Serviços Personalizados
artigo
Indicadores
Compartilhar
SMAD. Revista eletrônica saúde mental álcool e drogas
versão On-line ISSN 1806-6976
SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. port.) vol.13 no.2 Ribeirão Preto abr./jun. 2017
http://dx.doi.org/10.11606/issn.1806-6976.v13i2p64-70
ORIGINAL ARTICLE
DOI: 10.11606/issn.1806-6976.v13i2p64-70
Mental and behavioral disorders due to psychoactive substance use at a psychiatric hospital
Trastornos Mentales derivados del uso de drogas en un Hospital Psiquiátrico
Márcia Astrês FernandesI; Kellison Lucas Carvalho PintoII; José Alves Teixeira NetoII; Juliana Macêdo MagalhãesIII; Claudia Maria Sousa de CarvalhoIV; Ana Lívia Castelo Branco de OliveiraV
IPhD, Adjunct
Professor, Universidade Federal do Piauí, Teresina, PI, Brazil. RN, Hospital
Psiquiátrico Areolino de Abreu, Teresina, PI, Brazil
IIUndergraduate
student in Nursing, Centro Universitário Uninovafapi, Teresina, PI, Brazil
IIIMSc, Assistent
Professor, Centro Universitário Uninovafapi, Teresina, PI, Brazil. RN, Centro
de Atenção Psicossocial Álcool e Drogas III (CAPS-AD III), Teresina, PI,
Brazil
IVMSc, Assistent
Professor, Centro Universitário Uninovafapi, Teresina, PI, Brazil. RN, Fundação
Municipal de Saúde, Teresina, PI, Brazil
VMaster’s student,
Universidade Federal do Piauí, Teresina, PI, Brazil. RN, Prontomed, Teresina,
PI, Brazil
ABSTRACT
In this study, the objective was to describe the profile of patients hospitalized at a psychiatric hospital who had been diagnosed with mental and behavioral disorders due to psychoactive substance use. Documentary study with a retrospective design, obtained from the admission records in the service register. In total, 10.4% of the records of patients hospitalized in the year under study were evaluated. The data were organized in tables. The results showed that most patients were male, young adults, unemployed, with simultaneous drugs use. Alcohol was the most consumed substance. The rehospitalization rate in the year in question was 29.6%. Interdisciplinary interventions facilitate the quality of health, so that the professionals can act in the users’ welcoming and their health needs.
Descriptors: Substance-Related Disorders; Hospitals, Psychiatric; Mental Health; Nursing.
RESUMEN
El presente estudio tuve por objetivo describir el perfil de los pacientes ingresados en un hospital psiquiátrico con diagnóstico de "Trastornos Mentales y del Comportamiento Debido al consumo de sustancias psicoactivas". Estudio documental y retrospectivo, obtenido del registro de admisiónes en el libro del servicio. Un total de 10,4% de pacientes en internación en el año de estúdio fue valorada. Los datos fueron organizados en tablas. De los resultados, la mayoría era hombre, adulto/jóven, desempleado, con el uso simultâneo de drogas, el álcool siendo lo más consumida. Los reingresos en aquel año fueron 29,6%. La practica de intervenciones interdisciplinares facilita la calidad en salud, aún los profesionales puedan actuar en la acojida, incluso en sus necessidades de salud.
Descriptores: Trastornos Relacionados con Sustancias; Hospitales Psiquiátricos; Salud Mental; Enfermería.
Introduction
The presence of drugs use-related mental disorders has been demonstrated in Brazilian and international studies(1-3). The evidence found includes psychoactive substance abuse, which can result in complications for the user’s family and social context, besides high morbidity and mortality rates, especially when associated with psychiatric complications(4-5).
What psychoactive substances are concerned, alcohol is a legal drug the global population uses a lot. Its repercussions are related to symptoms of depression, anxiety and hypomania/mania during the periods of intoxication and abstinence(6-7). Researchers appointed high rates of alcohol addiction in the population, corresponding to 14.9%, followed by major depression (13%), dysthymia (4.9%), bipolar disorder and others(8).
In a study developed in 2011, involving 149 drug addicts in Paraguay, it was verified that the main disorders related to psychoactive substance use were: depression (17.4%), anxiety (17.4%) and bipolar disorder (15%)(9).
Cocaine abuse is equally related to depressive disorder, as verified in one study. Crack, the smoked variety of cocaine, has been the preferred drug of many, as illustrated by its economic accessibility. The same information was revealed in this study with regard to the high prevalence of psychopathologies(10).
A crucial aspect to prevent and/or treat mental disorders in chemical addicts is the nurse’s role, through the applicability of systemized care and in partnership with other multiprofessional team members. Thus, nursing care for these users aims to incorporate principles with a view to a care practice that is open to the needs of the users involved, in the context of chemical addiction(11).
In view of these considerations, it is important to highlight how seriously the theme should be treated, requiring a proposal for a postural change, considering the prominence of the theme, mainly in the field of citizenship, as drug consumption and mental disorders are health problems that should be addressed not only by the health team, but also by society.
As drugs can trigger and worsen mental disorders, considering the abuse of these substances and the increasing number of hospitalizations at general and psychiatric hospitals, an increasing number of people with mental disorders use drugs. The objective in this study was to describe the profile of patients hospitalized at a psychiatric hospital with a diagnosis of mental and behavioral disorders due to psychoactive substance use.
Method
A retrospective study was undertaken based on secondary data. This research was developed at the Psychiatric Hospital (PH) located in the city of Teresina, PI, Brazil. The place of study was selected because it is a reference service in mental healthcare in the Northeast of Brazil and because it is the only psychiatric hospital in the State. This public (state-owned) health service serves as an important teaching hospital affiliated with Universidade Federal do Piauí (UFPI). In 2014, 24,199 care sessions took place, 15,769 of which were outpatient consultations, 1,164 hospitalizations and 6,732 emergency care sessions.
A census study was undertaken: all clients hospitalized in 2014 were included, diagnosed with mental and behavioral disorders due to psychoactive substance use, classified by the International Classification of Diseases (ICD-10).
A Free and Informed Consent Term (FICT) was used according to CNS Resolution number 466/2012. Numerical codes were adopted to guarantee the complete anonymity of the collected information, complying with all ethical and legal premises of National Health Council Resolution 466.
The researchers collected the data based on the documentary analysis of the information in the service’s admission register. A form was elaborated to register the collected data, addressing the sociodemographic aspects related to the medical diagnosis and the associated psychiatric comorbidities, as well as the types of psychoactive substances used.
The data were collected in March 2015, after the approval by the Research Ethics Committee at Centro Universitário UNINOVAFAPI (CAAE 40844315.5.0000.5210).
After the data collection, the data were typed and analyzed, using the software PASW Statistics Data Editor, and presented in tables, using Microsoft Excel 2010 for Windows XP, distinguishing the descriptive results of the research variables.
Results
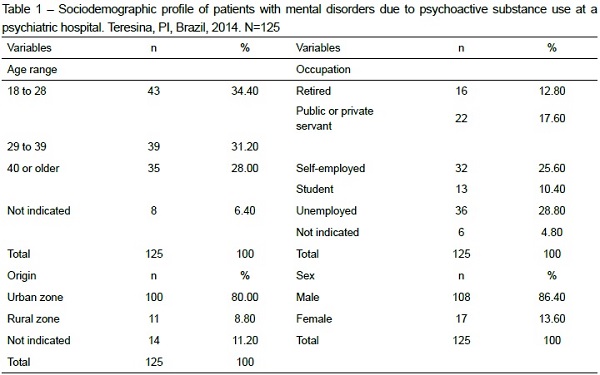
It was verified that, in 2014, in total, 1,164 hospitalizations took place at the place of study, resulting from a wide range of psychiatric diagnoses. In this group, 10.4% were hospitalized with mental disorders due to psychoactive substance use. For the purpose of this study, the sample was mostly male (86.45%), 28.8% of the participants were unemployed and were between 18 and 28 years of age (34.4%). What the origin is concerned, the majority lived in the urban zone (80.0%) (Table 1).
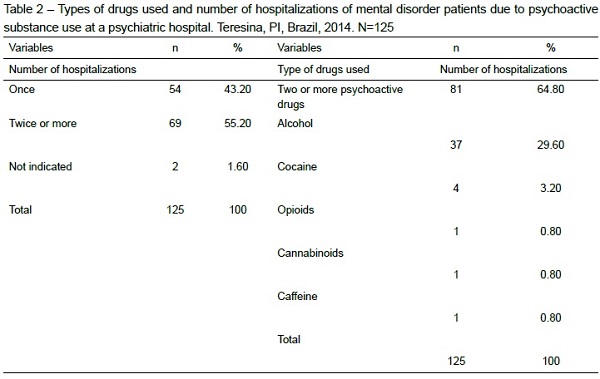
In Table 2, the most used types of drugs and the figures on the participants’ hospitalizations are presented. As observed, more than half of the participants (64.8%) used multiple drugs, alcohol being the most consumed substance (29.6%). What the number of hospitalizations is concerned, a considerable part of the sample (55.2%) was hospitalized twice or more during that year, indicating a considerable amount of rehospitalizations.
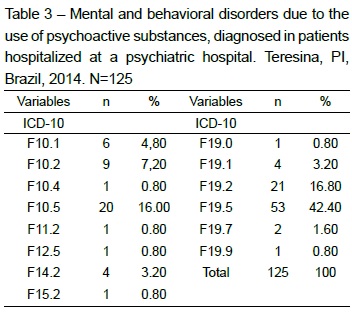
The most frequent mental and behavioral diagnoses among the study participants are displayed in Table 3. As observed, almost half of the participants (42.4%) had been diagnosed with mental/behavioral disorders due to the use of multiple psychoactive drugs (psychotic disorder).
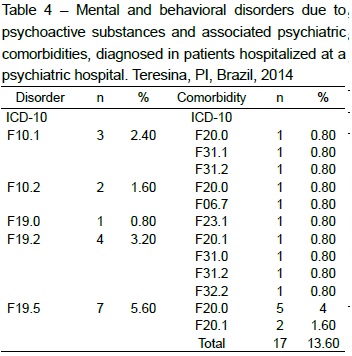
One relevant information refers to the presence of psychiatric comorbidities. Among the 125 participants, 17 (21.25%) presented another concomitant psychiatric diagnosis, the most prevalent (5.6%) being paranoid schizophrenia (F20.0), significantly associated with the diagnosis of mental and behavioral disorders due to the use of multiple drugs or other psychoactive substances – psychotic disorder (F19.5), as demonstrated in Table 4.
Discussion
As evidenced in this study, the diagnosis of mental and behavioral disorders due to the use of psychoactive substances at psychiatric hospitals stands out around the world(3,12). That represents a severe health problem, due to the possible repercussion on public spending in tertiary health care, family interrelations and in the professional and social spheres. The importance of an early diagnosis should be highlighted, as well as treatment compliance for this disorder, as the drugs users themselves, for different reasons, appoint that they are seeking clinical and psychotherapeutic treatment for psychoactive substance-related disorders.
What the sociodemographic profile in the sample is concerned, men were predominant, with a higher percentage of alcohol abuse, supporting the results of the study developed in 2011 at a Psychosocial Care Center AD in the city of Teresina, Piauí, in which 88.9% of the participants were under treatment for alcoholism and were men(13).
The young adult age range was predominant and this reflects the early awakening to drugs, which can contribute to the development of mental disorders. The abandonment of the family relationship, the search for socialization and the popular conquest make the young people receive further influence from friends, which can be one way to adhere to drugs(14).
That is the reality of young people living in situations of psychosocial and economic vulnerability, without opportunities for professionalization and space in the job market, issues reflects in the characteristics of the present study sample. Similarly, significant levels were found in a sociodemographic study undertaken in Curitiba, PR, in 2010, in which 45.2% of the hospitalized patients were unemployed and 38.5% worked without institutional affiliation(15).
As for the origin, the urban zone exceeded the rural zone. Urban areas do favor the obtention and use of drugs. This information supports the data presented in the first Brazilian survey on alcohol consumption patterns in the Brazilian population, in which a similar percentage was demonstrated(16).
Alcohol was the most consumed substance individually, followed by cocaine, opioids, cannabionoids and caffeine. What the simultaneous use of two or more drugs is concerned, alcohol also prevailed, besides cocaine and cannabinoids. The Brazilian Association of Psychiatry (ABP) has appointed this use(17).
Concerning alcohol, although the patients in this study prefer it, the use of new substances should be highlighted, also demonstrating further associations with psychiatric comorbidities. In a study developed in Minas Gerais, the historical trajectory of the psychiatric hospitalization profile was outlined between 1998 and 2009, showing a drop in hospitalizations due to alcohol-related mental disorders to the detriment of disorders associated with other drugs(18). This demonstrates increased production and consumption of increasingly harmful and accessible psychoactive substances.
Another piece of information refers to the number of hospitalizations in 2014, which can demonstrate the persistent use of psychoactive substances, indicating failure to continue the treatment in community care, as well as the need to review the patient’s discharge planning with a view to the user’s effective recovery.
What the occurrence of mental disorders due to drugs use is concerned, mental/behavioral disorders due to the use of multiple psychoactive drugs are more recurrent – psychotic disorder, and mental/behavioral disorders due to the use of multiple psychoactive drugs – alcoholism. It has been demonstrated in a study that the abstinence syndrome and alcoholism have been the main mental disorders due to psychoactive substance use(19).
It should be highlighted that a significant part of the study population presented other psychiatric comorbidities associated with mental and behavioral disorders due to the use of multiple psychoactive substances, as well as alcohol-related disorders, particularly paranoid schizophrenia, with significant frequency rates in this sample. Therefore, it is important to emphasize that the double diagnosis generally develops later and interferes in treatment compliance, besides the possibility of risk behaviors and suicidal ideas(20).
In a study developed in Norway, involving hospitalized psychiatric patients, the high prevalence of mental disorders related to psychoactive substances stood out in patients diagnosed with schizophrenia. Alcohol-related mental disorders were also responsible for high rates of schizophrenia (25%), bipolar disorder (20.1%) and depression (10.9%)(21). In another Brazilian study, depressive symptoms were found in drugs users, whose profile was similar to that found in this study(22).
Psychiatric comorbidities can interfere in the identification of drugs addiction and in the other mental disorder and vice-versa. In a study involving drugs users and the concomitant diagnosis of bipolar disorder, the overlapping of the symptoms was considered a limiting factor for the clinical diagnosis(23).
Comorbidities enhance the negative consequences of drugs use-related mental disorders and compromise the prognosis. In that sense, attention and caution are needed and holistic treatment should be offered to the user, addressing all health needs.
Final considerations
The higher prevalence of mental and behavioral disorders was found in young adult men who were unemployed and repeatedly hospitalized due to psychoactive substance use, especially alcohol, being the most common mental disorder related to multiple drug use. It is important to highlight the thematic relevance, the overlapping among mental and behavioral disorders due to psychoactive substance use, which has been highly relevant for health professionals, as they are confronting one of the severe public health problems.
The double psychiatric diagnosis increasingly emerges as a profile for these drugs users studies, representing the extension of this severe problem, involving failures ranging from education to prevent drugs use to the interruption of the treatment. That enhances the number of rehospitalizations and the length of the rehabilitation, demanding the nurse’s critical look, who should qualify her role in the rehabilitation of drugs users, expanding the possibilities of holistic care through humanized welcoming, active listening, besides other actions to continue the care involving users and their families.
We hope that this research can contribute to the clinical practice of nursing professionals who work with people diagnosed with mental disorders due to drugs use, and also arouse reflections on the theme, enhancing the visibility and encouraging the discussion, with a view to promoting changes in policies and acctions related the therapeutic approach and the continuity of the user’s treatment.
References
1. Hess AR, Binsfeld ARMM, Moraes AL. Comorbidades psiquiátricas em dependentes químicos em abstinência em ambiente protegido. Est Psicol. 2012;17(1):171-8. [ Links ]
2. Zaleski M, Laranjeira RR, Marques ACPR, Ratto L, Romano M, Alves NP, et al. Diretrizes da Associação Brasileira Comorbidades psiquiátricas em dependentes químicos 178 de Estudos do Álcool e outras Drogas (ABEAD) para o diagnóstico e tratamento de comorbidades psiquiátricas e dependência de álcool e outras substâncias. Rev Bras Psiquiatria. 2006;28(2):142-8. [ Links ]
3. Finlay AK. Sex Differences in Mental Health and Substance Use Disorders and Treatment Entry Among Justice-involved Veterans in the Veterans Health Administration. Medical Care. 2015;53(4):105-11. [ Links ]
4. Chalub M, Telles LEB. Álcool, drogas e crime. Revista Brasileira de Psiquiatria. 2006;28(2): 69-73. [ Links ]
5. Kolling NM, Silva CR, Carvalho JCN, Cunha SM, Kristensen CH. Avaliação neuropsicológica em alcoolistas e dependentes de cocaína. Avaliação Psicol. 2007;6(2):127-37. [ Links ]
6. Alves H, Kessler F, Ratto LRC. Comorbidade: uso de álcool e outros transtornos psiquiátricos. Rev Bras Psiquiatria. 2004;26(1):51-3. [ Links ]
7. Almeida RMM, Flores ACS, Scheffer M. Ideação suicida, resolução de problemas, expressão de raiva e impulsividade em dependentes de substâncias psicoativas . Psicol Reflex Crit. 2013; 26(1):1-9. [ Links ]
8. Leal EM, Delgado PGG, Man R, Strilke C, Brands B., Khenti A. Estudo de comorbidade: sofrimento psíquico e abuso de drogas em pessoas em centros de tratamento, Macaé - Brasil. Texto Contexto - Enferm. 2012;21(spe):96-104. [ Links ]
9. Lopez RP, Brands B, Strilke C, Man R, Khenti A. Estudio de la comorbilidad entre el distres psicológico y abuso de drogas en pacientes en dos centros de tratamiento, Asunción - Paraguay. Texto Contexto-Enferm. 2012;21(spe):168-73. [ Links ]
10. Scheffer M, Pasa GG, Almeida RMM. Dependência de álcool, cocaína e crack e transtornos psiquiátricos. Psicologia: Teor Pesq. 2010;26(3):533-41. [ Links ]
11. Reinaldo AMS, Pillon SC. História da enfermagem psiquiátrica e a dependência química no Brasil: atravessando a história para reflexão. Esc. Anna Nery Rev. Enferm. 2007;11(4):688-93. [ Links ]
12. Scisleski ACC, Maraschin C, Silva RNA. Manicômio em circuito: os percursos dos jovens e a internação psiquiátrica. Cad Saúde Pública. 2008; 24(2):342-52. [ Links ]
13. Monteiro CFS, Fé LCM, Moreira MAC, Albuquerque IEM, Silva MG, Passamani MC. Perfil sociodemográfico e adesão ao tratamento de dependentes de álcool em CAPS-ad do Piauí. Esc Anna Nery. 2011;15(1):90-5. [ Links ]
14. Carvalho M, Matos MG. Psychosocial Determinants of Mental Health and Risk Behaviours in Adolescents. Global J Health Sci. 2014;6(4):22-35. [ Links ]
15. Capistrano FC, Ferreira ACZ, Silva TL, Kalinke LP, Maftum MA. Perfil sociodemográfico e clínico de dependentes químicos em tratamento: análise de prontuários. Esc Anna Nery. 2013;17(2):234-41. [ Links ]
16. Duarte PCAV. I Levantamento Nacional de álcool e droga. Consumo de álcool [Internet]. Brasília: Secretaria Nacional Antidrogas; 2007. [Acesso 20 abr 2015]. Disponivel em: http://bvsms.saude.gov.br/bvs/publicacoes/relatorio_padroes_consumo_alcool.pdf. [ Links ]
17. Associação Brasileira De Psiquiatria. Projetos e Diretrizes. Abuso e Dependência de Múltiplas Drogas [Internet]. 2012 [Acesso 27 abr 2015]. Disponível em: <http://www.projetodiretrizes.org.br/projeto_diretrizes2013/drogas.pdf> [ Links ].
18. Campos CG, Costa J, Moacyr L. Causas múltiplas de óbito e as internações psiquiátricas por uso e abuso de substâncias psicoativas em um município de minas gerais. SMAD, Rev Eletrônica Saúde Mental Álcool Drog. (Ed. port.) [Internet]. 2013 [Acesso 18 out 2016]; 9(3): 111-5. Disponível em: http://pepsic.bvsalud.org/scielo.php?script=sci_abstract&pid=S1806-69762013000300003&lng=pt&nrm=iso&tlng=pt [ Links ]
19. Sousa FSP, Oliveira EN. Caracterização das internações de dependentes químicos em Unidade de Internação Psiquiátrica do Hospital Geral. Ciênc Saúde Coletiva.2010;15(3):671-7. [ Links ]
20. Anne ML, Ulrik FM, Stein O. Comorbid mental disorders in substance users from a single catchment area - a clinical study. BMC Psychiatry. 2011;11:25. doi: 10.1186/1471-244X-11-25 [ Links ]
21. Nesvåg R, Knudsen GP, Bakken IJ, Ystrom E, Surén P, Reneflot A, et al. Substance use disorders in schizophrenia, bipolar disorder, and depressive illness: a registry-based study. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1267–76. [ Links ]
22. Marcon SR, Rubira EA, Espinosa MM, Barbosa DA. Quality of life and depressive symptoms among caregivers and drug dependent people. Rev. Latino-Am. Enfermagem. 2012;20(1):167-74. doi: http://dx.doi.org/10.1590/S0104-11692012000100022 [ Links ]
23. Theodore RS, Basco MR, Biggan JR. Diagnostic Disagreements in Bipolar Disorder: The Role of Substance Abuse Comorbidities. Depression Res Treat. 2012;(2012): Article ID 435486, 6 pages, 2012. doi:10.1155/2012/43548 [ Links ]
Received: Oct. 31st 2015
Accepted: Nov. 4th 2016
Corresponding Author:
Márcia Astrês Fernandes
Universidade Federal do Piauí
Campus Universitário Ministro Petrônio Portela,
Bairro Ininga, Bloco 12
CEP: 64049-550 , Teresina, PI, Brasil
E-mail: m.astres@ufpi.edu.br











 texto em
texto em 


