Serviços Personalizados
artigo
Indicadores
Compartilhar
SMAD. Revista eletrônica saúde mental álcool e drogas
versão On-line ISSN 1806-6976
SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. port.) vol.16 no.1 Ribeirão Preto jan./mar. 2020
http://dx.doi.org/10.11606/issn.1806-6976.smad.2020.160754
ORIGINAL ARTICLE
Characteristics of users diagnosed with depressive disorder undergoing treatment at a Psychosocial Care Center
Lorraine Garbellini Barbosa LimaI ; Ariana Elite dos SantosII
; Ariana Elite dos SantosII ; Bruna Lopes Cardoso dos SantosI
; Bruna Lopes Cardoso dos SantosI ; Luiz Jorge PedrãoI
; Luiz Jorge PedrãoI
IUniversidade de São Paulo, Escola de Enfermagem de Ribeirão Preto, PAHO/WHO Collaborating Centre for Nursing Research Development, Ribeirão Preto, SP, Brazil
IIUniversidade Federal da Paraíba, Departamento de Fonoaudiologia, João Pessoa, PB, Brazil
ABSTRACT
OBJECTIVE: to describe the profile of users diagnosed with depressive disorder undergoing treatment at a psychosocial care center in a city in São Paulo state, Brazil.
METHOD: quantitative, descriptive, exploratory, and epidemiological. Data were collected from the records of patients treated in the selected period, compiled on a Microsoft Excel 2016 sheet and analyzed by the statistical software Stata 16.
RESULTS: prevalence of females, mean age of 48 years old, no partners, no significant variation in family history, educational level that allows for entering the labor market, no comorbidities, no use of chemical substances and no significant variation in terms of suicidal ideation.
CONCLUSION: the analysis of variables allowed for better understanding the characteristics of users, which can contribute to more appropriate care planning for this population.
Descriptors: Psychiatric Nursing; Psychiatric; Mental Health; Depressive Disorder.
Introduction
Mental disorders are chronic noncommunicable diseases. They represent a global health problem and a threat to human development(1). According to the fifth edition of the "Diagnostic and Statistical Manual of Mental Disorders" (DSM-V), a mental disorder is defined as a behavioral pattern that occurs in an individual and is associated with significant increased risk for suffering and/or disability in his or her life, that is, individuals who suffer from a disorder may develop disabilities that will have negative consequences, both professionally and personally(2).
DSM-V provides clear descriptions of diagnoses and the "International Classification of Diseases" (ICD 10), published by the World Health Organization (WHO), divides disorders into categories and subcategories. Together they can guide mental health professionals and researchers regarding the studies and planning of the care required by their target patients(3-4).
As one of the divisions provided by ICD 10, mood is a prolonged state that influences one's personality and functioning in life. Some mood variations are part of human existence(5). The problem arises when an individual's mood is abnormal, as it interferes negatively with other components of his or her life. Thus, a mood and/or affective disorder is the one the main symptom of which is change in a person's mood that is detrimental to his or her physical and/or mental health(5). The factors that can trigger such disorder vary from biological to psychological and sociocultural dimensions, and it is important to point out the identification of psychosocial aspects that have preceded the clinical condition(6).
The risk of an individual's having the disorder in question is 8% during his or her lifetime and some reports have shown that up to 48% of North-Americans have had one or more episodes of mood swings at some time, which can impact on the production and development of a country, since, among North-Americans, those diagnosed with a depressive mood had 7.7-fold greater impairment in social, family and professional functional performance than those who had no depressive signs(7).
WHO reports that depression is currently a major public-health problem, and it is considered a serious recurring disorder that leads to important functionality loss. Worldwide, it is estimated that over 300 million people live with depression (an increase of over 18% between 2005 and 2015). In the Americas, the number of people affected is approximately 50 million, and that is considered to be the fourth most important disease to cause incapacity as it results in loss of quality of life(8).
In Brazil, in the mid-1970s, the Psychiatric Reform process gained strength. Its goal was to overcome the then existing asylum model and seek improvements in care-provision conditions for people with mental disorders. New devices were created at the time, and they still have been designed every day in order to contribute to the construction of new places that are not focused on the asylum model(9).
The National Mental Health Policy (PNSM), supported by Law 10.216/02, has consolidated an open, community-based mental health care model to ensure the free movement of people with mental disorders through services and communities as well as to provide care based on resources offered by such individuals(10).
Then, there was the creation of Psychosocial Care Centers (CAPs), which represent the main strategy for the organization of mental health services, since they broaden the concept of clinical care and strengthen users' socialization processes by utilizing their own environment as a space for social living in order to achieve diversified development, thus differing from office practice(11).
According to Decree no. 336/GM, established in 2002 by the Ministry of Health, CAPs comprise service modalities according to population coverage, and they serve the population in their territory on a daily basis by providing clinical monitoring and psychosocial rehabilitation to individuals with mental suffering. They have a multidisciplinary team that provide care for individuals and/or groups, therapeutic workshops, home visits, family care and community activities, among other services(12).
The World Health Organization (WHO) recommends that in order to make mental health care more appropriate, it is necessary to invest in the production of concrete data on existing services and resources with the purpose to define and design public strategies, that is, it is necessary to invest in epidemiological studies as they are very useful tools, and the results of such studies contribute for the management of care to advance in terms of accessibility, humanization and health promotion(3,13).
Epidemiological studies on mental disorders at recent times have provided a broader understanding of their occurrence and have contributed to an assessment of the possible direct and indirect consequences of illness and impairment in individual, family and social functioning(14).
Epidemiological knowledge of mood disorders complements clinical research, which provides amplitude and temporal dimension to the clinical picture. Such information is of utmost importance for a proper understanding of the natural history of depression. It also provides information on other aspects of depressive illness such as risk and prognostic factors and historical trends(13).
Thus, the importance of the study on depressive disorders is remarkable, since by analyzing the characteristics of service users, it is possible to offer contributions to a better direction as to the type of mental health care that can be provided, as well as to future research, especially that related to Psychosocial Care Centers (CAPs).
Thus, this study aimed to describe the profile of users of a Psychosocial Care Center in a city in São Paulo state.
Method
This is a quantitative, cross-sectional, descriptive, exploratory and epidemiological study. This design uses the quantitative approach, through statistical methods that utilize the relative distribution of the data obtained and a descriptive analysis that enables the reduction, summarization and organization of information(14).
The choice for a non-experimental design is justified by the need to collect descriptions about the variables that will enable a sociodemographic evaluation as well as the understanding of the relationship between the variables studied.
Psychosocial Care Center (CAPS) III "Dr. André Santiago" was chosen because it serves the whole municipality in question, and it is more consolidated in terms of the local mental health care. In addition, the service is considered to be the best suited to accomplish the psychosocial rehabilitation that is so widespread in the Psychiatric Reform Movement.
CAPs III provides care to people in psychotic crises, offering them means of recovery through multidisciplinary care. The unit operates on an intensive basis, 24 hours a day, serving the entire area covered by the municipality. It features two flow elements: to District Basic Health Units and other Mental Health Units with their specificities. Users treated at the site are referred to the hospital, for longer full-time hospitalization, only if their conditions cannot be controlled by the resources existing in the service.
In the service, there are five beds for permanence lasting up to seven continuous days or ten discontinuous days. Other services provided comprise workshops for the social inclusion and rehabilitation of patients with mental problems requiring a more intensive regime, Family School activities to integrate families into treatments and to address the difficulties faced with the disorder, external care and referral to Basic and District Health Units for the evaluation of urgent psychiatric cases, support to the Medical Regulation Center for monitoring cases regulated at the District Units or with indication for psychiatric hospitalization, outpatient follow-up for patients who have undergone intensive care and have not yet had their return appointments scheduled at the regionalized referral units.
This study is an amendment to the project entitled "Characteristics of users treated at a level-III Psychosocial Care Center (CAPs III) in the city of Ribeirão Preto", evaluated and approved by the Ethics Committee for Human Research of the University of São Paulo at Ribeirão Preto College of Nursing (CEP/EERP/USP), with registration number CAAE 71050617.8.0000.5393. In that project, the sample consisted of the medical records of users at CAPs III, in the city of Ribeirão Preto, São Paulo state, who had been treated at the site from May 2013 to May 2015.
The medical records were selected from a list provided by the service with all HYGIA identification numbers (this is a user's medical record identification number linking all the units in the care-provision network between municipalities and states) of users who entered the service at the period of time chosen for collection. After the list was made available, a data collection form was designed containing the following information: HYGIA number, full name, date of birth, gender, marital status, education, profession, family history of psychiatric illness, diagnosis, comorbidities, use of chemical substances, suicidal ideation, presence and duration of night care provision at the service, referral and coverage area. The data were collected by students from the Ribeirão Preto College of Nursing, of whom one was a doctoral student and three were undergraduate students. Collection took place on site in five periods distributed on weekdays, in an appropriate room for that purpose until all the data were obtained from the medical records selected and subsequently made available for analysis.
From the total of 2,000 users whose HYGIA numbers were available on a list provided by the service, 1,594 records were found. The reason for not locating 406 records was the fact that the service had not yet adhered to the computerized electronic recording system, which made it difficult to find such records even with help from the service's employees.
Furthermore, because it was the analysis of medical records that contained, in their structure, multiple choice questionnaires and descriptions made by several professionals, in addition to limitations to the information, it was not possible to make a further search.
Thus, this project was developed based on the data collected for the larger project and submitted to CEP/EERP/USP as an amendment, in compliance with the norms established by Resolution 466/12 of the National Health Council. As risks from the entire established procedure were not expected, since it was a search on medical records, a request was made for waiving the use of informed consent.
As a minimum risk, the identification of users and the disclosure of the information on their medical records can be considered, but since the records were handled in compliance with all ethical standards in terms of confidentiality regarding the users' identities, such risk can be disregarded. Even so, in case any information leaked, corrective actions were taken after being discussed among the researchers involved, the research supervisor and the director of the Psychosocial Care Center III (CAPs III).
As for the benefits, the results of this study aim to direct more appropriate care to the needs of the center's users diagnosed with depressive disorder, thus contributing to an improvement in care provision and to further research related to the topic and the site under study.
For analysis of results, a database was designed on a spreadsheet prepared in Microsoft Excel 2016 specifically for this purpose, including all the previously mentioned variables. The data obtained were carefully transferred to such database in order to prevent errors related to that procedure. The data obtained were analyzed using Stata 16 software, and the following variables were selected: patients diagnosed with depressive disorder (F32, F32.1, F32.2 F32.3, F32.8 and F32.9), date of birth (age), gender, marital status, education, profession, family history of psychiatric illness, comorbidities, chemical substance use and suicidal ideation.
These variables were chosen because they have been shown, by articles and research, to be the main factors for association and description of the population that is affected by the depressive disorder.
Of the 1,594 records selected, 344 (≅21.58%) comprised the final sample. Of these, 80 reported having only the depressive disorder as the sole diagnosis of mental disorder; however, this study used the 344 medical records of users, since the depressive disorder may be interconnected with other mental disorders and/or even lead the user to develop (an)other mental disorder(s)(15).
Results
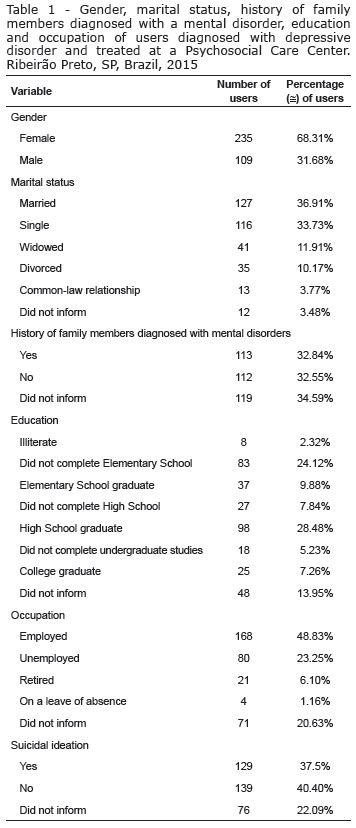
Results showed that, in the medical records of CAPS III users with depressive disorder, there was a prevalence of females with a mean age of 48 years, that is, a minimum age of 17 and a maximum of 78 years. Most of them showed characteristics of not being in a relationship during the study period and an educational level that allowed them to enter and stay active in the job market; no significant variation in the history of family members diagnosed with a mental disorder was found, and finally, no significant variation concerning suicidal ideation was observed. These data are shown in more detail in Table 1.
Most service users had no clinical comorbidities (Figure 1). In the medical records, the word "comorbidity" was used; however, it was not possible to obtain information on how long such users had had that diagnosis or if it was established before or after the diagnosis of depressive disorder. Thus, it was not possible to make an association whether the aforementioned depressive disorder contributed to the emergence of other medical diagnoses or even if the opposite occurred
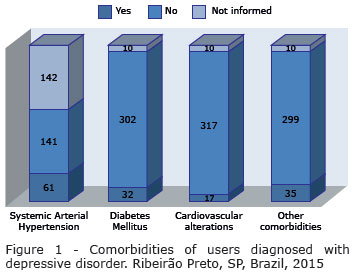
In the medical records evaluated, the questions were objectively presented: that is, only with options to check "Yes", if the user had certain comorbidity, or "No", if he or she did not. Thus, a user who reported having systemic arterial hypertension could also be included in the count of patients with diabetes mellitus, if this occurred, and in a similar fashion the same could occur in relation to other comorbidities. As a consequence, the user could have only one of the comorbidities, two or all of those described in the medical records as options. These data are presented in Figure 1.
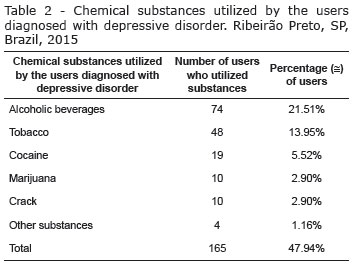
Regarding the use of chemical substances, the questionnaire was designed similarly to that for clinical comorbidity, and again the user could have reported using a chemical substance or not, or could have reported using one or more substances. Thus, he or she could have been included for only one of the chemical substances investigated or for all of those mentioned. According to the medical records, 121 (≅35.17%) users reported the use of a chemical substance, 155 (≅45.05%) reported not using it, and 68 (≅13.76%) did not provide any information. The chemical substances used by the individuals diagnosed with depressive disorder are described in Table 2.
Discussion
Epidemiological studies contribute to a better understanding of the profile of CAP users, which favors the development of strategies addressed at such users as well as further research, especially that related to these psychosocial care centers.
By means of bibliographic surveys, researchers explain that there are some risk factors for the development of a depressive disorder, such as: family history of depression, being a female, a large number of stressful events, low social support and intellectual level, health problems, reduced capacity for coping with stressful situations, excessive personal dependence and genetic factors, among others(16-18).
Importantly, the sample composition has a limitation, and that should be taken into account as data were collected from only one location for a period of two years.
The results in this study showed that there was a higher prevalence of females (≅ 68.31%), which is in agreement with those in several previous investigations(15-16). It is suggested that females have greater sensitivity because of hormonal changes that begin at the onset of menarche and increase their vulnerability to psychological, environmental and physiological stressors during life(16). In women who are more susceptible, such stressors trigger the alteration of a state that is already vulnerable to the manifestation of a mood disorder(16-18).
A study conducted by means of psychiatric interviews showed that the mean prevalence of depression during life was 14.6% for females and 5.5% for males in ten high-income countries, and 11.1% for females and 5.9% for males in eight middle- and low-income countries. In Brazil, in the state of São Paulo, the prevalence was 18.4% for females and 10.4% for males(17). Thus, the data show that women are twice as likely to have depression as men(18).
As for users with a family history of mental illness, research reports that the risk of unaffected first-degree relatives' representing the general population is approximately 5% for depressive episodes. When comparing such risk with that of first-degree relatives of patients with depression, it is observed that, for depressive episodes, the risk increases approximately threefold(19-20), that is, depressive disorder is prevalent among people with a high degree of kinship. However, in the sample there was not a large variation between users who had a family history (≅32.84%) and those who did not (≅32.55%).
According to WHO, a strong relationship between depression and other illnesses has been identified. Depressive disorder increases the risk for developing diabetes and heart disease, and the opposite may also occur, which means that people with other conditions have a higher risk for developing this disorder, as chronic diseases may impose limitations, such as those in mobility, eating, physical activity and the performance of daily, social and work activities(15).
This study showed that most center users had no comorbidities, but it should be pointed out that, given the epidemiological picture presented by several studies, a strong association has been found between depressive disorder and chronic diseases and that people with depression have worse outcomes as to clinical conditions. It is essential that health professionals and services design specific policies and actions for this population(21-22).
WHO encourages investment in mental health as it benefits a country's economic development. Every dollar invested in treating depression has a 4-dollar return in the form of better health and work capacity(8). According to a study conducted by WHO, low levels of acknowledgement and access to care for depression result in a global economic loss of one trillion US dollars each year(8). Losses happen to families, employers and the government alike. Families lose financially when people cannot work; employers suffer when employees become less productive and unable to work, and governments have to pay higher health and welfare expenses(15).
According to the results, the users showed a level of education that would enable them to attend a certificate program or a specialization course and would, therefore, have great chances of entering the labor market. This has been confirmed, as ≅48.83% were active in the labor market (taking into account that ≅6.10% were retiring, that is, that they had contributed in the past). It is also noteworthy that, in addition to being important for the country's economic development, investment in mental health also benefits these people's quality of life.
Research(19-21) shows that people diagnosed with depressive disorder tend to consume more alcohol and that even though that disorder is more prevalent in women, men consume more alcohol and/or drugs when they feel depressed. This shows that men use coping strategies by externalizing, while women tend to internalize symptoms and express sadness in the standard way (withdrawing, dodging social situations and crying). In the study, ≅45.05% of users did not use any chemical substances; however, ≅35.17% of users reported doing it; ≅21.51% reported smoking tobacco, and ≅1.95% reported ingesting alcoholic substances.
As regards to suicidal ideation, WHO points out that depression is a risk factor. Since depression is characterized by persistent sadness and loss of interest in activities that a person normally enjoys. Along with the inability to perform daily activities, it leads to the onset of the following symptoms: loss of energy, changes in appetite, fewer or more sleep hours than usual, anxiety, feelings of worthlessness, guilt and hopelessness, thoughts of self-harm, and ultimately, it can lead to suicide(15). The results in this study show that ≅40.40% reported never having thought about and/or attempted suicide, and ≅37.5% reported having thought about and/or attempted it.
The latter figure, although not the majority, is in agreement with what WHO reports and with the importance of investing in research that describes the profile, incidence and recurrence of mood disorders in order to design programs with support and adequate treatment for the population diagnosed with the disorder.
Conclusion
This study showed that the profile of CAPS III users in Ribeirão Preto had a prevalence of single or divorced/separated female individuals, with a mean age of 48 years, without a family history of mental disorder and with a relatively good educational level, who were active in the job market. In addition, most users had no clinical comorbidities (however, the largest number of those showing one had systemic arterial hypertension). As for the users who utilized a chemical substance, tobacco was reported, followed by alcoholic beverages. Regarding suicidal ideation, although not the majority, there was a large number of users who answered "yes" to both having attempted and having thought of it.
Over the years, WHO has reported that increased financial investment in the mental health field is necessary. In many countries, there is little support available for people with mental disorders, and even in high-income countries, almost 50% of people with depression receive no treatment.
Even though the data were collected from only one mental health service, it is expected that the results in this study will contribute to a better understanding of the users diagnosed with depressive disorder who have been treated at Psychosocial Care Centers or other similar psychiatric care services. From the analysis of variables, services will be able to provide more appropriate treatment to the needs of these users, thus contributing to improvement in the care provided.
References
1. Reis L, Simplicio J, Gherardi-Donato E, Zanetti A. The probabilities of psychiatric hospitalization of mental health clinic patients. SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. [Internet]. 2015;11(2):61-9. [cited Oct 29 2017]. Available from: <https://www.revistas.usp.br/smad/article/view/104738> [ Links ].
2. American Psychiatric Association. DSM-V-TR - Manual Diagnóstico e Estatístico de Transtornos Mentais. 5.ed. Porto Alegre: Artmed; 2014. 976 p. [ Links ]
3. Ministério da Saúde (BR). DATASUS - Departamento de informática do SUS. F30-F39 Transtornos do humor [afetivos] [Internet]. Brasília; 2008. Secretaria - Executiva/MS. [Acesso 29 out 2017]. Disponível em: <http://www.datasus.gov.br/cid10/V2008/cid10.htm> [ Links ].
4. Araújo Á, Lotufo F Neto. A Nova Classificação Americana para os Transtornos Mentais - o DSM-5. RBTCC, Rev Bras Ter Comport Cogn. [Internet]. 2014;16(1):67-2. [Acesso 29 out 2017]. Disponível em: <http://www.usp.br/rbtcc/index.php/RBTCC/article/view/659> [ Links ].
5. Stuart GW, Laraia MT. Enfermagem Psiquiátrica: princípios e prática. 6. ed. São Paulo: Artmed; 2001. 960 p. [ Links ]
6. Demétrio FN, Minatogawa-Chang TM. Curso de capacitação em saúde mental: modulo III: transtornos do humor. [Internet]. São Luis: Universidade Federal do Maranhão, UNASUS/UFMA; 2013. [Acesso 24 out 2017]. Disponível em: <https://ares.unasus.gov.br/acervo/handle/ARES/2044> [ Links ].
7. Dubovsky SL, Dubovsky AN. Transtornos de Humor. Porto Alegre: Artmed; 2004. 328 p. [ Links ]
8. Organização Pan-Americana da Saúde, Organização Mundial da Saúde. Tema do Dia Mundial da Saúde de 2017 - depressão é debatida por especialistas. [Internet]. 2017. [Acesso 24 out 2017]. Disponível em: <http://www.paho.org/bra/index.php?option=com_content&view=article&id=5391:tema-do-dia-mundial-da-saude-de-2017-depressao-e-debatida-por-especialistas-em-evento-na-opas-oms&Itemid=839> [ Links ].
9. Feitosa KMA, Silva T, Silveira MFA, Santos HPO Junior. (Re)construção das práticas em saúde mental: compreensão dos profissionais sobre o processo de desinstitucionalização. Psicol Teor Prat. [Internet]. 2012;14(1),40-54. [Acesso 24 out 2017]. Disponível em: <http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1516-36872012000100004&lng= pt&tlng=pt> [ Links ].
10. Lei nº. 10.216, de 6 de abril de 2001 (BR). Dispõe sobre a proteção e os direitos das pessoas portadoras de transtornos mentais e redireciona o modelo assistencial em saúde mental. [Internet]. 2001. [Acesso 29 out 2017]. Disponível em: <http://www.planalto.gov.br/ccivil_03/leis/leis_2001/l10216.htm> [ Links ].
11. Onocko Campos, RT, Pereira Furtado J, Passos E, Ferrer AL, Miranda L, Pegolo da Gama, CA. Avaliação da rede de centros de atenção psicossocial: entre a saúde coletiva e a saúde mental. Rev Saúde Pública. [Internet]. 2009;43(1):16-22. [Acesso 29 out 2017]. Disponível em: <http://www.redalyc.org/articulo.oa?id=67240181004> [ Links ].
12. Ministério da Saúde (BR). Portaria nº. 336, de 19 de fevereiro de 2002. Dispõe sobre a proteção e os direitos das pessoas portadoras de transtornos mentais e redireciona o modelo assistencial em saúde mental. [Internet]. 2002. [Acesso 29 out 2017]. Disponível em: <http://bvsms.saude.gov.br/bvs/saudelegis/gm/2002/prt0336_19_02_2002.html> [ Links ].
13. Carvalho ER, Rocha HAL. Estudos epidemiológicos. Site do Módulo de Epidemiologia e Bioestatística [Internet]. Fortaleza: Universidade Federal do Ceará: Faculdade de Medicina; 2008. [Acesso 29 out 2017]. Disponível em: <http://www.epidemio.ufc.br/files/05estudosepidemiologicos.pdf> [ Links ].
14. Lima MS de. Epidemiologia e impacto social. Rev Bras Psiquiatr. [Internet]. 1999;21(Suppl1):1-5. [Acesso 29 out 2017]. Disponível em: <http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1516-44461999000500002&lng=en> [ Links ].
15. Baptista MN, Baptista ASD, Oliveira MG de. Depressão e gênero: por que as mulheres deprimem mais que os homens?. Temas Psicol. [Internet]. 1999;7(2):143-56. [Acesso 29 out 2017]. Disponível em: <http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1413-389X1999000200005&lng=pt> [ Links ].
16. Zinga D, Phillips SD, Born L. Depressão pós-parto: sabemos os riscos, mas podemos preveni-la?. Rev Bras Psiquiatr. [Internet]. 2005;27(Suppl2):s56-s64. [Acesso 29 out 2017]. Disponível em: <http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1516-44462005000600005&lng=en> [ Links ].
17. Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, Girolamo G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. [Internet]. 2011;9(1):1-54. [cited Oct 24 2017]. Available from: <https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-9-90> [ Links ].
18. Martin D, Cacozzi A, Macedo T, Andreoli SB. Significado da busca de tratamento por mulheres com transtorno depressivo atendidas em serviço de saúde público. Interface. (Botucatu) [Internet]. 2012;16(43):885-99. [Acesso 29 out 2017]. Disponível em: <http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1414-32832012000400003&lng=pt> [ Links ].
19. Lima IVM, Sougey EB, Vallada FHP. Genética dos transtornos afetivos. Rev Psiquiatr Clín. [Internet]. 2004;31(1):34-9. [Acesso 24 out 2017]. Disponível em: <http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0101-60832004000100006&lng=en> [ Links ].
20. Lafer B, Vallada FHP. Genética e fisiopatologia dos transtornos depressivos. Rev Bras Psiquiatr. [Internet]. 1999;21(Suppl1):12-17. [Acesso 24 out 2017]. Disponível em: <http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1516-44461999000500004&lng=en> [ Links ].
21. Andrade TMR, Argimon IIL. Sintomas depressivos e o uso de substâncias psicoativas durante a vida em adolescentes. Rev Bras Terap Cognitivas. [Internet]. 2006;2(1):95-104. [Acesso 24 out 2017]. Disponível em: <http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1808-56872006000100010&lng =pt&tlng=pt> [ Links ].
22. Perez GH, Nicolau JC, Romano BW, Laranjeira R. Depressão e síndromes isquêmicas miocárdicas instáveis: diferenças entre homens e mulheres. Arq Bras Cardiol. [Internet]. 2005;85(5):319-26. [Acesso 24 out 2017]. Disponível em: <http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0066-782X2005001800004&lng=en> [ Links ]
Received: Aug 5th 2019 Authors' contribution: Study design and planning: Lorraine Garbellini Barbosa Lima, Ariana Elite Dos Santos, Luiz Jorge Pedrão. Data collection: Lorraine Garbellini Barbosa Lima, Ariana Elite Dos Santos, Bruna Lopes Cardoso Dos Santos. Data analysis and interpretation: Lorraine Garbellini Barbosa Lima, Ariana Elite Dos Santos, Luiz Jorge Pedrão. Manuscript writing: Lorraine Garbellini Barbosa Lima. Critical review of the manuscript: Lorraine Garbellini Barbosa Lima, Ariana Elite Dos Santos, Luiz Jorge Pedrão. Corresponding author:
Corresponding author:
Lorraine Garbellini Barbosa Lima
E-mail:lorrainegbl@hotmail.com
Accepted: Sept 11th 2019
All authors approved the final version of the text.
Conflict of interests: The authors attest that there are no conflicts of interest.











 texto em
texto em 


