Services on Demand
article
Indicators
Share
SMAD. Revista eletrônica saúde mental álcool e drogas
On-line version ISSN 1806-6976
SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. port.) vol.15 no.3 Ribeirão Preto July/Sept. 2019
http://dx.doi.org/10.11606/issn.1806-6976.smad.2019.151548
REVIEW ARTICLE
Mental health consultation-liaison from the perspective of the primary health care team*
Ana Carolina Guidorizzi ZanettiI; Sueli Aparecida Frari GaleraII; Jacqueline de SouzaIII; Kelly Graziani Giacchero VedanaIV; Edilaine Cristina da Silva Gherardi-DonatoV; Margarita Antonia Villar LuisVI; Lisa Laredo de CamargoVII; João Mazzoncini de Azevedo MarquesVIII
IUniversidade de São Paulo, Escola de Enfermagem de
Ribeirão Preto, PAHO/WHO Collaborating Centre for Nursing
Research Development, Ribeirão Preto, SP, Brazil
IIUniversidade de São Paulo, Escola de Enfermagem de
Ribeirão Preto, PAHO/WHO Collaborating Centre for Nursing
Research Development, Ribeirão Preto, SP, Brazil
IIIUniversidade de São Paulo, Escola de Enfermagem de
Ribeirão Preto, PAHO/WHO Collaborating Centre for Nursing
Research Development, Ribeirão Preto, SP, Brazil
IVUniversidade de São Paulo, Escola de Enfermagem de
Ribeirão Preto, PAHO/WHO Collaborating Centre for Nursing
Research Development, Ribeirão Preto, SP, Brazil
VUniversidade de São Paulo, Escola de Enfermagem de
Ribeirão Preto, PAHO/WHO Collaborating Centre for Nursing
Research Development, Ribeirão Preto, SP, Brazil
IVUniversidade de São Paulo, Escola de Enfermagem de
Ribeirão Preto, PAHO/WHO Collaborating Centre for Nursing
Research Development, Ribeirão Preto, SP, Brazil
VIIUniversidade de São Paulo, Escola de Enfermagem de
Ribeirão Preto, PAHO/WHO Collaborating Centre for Nursing
Research Development, Ribeirão Preto, SP, Brazil / Scholarship holder at the Coordenação de Aperfeiçoamento
de Pessoal de NÃvel Superior (CAPES), Brazil
VIIIUniversidade de São Paulo, Faculdade de Medicina de Ribeirão Preto, Ribeirão Preto, SP, Brazil
ABSTRACT
OBJECTIVE: analyze the consulting and liaison activities carried out by professionals specialized in mental health from the perspective of the PHC.
METHOD: an exploratory study, realized in five Family Health centers, in a municipality in the countryside of São Paulo, in 2010. Data were collected through interviews, which were submitted to content analysis.
RESULTS: as consultation-liaison activities were shown as a space for mutual learning between specialists in psychiatry and mental health and PHC teams.
CONCLUSION: it is recommended to increase the number of activities that articulate mental health actions with PHC, such as consultation and liaison, in order to favor the sensitivity of the teams to the demands of mental health in the PHC and consolidation of the integral care.
Descriptors: Mental Health; Primary Health Care; Family Health Strategy; Family Health.
Introduction
The conditions for the Unified Health System to be consolidated as a health model, goes through the effective implementation of the Primary Health Care (PHC) network, particularly through the Family Health Strategy (FHS). Within the work process of the FHS, the concept of territorialization, a field that delimits the action of the Health Unit regarding space and population, is fundamental(1). The professionals of the FHS team should carry out the active search of the people inserted in a defined territory, identifying those with health problems, including psychosocial problems and mental disorders properly(1). It is recognized that in PHC the prevalence of psychosocial problems is of the order of 40% and of mental disorders, 25%(2). A study carried out in Rio Grande do Sul showed that the prevalence of mental disorders of individuals attended in a PHC service was approximately 51%(3). For most of these individuals the only care offered is the one performed by the professionals of the FHS teams(3).
Studies show that all mental health services/professionals, even in high-income countries with universal health systems, serve a maximum of 3% of the population annually, while the annual prevalence of mental disorders is around 30% which points out important gaps between the supply and demand of care in this area(4-5). The World Health Organization (WHO) recognizes that PHC services can function as important articulators of Mental Health (MH) networks, since, because of their proximity to communities, families and individuals, they have the potential to detect more mental health problems and provide appropriate interventions to the unique and contextual characteristics of each situation (including through referral to specialized services when necessary)(6-7).
However, studies show that PHC teams detect approximately 50% of people with mental health problems within their territory and that even when the problem is detected, the appropriate treatment rate is low(6). In Brazil, despite the efforts made in the last years, the professionals of the FHS teams often still lack capacity for the development of actions in mental health. In addition, there are difficulties in the capacity to develop actions that extend to the wider social space(8).
Since 1999, in a city in the state of São Paulo, health professionals, linked to the medical and nursing courses of a public university, began actions of integrated mental health care in the FHS services, a care characterized by periodic meetings and facilitation of communication between the professionals of these services and professionals specialized in mental health, aiming to provide support to the FHS teams in the management of situations involving psychosocial problems and/or mental disorders and, consequently, in their mental health training.
The theoretical-practical references for these integrated mental health care actions were British, Canadian and North American experiences in mental health counseling and liaison in PHC(9-12). This concept of consultation and connection in mental health in PHC is characterized by: Periodic meetings between professionals of the PHC teams and specialized professionals, which can include joint patient care and discussion of cases and topics requested by these teams; Communication facilitated by professionals also through telephone and/or internet contacts; Assistance from mental health professionals in referral of patients to specialized care outside PHC and in providing care information to the primary care team. As such, this model of consultation and liaison in PHC maintains the central role of PHC professionals/teams as providers of care for the vast majority of people monitored at this level. The professionals specialized in mental health described in the literature as actuators of this model are diverse: nurses, psychologists, doctors or social workers(6,9,11,13-15).
For example, the role of nursing professionals as mental health consultants has been in place since the 1970s in developed countries and is still in the process of being consolidated in developing countries(16). It is believed that the involvement of the nurse in consulting activities can facilitate the resolution of less complex issues involving mental health, speed up the identification of cases of mental disorders with greater accuracy, favor the provision of less complex care, quality of life of the family's health service user and improve articulation with other health services. Also, it can promote the training and supervision of the nursing team and the recognition of the family and social bonds established between health professionals and the community(16-17).
In Brazil, starting in 2003, the first guidelines for the approximation of mental health with the FHS began, with the publication of the document the Supporting Matrix of Mental Health to the FHS teams. The Matrix Health Support establishes the model of consultation and linkage based on the therapeutic link. This model values therapeutic actions within the territory, emphasizes the singularity of the individual, avoiding the fragmentation of care, and considers the family, socio-cultural, economic and biopsychosocial dimensions that involve the daily actions to promote mental health(18).
In the national and international literature there is recognition that, although the health management agencies in Brazil and in the world point out that FHS teams play a key role in the prevention and maintenance of mental health problems, there are gaps in knowledge about how FHS teams are articulated to meet the demands of mental health(7,19-20).
While there is an optimistic outlook for counseling and liaison activities between a specialized mental health service for FHS teams facing the possibilities of facilitating access, early diagnosis of problems, initiation of appropriate and immediate person-centered interventions and creation of a non-stigmatizing environment, FHS professionals do not always feel or are prepared to meet mental health need.
The justifications for this study were the frequent difficulties described by PHC teams/professionals to manage mental health problems and the experience gained in the consulting and liaison work developed in a city in the interior of São Paulo to deal with this issue.
Objectives
This study aimed to analyze the consulting and liaison activities carried out by professionals specialized in mental health and psychiatry from the perspective of the FHS professionals.
Method
This is an exploratory descriptive study, carried out with five FHS teams from the city of Ribeirão Preto, linked to the University of São Paulo, in 2010. The professionals of these teams had access to consulting and liaison activities, in which a physician participated and a nurse, specializing in psychiatry and mental health. Consultancy and liaison activities covered: Discussion of themes and cases; Joint care, including home visits; Attendance of specialized professionals without simultaneous participation of PHC professionals; Discussion of organizational aspects and the work process of the FHS team; Rapid referral to specialized secondary level outpatient clinic where the psychiatrist and mental health nurse also worked, if so agreed with the PHC team; Facilitation of referral to other specialized services, such as Day-Hospital, Psychosocial Care Center for Alcohol and Drug Users and full psychiatric hospitalization.
The project was approved by the Research and Ethics Committee on July 15, 2009, Protocol No. 17/2009, in accordance with resolution CNS 466/96(21). The health professionals were recruited in the Family Health centers after approval of the project by the research ethics committee. Fifty-five professionals from these five FHS teams were invited to participate in the study. Seven declined to attend and one disconnected from service before their interview was scheduled. Then, a final convenience sample consisted of 50 health professionals.
Data was collected using a structured script containing the sociodemographic variables (gender, age, institution where the training took place, training in the area of mental health and psychiatry, place and current working time) and a semi-structured interview script containing the following guiding question: How do you feel about your consulting and liaison work in mental health and psychiatry at your service?
The data was obtained through interviews, at a pre-determined time by the participant, in rooms reserved in said nuclei. Firstly, the objectives and nature of the study were clarified and after the agreement and signing of the informed consent, the interview was started. The average interview time was thirty minutes and at the end, the interviewer was available for additional clarification. The data collection period was from July 2009 to January 2010.
The interviews were recorded, transcribed and the data that could identify the professional was withdrawn. After this step, the data was submitted to content analysis according to Bardin(22). The interviews were read in order to identify similarities and differences in the contents expressed by the participants, aiming to identify the consulting and liaison activities carried out by professionals specialized in mental health and psychiatry from the perspective of the family health strategy teams. The codification of the units of meaning was carried out by two researchers with the consulting and liaison actions described in previous studies(9-11). After this step the codes were grouped into the following categories: mental health demands in the FHS and the role of consulting and liaison as a support element in the FHS. The parameters for the analysis of the results were the recommendations for the operationalization of the matrix support in primary health care(23-24).
Results
Of the 50 (100%) professionals of the FHS teams, 19 (38%) were community health agents, women, 39 (78%), mean age 34 years (SD = 8.6), average 48 months (SD = 35.5). The totality of those investigated had no prior training as a mental health specialist. This can be seen in Table 1.
The following two categories of analysis are extracted from the participants' testimonies: mental health demands in the FHS and the role of counseling and liaison in the role of support in FHS.
The first category of analysis called mental health demands in the FHS showed that FHS professionals are faced with various mental health demands of health service users. These demands are related to the needs of the users in view of the high number of cases and problems inherent in the various diagnoses of mental disorders (depression, anxiety, substance use, schizophrenia, bipolar disorder, dementia, etc.) as follows:
...many cases of depression and anxiety.(RESIDENT); ...the problems or situations are several. [...] the most common are depression and anxiety disorder. (DOCTOR); problems like depression, anxiety too, and a lot of things.(COMMUNITY HEALTH AGENT); ...about 70% of the population has some mental health related demand. (NURSE)
The testimonies also show that there are situations of social vulnerability such as low self-esteem, poor access to information, difficulties in interaction among family members, domestic and conjugal violence, child abuse and neglect, and suicide attempts and / or suicide which demand support from a health professional with specialization in psychiatry and mental health.
physical and verbal aggression from mother to child, family conflicts.(COMMUNITY HEALTH AGENT); ...so the problems are many, people who have a problem with self-esteem, people who have little information. (COMMUNITY HEALTH AGENT)
In the testimonies it is verified that the consulting and liaison activities take place through direct contact of the mental health specialists in the consultations together with the service team. The speeches show that health professionals recognize consulting and liaison as an element of support in the FHS. This recognition was found in all professional categories investigated, irrespective of the level of training.
Thus, it is understood that consulting and liaison activities from the perspective of PHC professionals increased their safety in handling mental health demands, contributed to their continued education, expanded their repertoire of theoretical and practical knowledge, and favored their the resolving ability.
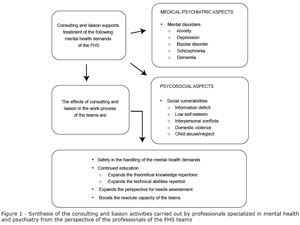
....over the years we have been prepared by consulting and this is very important. (NURSE); ... in the beginning I was very insecure, (...) but with the consultancies here, both in the internship and in the Emergency Unit, today I have more security, much more than when I started.( RESIDENT); ...with consulting and liaison we learn to interview, handle, adjust the medicines, I think it helps a lot, it makes a lot of difference.(DOCTOR); We start to have a different look at mental health in the FHS (NURSE), can be verified in Figure 1.
Discussion
When analyzing the consulting and liaison activities carried out by professionals specialized in mental health from the perspective of the professionals of the FHS, the participants recognize the activities of consultation and liaison as essential to assist in the management of both specific mental health demands (such as disorders mental disorders and their manifestations), as well as situations of social vulnerability. The activities of counseling and liaison stimulated the therapeutic actions that valued the singularities of the people, helping to think about actions that deal not only with the biological dimension and with psychiatric medical diagnosis, but also with social aspects (family, neighborhood, economic aspects, etc.) and psychological (the subjectivity, the experience lived by the person). The results corroborate other studies that emphasize the biopsychosocial, holistic and people-centered character that the matrix support has the power to take over(20,26). For example, a study that evaluated the matrix support in mental health in the city of Porto Alegre, in two FHS teams, showed that this support favored the qualification of the teams in the medical monitoring, clinical evaluation and discussion of user needs, among other activities(26). Thus, the consulting and liaison activities carried out by professionals specialized in mental health and psychiatry from the perspective of the FHS professionals can point to the potential of expanding the technical capacity of health teams in FHS, corroborating previous studies(25-27).
Regarding the high demand of users who seek the FHS for mental health treatment, our findings are in agreement with the multicenter study conducted in 14 countries and coordinated by the World Health Organization (6), which showed that, on average, 24% of people cared for in primary care had at least one current mental disorder and another 9% had clinically significant sub-syndromic conditions. According to the testimonies, the professionals of the FHS teams found that they need permanent education to increase their theoretical and technical knowledge and their abilities to manage mental health problems due to the high demand of people with these problems that they face day to day.
It is noteworthy that of the 50 (100%) participants, 19 (38%) were community health agents and constitute a significant portion of mental health professionals who are closer to the users. On the other hand, it is recognized that community workers still lack the skills to deal with people with mental disorders. The lack of training of health professionals to deal with mental health problems can produce psychic suffering and compromise the intervention's resolution(7).
According to health care guidelines in the FHS, care must be expanded and should take place in the social space of the individual. In this area, comprehensive care and psychosocial rehabilitation are some of the presuppositions of psychosocial care that allow the mental health actions carried out in the FHS to be organized. This organization should involve the professionals specialized in the orientation, discussion and proposal of interventions to maintain the care of the FHS teams (26). Thus, it is expected that psychiatry and liaison counseling can play a key role in the integrality of mental health care.
Conclusion
Consulting and liaison activities have proved to be a mutual learning space between psychiatric and mental health specialists and FHS staff. It is recommended to increase the number of activities that articulate mental health actions with the FHS, such as counseling and liaison, in order to favor the sensitivity of the teams to the demands of mental health in the FHS and consolidation of the integral care. In addition, such activity has the potential to promote interdisciplinarity in daily work in mental health services and to consolidate more powerful and resolute work processes. However, consulting and liaison are challenging approaches, as they constantly question the boundaries between levels of health care, knowledge, practices, and goals of health professionals, among others.
References
1. Barban EG, Oliveira AA. O modelo de assistência da equipe matricial de saúde mental no Programa Saúde da Família do município de São José do Rio Preto. Arq Cienc Saúde. 2007;14(1):54-65. [ Links ]
2. Kate N, Craven M, Crustolo AM, Nikolaou L, Allen C. Integrating mental health services within primary care - a Canadian Program. Gen Hosp Psychiatry. 1997;19:324-32. [ Links ]
3. Gonçalves DM, Kapczinski F. Prevalência de transtornos mentais em indivíduos de uma unidade de referência para Programa Saúde da Família em Santa Cruz do Sul, Rio Grande do Sul, Brasil. Cad Saúde Pública. [Internet]. set 2008 [Acesso 12 fev 2018]; 24(9):2043-53. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2008000900010&lng=en. http://dx.doi.org/10.1590/S0102-311X2008000900010. [ Links ]
4. Goldberg D. Implications of epidemiological findings for the management of mental disorders encountered in primary care settings. Europ Psychiatry. 1997;12(suppl 2):56s-62s. https://doi.org/10.1016/S0924-9338(97)80208-8 [ Links ]
5. Einseberg L. Public Health Importance. In: Jenkins R, Ustun TB, editors. Preventing Mental Illness: Mental Health Promotion in Primary Care. Chichester (England): John Wiley & Sons; 1998. p.141-53. [ Links ]
6. Organização Mundial da Saúde. Relatório sobre a saúde no mundo, 2001. Saúde Mental: nova concepção, nova esperança. Lisboa; 2002. [ Links ]
7. Gama CAP, Campos RO. Saúde mental na Atenção Básica- Uma pesquisa bibliográfica exploratória em periódicos de saúde coletiva (1997-2007). Cad Bras Saúde Mental. out/dez 2009;1(2):112-31. [ Links ]
8. Nunes M, Jucá VJ, Valentim CPB. Ações de saúde mental no Programa Saúde da Família: confluências e dissonâncias das práticas com os princípios das reformas psiquiátrica e sanitária. Cad Saúde Pública. out 2007;23(10):2375-84. [ Links ]
9. McWhinney IR. Philosophical and Scientific Foundations of Family Medicine (Chapter 5). In: Textbook of Family Medicine. New York (USA): Oxford University Press; 2003. [ Links ]
10. Borrel-Cárrio F, Suchman AL, Epstein RM. The Biopsychosocial Model 25 years later: principles, practice and scientific inquiry. Ann Fam Med. 2004; 2:576-82. [ Links ]
11. McDaniel SH, Hepworth J, DohertyWJ. Terapia Familiar Médica: um enfoque biopsicossocial às famílias com problemas de saúde mental. Porto Alegre; 1994. [ Links ]
12. Azevedo-Marques, J.M. Detecção e diagnóstico de transtornos mentais pela equipe de saúde da família. Tese [Doutorado]. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo; 2009. [ Links ]
13. - Gillies D, Buykx P, Parker AG, Hetrick SE. Consultation liaison in primary care for people with mental disorders. Cochrane Database Syst Rev. 2015 Sep 18;(9):CD007193. doi: 10.1002/14651858.CD007193.pub2. Review. PubMed PMID: 26384252. [ Links ]
14. - Moscovici L, Azevedo Marques JM, Zuardi AW. 2016: Integrated mental healthcare: outcomes from Brazilian primary care. Eur J Person Centered Healthcare. 2016;4:669-74. [ Links ]
15. Moscovici L, Azevedo-Marques JM, Bolsoni LM, Rodrigues-Junior AL, Zuardi AW. Impact of different approaches of primary care mental health on the prevalence of mental disorders. Prim Health Care Res Dev. 2017 Dec 5;19(3):256-63. [ Links ]
16. Sharrock J, Grigg M, Happell B, Keeble-Devlin B, Jennings S.The mental health nurse: a valuable addition to the consultation-liaison team Int J Ment Health Nurs. 2006 Mar;15(1):35-43. [ Links ]
17. Martin AC, Davis LL. Mental health problems in primary care: a study of nurse practitioners' practice. Nurse Pract. 1989;14(10):46-7,50-6. [ Links ]
18. Ministério da Saúde (BR). Secretaria de Atenção à Saúde, Coordenação de SM e Coordenação da Gestão da AB. SM e AB - O vinculo e o diálogo necessários - Inclusão das ações de SM na AB. Circular conjunta n. 01/03 de 13/11/2003. [ Links ]
19. Munari DB, Melo TS, Pagotto V, Rocha BS, Soares CB, Medeiros M. Saúde Mental no contexto da atenção básica: potencialidades, limitações, desafios do Programa Saúde da Família. Rev Eletr Enferm. 2008;10(3):784-95. Disponível em: http://www.fen.ufg.br/revista/v10/n3/v10n3a24.htm [ Links ]
20. Lucchese R, Oliveira AGB, Conciani ME et al. Mental health and the Family Health Program: pathways and obstacles in a necessary approach. Cad Saúde Pública. 2009;25(9):2033-42. [ Links ]
21. Ministério da Saúde (BR). Conselho Nacional de Saúde. Resolução nº 196/96. Dispõe sobre normas de pesquisa envolvendo seres humanos. Brasília: MS; 1996. 24 p. [ Links ]
22. Bardin, L. Análise de Conteúdo. Lisboa (PT): Edições 70; 1977. [ Links ]
23. Campos GWS, Domitti AC. Apoio matricial e equipe de referência: uma metodologia para gestão do trabalho interdisciplinar em saúde. Cad Saúde Pública. 2007;23(2):399-407. [ Links ]
24. Cunha GT, Campos GWS. Apoio Matricial e Atenção Primária em Saúde. Saúde Soc. 2011;20(4):961-70. [ Links ]
25. Figueiredo MD, Campos RO. Saúde Mental na atenção básica à saúde de Campinas, SP: uma rede ou um emaranhado?. Ciênc Saúde Coletiva. fev 2009; [Internet]. [Acesso 12 fev 2018] ; 14(1):129-38. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1413-81232009000100018&lng=en. http://dx.doi.org/10.1590/S1413-81232009000100018. [ Links ]
26. Mielke FB, Olchowsky A. Saúde mental na Estratégia Saúde da Família: avaliação de apoio matricial. Rev Bras Enferm. nov-dez. 2010;63(6):900-7. [ Links ]
27. Thielke S, Vannoy S, Unützer J. Integrating Mental Health and Primary Care. Primary Care: Clinics in Office Practice. 2007;34:571-92. [ Links ]
Received: May 11th 2017 Corresponding Author:
Corresponding Author:
Ana Carolina Guidorizzi Zanetti
E-mail: carolzan@eerp.usp.br
Accepted: Dec 7th 2018











 text in
text in