Servicios Personalizados
Articulo
Indicadores
Compartir
SMAD. Revista eletrônica saúde mental álcool e drogas
versión On-line ISSN 1806-6976
SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. port.) vol.13 no.2 Ribeirão Preto abr./jun. 2017
http://dx.doi.org/10.11606/issn.1806-6976.v13i2p78-85
ORIGINAL ARTICLE
DOI: 10.11606/issn.1806-6976.v13i2p78-85
Attention deficit hyperactivity disorder and crack cocaine: what does the comparison between a group of users and non-users indicate?1
Trastorno por Déficit de Atención y Hiperactividad y Cocaína de crack: que indica la comparación de los usuarios y no usuarios?
Ana Carolina Maciel CancianII; Luiza Drissen Signorelli GermanoIII; Fernanda CeruttiIV; Margareth da Silva OliveiraV
IIMaster’s student,
Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS,
Brazil
IIIUndergraduate
student in Nursing, Pontifícia Universidade Católica do Rio Grande do Sul,
Porto Alegre, RS, Brazil
IVDoctoral student,
Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS,
Brazil
VPhD, Professor,
Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS,
Brazil
ABSTRACT
The objective in this study was to analyze the relation between the use of crack-cocaine and the diagnosis attention deficit hyperactivity disorder. Associations were analyzed between the clinical group of crack-cocaine users and the non-clinical group, taken from the general population, through a sample of 971 participants who answered the Adult Self-Report. Significant differences were found in the presence of the attention deficit hyperactivity disorder diagnosis (p=0.001), such as attention problems (p=0.001), which can be related to changes associated with the search for rewarding situations, such as substance use. This, allied with the impulsiveness in both disorders, would make this association worthy of formulating specific guidelines to maximize the treatment efficacy.
Descriptors: Attention Deficit Hyperactivity Disorder; Crack-Cocaine; Adult Self-Report.
RESUMEN
El objetivo de este estudio es analizar la relación entre el consumo de cocaína crack y el diagnóstico de Trastorno por Déficit de Atención y Hiperactividad. Se analizaron asociaciones entre el grupo clínico de los consumidores de cocaína crack y no clínico de la población general de una muestra de 971 participantes que completaron el Adult Self-Report (ASR). Diferencias significativas fueron encontradas en relación al diagnóstico de Trastorno por Déficit de Atención y Hiperactividad (p = 0,001), como más problemas de atención (p = 0,001), que pueden estar vinculados a una mayor búsqueda de situaciones gratificantes, como el uso de sustancias. Esto, junto a la impulsividad en ambos trastornos, es digno de directrices específicas para maximizar la eficacia del tratamiento.
Descriptores: Trastorno por Déficit de Atención e Hiperactividad; Crack; Adult Self-Report.
Introduction
The annual use of cocaine presents higher prevalence rates in South America (1.3% of the adult population), in comparison with figures in North America. In a recent survey, significant growth can be noted in the use of this illegal substance in Brazil(1).
Crack is a substance deriving from cocaine, whose compulsive use develops in a short time period. It is currently considered a severe public health problem in Brazil, due to the easy access to the substance and the severe damage caused to the user’s quality of life(2). The profile of crack users in the country consists of young people with a mean age of 27.3 years, predominantly male, with low education level and unemployed, and approximately 40% living on the street(2-4). In addition, in research, this population is frequently associated with criminality – thefts, violence and indebtedness with traffickers -, therefore increasing the risk of death by homicide(4).
In Brazil, crack is more frequently consumed in pipes, but aluminum cans are also use, representing a great risk of contamination by heavy metals, besides the human immunodeficiency virus (HIV) and hepatitis C(2). The losses crack causes and the characteristics deriving from its use in the population of users have been addressed in increasingly specific and in-depth studies on the losses associated with its use, as well as ways to grant these individuals quality of life(2).
Problematic cocaine and crack use has been associated with different comorbidities, with the significant presence of Attention Deficit Hyperactivity Disorder (ADHD), which can be related with Substance Use Disorder (SUD) in about 20% of individuals, independently of gender or ethnic origin(5). In other studies, the suggestion is raised that the relation with ADHD can range between 2 and 83% in substance users who seek treatment(6). Researchers suggest that these two diagnoses can result from overlapping risk factors, such as genetic vulnerability(5).
According to the Diagnostic and Statistical Manual of Mental Disorders – DSM 5, ADHD is defined as a persistent and dysfunctional pattern of inattention, which can be associated with symptoms of hyperactivity and impulsiveness. This pattern develops during childhood and can interfere in development. About 5% of the children are diagnosed with ADHDH, and this condition can follow the individual in adult age, especially inattention. About 3% of adults are diagnosed with ADHD(7).
Cocaine users with ADHD can present losses in behavioral self-regulation. In hypotheses, it is indicated that the repetitive dopaminergic activation of the neural circuits through chronic cocaine use can cause losses in inhibitory functions, leading to a loss of control over impulsive behaviors, including the self-administration of cocaine(8).
What the cognitive factors of Cocaine Use Disorder (CUD) are concerned, evidence appoints increased motor and cognitive impulsiveness (i.e., impulsive decision making). ADHD, then, departs from the combination of losses in the reward/motivation system, which can be a key element in this psychopathology, in view of the search for instantaneous rewards and the delay of unpleasant activities. Therefore, in view of overlapping deficits in the processing of rewards, attention and working memory among individuals with ADHD and psychoactive substances, cocaine-addicted individuals with ADHD present significantly higher levels of motor and cognitive impulsiveness(9).
The presence of ADHD in SUD interferes in the prognosis, being related with more cases of relapse and lower treatment compliance(10). Evidence appoints that cocaine users with ADHD who seek treatment feel greater fissure during the days after the onset of treatment and remain abstinent for a shorter period(11). ADHD is associated with school and occupational problems, and the impulsiveness present in the disorder can be a problem, especially in adult age(7). Therefore, Brazilian studies are needed in which this association is investigated, aiming to develop more targeted treatment forms. Therefore, the objective in this study was to analyze the relation between crack use and the ADHD diagnosis through the comparison between a clinical and another non-clinical group.
Method
Participants
A convenience sample was composed, consisting of 971 participants, all adults, between 18 and 59 years of age. The total sample was divided in two groups: clinical (n=407) and non-clinical (n=564). The inclusion criteria for the clinical group, consisting of crack-cocaine users, were: a) being hospitalized at specialized public and/or private health services that attend to patients from the state capital Porto Alegre, RS, Brazil and the Metropolitan Region; b) being between the 7th and 15th day of abstinence from psychoactive substances; c) having completed at least five years of formal education and d) reporting on the use of crack-cocaine as a factor that motivated the search for hospitalization.
The non-clinical group consisted of patients living in the State of Rio Grande do Sul, mainly in the Metropolitan Region of Porto Alegre. The participants were chosen based on the following inclusion criteria: a) adults between 18 and 59 years of age; b) male and female; c) with at least five years of education; d) who were not receiving any psychological or psychiatric treatment and e) who had not been diagnosed with mental disorders.
Instruments
The Adult Self-Report (ASR) was used, which is an Achenbach System of Empirically Based Assessment (ASEBA) scale that specifically targets individuals between 18 and 59 years of age. The use of this self-reported tool is intended to assess adaptive and psychopathological functioning aspects, consists of 126 distinct items and takes about 30 minutes to apply(12).
The instrument is divided in four large evaluation areas, subdivided in scales. The first evaluation area is called scales that assess syndromes (internalizing and externalizing behaviors). The internalizing symptoms correspond to anxiety/depression, isolation/depression and somatic problems; and the externalizing to aggressive and intrusive behaviors and rule-breaking(12).
The second assessment area is called scales that assess current adaptive functioning (family, work, marriage, friendships, education and general adaptive average). The third area refers to scales that assess substance use (tobacco, alcohol, drugs and mean substance use). The fourth and final assessment area, scales guided by the DSM (clinical disorders and personality disorders)(12).
There are specific cut-off points for each scale assessed, which classify the score as normal, borderline or clinical(12). The validity evidence of the ASR was studied to adapt the scale to the Brazilian reality, involving a total sample of 1,444 individuals, divided in three subsamples (general population, chemical addicts and people with clinical or emotional problems). The internal consistency rates between the scales ranged between α=0.70 and α=0.86(13).
Procedures
Approval for the research was obtained from the Research Ethics Committee at Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), under No. 09/04941. The secrecy and anonymity of the participants’ data were guaranteed, and the assessment only took place after the participants had understood the study objectives, accepted to participate and signed two copies of the Free and Informed Consent Form (FICF), one for the participant and the other for the researcher.
The data were collected by psychologists and trained psychology undergraduates. The clinical group consisted of individuals attended at outpatient and inpatient clinics specialized in chemical addiction treatment, who were invited to answer the tools after a screening process to verify the inclusion criteria. The general participants were recruited at the university where the research was developed and at the city’s bus station, after previous authorization to collect the data. All participants were instructed on the tools and signed the FICF.
Data analysis
To analyze the ASR data, first, the Assessment Data Manager (ADM) software was used, a resource to correct the ASEBA(14) scales. Next, the calculated data were exported and analyzed in the Statistical Package for the Social Sciences (SPSS), version 17.0. Descriptive (percentages and standard deviations – sd) and association analyses were developed using Pearson’s chi-squared test, considering the analysis of the adjusted residuals.
Results
Based on the descriptive analysis of the sociodemographic data, considering all participants (N=971), it was evidenced that the majority was male (63.2%), with a higher education degree (49.2%) and an average age in percentage of 31.13% (sd=11.18). In Table 1, the participants’ data are presented, divided between the two groups (clinical and non-clinical).
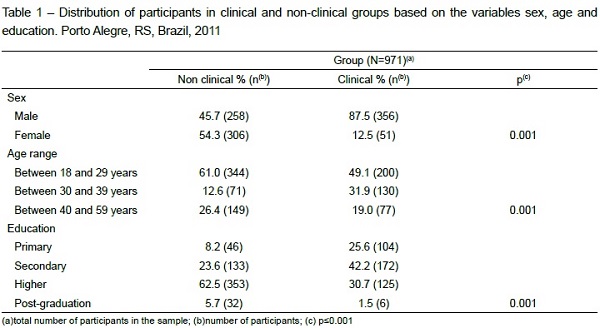
As can be observed in Table 1, the clinical group consisted of 407 crack-cocaine users, with a mean age of 31.55 years (sd=9.60). Most participants were male (87.5%), with finished secondary education (42.3%). The discrepancy between the percentages of the gender variable, in which crack-cocaine is more prevalent among men, was considered and controlled in the statistical analysis. The non-clinical group included 564 participants from the general population, with a mean age of 30.84 years (sd=12.19), mostly female (54.3%), with finished higher education (62.6%).
What the analyses of associations between the clinical and non-clinical groups are concerned, and also with the variable attention problems, most participants in the group of crack-cocaine users (21%; n=85) demonstrated significant involvement in the clinical category (p=0.001), while the participants from the general population (88.6%; n=499) predominantly ranked in the normal category of attention problems (p=0.001).
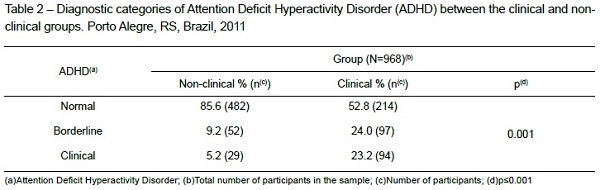
What the ADHD diagnosis is concerned, there were significant differences between the clinical and non-clinical groups (p<0.001), as presented in Table 2. The distribution among the normal, borderline and clinical groups showed the higher prevalence of participants from the non-clinical group (85.6%; n=482) in the normal range of that clinical diagnosis. On the opposite, the borderline (24%; n=97) and clinical (23.2%; n=94) classifications mostly represented crack-cocaine users. The linear-by-linear association indicates that, the higher the severity score of ADHD symptoms, the greater the probability of belonging to the clinical group (p<0.001).
Discussion
The results found in this study confirm the evidence appointed in the literature about the association between ADHD and cocaine use. The results found in this study confirm the evidences appointed in the literature on the association between ADHD and cocaine use. This association can be explained by the sensitivity in the rewarding system, as evidence appoints that individuals with ADHD have less dopamine receptors(15-16). In neuroimaging tests of ADHD patients, neural dissociation is shown between decisions on immediate and postponed reward and orbitofrontal hypo-activation, which would explain the altered responses to the strengthening(17). Thus, these individuals would seek more rewarding situations and this can be directly associated with cocaine use, as appointed in the literature(15-16).
One of the theories that is intended to conceptualize the cognitive functioning of these individuals is the Dualist Model of ADHD, which presents this disorder as a result of executive dysfunctions underlying these dopaminergic disorders. That would explain important changes in the motivation which, in turn, would justify the search for reward and the aversion against delayed rewards(17-18). ADHD in adults is also associated with other executive function deficits, such as working memory, emotional processing, temporal processing and inhibitory control. As ADHD is considered a developmental disorder, most of these symptoms are expected to decrease in adult life. The persisting symptoms seem to be related to the impulsiveness facet. That would be a clear characteristic of ADHD as well as SUD(9).
Impulsiveness is related to inhibitory control errors, which would present deficits in substance users. In a study involving chronic cocaine addicts, losses were found in the frontal lobe functions, which are considered important for behavioral control and regulation, through neuroimaging tests. The environment would serve as a trigger for behaviors: the regulation error, through the frontal lobe, would lead to difficulties in the inhibitory control when the stimulus is present(8).
In addition, the motor and cognitive impulse control is deficient in ADHD patients as well as frequent cocaine users, and worsens when both disorders are associated. The inhibitory control depends on the proper functioning of the frontal lobes, which are related various subtypes of inhibition. The authors speculate that these individuals need more – or perhaps overlapping – circuits in the frontal lobe, so that proper impulse control can be achieved. Therefore, individuals with ADHD and cocaine addiction are more impulsive than individuals without cocaine use due to their dysfunctional executive and reward/motivational circuits(9).
In order to find differences in the impulsiveness characteristics, in another study, neuropsychological and self-reported tests were used in a sample of cocaine users with and without ADHD. In that study, no significant differences were found in the cognitive tests but, using the Barrat Impulsiveness Scale (BIS), it was evidenced that the group of cocaine users with ADHD was significantly more impulsive(9). In evidence, it is appointed that the presence of ADHD can accelerate what is appointed in the Progression Theory of Drugs Use and can be related with impulsiveness. In that theory, it is suggested that the early consumption of legal substances could serve as an entry door for the consumption of more harmful illegal substances. ADHD was significantly more associated with early substance use, including cocaine(10,19), and more associated with severity than substance use in adult age(19-21).
Early marihuana users with attention problems in childhood seem to be more prone to cocaine use during life and can also represent a risk group for the use of other substances(22). Even after controlling for risk variables like early substance use, school difficulties and family problems, the significant results were maintained, indicating that the attention problems in childhood are possibly associated with the risk for cocaine use in adult life. In addition, in a meta-analytic review, evidence was raised from different studies, appointing that the presence of ADHD in childhood is more associated with the development of problematic cocaine use in adult age and that this inference can be causal(23).
Another point to be highlighted is the medication treatment using methylphenidate, the most prescribed drug for ADHD treatment in childhood. This psychostimulant drug can alter the neuronal development trajectory during adolescence(24). Both the methylphenidate and the cocaine act on the dopamine carriers, which is presumed to be the key understanding about the strengthening mechanism of cocaine, as they link up with the transporters and inhibit its reabsorption in the synaptic cleft.
When administered in adolescence but interrupted later, the methylphenidate increases the motivation to self-administer cocaine in animal models, suggesting that the medication should follow its prescription in detail. When self-administered, the cocaine goes directly to the medial frontal lobe. Therefore, this mechanism can act by strengthening and/or motivating the subject to use cocaine again. In animal models, it is shown that the administration of methylphenidate in the pre-treatment phase inhibits the dopamine carriers, reducing the link of the cocaine in these transporters and reducing its impact(24).
Conclusion
In this study, we aimed to analyze the relation between crack-cocaine use and the ADHD diagnosis. The results show a significant association between both conditions, confirming the background literature findings. Various hypotheses are involved in the relation of ADHD and SUD, including greater sensitivity in the reward system, as individuals with ADHD would have less dopamine receivers. Thus, changes would be caused in the motivation and search for rewarding situations and in impulsiveness, which is characteristic of both disorders.
Nevertheless, in the interpretation of the results, the research limitations should be taken into account, with the cross-sectional design and self-reported instruments. Therefore, no cause-and-effect relation can be attributed between the ADHD diagnosis and crack-cocaine use. Instead, inferences only relate to a significant association, which is not as clear as in the group that does not use drugs. In view of these aspects, research is suggested to investigate the theme longitudinally and use other research resources, such as neuroimaging.
In short, it is important to develop studies in which the comorbidities of psychoactive substance users are assessed, as comorbidities like ADHD interfere in the prognosis and treatment of SUD. Hence, investigating ADHD in crack-cocaine users is fundamental to understand individuals, their difficulties and characteristics, which are part of the detoxification and rehabilitation process. It is interesting for health professionals to be able to identify these associations in order to effectively guide the user’s treatment.
References
1. UNODC, United Nations Office on Drugs and Crime. World Drug Report 2013. United Nations publication; 2013. 151 p. (Sales No. E.13.XI.6). [ Links ]
2. Bastos FI, Bertoni N. Pesquisa Nacional sobre o uso de crack: quem são os usuários de crack e/ou similares do Brasil? Quantos são nas capitais brasileiras? Rio de Janeiro (RJ): ICICT; 2014. 228 p. [ Links ]
3. Duailibi LB, Ribeiro M, Laranjeira R. Profile of cocaine and crack users in Brazil. Cad Saúde Pública. 2008 Apr;24(4 Suppl):545-57. [ Links ]
4. Guimarães CF, Santos DVV, Freitas RC, Araujo RB. Perfil do usuário de crack e fatores relacionados à criminalidade em unidade de internação para desintoxicação no Hospital Psiquiátrico São Pedro de Porto Alegre (RS) = Profile of crack users and factors related to criminality at the detoxication ward at Hospital Psiquiátrico São Pedro, Porto Alegre, Brazil. Rev Psiquiatr Rio Gd. Sul. 2008 Feb;30(2):101-8. Portuguese, English. [ Links ]
5. van Emmerik-van Oortmerssen K, van de Glind G, van den Brink W, Smit F, Crunelle CL, Swets M, et al. Prevalence of attention-deficit hyperactivity disorder in substance use disorder patients: a meta-analysis and meta-regression analysis. Drug Alcohol Depend. 2012 Apr;122(1):11-9. [ Links ]
6. van de Glind G, Konstenius M, Koeter MW, van Emmerik-van Oortmerssen K, Carpentier PJ, Kaye S, et al. Variability in the prevalence of adult ADHD in treatment seeking substance use disorder patients: Results from an international multi-center study exploring DSM-IV and DSM-5 criteria. Drug Alcohol Depend. 2014 Jan;134(1):158-66. [ Links ]
7. American Psychiatric Association (APA). Manual diagnóstico e estatístico de transtornos mentais. 5 ed. Porto Alegre (RS): Artmed; 2014. 976 p. [ Links ]
8. Fillmore MT, Rush CR. Impaired inhibitory control of behavior in chronic cocaine users. Drug Alcohol Depend. 2002 May;66(3):265-73. [ Links ]
9. Crunelle CL, Veltman DJ, van Emmerik-van Oortmerssen K, Booij J, van den Brink W. Impulsivity in adult ADHD patients with and without cocaine dependence. Drug Alcohol Depend. 2013 Apr;129(1):18-24. [ Links ]
10. Szobot CM, Romano M. Co-ocorrência entre transtorno de déficit de atenção/hiperatividade e uso de substâncias psicoativas. [Co-occurency between attention deficit hyperactivity disorder and psychoactive substances]. J Bras Psiquiatr. 2007 Jan;56(1 Suppl):39-44. Portuguese. [ Links ]
11. de los Cobos JP, Siñol N, Puerta C, Cantillano V, Zurita CL, Trujols J. Features and prevalence of patients with probable adult attention deficit hyperactivity disorder who request treatment for cocaine use disorders. Psychiatry Res. 2011 Jan;185(1):205-10. [ Links ]
12. Achenbach TM, Rescorla LA. Manual for the ASEBA Adult Forms & Profiles. Burlington, (VT): University of Vermont, Research Center for Children, Youth & Families; 2003. 216 p. [ Links ]
13. Lucena-Santos P, Moraes JFD, Oliveira MS. [Analysis of the factor structure of syndromes scales of ASR (Adult Self-Report)]. Interam J Psychol. 2014 Jan;48(3):252-64. Portuguese. [ Links ]
14. Bolsoni-Silva AT, Marturano EM. Evaluation of group intervention for mothers/caretakers of kindergarten children with externalizing behavioral problems. Interam J Psychol. 2010 Jan;44(3):415-21. [ Links ]
15. Balconi M, Finocchiaro R, Campanella S. Reward sensitivity, decisional bias, and metacognitive deficits in cocaine drug addiction. J Addict Med. 2014 Nov-Dec;8(6):399-406. [ Links ]
16. Volkow ND, Wang GJ, Newcorn JH, Kollins SH, Wigal TL, Telang F, et al. Motivation deficit in ADHD is associated with dysfunction of the dopamine reward pathway. Mol Psychiatry. 2011 Nov;16(11):1147-54. [ Links ]
17. Wilbertz G, van Elst LT, Delgado MR, Maier S, Feige B, Philipsen A, et al. Orbitofrontal reward sensitivity and impulsivity in adult attention deficit hyperactivity disorder. Neuroimage. 2012 Mar;60(1):353-61. [ Links ]
18. Sonuga-Barke EJ. The dual pathway model of AD/HD: an elaboration of neuro-developmental characteristics. Neurosci Biobehav Rev. 2003 Nov;27(7):593-604. [ Links ]
19. Dunne EM, Hearn LE, Rose JJ, Latimer WW. ADHD as a risk factor for early onset and heightened adult problem severity of illicit substance use: An accelerated gateway model. Addict Behav. 2014 Dec;39(12):1755-8. [ Links ]
20. Daigre C, Roncero C, Grau-López L, Martínez-Luna N, Prat G, Valero S, et al. Attention deficit hyperactivity disorder in cocaine-dependent adults: A psychiatric comorbidity analysis. Am J Addict. 2013 Sep-Oct;22(5):466–73. [ Links ]
21. Delavenne H, Ballon N, Charles-Nicolas A, Garcia FD, Thibaut F, Lacoste J. Attention deficit hyperactivity disorder is associated with a more severe pattern of cocaine consumption in cocaine users from French West Indies. J Addict Med. 2011 Dec;5(4):284-8. [ Links ]
22. Galéra C, Pingault JB, Fombonne E, Michel G, Lagarde E, Bouvard MP, et al. Attention problems in childhood and adult substance use. J Pediatr. 2013 Dec;163(6):1677-83. [ Links ]
23. Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin Psychol Rev. 2011 Apr;31(3):328-41. [ Links ]
24. Baskin BM, Dwoskin LP, Kantak KM. Methylphenidate treatment beyond adolescence maintains increased cocaine self-administration in the spontaneously hypertensive rat model of attention deficit/hyperactivity disorder. Pharmacol Biochem Behav. 2015 Apr;131(1):51-6. [ Links ]
Received: Jan.
18th 2016 Corresponding Author: 1This research was supported by Conselho Nacional
de Desenvolvimento Científico e Tecnológico (CNPq), Brazil, process
#306661/2009-8.
Accepted: Jan. 23rd 2017
Margareth da Silva Oliveira
Pontifícia Universidade Católica do Rio
Grande do Sul
Av. Ipiranga, 6681, prédio 11, sala 927
CEP: 90619-900, Porto Alegre, RS, Brasil
E-mail: marga@pucrs.br











 texto en
texto en 


