Serviços Personalizados
artigo
Indicadores
Compartilhar
SMAD. Revista eletrônica saúde mental álcool e drogas
versão On-line ISSN 1806-6976
SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. port.) vol.10 no.1 Ribeirão Preto abr. 2014
http://dx.doi.org/10.11606/issn.1806-6976.v10i1p-17-22
ORIGINAL ARTICLE
DOI: 10.11606/issn.1806-6976.v10i1p-17-22
Tobacco use among users of psychosocial care centers and residential therapeutic services
El uso de tabaco entre usuarios de centros de atención psicosocial y servicios residenciales terapéuticos
Luciane Prado KantorskiI; Vanda Maria da Rosa JardimII; Michele Mandagará de OliveiraII; Roberta Zaffalon FerreiraIII; Milena Oliveira do Espírito-SantoIV; Raísa Lopes AguiarIV
IPhD, Associate Professor, Faculdade de Enfermagem, Universidade Federal de Pelotas, Pelotas, RS, Brazil
IIPhD, Adjunct Professor, Faculdade de Enfermagem, Universidade Federal de Pelotas, Pelotas, RS, Brazil
IIIDoctoral Student, Faculdade de Enfermagem, Universidade Federal de Pelotas, Pelotas, RS, Brazil. Substitute Professor, Faculdade de Enfermagem, Universidade Federal de Pelotas, Pelotas, RS, Brazil
IVUndergraduate Student, Faculdade de Enfermagem, Universidade Federal de Pelotas, Pelotas, RS, Brazil
ABSTRACT
People with psychic disorders tend to be most vulnerable to smoking. Because of the relation between smoking and the occurrence of mental illness, came to light the interest to check the consumption of tobacco among users of Psychosocial Care Centers and Residential Therapeutic Services. This is a descriptive and quantitative study conducted with 392 users of mental health services through questionnaires. The main data showed the influence of smoking with the person with psychic disorder and the diagnosis, since these people show behavioral patterns which justify smoking. Therefore, we should think on harm reduction and prevention as care strategies for these people.
Descriptors: Rehabilitation Centers; Mental Disorders; Smoking.
RESUMEN
Personas portadoras de trastornos psíquicos tienden a ser un grupo más vulnerable al hábito de fumar. Frente la relación existente entre tabaquismo y la ocurrencia de la enfermedad mental, surgió el interés de verificar el consumo de tabaco en usuarios de Centros de Atención Psicosocial y Servicios Habitacionales Terapéuticos. Se trata de un estudio descriptivo y cuantitativo realizado con 392 usuarios de servicios de salud mental, mediante aplicación de cuestionarios. Los principales datos revelados fueron la superioridad del humo entre esta población y la relación con el diagnóstico, pues estas personas presentan calidades comportamentales sumado al tratamiento farmacológico que justifican lo gusto por el hábito de fumar. Por tanto, se debe pensar en la reducción de daños y prevención como estrategias de cuidado a estas personas.
Descriptores: Centros de Rehabilitación; Trastornos Mentales; Hábito de Fumar.
INTRODUCTION
Smoking, a cultural practice among indigenous groups and disseminated worldwide by the tobacco industry, is a epidemic related to various diseases, directly or indirectly(1).
Regardless of creed, race or social class, the use of psychoactive substances has always been present in our culture(2). The reasons for the use of these substances are cults, rituals, commemorative events, pleasure feelings, pain relief, among others(3).
However, smoking is responsible for an average of 200,000 deaths each year in Brazil and exceeds the deaths due to alcoholism, AIDS, traffic accidents, homicides and suicides(4).
Due to the attention to mental disorders, the Brazilian psychiatric reform movement is been developing since the late of the 1970 decade. The main goal of this movement is replacing the psychiatric hospital as treatment space, in favor of other therapeutic practices that recover citizenship and autonomy of the mentally ill patients across the country(5).
Thus, places such as the Psychosocial Care Centers (PCC) provide mental health care with the objective to provide service to users, perform clinical monitoring and encourage social reintegration, creating the possibility to substitute the psychiatric hospital(6-7).
Also in this context, Residential Therapeutic Services (RTS) strengthen the hospital-centered model substitution. These services are alternatives of assisted living for people who experience psychiatric hospitalization for a long period and are deprived of family care. It can also be considered as a support to other mental health services and support to ensure the permanence of users outside asylums(8-9).
Psychological disorders people tend to be a vulnerable group to smoking. For many years, the impact of smoking in this population has been neglected due to failure to recognize that smoking is an addiction. Studies show that smoking in people suffering from mental disorders is higher than in the general population, including higher levels of tolerance and dependence(10).
Studies indicate close relationship between smoking and psychopathological features, in which stand out schizophrenia and depression(11).
Because of this relationship between smoking and the occurrence of mental illness the interest to verify the consumption of tobacco in PCC and RTS users was created. This is a study that enables greater knowledge about tobacco consumption in people with mental disorders.
s
METHOD
The presentation of this study belongs to the research entitled "Rehabilitate networks – Evaluating innovative experiences in the composition of networks of psychosocial care" (REDESUL) with a quantitative, descriptive and transversal approach. However, this paper presents a descriptive analysis.
PCC users and residents of the RTS from Brazilian southern (Alegrete, Bagé, Caxias do Sul, Porto Alegre and Viamão) were interviewed and selected for the sample from 07 to 10 September 2009. Questionnaires were given to users and their companions. A nominal variable (smoking) was used to identify the existence of smokers, ex-smokers and non-smokers in health services. There were no specific and validated questionnaires regarding tobacco use. There were three empirical issues related to tobacco use, period of use and number of cigarettes consumed in a day.
To calculate the sample an alpha value equal to 5% and a power of 80% was used, and the calculation was performed on Epi-info 6.04 through different measures and indicators of variability found in the literature.
The study included 392 users in the quantitative stage. From the five cities selected for the sample we interviewed 143 users from Residential Therapeutic Services and 249 interviewees in PCCs, among users of semi-intensive care and intensive care. Children, alcohol and drugs from PCCs were not sampled, given their specificities. As the criterion for identifying was defined from a Residential Therapeutic Services, the services were identified in the five cities in Rio Grande do Sul with RTS.
To test the tools and enable them to the needs, a pilot project was created. It was performed in a PCC in Pelotas/RS, a city which has not been selected in the sample, after training of interviewees and development of instruments.
The REDESUL research was approved by the Ethics Committee of the School of Dentistry, Federal University of Pelotas – UFPel, No. 073/2009. All participants signed an informed consent.
RESULTS
DISCUSSION
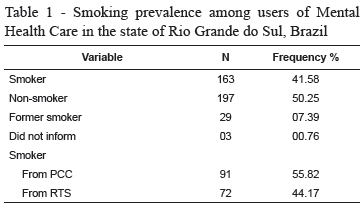
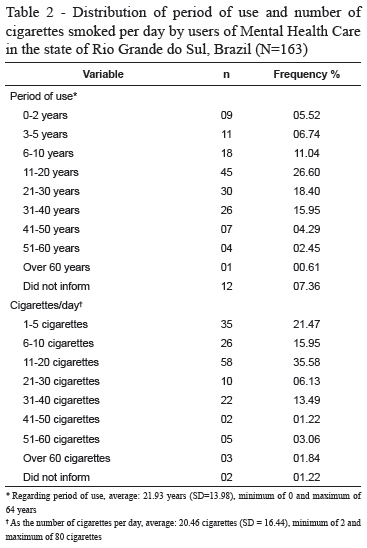
This study presents 41.58% of smokers in health care service with an average time of use of 21.93 years and average consumption of 20.46 cigarettes per day. Given these results, it can be stated that Brazil, for its great cultural, social and economic diversity, can directly influence smoking habits. The literature shows that the prevalence of daily smoking, pointed out in a study conducted in Southern Brazil(12), was higher in the South and Southeast regions. This study shows findings that corroborate with the results found in searches of the Protective and Risk Factors for Chronic Diseases by Telephone Survey (VIGITEL – in Portuguese), which has been monitoring, among others, smoking in the adult population of 26 state capitals and the Federal District(12).
Smoking is caused by several factors, including individual characteristics of human being and also the strong influence of the family and the social group. Adolescence is characterized as the period when the person is more likely to adopt behavior changes, and this may reflect initial actions and behaviors to acquire habits like smoking and alcohol(13).
Strengthening the idea of the role of the family against smoking, there is a study that reported exposure to tobacco influenced by cultural behavior in society and family. In large urban centers, such as São Paulo-SP, there are families that support and consent smoking, particularly in psychiatric patients, with the intention that this habit provides "welfare" and keep the patient calm and the mental disorder "under control". This practice is also accepted in psychiatric hospitals under the same conditions(12). In countries where smoking is prohibited by the family and those with mental illness live and rely on their families for their care, the prevalence and exposure to alcohol and tobacco decrease(14).
Smoking is directly harmful to health. Smokers can be considered chronic ill and patients susceptible to multiple health problems had higher chances of developing lung cancer or other in organs, chronic obstructive pulmonary disease (COPD), heart and circulatory complications, skin problems and oral cavity, among others(15). Tobacco consumption causes not only proven health risks, it is characterized as a legal drug, unlike other drugs, which causes the greatest challenges to promote its control as its consumption is tolerated in the society(16).
Given this reality of non-restraint tobacco consumption, it is thought, as a control strategy, prevention, reduction and harm reduction for those who already have the habit(16).
This study shows smoking prevalence of 41.58%, a rate below the average reported by other studies, which justifies its contents by the connection between nicotine dependence and psychiatric disorders, as the prevalence of tobacco use is higher among people with mental disorders (50 to 84%) compared to the general population (27 to 58%)(17).
Patients with mental disorders have higher tendency to acquire the habit of smoking, because the action of nicotine in the body causes a positive effect on mood and cognition of the individual(18).
Thus, it is believed that smoking is common among schizophrenics. Based on the analysis of table 3 we noticed that, in this study, 44.4% people with this diagnosis are smokers.
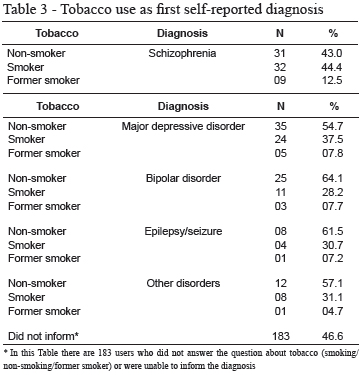
In other studies high prevalence of smokers (80%) with schizophrenia was observed, surpassing what was found in this study(17). Studies in other countries also state these findings presenting a prevalence of 64% of smoking in schizophrenics, in a survey carried out in Spain(19).
Smoking is more severe when associated with factors such as young age, early onset of mental disorders, higher number of hospitalizations and high doses of antipsychotic medications(20).
The literature discusses tobacco use among schizophrenic patients as a reflection of the institutionalization process, boredom and low impulse control of individuals with this disease. Reports of patients claim that smoking is relaxing, reduces anxiety and side effects of medications. It can also improve concentration and reduce unpleasant arousal experienced by some schizophrenics(11).
Another relevant fact pointed out by this study refers to the prevalence of smoking among patients with depression. However, the results indicated in this study (54.7% of patients with depression do not smoke) contradict the findings of other studies. This disparity of results can be understood due to the limitations of the study because the diagnoses were self-referenced by respondents and also by the possible reduction in the number of smokers in the Brazilian general population which dropped in 65% from 1980 to 2010. In 2010 there was the slightest record of cigarette consumption per capita (682 units) throughout this period(21). A study made in 2010 revealed that the occurrence of depression was higher in smokers than in people who never smoked(18).
A study that brings a non-systematic review of literature of the relationship between smoking and psychiatric disorders states that the act of quitting smoking is reduced in patients with depression. And yet, when this practice is left behind, such action may contribute to worsening of symptoms evolving, possibly, for the occurrence of new depressive episode(11).
One acceptable explanation to justify the relationship between smoking and depressive disorders is that tobacco use can cause a relief feeling from sadness and negative mood, assuming the role of "self-medication". There is even scientific evidence that nicotine acts on the neurotransmitter system reflecting in mood regulation(11). Another determinant factor of this connection between smoking and depression is because of the unidirectional relation, where the occurrence of one substance influences directly on the other. People who smoke and are depressed use this habit in an attempt to relieve negative feelings, smoking becomes reinforcing and stimulating(11).
In discussions about smoking it is very clear the search and desire for abstinence, so it is worth reflecting on the care approach to patients dependent on licit or illicit substances. Nowadays, there is the understanding for care and expanded clinic, whose practice is the transformation of the biological and individual attention given to the patient as a whole, being understood on all aspects(22). In relation to tobacco dependence, it can be considered as an alternative to reducing damage to the patient, seeking the possibility of reducing consumption in order to minimize damage to health, respecting the uniqueness and the free will of each individual. This dependency can involve strong psychological factors that should not be disregarded from care plan and attention, valuing the person and his/her experience in every aspect of his/her life(15-16).
FINAL CONSIDERATION
This study provided a better understanding of the connection between tobacco consumption and the occurrence of mental illness. Relevant data were revealed regarding the practice of smoking and the care services that these people attend. The diagnosis was a relevant explanation for this connection, because for people with these diagnoses have behavioral patterns linked to pharmacologic treatment to justify smoking.
It should be thought on tobacco and smoking from the idea that tobacco is considered a legal drug without any legal restriction and the practice of smoking as culturally accepted in our society, however, very harmful to health. Therefore, abstinence during healthcare practice is to be considered, since it is the patient’s will.
Currently, there is the concept of expanded health care, which in practice reflects respect for the individual and complete view of the subject. Thus, it should be based on the concept of harm reduction to these people who opt for smoking and still invest in prevention, because a country with fewer cases of smoking means less spending on health and fewer cases of associated diseases, resulting from tobacco, with the possibility of investing in other sectors.
REFERENCES
1. Kroeff LR, Mengue SS, Schmidt MI, Duncan BB, Favaretto ALF, Nucci LB. Fatores associados ao fumo em gestantes avaliadas em cidades brasileiras. Rev Saúde Pública. 2004;38(2):261-7. [ Links ]
2. Duncan BB, Schmidt MIS. Medicina embasada em evidências. Rev Assoc Med Bras. 1999; 45(nº esp):247-54. [ Links ]
3. Spricigo JS, Alencastre MB. The nurse from health unit and the drug user: one analysis in Biguaçu/SC. Rev. Latino-Am. Enfermagem. 2004;12(spec number):427-32. [ Links ]
4. Menezes AMB, Dumith SC, Martínez-Mesa J, Silva AER, Cascaes AM, Domínguez GG, et al. Problemas de saúde mental e tabagismo em adolescentes do sul do Brasil. Rev Saúde Pública. 2011;45(4):700-5. [ Links ]
5. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Coordenação geral de saúde mental. Reforma psiquiátrica e política de saúde mental no Brasil. Conferência Regional de Reforma dos Serviços de Saúde Mental: 15 anos depois de Caracas. Brasília: OPAS, Ministério da Saúde; 2005. [ Links ]
6. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Saúde Mental no SUS: os centros de atenção psicossocial. Brasília (BR): Ministério da Saúde; 2004. [ Links ]
7. Kantorski LP, Machado RA, Lemões MAM, Quadros LCM, Coimbra VCC, Jardim VMR. Avaliação da estrutura e processo na visão dos familiares de usuários de saúde mental. Cienc Cuidado Saúde. 2012;11(1):173-80. [ Links ]
8. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Residências terapêuticas: o que são, para que servem. Brasília (BR): Ministério da Saúde; 2004. [ Links ]
9. Argiles CTL, Kantorski LP, Willrich JQ, Antonacci MH, Coimbra VCC. Redes de sociabilidade: construções a partir do serviço residencial terapêutico. Ciênc Saúde Coletiva. 2013;18:2049-58. [ Links ]
10. Scherer EA, Scherer ZAP, Azevedo HA, Durão MAS. Opinião de pacientes psiquiátricos internados sobre o hábito de fumar. SMAD, Rev Eletronica Saúde Mental, Álcool e Drog. [Internet]. 2012 [acesso 20 dez 2012]; 8(1):25-33. Disponível em: http://pepsic.bvsalud.org/pdf/smad/v8n1/05.pdf [ Links ]
11. Rondina RdC, Gorayeb R, Botelho C. Relação entre tabagismo e transtornos psiquiátricos. Rev Psiquiatr Clín. 2003;30(6):221-8. [ Links ]
12. Barros AJD, Cascaes AM, Wehrmeister FC, Martínez-Mesa J, Menezes AMB. Tabagismo no Brasil: desigualdades regionais e prevalência segundo características ocupacionais. Ciênc Saúde Coletiva. 2011;16(09):3707-16. [ Links ]
13. Breslau N, Kilbey MM, Andreski P. Nicotine dependence, major depression and anxiety in young adults. Arch Gen Psychiatry. 1991;48:1069-74. [ Links ]
14. Ratto LRC, Menezes PR, Gulinelli A. Prevalência de tabagismo em indivíduos com transtornos mentais graves, São Paulo, Brasil. Rev Saúde Pública. 2007;41(4):510-6. [ Links ]
15. Silva LCC. Tabagismo: doença que tem tratamento. Porto Alegre: Artmed; 2012. 309 p. [ Links ]
16. Ministério da Saúde (BR). Drogas e redução de danos: uma cartilha para profissionais de saúde. São Paulo: Ministério da Saúde; 2008. [ Links ]
17. Malbergier A, Oliveira Jr HP. Dependência de tabaco e comorbidade psiquiátrica. Rev Psiquiatr Clín. 2005;32(5)276-82. [ Links ]
18. Castro MRPd, Matsuo T, Nunes SOB. Características clínicas e qualidade de vida de fumantes em um centro de referência de abordagem e tratamento do tabagismo. J Bras Pneumol. 2010;36(1):67-74. [ Links ]
19. Herran A, Santiago AD, Sandoya M, Fernández MJ, Diez-Manrique JF, Vásquez-Barquero JL. Determinants of smoking behaviour in outpatients with schizophrenia. Schizoph Res. 2000;41:373-81. [ Links ]
20. Goff DC, Henderson DC, Amico E. Cigarette smoking in schizophrenia: relationship to psychopathology and medication side effects. Am J Psychiatry. 1992; 149:1189-94. [ Links ]
21. Instituto Nacional do Câncer (BR). [Internet]. INCA: Observatório da política nacional de controle do tabaco. [acesso 7 jan 2013]. Disponível em http://www.2inca.gov.br [ Links ]
22. Cunha GT. A construção da clínica ampliada na atenção básica. [Dissertação de mestrado em Saúde Coletiva]. Campinas: Faculdade de Ciências Médicas da Universidade Estadual de Campinas; 2004. 199 p.
 CORRESPONDENCE
CORRESPONDENCE
Roberta Zaffalon Ferreira
Rua Presbítero Claudio Neutzling, 103, Apto. 205B
Bairro: Três Vendas
CEP: 96055-068, Pelotas, RS, Brasil
E-mail: betazaffa@gmail.com
Received: Mar. 26th 2013
Accepted: Nov. 11th 2013











 texto em
texto em 

