoholic patients, 1796 (81.5%) were admitted one time, 303 (13.8%) were admitted two times and 104 (4.7%) were admitted three or more times at CSBM.
As for the patients' gender, there was a predominance of males, with 1815 (82.4%) cases, and 388 (17.6%) of females, resulting in a ratio of 4.6 males to every female.
The prevalence of alcoholism in males is in agreement with the vast majority of national and international studies conducted in psychiatric services. In this sense, we can cite the study(4) done with 8589 interviewed people in 107 Brazilian cities, with more than 200,000 inhabitants, which found a prevalence of alcohol dependence of 17.1% among males and 5.7% among females.
Regarding the age of the higher number of patients, 715 (32.5%) were from 41 to 50 years old, followed by 667 (30.2%) from 31 to 40 years old; 332 (15.1%) from 51 to 60 years old; 330 (15%) between 21 to 30 years old; 94 (4.3%) between 61 to 70 years old, 34 (1.5%) from 10 to 20 years old and 31 (1.4%) over 70 years old. The mean age was 36.6 years old.
The prevalence of patients from 41 to 50 corresponds to what was observed by several authors who have conducted studies on hospital services such as the CSBM. More people from 41 to 50 years consist with the manifestation stage of chronic symptoms presented by patients regarding alcohol abuse for several years(4).
Regarding skin color, the majority of patients 1901 (86.3%) were classified as white, and the others were almost equally distributed with 163 (7.4%) as afro-descendants and 133 (6%) as mulattos. The predominance of white patients, followed by afro-descendants, mulattos and oriental resembles other studies(5-6).
When evaluating the marital status we have found a small predominance of 1048 (47.6%) married patients, followed by 918 (41.7%) single patients; 158 (7.2%) divorced and 79 (3.6%) widowed.
In a study(7) conducted with a sample of 300 alcoholic patients, it was found that 48.7% of patients were married. These patients have presented a better stability level and/or responsibility in the treatment and adhering it for longer.
On the education level there was a prevalence of 1073 (48.7%) patients with primary education; followed by 816 (37%) with secondary education; 187 (8.5%) semiliterate; 63 (2,9%) with incomplete higher education; 39 (1.8%) with a college degree and 25 (1.1%) illiterate.
The results of the study(8) also show that the lower the education and individual income the higher risk for hospitalization for alcoholism and for non-adherence to treatment, resulting in a longer hospitalization. In addition, the data have showed the severe social and economic situation of the majority of alcoholic inpatients in surveyed health services.
In relation to the occupation of 2203 patients, were found 1172 records of different professional activities reported at the hospitalization moment. Through this multiplicity of occupations, it was not possible the study and comparison of information about their jobs. Thus, we performed the codification of declared occupations following the specifications and groupings of the Brazilian Classification of Job Occupations.
Thus, it was found that most of the patients, 591 (26.8%) are self-employed, trade sellers in shops and markets. Therefore, followed by a significant number of agricultural, forestry, hunting and fishing workers (376, 17.1%) and production workers of industrial goods and services, metallurgy and civil construction (327, 14.8%).
There is also a considerable number of unemployed, 235 (10.7%); retired 201 (9.1%); mid-level technicians, 136 (6.2%); maintenance and repair workers, 107 (4.9%); production workers of industrial goods and services (food and textiles), 94 (4.3%); senior members of the government, leaders of public interest organizations and companies and managers, 47 (2.1%); science and arts professionals, 44 (2.1%); military forces, police and firefighters, 24 (1.1%) and administrative workers, 21 (1%).
About the patients' origin for hospitalization, the largest number (943, 42.8%) was taken to the CSBM by their own families, which leads us to consider the fact that this same number is equal to the total number of hospitalizations paid by health insurance (530, 24%) and particular (413, 18.7%), which implies a greater facility for hospitalization.
It is also worrying the large number (455, 20.6%) of patients from Psychosocial Care Center for hospitalization, a fact contrary to the philosophy of these services designed to end the stigma of hospitalization. The remaining 247 (11.2%) patients came from particular doctors; 246 (11.1%) from the Regional Emergency; 162 (7.3%) because of Court Order and 150 (6.8%) from Clinical Hospital.
It is also appropriate to point out the large number of admissions (1232, 55.9%) financed by SUS (Brazilian Health System). However, because it is a philanthropic hospital in which 80% of their beds (96 from 120) are intended to SUS, it is expected this prevalence.
Regarding if the patient was accompanied during the moment of hospitalization, it was observed that most (2130, 96.7%) had someone with them at the time of hospitalization. Thus, only 73 (3.3%) patients were unaccompanied. This fact demonstrates their need for support when facing the illness and hospitalization.
Regarding voluntary or involuntary hospitalization, we found over the years a considerable drop in the number of involuntary admissions. It was possible to observe a substantial decline beginning in 1996, a period marked by the opening of community services of mental health care; named as Psychosocial Care Centers (NAPS). When evaluating the hospitalization period, we also found that patients under voluntary admission had superior average stay comparing to patients under involuntary hospitalization (23.1 vs. 21.8 days), which evidences the desire for a cure, remaining the maximum period necessary.
During the studied period, from 2203 patients, 607 (27.6%) had a diagnosis of hospitalization based on ICD-9. It is worth saying that during this period the high number of unspecified diagnoses (288, 47.4%) and classified as 'other', 42 (6.9%), implies incompetence in conducting clinical diagnostics. It is also important noting that the majority of diagnoses (116, 19.1%) refer to alcoholic hallucinosis, which clearly shows the character of the acute cases. Followed by 74 (12.1%) with delirium tremens; pathological intoxication, 34 (5.6%); other alcoholic dementia, 30 (4.9%); Korsakov's psychosis, 17 (2.8%) and 6 (1%) alcoholic jealousy.
The other 1596 (72.4%) patients had their diagnoses based on ICD-10. It is noteworthy that different from what was observed in diagnoses based on ICD-9, there were a higher number of alcohol ingestion chronic cases, i.e., 695 (43.5%) cases of alcohol - dependence syndrome. The remaining patients, 415 (26.2%) had a diagnosis of alcohol use - acute intoxication; 148 (9.2%) alcohol use - psychotic disorders; 136 (8.5%) alcohol and psychoactive substance use; 78 (4.9%) alcohol use - syndrome [state] withdrawal, 39 (2.4%) alcohol use - abstinence syndrome; 29 (1.8%) alcohol use - harmful to health; 24 (1.5%) alcohol use - residual psychotic disorder, 18 (1.1%) alcohol use - amnestic syndrome and 14 (0.9%) alcohol use - other mental and behavioral disorders.
By studying inpatients due to alcoholism, it was established that the 2203 cases, 174 (7.9%) had restricted visits; 167 (7.6%) license restriction; 166 (7.5%) readmission restriction and 166 (7.5%) discharge restriction. Thus, a total of 673 (30.5%) patients submitted to some type of administrative action and/or considered therapeutic.
When evaluating the year of the first hospitalization, we have observed, in general, a progressive increase in cases numbers, however, as already noted, it is possible to identify a considerable drop in the number of new admissions for alcohol abuse in 1996, the opening period of the first NAPS; however, we did not observe a significant reduction in 2002 (date of creation and early implementation of Psychosocial Care Center) as well as in subsequent years.
By relating the year of first hospitalization with duration of hospitalization, we found a significant reduction in hospital mean period of 30 to 40 days (80's) for 20 to 30 days (the 90's), as well as in the following years.
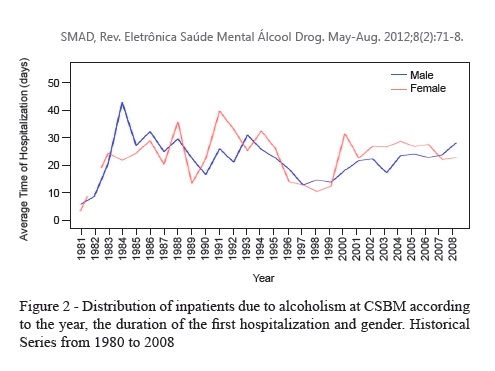
When we associate the year of the first hospitalization and duration of the hospitalization and the gender of patients, we identified a reversal in the duration of hospitalization of patients according to gender, which is a reduction of time of male patients and increase duration of hospitalization of female patients.
With respect to the type of discharge, the number of medical discharge was prevalent (1950, 88.5%), which leads us to consider a good indicator of adherence to the treatment. Followed by 118 (5.3%) discharges due to request; 53 (2.4%) transfers to medical clinic; 42 (1.9%) discharges for abandonment; 16 (0.7%) transfers (other); 12 (0.5%) administrative discharges and 12 (0.5%) due to evasion.
Of the 2203 diagnoses for hospitalizations and for discharges, it was found that 607 (27.6%) of inpatients with diagnoses based on ICD-9, 567 (25.7%) maintained the same diagnosis for discharge. Thus, only 40 (1.8%) of the patients had their discharge diagnoses different from what was received at admission.
The 1596 (72.4%) patients who had diagnoses of hospitalization based on ICD-10, at discharge, only 1398 remained with the same diagnosis. Thus, 198 (8.9%) patients had their diagnoses changed.
About the patients who got discharge diagnosis different from the admission, we can verify that 40 patients were classified differently, i.e., with diagnoses made by other ICD-9 chapters. Eleven (27.5%) were discharge with diagnoses referent as "Organic Psychiatric Disturbances", followed by 9 (22.5%) with a diagnosis of "Schizophrenic Psychoses"; 6 (15%) neurotic depression; 6 (15 %) acute response to stress; 5 (12.5%), anxiety and 3 (7.5%) frigidity and impotence.
We found that 198 patients discharge with diagnoses made by other ICD-10 chapters, the largest proportion (58, 29.2%) were diagnosed with "Paranoid Schizophrenia", followed by 40 (20.2%) with diagnosis of "Organic Mental Disorders" and 34 (17.1%) with a diagnosis of "Nonorganic Psychosis Unspecified"; 27 (13.6%) bipolar disorder - manic; 19 (9.6%) eating disorders; 12 (6.1%) dissocial personality and 8 (4%) histrionic personality.
By analyzing the distribution of patients according to referral after discharge (Reference Service), we found that the majority (970, 44%) of patients were referred to the Psychosocial Care Center (CAPS), which reveals that the institution has sought to comply with the provisions of Law no. 10,216 of 06/April/2001, which regulates the principles of psychiatric reform in its items and has CAPS as regulators of psychiatric hospitalizations, becoming, thus, mandatory as reference and counter-reference services for hospitalizations paid by SUS(9).
However, it is worrying to find that the second highest number of referrals (513, 23.2%) after discharge, were to private doctors, which brings us to some considerations regarding the maintenance of the mercantile system of health care.
It also important to emphasize the large number of patients (641, 29%) who had the referral after discharge (Reference Service), classified as "other." It is a variety of services, among which we can mention: recovery farms for drug addicts and alcoholics, religious temples, military institutions etc. Referral was requested to the physician by the patient and/or family.
Comparing the origin and routing of patients after discharge, we can verify that from the 943 (42.8%) patients registered to hospitalization by their own family, only 9 (0.4%) received referrals after discharge to come back to their families. We can, thus, assume a concern by the attending physician with the maintenance and continuity of treatment after discharge.
It should be also important to note that having occurred 150 (6.8%) admissions of patients coming from Clinical Hospital, as well as 246 (11.1%) coming from the Regional Emergency and 37 (1.6%) and 31 (1.4%) referrals after discharge for Clinical Hospital and Regional Emergency, respectively. By addressing the clinical compromising that involves the majority of cases of alcoholism, it is to consider the ability of solving clinical problems presented by psychiatric hospital.
By identifying the geographical distribution of cases in the Midwest region of Minas Gerais, i.e., the city where the patient lives and hence forwarded to the hospitalization. For better analysis the hospitalization rate was calculated (per thousand inhabitants), using the number of inhabitants in each municipality(9) by the number of inpatients at CSBM.
We were impressed by the fact that the municipalities with lower population presented the highest number of hospitalizations for alcoholism. These data are compatible with other studies(10-11), which also found a predominance of alcoholism and a large number of hospitalizations in small cities of countryside regions.
The Midwest region of Minas Gerais has 56 municipalities, 9 are considered medium sized, with between 30,000 to 80,000 inhabitants and the municipality of Divinópolis with over 200 thousand inhabitants, considered a big city(12). In this respect, we can infer the high alcohol consumption and high numbers of admissions of patients originating from the small municipalities. Thus, it could be related to low job offer, professional education, leisure and culture.
The municipalities Leandro Ferreira with 2955 inhabitants and Araújos with 7201 inhabitants had the highest rate of hospitalization due alcoholism at CSBM/1,000 inhabitants, i.e., over 5.0 patients per 1,000 inhabitants. Therefore, they are two of ten municipalities with lower population in the Midwest region of Minas Gerais.
Final Consideration
As shown by the results of this study, we can consider that the relation between man and alcohol was and remains very confrontational, generating at the end, more disadvantage than benefit. Thus, alcohol consumption is confirmed as a major health problem in the state of Minas Gerais, in all municipalities and has possible relation with negative personal and social factors, making it essential to continuous pursuit knowledge about alcoholism which increasingly will provide a fresh look at this problem. Likewise, there are doubts to the fact that there are modifications of diagnoses in patients upon admission and discharge, as well as referral of patients after discharge for private doctors. Both situations deserve specific researches.
Among the limitations of this study there is the reduced possibility to generalizability of the results, since the admission of the individuals obey only the administrative and clinical considerations associated with the welfare and administrative policies adopted by CSBM and by the Unified Health System in Midwest region of Minas Gerais. However, the design used for its development allows it to be easily reproduced in different assistance contexts.
The high number of patients included in this study is hardly found in Brazilian studies, and it must also be considered that studies based on data from existing information systems have been increasingly valued, precisely because they allow important discussions about aspects regarding the effectiveness of care practices.
References
1. Secretaria Nacional de Atenção à Saúde. SENAS (BR). Departamento de Ações Programáticas Estratégicas. Manual: Álcool e redução de danos: uma abordagem inovadora para países em transição. Brasília (DF): SENAS; 2008. [ Links ]
2. Centro Brasileiro de Informaçoes sobre Drogas Psicotrópicas (CEBRID). II Levantamento Domiciliar Sobre o Uso de Drogas Psicotrópicas no Brasil: Estudo Envolvendo as 108 Maiores Cidades do País. Sao Paulo (SP): CEBRID; 2006. [ Links ]
3. Heim J, Andrade AG. Efeitos do uso do álcool e das drogas ilícitas no comportamento de adolescentes de risco: uma revisão das publicações científicas entre 1997 e 2007. Rev. psiquiatr. clín. 2009;35(supl 1):61-4. [ Links ]
4. Galduroz JCF, Caetano R. Epidemiologia do uso de álcool no Brasil. Rev. Bras. Psiquiatr. 2009;26(1):3-6. [ Links ]
5. Gigliotti A, Bessa MA. Síndrome de Dependência do Álcool: critérios diagnósticos. Rev. Bras. Psiquiatr. 2009;26(1):11-3. [ Links ]
6. Meloni JN, Laranjeira R. Custo social e de saúde do consumo do álcool. Rev. Bras. Psiquiatr. 2004;26(1):7-10. [ Links ]
7. Seifert J. The development of alcohol dependence in Germany results from a multicenter study. Journal Psychiatr Prax. 2004;31(2):83-9. [ Links ]
8. Ribeiro MS. Fatores associados à adesão a um programa de tratamento de alcoolistas. J. Bras. Psiquiatr 2008;57(3):203-11. [ Links ]
9. Lei n. 10.216 (BR). 06 de abril de 2001. Dispõe sobre a proteção e os direitos das pessoas portadores de transtornos mentais e redireciona o modelo assistencial em saúde mental. Diário Oficial da União; 09 de Abr. 2001. [ Links ]
10. Mateos R, Páramo M, Carrera I, Rodrígues-López A. Alcohol consumption in a southern European region (Galicia, Spain). Subst Use Misuse. 2002;37(14):1957-76. [ Links ]
11. Gallassi AD, Alvarenga PG, Andrade AG, Couttolenc BF. Custos dos problemas causados pelo abuso do álcool. Rev. psiquiatr. Clín. 2008;35(suppl 1):25-30. [ Links ]
12. Ministério do Planejamento Orçamento e Gestão (BR). Distribuição Geográfica, Espacial e Delimitação Territorial. Brasília (DF): Ministério do Planejamento; 2008. [ Links ]
Received: May 31st 2010 Correspondence
Correspondence
Richardson Miranda Machado
Av. Governador Magalhães Pinto, 209, Apto.
304
Bairro: Niterói
CEP: 35500-221, Divinópolis, MG, Brasil
E-mail: richardson@usp.br
Accepted: Jan.
25th 2013











 texto em
texto em 

